Abstract
Neuromuscular blocking agents play a significant role in improving the success rate for urgent intubation, although there is limited evidence about the effect on subsequent outcomes, such as the incidence of tracheostomy. In this retrospective cohort study, we aimed to examine the association between avoidance of neuromuscular blocking agents for urgent tracheal intubation and incidence of tracheostomy among patients in the intensive care unit (ICU). The setting of this study was an eight-bed ICU at a tertiary-care hospital in Okayama, Japan. We included patients who underwent urgent tracheal intubation at the emergency department or the ICU and were admitted to the ICU between April 2013 and November 2017. We extracted data on methods and medications of intubation, predictors for difficult intubation, Cormack–Lehane grade, patient demographics, primary diagnoses, reintubation. We estimated odds ratios and their 95% confidence intervals for elective tracheostomy during the ICU stay using logistic regression models. Of 411 patients, 46 patients underwent intubation without neuromuscular blocking agents and 61 patients underwent tracheostomy. After adjusting for potential confounders, patients who avoided neuromuscular blocking agents had more than double the odds of tracheostomy (odds ratio 2.59, 95% confidence interval 1.06–6.34, p value = 0.04). When stratifying the subjects by risk status for tracheostomy, the association was more pronounced in high-risk group, while we observed less significant association in the low-risk group. Avoidance of neuromuscular blocking agents for urgent intubation increases the risk of tracheostomy among emergency patients, especially those who have a higher risk for tracheostomy.
Electronic supplementary material
The online version of this article (10.1007/s11739-019-02214-0) contains supplementary material, which is available to authorized users.
Keywords: Airway management, Emergency patients, Neuromuscular blocking agents, Tracheostomy
Introduction
Tracheostomy should generally be performed for mechanically ventilated patients in the intensive care unit (ICU). There are notable differences between patients undergoing planned surgery and emergency patients with respect to patient characteristics and the circumstances under which tracheal intubation is performed. Despite these known differences, however, the evidence for factors associated with the increased risk of tracheostomy for emergency patients remains sparse. There have been no studies examining risk factors for tracheostomy in patients undergoing urgent tracheal intubation.
A previous study suggested the importance of using a neuromuscular blocking agent (NMBA) to facilitate tracheal intubation under urgent conditions [1]. A meta-analysis showed that avoiding NMBA was associated with an increased risk of both a difficult tracheal intubation and an upper airway injury [2]. Because these complications could lead to subsequent negative outcomes, such as reintubation or tracheostomy, it is important to examine the effects of avoiding NMBA for urgent tracheal intubation. This is especially true in emergency departments (EDs) in Japan, where using NMBA for emergency airway management is not very common [3] (although we do use NMBA in our ED). Despite the potential benefit of this modifiable intervention, however, it remains unclear whether the avoidance of NMBA is associated with subsequent negative in-hospital outcomes.
Accordingly, we aimed to examine the association between the avoidance of NMBA for urgent tracheal intubation and the incidence of tracheostomy among patients in an ICU in Japan.
Methods
The setting of this study was an eight-bed ICU at the Emergency and Critical Care Center of Kurashiki Central Hospital, which is a tertiary-care hospital located in Okayama prefecture, Japan. The ICU accommodates patients who need emergency admission, including medical, trauma, and emergency surgery patients. The ED has emergency attending physicians and is affiliated with an emergency medicine residency program. The hospital receives approximately 60,000 ED visits annually.
Rocuronium bromide is typically used for tracheal intubation in our ED, although succinylcholine is occasionally used, depending on the patient’s clinical situation. By tradition, we use a rapid-sequence intubation technique, unless a difficult airway or high risk of desaturation is predicted. In such cases, we perform awake intubation or perform delayed-sequence intubation. A C-MAC videolaryngoscope (Karl Storz, Tuttlingen, Germany) and direct laryngoscope are available in our ED. In collaboration with other medical specialists, a team of intensivists cares for all patients in the ICU and assesses the timing and indication for tracheostomy.
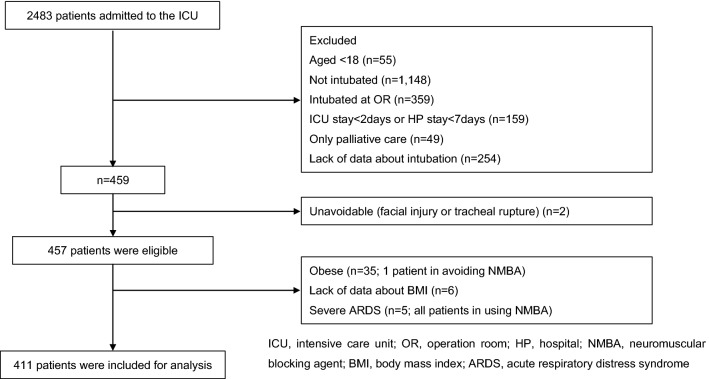
For the current study, we included data from all patients who were admitted to our ICU via the ED and eventually underwent urgent intubation between April 2013 and November 2017. The intubation had to take place in the ED or ICU. We excluded those patients who required only palliative care, were younger than 18 years of age, and/or in whom tracheostomy was unavoidable because of their primary disease or a failed intubation. We also excluded patients who underwent intubation in the operating room, because such patients were electively intubated. In general, patients are either critical and die shortly after admission or leave the ICU quickly without a critical situation. Because such patients are unlikely to undergo elective tracheostomy during their ICU stay, we excluded patients whose length of ICU stay was less than 2 days and/or whose overall length of hospital stay was less than 7 days. Further, because we often transfer patients with severe acute respiratory distress syndrome (ARDS) to an extracorporeal membrane oxygenation (ECMO) center and are unable to collect the data of primary outcome, we excluded these patients as well. The diagnosis and classification of ARDS were made according to the Berlin definition [4].
Data collection
We collected the following data from the Kurashiki Central Hospital’s ICU database: whether elective tracheostomy was performed, patient demographics (age, sex, height, weight, comorbidities), diagnosis on admission, the Sequential Organ Failure Assessment (SOFA) score [5], Injury Severity Score (ISS) [6], the presence of delirium, ventilator-associated pneumonia (VAP), the presence of ARDS, whether reintubation was required, the number of days on a ventilator, and ICU mortality. Diagnoses on admission were categorized into the following 11 disease groups: cardiovascular, respiratory, gastrointestinal and liver, neurological, sepsis (from a urinary tract infection or unknown origin), trauma, metabolic, hematologic, urogenital, musculoskeletal, and uncategorized medical disease. VAP was diagnosed according to the new Centers for Disease Control and Prevention criteria for ventilator-associated events [7]. For the purposes of this study, VAP includes infection-related ventilator-associated complications and possible VAP. We also obtained information about the length of hospital stay and hospital mortality from medical records.
Additionally, we extracted a subset of patient data from the registry of the Japanese Emergency Airway Network 2 (JEAN2) study. The JEAN2 study was a prospective, observational, multicenter study designed to characterize current airway management practices in Japanese EDs. The study’s setting, methods of measurement, and measured variables have been previously described [8, 9]. From the registry, we collected information about adverse events during intubation (including hypoxemia, defined as a pulse oximetry saturation < 90%; hypotension, defined as a systolic blood pressure < 90 mmHg; esophageal intubation; and the presence of an airway injury, defined as any oral, laryngeal, and/or pharyngeal edema, laceration, bleeding, or dental injury related to the intubation procedure); methods, devices, and medications used for airway management; whether intubation was performed during cardiopulmonary resuscitation (CPR); predictors for difficult intubation (such as an abnormal facial shape, including those due to facial injury and anatomic abnormalities; neck mobility limitations; airway obstruction, except for sputum and glossoptosis; and a mouth opening of less than three finger breadths); the Cormack–Lehane grade [10]; the level of training and specialty of the intubator; and the number of intubation attempts. The number of intubation attempts was defined as the number of insertions of the laryngoscope past the teeth. In the JEAN2 database, the intensivists in our institution were registered as emergency physicians due to the lack of such items for that study. All intensivists in our institution complete a fellowship for emergency physicians and become board-certified emergency physicians.
Outcome measures
Our primary outcome of interest was the incidence of elective tracheostomy that was required during the ICU stay. We used the incidence of tracheostomy itself as our outcome, irrespective of the reason that tracheostomy was required, so as not to underestimate the effect of avoiding NMBA. We examined adverse events during intubation (i.e., hypoxemia, hypotension, esophageal intubation, and airway injury), which were assessed at the time of intubation, as secondary outcomes.
Statistical analysis
To evaluate patient characteristics and outcomes, we used the Mann–Whitney U test for continuous variables and Fisher’s exact test or the Chi-squared test for categorical variables. Then, we performed a multivariable logistic regression analysis to estimate odds ratios (ORs) and their 95% confidence intervals (CIs) for the need for tracheostomy during the ICU stay and adverse events during intubation. To account for potential confounders, we adjusted for age, sex, the performance of cardiopulmonary arrest before intubation, an abnormal facial shape, the presence of an airway obstruction, and neck mobility limitations. We also considered obesity as a potential confounder, and patients with a body mass index ≥ 30 kg/m2 were excluded from analysis because the numbers of these patients were extremely low, especially in the non-NMBA group. A previous study reported an association between reintubation and a higher incidence of tracheostomy [11]. Because we considered reintubation as an intermediate variable between avoiding NMBA and tracheostomy, we did not adjust for reintubation.
We conducted subgroup analyses after stratifying by the risk for tracheostomy (high vs. low). As reported in previous studies [12–17], the high-risk group was defined as those with cardiopulmonary arrest (CPA), intracranial hemorrhage, infection of the central nervous system, epilepsy, convulsion, altered mental status (e.g., metabolic encephalopathy), spinal cord injury, traumatic brain injury, and/or respiratory disease. We also performed a sensitivity analysis after excluding patients who underwent intubation during CPR.
All analyses were performed using Stata version 15.1 software (Stata, College Station, TX). We considered a p value of < 0.05 (two-tailed) as statistically significant.
This study was approved by the institutional ethics committees at Kurashiki Central Hospital (No. 2955, November 13, 2018) and Okayama University (No. 1901-024, January 25, 2019). The need for informed consent was waived due to the retrospective nature of the study.
Results
A total of 411 patients were included in the analysis (Fig. 1). Their baseline characteristics are shown in Table 1. Tracheostomy was performed in 61 (14.8%) patients. Intubation using video laryngoscopy was performed in 386 patients (93.9%), and direct laryngoscopy was used for the remaining patients. No patients were intubated using flexible fiber optic intubation, nasotracheal intubation, or digital intubation. The numbers of CPA patients and urgent surgery patients were 16 (3.9%) and 139 (33.8%), respectively. The number of trauma patients was 170 (41.4%), and their median ISS was 23.5 (interquartile range 14‒34).
Fig. 1.
study flow diagram
Table 1.
Characteristics of the study participants by avoiding neuromuscular blocking agent
| Total n = 411 | Avoiding NMBA n = 46 | Using NMBA n = 365 | p value | |
|---|---|---|---|---|
| Tracheostomy during the ICU stay, n (%) | 61 (14.8) | 16 (34.8) | 45 (12.3) | < 0.001 |
| Adverse events during intubation, n (%) | 98 (23.8) | 8 (17.4) | 90 (24.7) | 0.18 |
| Esophageal intubation, n (%) | 2 (0.5) | 0 (0) | 2 (0.6) | 1.00 |
| Airway injury, n (%) | 7 (1.7) | 1 (2.2) | 6 (1.6) | 0.57 |
| Hypoxemia, n (%) | 23 (5.6) | 3 (6.5) | 20 (5.5) | 0.73 |
| Hypotension, n (%) | 73 (17.8) | 4 (8.7) | 69 (18.9) | 0.10 |
| ICU mortality, n (%) | 17 (4.1) | 3 (6.5) | 14 (3.8) | 0.42 |
| Hospital mortality, n (%) | 74 (18.0) | 12 (26.1) | 62 (17.0) | 0.15 |
| Length of ICU stay (days), median (IQR) | 6 (4–10) | 7.5 (5–12) | 6 (4–10) | 0.09 |
| Length of HP stay (days), median (IQR) | 26 (14–42) | 21 (11–42) | 26 (15–42) | 0.15 |
| Ventilator days, median (IQR) | 4 (2–7) | 5 (3–9) | 4 (2–7) | 0.01 |
| Sex (male), n (%) | 259 (63.0) | 27 (58.7) | 232 (63.6) | 0.52 |
| Age (years), median (IQR) | 70 (55–79) | 74 (61–82) | 69 (55–79) | 0.12 |
| BMI (kg/m2), median (IQR) | 21.9 (19.7–24.4) | 20.7 (17.9–23.2) | 22.1 (19.9–24.6) | 0.006 |
| SOFA score, median (IQR) | 6 (4–9) | 7 (4–10) | 6 (4–9) | 0.14 |
| ISS, median (IQR) | 23.5 (14–34) | 22 (17–26) | 25 (14–34) | 0.94 |
| Underlying disease, n (%) | ||||
| Chronic kidney disease | 15 (3.7) | 2 (4.4) | 13 (3.6) | 0.68 |
| Dialysis | 8 (2) | 2 (4.4) | 6 (1.6) | 0.22 |
| Liver cirrhosis or failure | 24 (5.8) | 2 (4.4) | 22 (6.0) | 0.48 |
| Malignancies | 28 (6.9) | 1 (2.2) | 27 (7.5) | 0.35 |
| Immunosuppressive state | 6 (1.5) | 2 (4.4) | 4 (1.1) | 0.13 |
| Diabetes mellitus | 101 (24.6) | 13 (28.3) | 88 (24.1) | 0.59 |
| Disease group, n (%) | ||||
| Cardiovascular | 19 (4.6) | 11 (23.9) | 8 (2.2) | |
| Pulmonary | 60 (14.6) | 10 (21.7) | 50 (13.7) | |
| Gastrointestinal and liver | 77 (18.7) | 2 (4.4) | 75 (20.6) | |
| Neurogenic | 21 (5.1) | 1 (2.2) | 20 (5.5) | |
| Sepsis (unknown origin or urinary tract infection) | 15 (3.7) | 2 (4.4) | 13 (3.6) | |
| Trauma | 170 (41.4) | 14 (30.4) | 156 (42.7) | |
| Metabolic | 25 (6.1) | 5 (10.9) | 20 (5.5) | |
| Hematology | 1 (0.2) | 0 (0) | 1 (0.3) | |
| Urinary | 8 (2) | 0 (0) | 8 (2.2) | |
| Musculoskeletal | 11 (2.7) | 1 (2.2) | 10 (2.7) | |
| Medical (other) | 3 (0.7) | 0 (0) | 3 (0.8) | |
| Obstetrics and gynecology | 1 (0.2) | 0 (0) | 1 (0.3) | < 0.001 |
| CPA before intubation, n (%) | 16 (3.9) | 14 (30.4) | 2 (0.6) | < 0.001 |
| Reintubation, n (%) | 26 (6.3) | 6 (13) | 20 (5.5) | 0.06 |
| VAP, n (%) | 24 (5.8) | 3 (6.5) | 21 (5.8) | 0.74 |
| Delirium, n (%) | 87 (23.5) | 9 (24.3) | 78 (23.4) | 0.84 |
| Methods and medication of intubation, n (%) | ||||
| No drug | 26 (6.3) | 26 (56.5) | – | |
| Analgesic + sedatives | 20 (4.9) | 20 (43.5) | – | |
| RSI (NMBA + analgesic + sedatives) | 351 (85.4) | – | 351 (96.2) | |
| NMBA | 7 (1.7) | – | 7 (1.9) | |
| NMBA + sedatives | 7 (1.7) | – | 7 (1.9) | < 0.001 |
| Video laryngoscopy, n (%) | 386 (93.9) | 37 (80.4) | 349 (95.6) | 0.001 |
| Abnormal facial shape, n (%) | 23 (5.8) | 4 (8.7) | 19 (5.4) | 0.32 |
| Airway obstruction, n (%) | 8 (2.0) | 5 (10.9) | 3 (0.8) | 0.001 |
| Neck mobility limitation, n (%) | 115 (28.4) | 13 (28.9) | 102 (28.3) | 1.00 |
| Opening mouth limitation, n (%) | 92 (25.9) | 12 (31.6) | 80 (25.2) | 0.43 |
| GCS before intubation, median (IQR) | 13 (7–15) | 3.5 (3–13) | 13 (9–15) | < 0.001 |
| Cormack–Lehane grade, n (%) | ||||
| 1 | 290 (72) | 25 (55.6) | 265 (74) | |
| 2 | 93 (23.1) | 14 (31.1) | 79 (22.1) | |
| 3 | 18 (4.5) | 5 (11.1) | 13 (3.6) | |
| 4 | 2 (0.5) | 1 (2.2) | 1 (0.3) | 0.01 |
| Specialty of the intubator, n (%) | ||||
| Resident (PGY 1, 2) | 72 (17.5) | 5 (10.9) | 67 (18.4) | |
| EM resident (PGY 3–5) | 201 (48.9) | 22 (47.8) | 179 (49.0) | |
| EM fellow or attendinga | 130 (31.6) | 19 (41.3) | 111 (30.4) | |
| Anesthesiologist | 2 (0.5) | 0 (0) | 2 (0.6) | |
| Pediatrician | 6 (1.5) | 0 (0) | 6 (1.6) | 0.53 |
| Multiple attempts, n (%) | 56 (13.6) | 12 (26.1) | 44 (12.1) | 0.02 |
IQR interquartile range, SD standard deviation, NMBA neuromuscular blocking agent, ICU intensive care unit, HP hospital, BMI body mass index, SOFA score Sequential Organ Failure Assessment Score, ISS Injury Severity Score, CPA cardiopulmonary arrest, VAP ventilator associated pneumonia, ARDS acute respiratory distress syndrome, RSI rapid sequence induction, GCS Glasgow Coma Scale, PGY post graduate year, EM emergency medicine
aEM attending included intensivist
Compared with patients who underwent intubation with NMBA, those who avoided NMBA tended to undergo tracheostomy and were more often admitted because of respiratory disease and CPA. Most patients in the cardiovascular group (81.3%) had CPA before tracheal intubation.
We examined the association between the avoidance of NMBA and tracheostomy with logistic regression models (Table 2). In a crude model, the OR for tracheostomy among patients who avoided NMBA compared with patients who used NMBA was 3.79 (95% CI 1.92‒7.50, p < 0.001). Even after adjusting for potential confounders, patients who avoided NMBA had more than double the risk of tracheostomy compared to those who used NMBA (OR 2.59, 95% CI 1.06‒6.34, p = 0.04).
Table 2.
Odds ratios for tracheostomy associated with avoiding neuromuscular blocking agent
| Variables | Crude model | Adjusted model | ||
|---|---|---|---|---|
| OR (95% CI) | p value | OR (95% CI) | p value | |
| Avoiding NMBA | 3.79 (1.92–7.50) | < 0.001 | 2.59 (1.06–6.34) | 0.04 |
| Age (years) | 1.02 (1.00–1.04) | 0.02 | ||
| Sex (male) | 0.92 (0.50–1.70) | 0.79 | ||
| Intubated during CPR | 3.94 (0.85–18.22) | 0.08 | ||
| Abnormal facial shape | 6.45 (2.34–17.83) | < 0.001 | ||
| Neck mobility limitation | 1.59 (0.80–3.13) | 0.18 | ||
| Airway obstruction | 1.90 (0.31–11.81) | 0.49 | ||
NMBA neuromuscular blocking agent, OR odds ratio, CI confidence interval, CPR cardiopulmonary resuscitation
When stratifying patients by risk status for tracheostomy, the association between the avoidance of NMBA and tracheostomy was more pronounced in the high-risk group than in the low-risk group (Table 3). After excluding patients who underwent intubation during CPR, we observed similar results (Table 4).
Table 3.
Modification of the effect of avoiding neuromuscular blocking agent on tracheostomy by risk status
| Using NMBA | Avoiding NMBA | OR (95% CI); within strata of risk status | p value | |||||
|---|---|---|---|---|---|---|---|---|
| n with/without outcome | OR (95% CI) | p value | n with/without outcome | OR (95% CI) | p value | |||
| Low risk | 16/233 | Reference | 3/17 | 1.65 (0.37–7.36) | 0.52 | 1.65 (0.37–7.36) | 0.52 | |
| High risk | 29/87 | 4.00 (1.96–8.18) | < 0.001 | 13/13 | 12.12 (3.81–38.48) | < 0.001 | 3.39 (1.08–10.62) | 0.04 |
ORs are adjusted for age, sex, neck mobility limitation, abnormal facial shape, airway obstruction, and cardiopulmonary arrest before intubation
High-risk status: post cardiac arrest, cerebral bleeding, infection of the central nervous system, epilepsy, convulsion, altered mental status (e.g. metabolic encephalopathy), spinal cord injury, traumatic brain injury, and respiratory disease
NMBA neuromuscular blocking agent, OR odds ratio, CI confidence interval
Table 4.
Modification of the effect of avoiding NMBA in the analysis excluding patients who underwent intubation during CPR
| Using NMBA | Avoiding NMBA | OR (95% CI); within strata of risk status | p value | |||||
|---|---|---|---|---|---|---|---|---|
| n with/without outcome | OR (95% CI) | p value | n with/without outcome | OR (95% CI) | p value | |||
| Low risk | 16/233 | Reference | 3/16 | 1.69 (0.37–7.72) | 0.50 | 1.69 (0.37–7.72) | 0.50 | |
| High risk | 29/87 | 3.99 (1.94–8.18) | < 0.001 | 8/9 | 11.45 (3.56–36.82) | < 0.001 | 3.24 (1.04–10.07) | 0.04 |
ORs are adjusted for age, sex, neck mobility limitation, abnormal facial shape, airway obstruction
High-risk status: post cardiac arrest, cerebral bleeding, infection of the central nervous system, epilepsy, convulsion, altered mental status (e.g. metabolic encephalopathy), spinal cord injury, traumatic brain injury, and respiratory disease
CPR cardiopulmonary resuscitation, NMBA neuromuscular blocking agent, OR odds ratio, CI confidence interval
Regarding adverse events during intubation, we found no remarkable differences between the NMBA group and the non-NMBA group (Table 1). Furthermore, we found no significant association between avoiding NMBA for urgent intubation and adverse events during intubation (Online Resource 1).
Discussion
In this retrospective cohort study, we investigated the association between the avoidance of NMBA for urgent tracheal intubation and the incidence of tracheostomy in the ICU. Our findings suggest that avoiding NMBA is associated with a high incidence of tracheostomy during the ICU stay among high-risk patients, but we observed a less clear association among low-risk patients. To our knowledge, this is the first study to examine the association between the avoidance of NMBA for urgent intubation and in-hospital outcomes.
The association between the avoidance of NMBA and subsequent tracheostomy could potentially be explained by the mechanism of soft tissue damage during tracheal intubation. A previous study reported that difficulties in tracheal intubation can cause serious soft tissue damage [18]. Injury to the larynx or trachea can yield upper airway obstruction and/or vocal cord paralysis, resulting in the need for tracheostomy. Because NMBA inhibits muscular contractions and improves conditions for tracheal intubation [19], it would consequently decrease soft tissue damage and the need for tracheostomy.
In a subgroup analysis, the association between the avoidance of NMBA and subsequent tracheostomy was more pronounced in the high-risk group than in the low-risk group, suggesting effect modification by the risk status for tracheostomy. These findings suggest that airway injuries were more likely to develop due to certain mechanisms among the patients with a higher risk for tracheostomy. We a posteriori hypothesized that the variables associated with difficult intubation (i.e., Cormack–Lehan grade, the number of predictors for difficult intubation) resulted in an increased risk of airway injury among these patients. However, the distributions of these variables were similar between the high-risk group and the low-risk group, and the number of airway injuries was quite small (Online Resource 2). We should note that it is possible that this information was inaccurate because the injuries were self-reported. Furthermore, the data we collected may be insufficient for evaluating the extent of soft tissue damage during urgent intubation. For example, information about the amount of time required for intubation and how gently intubation was performed is necessary. In addition, minor soft tissue damage is often unrecognized and unreported at the time of intubation, which presents as vocal cord paralysis or laryngeal edema only after extubation, and unreported airway injuries would also more likely lead to the need for tracheostomy. Further studies are needed to validate the potential effect modification observed in this study.
Consistent with the results of a previous study [20], we found no significant association between the avoidance of NMBA and the incidence of adverse events during intubation. This result suggests that our finding about the incidence of tracheostomy in the ICU may be applicable to other populations. Further, it is notable that the avoidance of NMBA may result in long-term negative outcomes (i.e., the incidence of tracheostomy), whereas it may have no substantial effect on short-term outcomes.
The two prospective databases used in this study included relatively little missing data. The ICU database contained data for all consecutive patients who were admitted to our ICU. The capture rate of data for the JEAN2 study was reported to be high (96%), and the investigators monitored physicians’ compliance with data form completion. Furthermore, they immediately reviewed medical records and interviewed the involved physicians to ascertain airway management details [21, 22]. These procedures contributed to providing us with high-quality data.
In our cohort, more than 10% of patients underwent intubation without NMBA, and 61 patients (14.8%) underwent tracheostomy later during the ICU stay. In previous studies, 16–28% of emergency intubations were performed without NMBA [1, 23]. Furthermore, previous studies have reported that 13–24% of critically ill patients were tracheotomized [12, 24]. Thus, the proportions of patients who were intubated without NMBA or who were tracheotomized during the ICU stay were similar to those in previous studies. We therefore believe that our findings are generalizable across different contexts and patient populations.
There are some limitations to this study. First, because the sample size was relatively small, the number of patients who underwent tracheostomy was small. We therefore could only adjust for a limited number of potential confounders and only stratify by two groups. By carefully choosing potential confounders based on pathophysiological hypotheses, we considered the number of intubation attempts, VAP, prolonged ventilation, and reintubation as intermediate variables between avoidance of NMBA and tracheostomy.
Second, this is a single-center study, and the generalizability of our findings may be limited. Because cardiogenic shock, stroke, and neurosurgery patients mainly get admitted to other intensive care units in Kurashiki Central Hospital, our findings may not apply to these patients. Furthermore, we decided to exclude patients with obesity or severe ARDS from the analysis because the number of these patients was very small. However, given that our center accepts most emergency patients from a typical medium-sized city in Japan, we believe that our study participants include a wide range of emergency patients requiring critical care.
Conclusions
Our study suggests that the avoidance of NMBA for urgent intubation increases the risk of subsequent tracheostomy among emergency patients, especially among those who have a higher risk for tracheostomy. This finding is vital because NMBA can be easily implemented as a modifiable intervention for urgent intubation and can improve longer-term outcomes. Further studies are warranted to examine this hypothesis in larger and prospective settings, by determining whether the dose and effect of NMBA was optimal, the time required for intubation, the patient’s position at the time of intubation, and vocal cord dysfunction or laryngeal edema after extubation.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank Toshie Kaihara, Hiroshi Okamoto, Toshio Fukuoka, and Tetsunori Ikegami for their help with this study.
Author contributions
JF designed the study, collected data, performed statistical analysis of data, and writing the draft. ES helped with the study design, helped with the interpretation of data, and critically revised the manuscript. AK and MO critically reviewed the manuscript. HD helped with the study design and critically reviewed the manuscript. All authors read and approved the final version of the manuscript.
Funding
ES is supported by the Japan Society for the Promotion of Science (KAKENHI Grant Nos. JP17K17898, JP15K08776, and JP18K10104) and The Okayama Medical Foundation. The funding sources had no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
This study was approved by the institutional ethics committee at Kurashiki Central Hospital (No. 2955, November 13, 2018) and Okayama University (No. 1901-024, January 25, 2019).
Informed consent
The requirement to obtain informed consent was waived.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sakles JC, Laurin EG, Rantapaa AA, Panacek EA. Airway management in the emergency department: a 1-year study of 610 tracheal intubations. Ann Emerg Med. 1998;31:325–332. doi: 10.1016/S0196-0644(98)70342-7. [DOI] [PubMed] [Google Scholar]
- 2.Lundstrøm LH, Duez CHV, Nørskov AK, et al. Effects of avoidance or use of neuromuscular blocking agents on outcomes in tracheal intubation: a Cochrane systematic review. Br J Anaesth. 2018;120(6):1381–1393. doi: 10.1016/j.bja.2017.11.106. [DOI] [PubMed] [Google Scholar]
- 3.Okubo M, Gibo K, Hagiwara Y, et al. The effectiveness of rapid sequence intubation (RSI) versus non-RSI in emergency department: an analysis of multicenter prospective observational study. Int J Emerg Med. 2017;10:1. doi: 10.1186/s12245-017-0129-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.ARDS Definition Task Force Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307(23):2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 5.Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure: On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–710. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]
- 6.BAKER SUSAN P., OʼNEILL BRIAN, HADDON WILLIAM, LONG WILLIAM B. THE INJURY SEVERITY SCORE. The Journal of Trauma: Injury, Infection, and Critical Care. 1974;14(3):187–196. doi: 10.1097/00005373-197403000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Center for Disease Control and Prevention (2018) National Healthcare Safety Network: surveillance for ventilator-associated events. https://www.cdc.gov/nhsn/acute-care-hospital/vae/index.html. Accessed 7 Jun 2019
- 8.Goto T, Gibo K, Hagiwara Y, et al. Multiple failed intubation attempts are associated with decreased success rates on the first rescue intubation in the emergency department: a retrospective analysis of multicentre observational data. Scand J Trauma Resusc Emerg Med. 2015;23:5. doi: 10.1186/s13049-014-0085-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goto T, Watase H, Morita H, et al. Repeated attempts at tracheal intubation by a single intubator associated with decreased success rates in emergency departments: an analysis of a multicentre prospective observational study. Emerg Med J. 2015;32:781–786. doi: 10.1136/emermed-2013-203473. [DOI] [PubMed] [Google Scholar]
- 10.Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39:1105–1111. doi: 10.1111/j.1365-2044.1984.tb08932.x. [DOI] [PubMed] [Google Scholar]
- 11.Lin HT, Ting PC, Chang WY, Yang MW, Chang CJ, Chou AH. Predictive risk index and prognosis of postoperative reintubation after planned extubation during general anesthesia: a single-center retrospective case-controlled study in Taiwan from 2005 to 2009. Acta Anaesthesiol Taiwan. 2013;51:3–9. doi: 10.1016/j.aat.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 12.Abe T, Madotto F, Pham T, et al. Epidemiology and patterns of tracheostomy practice in patients with acute respiratory distress syndrome in ICUs across 50 countries. Crit Care. 2018;22:195. doi: 10.1186/s13054-018-2126-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Branco BC, Plurad D, Green DJ, et al. Incidence and clinical predictors for tracheostomy after cervical spinal cord injury: a National Trauma Databank review. J Trauma. 2011;70:111–115. doi: 10.1097/TA.0b013e3181d9a559. [DOI] [PubMed] [Google Scholar]
- 14.Heffernan DS, Vera RM, Monaghan SF, et al. Impact of socioethnic factors on outcomes following traumatic brain injury. J Trauma. 2011;70:527–534. doi: 10.1097/TA.0b013e31820d0ed7. [DOI] [PubMed] [Google Scholar]
- 15.Agarwal S, Sobczak E, Presciutti A, et al. Tracheostomy use, long-term survival, and neurological outcomes among cardiac arrest survivors. Resuscitation. 2018;129:e19–e20. doi: 10.1016/j.resuscitation.2018.06.017. [DOI] [PubMed] [Google Scholar]
- 16.McCredie VA, Ferguson ND, Pinto RL, et al. Airway management strategies for brain-injured patients meeting standard criteria to consider extubation: a prospective cohort study. Ann Am Thorac Soc. 2017;14:85–93. doi: 10.1513/AnnalsATS.201608-620OC. [DOI] [PubMed] [Google Scholar]
- 17.Schubert J, Brämer D, Huttner HB, et al. Management and prognostic markers in patients with autoimmune encephalitis requiring ICU treatment. Neurol Neuroimmunol Neuroinflamm. 2018;30(6):e514. doi: 10.1212/NXI.0000000000000514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Domino KB, Posner KL, Caplan RA, Cheney FW (1999) Airway injury during anesthesia: a closed claims analysis. Anesthesiology 91:1703–1711. Available from, http://anesthesiology.pubs.asahq.org/article.aspx?volume=91&page=1703. Accessed 21 Jun 2019 [DOI] [PubMed]
- 19.Higgs A, McGrath BA, Goddard C, et al. Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth. 2018;120:323–352. doi: 10.1016/j.bja.2017.10.021. [DOI] [PubMed] [Google Scholar]
- 20.Mosier JM, Sakles JC, Stolz U, et al. Neuromuscular blockade improves first-attempt success for intubation in the intensive care unit. A propensity matched analysis. Ann Am Thorac Soc. 2015;12:734–741. doi: 10.1513/AnnalsATS.201411-517OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yakushiji H, Goto T, Shirasaka W, et al. Associations of obesity with tracheal intubation success on first attempt and adverse events in the emergency department: an analysis of the multicenter prospective observational study in Japan. PLoS One. 2018;13(4):e0195938. doi: 10.1371/journal.pone.0195938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goto Y, Goto T, Hagiwara Y, et al. Techniques and outcomes of emergency airway management in Japan: an analysis of two multicentre prospective observational studies, 2010–2016. Resuscitation. 2017;114:14–20. doi: 10.1016/j.resuscitation.2017.02.009. [DOI] [PubMed] [Google Scholar]
- 23.Martin LD, Mhyre JM, Shanks AM, Tremper KK, Kheterpal S. 3,423 emergency tracheal intubations at a University Hospital: airway outcomes and complications. Anesthesiology. 2011;114:42–48. doi: 10.1097/ALN.0b013e318201c415. [DOI] [PubMed] [Google Scholar]
- 24.Nathens AB, Rivara FP, Mack CD, et al. Variations in rates of tracheostomy in the critically ill trauma patients. Crit Care Med. 2006;34:2919–2924. doi: 10.1097/01.CCM.0000243800.28251.AE. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.