Abstract
Background
Elevated high-sensitivity troponin (hsTnT) after noncardiac surgery is associated with higher mortality, but the temporal relationship between early elevated troponin and the later development of noncardiac morbidity remains unclear.
Methods
Prospective observational study of patients aged ≥45 yr undergoing major noncardiac surgery at four UK hospitals (two masked to hsTnT). The exposure of interest was early elevated troponin, as defined by hsTnT >99th centile (≥15 ng L−1) within 24 h after surgery. The primary outcome was morbidity 72 h after surgery, defined by the Postoperative Morbidity Survey (POMS). Secondary outcomes were time to become morbidity-free and Clavien–Dindo ≥grade 3 complications.
Results
Early elevated troponin (median 21 ng L−1 [16–32]) occurred in 992 of 4335 (22.9%) patients undergoing elective noncardiac surgery (mean [standard deviation, sd] age, 65 [11] yr; 2385 [54.9%] male). Noncardiac morbidity was more frequent in 494/992 (49.8%) patients with early elevated troponin compared with 1127/3343 (33.7%) patients with hsTnT <99th centile (odds ratio [OR]=1.95; 95% confidence interval [CI], 1.69–2.25). Patients with early elevated troponin had a higher risk of proven/suspected infectious morbidity (OR=1.54; 95% CI, 1.24–1.91) and critical care utilisation (OR=2.05; 95% CI, 1.73–2.43). Clavien–Dindo ≥grade 3 complications occurred in 167/992 (16.8%) patients with early elevated troponin, compared with 319/3343 (9.5%) patients with hsTnT <99th centile (OR=1.78; 95% CI, 1.48–2.14). Absence of early elevated troponin was associated with morbidity-free recovery (OR=0.44; 95% CI, 0.39–0.51).
Conclusions
Early elevated troponin within 24 h of elective noncardiac surgery precedes the subsequent development of noncardiac organ dysfunction and may help stratify levels of postoperative care in real time.
Keywords: cardiac, complications, myocardial injury, perioperative period, postoperative outcomes, surgery, troponin
Editor's key points.
-
•
Myocardial injury is typically defined by troponin elevation, and the timing of the latter (preoperative, early or late postoperative) may have different clinical implications.
-
•
In this study, clinically asymptomatic increases in troponin within 24 h of elective major noncardiac surgery were common (25%), and associated with higher risk of many postoperative complications, including death.
-
•
Early elevated troponin within 24 h of surgery could be used to stratify levels of postoperative care in real time.
Asymptomatic myocardial injury, as detected by high-sensitivity troponin (hsTnT) assays, occurs commonly after noncardiac surgery.1, 2, 3 Higher mortality rates are associated with pre- and postoperative hsTnT values above the 99th centile values.4, 5, 6 An increase ≥25% from baseline high-sensitive cardiac troponin T (hsTnT) values was associated with a higher rate of noncardiac complications within 30 days of major abdominal surgery.2 However, an increase in hsTnT occurs in about 25% of younger adult patients without known cardiovascular disease after surgery, suggesting that elevated troponin levels constitute a normal physiological process for many surgical patients.7 Thus, the temporal relationship between troponin elevation and the development, and severity, of noncardiac morbidity remains unclear, particularly across different types of elective noncardiac surgery.
As part of a large international prospective observational cohort study of myocardial injury after noncardiac surgery,1 UK centres additionally collected data prospectively on noncardiac morbidity using the Postoperative Morbidity Survey (POMS)8 in addition to grading the severity of morbidity (Clavien–Dindo grade).9 In this study, we examined the temporal relationship between early elevated troponin within the first 24 h after noncardiac surgery and the development, and severity of, subsequent extra-cardiac morbidity.
Methods
Data sources and study population
This was a planned secondary analysis of perioperative outcomes in participants undergoing elective noncardiac surgery at four UK centres that took part in a prospective multicentre observational cohort study.1 The study was approved by the UK National Research Ethics Service Committee London (MREC:10/WNo03/25) and conducted in accordance with the principles of the Declaration of Helsinki. Participants provided written informed consent for the study before surgery.
Participants were aged 45 yr or older and underwent elective noncardiac surgery under general or regional anaesthesia and required at least one night in hospital after surgery. Participants were excluded if they refused consent or if they had previously enrolled in the Vascular Events In Noncardiac Surgery Patients Cohort Evaluation (VISION) study.1 Elective intensive care utilisation was at the discretion of attending clinicians.
Data collection
Researchers collected a detailed and standardised dataset from patients and their medical records, before and during the 30 days after surgery, including morbidity at 3 and 7 days after surgery using the POMS8 (which was devised at Duke University Medical Center and has been used internationally to capture patient-centred outcomes; Supplementary Table S1) and Clavien–Dindo graded complications within 30 days of surgery (Supplementary Table S2). Blood samples were taken before and within 24 h of surgery. At two centres, investigators, patients, and healthcare providers were blinded to troponin results throughout the study period.
Explanatory variable
Serum high-sensitivity cardiac troponin T concentration (hsTnT) ≥15 ng L−1 defined an early troponin elevation (Elecsys; Roche, Basel, Switzerland) 24 h after surgery. This cardiac hsTnT assay enables the detection of cTnT at the 99th centile of an apparently healthy reference population with <10% variability, with a 5 ng L−1 limit of detection.10 We considered both ischaemic vs non-ischaemic causes of hsTnT elevation, using values above the 99th centile which are linked to poorer clinical outcomes regardless of aetiology.2 Although UK patients in VISION had preoperative hsTnT values measured, as both pre- and postoperative values >99th centile are associated with poorer clinical outcomes,2 we focused on absolute levels within 24 h after surgery.
Primary outcome
The primary outcome was the presence of morbidity on postoperative day 3 defined by the POMS.8 The presence of morbidity was compared between patients with elevated troponin (elevated hsTnT ≥15 ng L−1) and troponin-negative patients within 24 h of surgery.
Secondary outcome measures
We also assessed the association between troponin increase within 24 h of surgery with: (1) severity of postoperative complications, as defined by Clavien–Dindo grade within 30 days after surgery across surgical categories; (2) time to become morbidity free across surgical categories; (3) intensive care-free days within 30 days after surgery across surgical categories. In each centre, an intensive care stay exceeding 2 days after surgery was defined as a prolonged (unplanned) period of intensive care resource use.
Statistical analyses
The statistical analysis was prospectively planned and published online before analyses were undertaken (https://www.ucl.ac.uk/anaesthesia/trials). We used NCSS 11 (NCSS LLC, Kaysville, UT, USA) and STATA version 14 (StataCorp LP, College Station, TX, USA) for analysis. We stratified the baseline characteristics of the cohort according to whether patients had a troponin increase >99th centile within 24 h of surgery. Binary data were expressed as percentages, normally distributed continuous data as mean with standard deviation (sd), and non-normally distributed continuous data as median (25–75th centiles). Multivariable logistic regression was undertaken using established conventional risk factors (age, gender, and the Revised Cardiac Risk Index [RCRI]). Unadjusted time to become morbidity-free was analysed using the log-rank test. We calculated hazard ratios (95% confidence interval [CI]) for early-troponin and troponin-negative groups' time to become morbidity-free stay using Cox regression analysis, which took into account the type and duration of surgery, and established conventional risk factors (age, gender, and the RCRI). A two-sided P-value of <0.05 was considered statistically significant.
We further examined whether there were any particular morbidity that correlated most strongly with early troponin elevation within 24 h of surgery by using an unbiased, unsupervised variable clustering model (ClustOfVar, version 1.1).11 Similarity was calculated as the square of the canonical correlation between two variables. A distance metric was calculated for patients using Gower's general similarity coefficient with Podani's extension for ordinal variables (CluMix, version 2.1). We used Ward's minimum-variance hierarchical clustering method, by using an agglomerative (bottom–up) approach and Ward's linkage.12 Analyses were performed using R (version 3.4.2, www.r-project.org).
Sensitivity analysis
The relationship between timing of troponin elevation and the development of morbidity at 3 days after surgery was also assessed between the two centres where staff had access to troponin results, compared with the two centres that were blinded to troponin data. We also compared between early elevated troponin (hsTnT ≥15 ng L−1) and troponin-negative patients within 24 h of surgery according to age group (<60, 60–75, >75 yr).
Sample size estimation
Approximately 25% of patients develop elevated troponin within 72 h after noncardiac surgery.1 At least 50% of UK patients undergoing similar surgery types to those included in this study sustain postoperative morbidity 72 h after noncardiac surgery, as defined by POMS.13, 14, 15 We therefore estimated that at least 1610 patients for each surgical category would be required to detect a clinically significant 10% absolute difference between early troponin-positive and -negative patients in the incidence of all-cause postoperative morbidity within 72 h after surgery between early troponin-positive and troponin-negative patients (α=0.01; 1–β=0.9).
Results
Patient characteristics
Morbidity outcome data in 4335 patients aged ≥45 yr who underwent elective noncardiac surgery (mean [sd] age, 65 [11] yr) were analysed, of whom 2385 (45.1%) were female; 1084 (25%) were designated as ASA class 3 or higher (Fig. 1). Overall, elevated troponin occurred within 24 h after surgery in 992/4335 (22.9%) patients (Table 1), with 8.5% of the entire cohort having a preoperative hsTnT >99th centile. The median (inter-quartile range [IQR]) hsTnT in patients with elevated troponin within 24 h after surgery was 21 (16–32) ng L−1, compared with patients in whom values did not breach the 99th centile hsTnT threshold, 7 (<3–10) ng L−1; P<0.001.
Fig 1.
Patient flow diagram showing cases included in the primary analysis. RLH- Royal London Hospital; UCLH- University College London Hospital.
Table 1.
Patient characteristics. Data presented as patients who had early elevated troponin-T within the first 24 h after surgery vs patients in whom troponin-T remained <99th centile. Data are shown as absolute median (IQR) values or n (%). Odds ratio (OR) with 95% confidence intervals (CIs) shown, where applicable. COPD, chronic obstructive pulmonary disease; IQR, inter-quartile range; RCRI, Revised Cardiac Risk Index.
| Troponin, ≥15 ng L−1 | Troponin, <15 ng L−1 | OR (95% CI) | |
|---|---|---|---|
| Age (y) | 69 (59–78) | 64 (55–72) | – |
| BMI (kg m−2) | 28.0 (6.1) | 28.9 (6.5) | – |
| Female sex, n (%) | 331 (33.4) | 1621 (48.5) | 0.69 (0.63–0.76) |
| RCRI ≥2, n (%) | 238 (24.0) | 296 (8.9) | 2.71(2.32–3.17) |
| ASA ≥3, n (%) | 546 (55.0) | 821 (24.6) | 3.76 (3.24–4.36) |
| Coronary artery disease, n (%) | 234 (23.6) | 293 (8.8) | 2.69 (2.30–3.15) |
| Cardiac failure, n (%) | 29 (2.9) | 29 (0.9) | 3.37 (2.02–5.61) |
| Diabetes mellitus, insulin treated, n (%) | 70 (7.1) | 105 (3.1) | 2.25 (1.67–3.02) |
| Diabetes mellitus, tablet treated, n (%) | 149 (15.0) | 333 (10.0) | 1.51 (1.26–1.81) |
| Cirrhosis, n (%) | 8 (0.8) | 18 (0.5) | 1.50 (0.65–3.43) |
| Stroke/transient ischaemic attack, n (%) | 86 (8.7) | 169 (5.1) | 1.72 (1.34–2.20) |
| Asthma, n (%) | 83 (8.4) | 345 (10.3) | 0.81 (0.65–1.02) |
| COPD, n (%) | 111 (11.2) | 191 (5.7) | 1.96 (1.57–2.45) |
| Metastases (preop), n (%) | 40 (4.0) | 120 (3.6) | 1.12 (0.79–1.60) |
| Systolic (mm Hg) | 141 (23) | 137 (21) | – |
| Diastolic (mm Hg) | 74 (12) | 75 (13) | – |
| Heart rate (beats min−1) | 76 (14) | 76 (13) | – |
| Haemoglobin (g L−1) | 126 (19) | 134 (17) | – |
| Intraoperative | |||
| Duration of surgery (min) | 140 (80–220) | 136 (90–205) | – |
| Crystalloid (ml kg h−1) | 9.4 (6.0–14.3) | 9.3 (6.3–13.5) | – |
| Fluid including colloid (ml kg h−1) | 10.2 (6.5–15.2) | 9.9 (6.8–14.3) | – |
| Estimated blood loss >500 ml, n (%) | 114 (11.5) | 279 (8.3) | – |
| Blood administered, n (%) | 83 (8.3) | 123 (3.7) | – |
| Postoperative | |||
| Planned critical care, n (%) | 314 (31.7) | 678 (20.3) | 1.56 (1.39–1.75) |
Primary outcome: troponin elevation and morbidity after surgery
Morbidity recorded 48–72 h after surgery was more frequent in 494/992 (49.8%) patients with early elevated troponin, compared with 1127/3343 (33.7%) patients with hsTnT <15 ng L−1 (OR=1.95; 95% CI, 1.69–2.25; P<0.0001; Table 2 and Supplementary Fig. S1).
Table 2.
Postoperative morbidity 72 h after surgery. Morbidity defined by Postoperative Morbidity Survey (POMS), compared between patients with early elevated troponin within the first 24 h after surgery vs patients in whom troponin remained ≤14 ng L−1. †Two of 25 patients with myocardial ischaemia and 5/25 with new arrhythmia received anticoagulation. Data are presented as n (%). All comparisons made by two-tailed Fisher's exact test. CI, confidence interval; OR, odds ratio.
| Troponin ≥15 ng L−1 | Troponin <15 ng L−1 | OR (95% CI) | P-value | |
|---|---|---|---|---|
| Any POMS morbidity | 494 (49.8) | 1127 (33.7) | 1.95 (1.69–2.25) | <0.0001 |
| Pulmonary | 109 (11.0) | 275 (8.2) | 1.38 (1.09–1.74) | <0.0001 |
| Supplemental oxygen | 107 (10.8) | 271 (8.1) | 1.37 (1.08–1.74) | |
| Ventilation | 12 (1.2) | 18 (0.5) | 2.26 (1.09–4.71) | |
| Infection | 133 (13.4) | 275 (8.2) | 1.68 (1.39–2.02) | <0.001 |
| Antibiotics | 196 (19.8) | 428 (12.8) | 1.73 (1.38–2.16) | |
| Fever | 38 (3.8) | 76 (2.3) | 1.71 (1.15–2.54) | |
| Renal | 312 (31.5) | 643 (19.2) | 1.93 (1.64–2.26) | <0.001 |
| Oliguria | 16 (1.6) | 9 (0.3) | 6.07 (2.68–13.79) | |
| Catheterisation | 307 (30.9) | 639 (19.2) | 1.90 (1.62–2.23) | |
| Gastrointestinal | 116 (11.7) | 361 (10.8) | 1.09 (0.88–1.37) | 0.43 |
| Nausea/vomiting | 79 (8.0) | 280 (8.4) | 0.95 (0.73–1.23) | |
| Intolerant of enteral feed | 71 (7.2) | 172 (5.1) | 1.42 (1.07–1.89) | |
| Cardiovascular | 87 (8.8) | 84 (2.5) | 3.73 (2.74–5.08) | <0.001 |
| Myocardial infarction | 26 (2.6) | 11 (0.3) | 8.15 (4.01–16.56) | |
| Myocardial ischaemia | 12 (1.2) | 7 (0.2) | 5.84 (2.29–14.86) | |
| Hypotension | 27 (2.7) | 26 (2.3) | 3.57 (2.07–6.15) | |
| Pulmonary oedema | 2 (0.2) | 1 (0.03) | 6.75 (0.61–74.5) | |
| Arrhythmia | 33 (3.3%) | 30 (0.9) | 3.80 (2.31–6.26) | |
| Anticoagulation† | 25 (2.5%) | 33 (1.0) | 2.59 (1.54–4.38) | |
| Neurological | 30 (3.0%) | 31 (0.9) | 3.33 (2.01–5.53) | <0.001 |
| Coma | 7 (0.7%) | 4 (0.12) | 5.93 (1.73–20.31) | |
| Delirium | 22 (2.2%) | 23 (0.69) | 2.87 (1.47–5.60) | |
| Stroke | 4 (0.4%) | 8 (0.24) | 2.41 (0.77–7.62) | |
| Wound | 12 (1.2%) | 69 (2.1) | 0.58 (0.31–1.08) | 0.08 |
| Dehiscence | 4 (0.4%) | 6 (0.18) | 2.25 (0.63–8.00) | |
| Pus | 10 (1.0%) | 66 (1.97) | 0.56 (0.26–0.99) | |
| Haematological | 45 (4.5%) | 67 (2.0) | 2,32 (1.58–3.41) | <0.001 |
| Packed red cells | 44 (4.4%) | 65 (1.9) | 2.34 (1.59–3.46) | |
| Products | 5 (0.5%) | 7 (0.2) | 2.41 (0.77–7.62) | |
| Pain | 29 (2.9%) | 70 (2.1) | 1.41 (0.91–2.18) | 0.15 |
| Regional analgesia | 37 (3.7%) | 121 (3.6) | 1.18 (0.93–1.51) | |
| Parental opioids | 96 (9.7%) | 278 (8.3) | 1.39 (0.88–2.19) | |
| Mobility | ||||
| Bedbound | 146 (14.7%) | 226 (6.8) | 2.38 (1.91–2.97) | <0.001 |
| Unaided | 491 (49.5%) | 2193 (65.6) |
Secondary outcomes
POMS-defined morbidity by postoperative day 7 was more frequent in 494/992 (49.8%) patients with early elevated troponin, compared with 1127/3343 (33.7%) patients with hsTnT <15 ng L−1 (OR=1.95; 95% CI, 1.69–2.25; P<0.0001; Supplementary Table S3). Accordingly, the time to become free of POMS-defined morbidity by postoperative day 7 was delayed in patients with early elevated troponin (hazard ratio [HR]=1.35; 95% CI, 1.26–1.45; P<0.0001; Fig. 2). Adjusting for surgery type, operative duration, age, gender, and RCRI, early elevated troponin remained an independent associate of morbidity developing within the first 7 days after surgery (Supplementary Table S5).
Fig 2.
Time to become morbidity free within 7 days of surgery, in relation to early troponin increase. Kaplan–Meier plot showing time to become morbidity-free, stratified by early elevated troponin and troponin remaining <15 ng L−1 status within 24 h of surgery. POMS-defined morbidity persisted for at least 7 days early elevated troponin (HR=1.35; 95% CI, 1.26–1.45; P<0.0001). Coloured numbers at risk for each category are matched to coloured lines shown in graph panel. CI, confidence interval; HR, hazard ratio; hsTnT, high-sensitivity troponin; POMS, Postoperative Morbidity Survey.
Severity of complications and duration of hospitalisation
Patients with early elevated troponin were more likely to die (35/992 [3.5%] vs 62/3343 [1.9%]) compared with patients who had a hsTnT <15 ng L−1 (OR=1.94; 95% CI, 1.27–2.95; P<0.0001). Patients with early elevated troponin sustained serious complications (Clavien–Dindo ≥grade 3) more frequently (167/992 [16.8%]) than 319/3343 (9.5%) patients with hsTnT <15 ng L−1 (OR=1.92; 95% CI, 1.57–2.35; P<0.0001) within 30 days after surgery (Supplementary Fig. S2). Adjusting for surgery type, age, gender, and RCRI, prolonged hospitalisation occurred in patients who sustained early elevated troponin (HR=1.35; 95% CI, 1.26–1.45; P<0.0001; Supplementary Fig. S3).
Intensive care utilisation
Overall, 314/992 (32.7%) patients with early elevated troponin were electively admitted to critical care wards after surgery, in comparison with 678/3343 (20.3%) of patients with hsTnT <15 ng L−1 (OR=1.82; 95% CI, 1.55–2.13; P<0.0001). Moreover, 153/992 patients with early elevated troponin were more likely to require prolonged intensive care support after 2 days initial care (or subsequent unplanned readmission >72 h after surgery), compared with 235/3343 patients with hsTnT <15 ng L−1 (OR=2.05; 95% CI, 1.73–2.43; P<0.0001). Death occurred within 30 days after surgery more frequently in 35/992 (3.5%) patients with early elevated troponin, compared with 62/3343 (1.9%) troponin-negative patients (OR=1.94; 95% CI, 1.27–2.95; P<0.0001). Patients with early elevated troponin experienced fewer postoperative days free of intensive care (HR=1.15; 95% CI, 1.07–1.24; P<0.0001; Fig. 3) and delayed discharge from hospital regardless of whether they received scheduled critical care immediately after surgery (Supplementary Fig. S4).
Fig 3.
Critical care-free days. The risk of requiring intensive care was greater in patients with early elevated troponin 24 h after surgery (≥15 ng L−1; early troponin), who experienced fewer postoperative days free of critical care (HR=1.15; 95% CI, 1.07–1.24; P<0.0001, by log-rank test). CI, confidence interval; HR, hazard ratio.
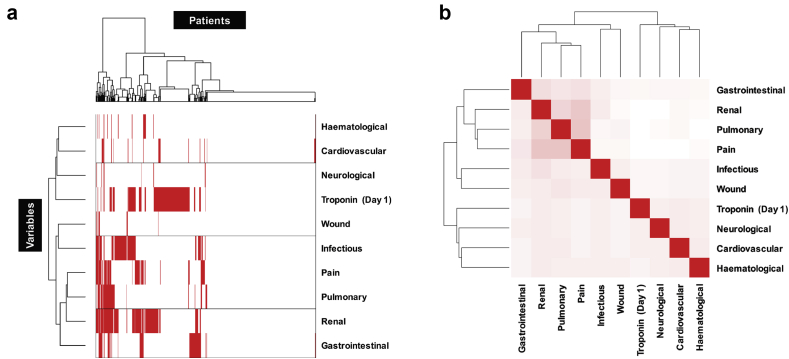
Hierarchical variable clustering analysis
Early elevated troponin was not associated with any specific extra-cardiac morbidity, but rather preceded a broad range of multi-organ morbidities (Fig. 4). In the absence of hsTnT (2025/2623 [77.2%] patients), noncardiac morbidity was less frequent (OR=0.44; 95% CI, 0.39–0.51; P<0.0001).
Fig 4.
Unsupervised variable clustering analysis. (a) Hierarchical clustering for all patients, using Postoperative Morbidity Survey (POMS) domains scored on day 3 and troponin on day 1 dichotomised as early elevated troponin (≥15 ng L−1) or within normal limits (<15 ng L−1). The dendogram illustrates how various morbidities cluster in different groups of patients. (b) Variable similarity for POMS domains recorded on day 3 and troponin measured on day 1, dichotomised as early elevated troponin (≥15 ng L−1) or within normal limits (<15 ng L−1). Bright red shaded boxes indicate 100% association (i.e. correlation between same variable); lighter shading indicates weaker association.
Sensitivity analyses
Blinding clinicians to troponin results had no effect on the qualitative observation that patients with early elevated troponin sustained more frequent morbidity (masked centres: OR=1.89; 95% CI, 1.58–2.26; unmasked centres: OR=2.47; 95% CI, 1.93–3.18) and utilised intensive care more often (masked centres: OR=2.11; 95% CI, 1.71–2.60; unmasked centres: OR=2.07; 95% CI, 1.53–2.79; Supplementary Fig. S4). Even earlier elevated troponin within 6–12 h after surgery was also associated with more all-cause morbidity in the next 72 h after surgery (Supplementary Table S5). Controlling for age, the association between elevated troponin within the first 6–12 h and POMS-defined morbidity remained consistent (Supplementary Fig. S6).
Discussion
The principal finding of this prospective observational cohort study is that clinically asymptomatic increases in troponin within 24 h of elective surgery occur commonly in a quarter of patients undergoing elective major noncardiac surgery and are strongly associated with increased risk of noncardiac complications and utilisation of intensive care resources.
Understanding the evolution of postoperative morbidity has been hampered by the lack of prospective, serial morbidity data collection combined with large-scale use of highly sensitive biomarkers for cellular injury. Our analysis provides insight into the temporal relationship between troponin elevation and subsequent morbidity (including severity of complications), which may shed light on shared mechanisms of both cardiovascular and extra-cardiovascular pathology after surgery. Our findings mirror those of single-centre studies where myocardial injury was associated with higher 1-yr all-cause mortality, independent of preoperative troponin values, in similar proportions (∼22%) as we report here.16 Similarly, mortality has been reported to be higher in patients with pre-existing preoperative high-sensitivity cardiac troponin T (hs-cTnT) elevations >99th percentile.2 Our data are also consistent with findings reported by a planned sub-analysis of the Evaluation of Nitrous Oxide in the Gas Mixture for Anaesthesia (ENGIMA)-II RCT, in which patients who sustained adverse noncardiac morbidity accompanied by troponin increase not attributable to myocardial infarction had the highest risk of death.17
These data generate several implications for both further research and clinical practice. Firstly, the data suggest that troponin may be useful for stratifying postoperative care dynamically in real time, rather than using only modestly predictive preoperative assessment tools18,19 for assessing the risk of morbidity after surgery. Our data support the contention that troponin monitoring potentially offers an objective, real-time assessment tool to facilitate rationalise postoperative care across several surgical subspecialties.20 The allocation of intensive care resources after noncardiac surgery is a daily clinical challenge internationally, with wide inter-hospital and -clinician variation in practice reflecting a lack of evidence and guidelines on this topic.21, 22, 23 In the absence of generalisable data, local organisational and cultural factors appear to determine whether patients receive postoperative intensive care.23 Given the volume of surgery internationally, the use of objective biomarkers such as troponin measurement may provide an alternative objective approach. The association between early troponin elevation and morbidity developed after planned postoperative ICU care immediately after surgery. These observations suggest that troponin increase does not merely occur after major surgery, in patients with comorbidity, or both that persuades clinicians that require critical care is required immediately after surgery.
Second, beyond an established link with mortality,1 we have now demonstrated that patients with early elevated troponin sustain substantially more all-cause morbidity in the next 72 h after surgery. Our prospective data extend previous findings where postoperative increases in cardiac troponin T by more than 100% from preoperative baseline values were associated with noncardiac complications and prolonged hospitalisation within 30 days in ∼200 patients after abdominal surgery.24 Given the temporal relationship our prospective data collection has revealed, early troponin monitoring may have utility beyond raising clinical vigilance for cardiovascular morbidity and mortality. Third, our data reinforce the need to understand mechanisms underlying postoperative morbidity which, given the patterns revealed, suggest a shared aetiology between the dysfunction evident across organs/systems. For example, early troponin elevation was associated with a substantial excess of infectious complications several days after early troponin elevation was detected. Fourth, the use of troponin monitoring may help refine clinical and mechanistic research through an adaptive study design approach.
The patterns of postoperative morbidity detected in relation to early troponin increase are compatible with several proposed mechanisms that may underpin poorer outcomes even after discharge after noncardiac surgery. Persistent prolonged immobility was more common in patients with elevated troponin within 24 h after surgery, which may promote morbidity. In keeping with cardiomyocyte injury, arrhythmias were persistently more common in patients with early elevated troponin for up to 1 week after surgery. Similarly, new full-dose anticoagulation was also more common in patients with early troponin increases, suggesting that early cardiomyocyte injury may reflect a pro-thrombotic state that is triggered early in the perioperative period (although a small minority had overt myocardial ischaemia treated with anticoagulation).25
Recruiting more than 4300 patients is a significant strength of this prospective work, which comprises a 20-fold larger study size compared with preceding work examining the link between troponin and noncardiac morbidity after noncardiac surgery. In contrast to the myocardial infarction literature, where age-related thresholds for troponin appear to be important,26,27 our data are in keeping with perioperative findings suggesting that even small increments from baseline (preoperative) troponin are prognostically relevant1 and associated with excess all-cause perioperative morbidity.2 The study captured several features of contemporary practice, including enhanced recovery based analgesic regimens and fluid therapy, which indicate broadly similar perioperative management and enhanced recovery practices across centres. Moreover, our agnostic hierarchical cluster analysis reveals a clear relationship between the absence of elevated troponin within 24 h of surgery and rapid, morbidity-free recovery.
The observational design of this study is a limitation, as causality cannot be inferred from the association between various postoperative morbidity and early troponin elevation. POMS largely uses clinical criteria which do not reflect the severity of postoperative morbidity. However, the parallel use of Clavien–Dindo grading addresses this drawback. Some features of POMS merely reflect processes of care rather than morbidity alone, although morbidity after surgery typically clusters. Many POMS domains when positive are inter-related, so it is possible that the burden of morbidity is over-estimated for some patients.
In summary, troponin elevation within 24 h of elective noncardiac surgery is associated with the development of persistent noncardiac organ dysfunction. Detecting elevated troponin early after noncardiac surgery in real time may help stratify the level of surveillance required for higher-risk surgical patients, the intensity of postoperative care, or both.
Authors' contributions
Study hypothesis: GLA
Design of analysis plan: GLA
Data analysis (independently): GLA, TEFA
Cluster analysis: TFJ
Drafting of the manuscript: GLA, TEFA, RMP
All authors were involved in the critical review of the manuscript
Declarations of interest
GLA is a member of the editorial advisory board for Intensive Care Medicine Experimental, editor for British Journal of Anaesthesia, and has undertaken consultancy work for GlaxoSmithKline; RMP holds research grants, and has given lectures, and/or performed consultancy work for BBraun, GlaxoSmithKline, Intersurgical and Edwards Lifesciences, and is a member of the Associate editorial board of the British Journal of Anaesthesia and BMJ Quality & Safety. The other authors declare that they have no conflicts of interest.
Funding
Medical Research Council and British Journal of Anaesthesia clinical research training fellowship (grant reference MR/M017974/1; TEFA); UK National Institute for Health Research Professorship (RMP); British Journal of Anaesthesia/Royal College of Anaesthetists basic science Career Development award, British Oxygen Company research chair grant in anaesthesia from the Royal College of Anaesthetists and British Heart Foundation Programme Grant (RG/14/4/30736; GLA).
Handling editor: Paul Myles
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bja.2020.02.003.
Contributor Information
Gareth L. Ackland, Email: g.ackland@qmul.ac.uk.
for the VISION-UK Investigators:
Rupert Pearse, Edyta Niebrzegowska, Andrew Wragg, Andrew Archbold, Elisa Kam, Kirsty Everingham, Phoebe Bodger, Thais Creary, Ben Bloom, Alice Carter, Neil MacDonald, Tom E.F. Abbott, Nirav Shah, Katarzyna Mrozek, Amy Richardson, Alex Fowler, and Zakaria Rob
University College Hospital:
Gareth Ackland, Robert Stephens, Anna Reyes, Laura Gallego Paredes, Pervez Sultan, David Cain, John Whittle, Mark Edwards, Simon Woldman, Ana Gutierrez del Arroyo, and Shamir Karmali
Royal Liverpool University Hospital:
Colin Williams, A. Rushton, I. Welters, Martin Leuwer, and Jane Parker
Leeds Teaching Hospitals:
Robert J. Sapsford, Julian Barth, Julian Scott, Alistair Hall, Simon Howell, Michaela Lobley, Janet Woods, Susannah Howard, Joanne Fletcher, and Nikki Dewhirst
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Writing Committee for the VSI, Devereaux P.J., Biccard B.M. Association of postoperative high-sensitivity troponin levels with myocardial injury and 30-day mortality among patients undergoing noncardiac surgery. JAMA. 2017;317:1642–1651. doi: 10.1001/jama.2017.4360. [DOI] [PubMed] [Google Scholar]
- 2.Puelacher C., Lurati Buse G., Seeberger D. Perioperative myocardial injury after noncardiac surgery: incidence, mortality, and characterization. Circulation. 2018;137:1221–1232. doi: 10.1161/CIRCULATIONAHA.117.030114. [DOI] [PubMed] [Google Scholar]
- 3.Gillies M.A., Shah A.S., Mullenheim J. Perioperative myocardial injury in patients receiving cardiac output-guided haemodynamic therapy: a substudy of the OPTIMISE trial. Br J Anaesth. 2015;115:227–233. doi: 10.1093/bja/aev137. [DOI] [PubMed] [Google Scholar]
- 4.Nagele P. Elevated cardiac troponin before surgery: perhaps not so benign. Br J Anaesth. 2020;124:6–7. doi: 10.1016/j.bja.2019.10.001. [DOI] [PubMed] [Google Scholar]
- 5.Liem V.G.B., Hoeks S.E., Grune F. Prognostic value of postoperative high-sensitivity troponin T in patients with different stages of kidney disease undergoing noncardiac surgery. Br J Anaesth. 2018;120:84–93. doi: 10.1016/j.bja.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 6.Ekeloef S., Alamili M., Devereaux P.J., Gogenur I. Troponin elevations after non-cardiac, non-vascular surgery are predictive of major adverse cardiac events and mortality: a systematic review and meta-analysis. Br J Anaesth. 2016;117:559–568. doi: 10.1093/bja/aew321. [DOI] [PubMed] [Google Scholar]
- 7.Duma A., Wagner C., Titz M. High-sensitivity cardiac troponin T in young, healthy adults undergoing non-cardiac surgery. Br J Anaesth. 2018;120:291–298. doi: 10.1016/j.bja.2017.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bennett-Guerrero E., Welsby I., Dunn T.J. The use of a postoperative morbidity survey to evaluate patients with prolonged hospitalization after routine, moderate-risk, elective surgery. Anesth Analg. 1999;89:514–519. doi: 10.1097/00000539-199908000-00050. [DOI] [PubMed] [Google Scholar]
- 9.Clavien P.A., Strasberg S.M. Severity grading of surgical complications. Ann Surg. 2009;250:197–198. doi: 10.1097/SLA.0b013e3181b6dcab. [DOI] [PubMed] [Google Scholar]
- 10.Giannitsis E., Kurz K., Hallermayer K., Jarausch J., Jaffe A.S., Katus H.A. Analytical validation of a high-sensitivity cardiac troponin T assay. Clin Chem. 2010;56:254–261. doi: 10.1373/clinchem.2009.132654. [DOI] [PubMed] [Google Scholar]
- 11.Chavent M., Kuentz V., Liquet B., Saracco L. ArXiv; 2011. ClustOfVar: an R package for the clustering of variables. arXiv: 1112.0295. [Google Scholar]
- 12.Everitt B., Landau S., Leese M. Oxford University Press; New York: 2001. Cluster Analysis. [Google Scholar]
- 13.Karmali S., Jenkins N., Sciusco A. Randomized controlled trial of vagal modulation by sham feeding in elective non-gastrointestinal (orthopaedic) surgery. Br J Anaesth. 2015;115:727–735. doi: 10.1093/bja/aev283. [DOI] [PubMed] [Google Scholar]
- 14.Ackland G.L., Moran N., Cone S., Grocott M.P.W., Mythen M.G. Chronic kidney disease and postoperative morbidity after elective orthopedic surgery. Anesth Analg. 2011;112:1375–1381. doi: 10.1213/ANE.0b013e3181ee8456. [DOI] [PubMed] [Google Scholar]
- 15.Ackland G.L., Iqbal S., Paredes L.G. Individualised oxygen delivery targeted haemodynamic therapy in high-risk surgical patients: a multicentre, randomised, double-blind, controlled, mechanistic trial. Lancet Respir Med. 2015;3:33–41. doi: 10.1016/S2213-2600(14)70205-X. [DOI] [PubMed] [Google Scholar]
- 16.van Waes J.A., Grobben R.B., Nathoe H.M. One-year mortality, causes of death, and cardiac interventions in patients with postoperative myocardial injury. Anesth Analg. 2016;123:29–37. doi: 10.1213/ANE.0000000000001313. [DOI] [PubMed] [Google Scholar]
- 17.Beattie W.S., Wijeysundera D.N., Chan M.T.V. Implication of major adverse postoperative events and myocardial injury on disability and survival: a planned subanalysis of the ENIGMA-II trial. Anesth Analg. 2018;127:1118–1126. doi: 10.1213/ANE.0000000000003310. [DOI] [PubMed] [Google Scholar]
- 18.Ackland G.L., Harris S., Ziabari Y., Grocott M., Mythen M., Investigators S.O. Revised cardiac risk index and postoperative morbidity after elective orthopaedic surgery: a prospective cohort study. Br J Anaesth. 2010;105:744–752. doi: 10.1093/bja/aeq245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wong D.J.N., Oliver C.M., Moonesinghe S.R. Predicting postoperative morbidity in adult elective surgical patients using the Surgical Outcome Risk Tool (SORT) Br J Anaesth. 2017;119:95–105. doi: 10.1093/bja/aex117. [DOI] [PubMed] [Google Scholar]
- 20.Polok K., Fronczek J., Szczeklik W. Myocardial infarction after vascular surgery: a systematic troponin surveillance and a uniform definition is needed. JAMA Surg. 2018;153:496. doi: 10.1001/jamasurg.2017.6143. [DOI] [PubMed] [Google Scholar]
- 21.Kahan B.C., Koulenti D., Arvaniti K. Critical care admission following elective surgery was not associated with survival benefit: prospective analysis of data from 27 countries. Intensive Care Med. 2017;43:971–979. doi: 10.1007/s00134-016-4633-8. [DOI] [PubMed] [Google Scholar]
- 22.Wunsch H., Gershengorn H.B., Cooke C.R. Use of intensive care services for Medicare beneficiaries undergoing major surgical procedures. Anesthesiology. 2016;124:899–907. doi: 10.1097/ALN.0000000000001024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ghaffar S., Pearse R.M., Gillies M.A. ICU admission after surgery: who benefits? Curr Opin Crit Care. 2017;23:424–429. doi: 10.1097/MCC.0000000000000448. [DOI] [PubMed] [Google Scholar]
- 24.Noordzij P.G., van Geffen O., Dijkstra I.M. High-sensitive cardiac troponin T measurements in prediction of non-cardiac complications after major abdominal surgery. Br J Anaesth. 2015;114:909–918. doi: 10.1093/bja/aev027. [DOI] [PubMed] [Google Scholar]
- 25.Gorka J., Polok K., Iwaniec T. Altered preoperative coagulation and fibrinolysis are associated with myocardial injury after non-cardiac surgery. Br J Anaesth. 2017;118:713–719. doi: 10.1093/bja/aex081. [DOI] [PubMed] [Google Scholar]
- 26.Welsh P., Preiss D., Shah A.S.V. Comparison between high-sensitivity cardiac troponin T and cardiac troponin I in a large general population cohort. Clin Chem. 2018;64:1607–1616. doi: 10.1373/clinchem.2018.292086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shah A.S.V., Anand A., Strachan F.E. High-sensitivity troponin in the evaluation of patients with suspected acute coronary syndrome: a stepped-wedge, cluster-randomised controlled trial. Lancet. 2018;392:919–928. doi: 10.1016/S0140-6736(18)31923-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.