Abstract
Context:
The prescription of opioids after elective surgical procedures has been a contributing factor to the current opioid epidemic in North America.
Objective:
To examine the opioid prescribing practices and rates of opioid consumption among patients undergoing common sports medicine procedures.
Data Sources:
A systematic review of the electronic databases EMBASE, MEDLINE, and PubMed was performed from database inception to December 2018.
Study Selection:
Two investigators independently identified all studies reporting on postoperative opioid prescribing practices and consumption after arthroscopic shoulder, knee, or hip surgery. A total of 119 studies were reviewed, with 8 meeting eligibility criteria.
Study Design:
Systematic review.
Level of Evidence:
Level 4.
Data Extraction:
The quantity of opioids prescribed and used were converted to milligram morphine equivalents (MMEs) for standardized reporting. The quality of each eligible study was evaluated using the Methodological Index for Non-Randomized Studies.
Results:
A total of 8 studies including 816 patients with a mean age of 43.8 years were eligible for inclusion. A mean of 610, 197, and 613 MMEs were prescribed to patients after arthroscopic procedures of the shoulder, knee, and hip, respectively. At final follow-up, 31%, 34%, and 64% of the prescribed opioids provided after shoulder, knee, and hip arthroscopy, respectively, still remained. The majority of patients (64%) were unaware of the appropriate disposal methods for surplus medication. Patients undergoing arthroscopic rotator cuff repair had the highest opioid consumption (471 MMEs), with 1 in 4 patients receiving a refill.
Conclusion:
Opioids are being overprescribed for arthroscopic procedures of the shoulder, knee, and hip, with more than one-third of prescribed opioids remaining postoperatively. The majority of patients are unaware of the appropriate disposal techniques for surplus opioids. Appropriate risk stratification tools and evidence-based recommendations regarding pain management strategies after arthroscopic procedures are needed to help curb the growing opioid crisis.
Keywords: arthroscopy, narcotics, pain management, analgesia
The United States is currently experiencing an opioid epidemic characterized by an increasing death toll due to opioid misuse and overdose.39,52 This epidemic has been aggravated by the excessive prescription of opioids for chronic or postoperative pain management by health care providers.38 Currently, orthopaedic surgeons account for approximately 7.7% of prescribed opioids in the United States and are the third-leading prescribers among all specialties.5,45 In an attempt to curb the opioid epidemic, the American Academy of Orthopedic Surgeons has advocated for evidence-based prescription guidelines that take into account specific risk factors that may lead to abuse or misuse of opioids postoperatively.45 As a result, prescription and consumption trends have been closely evaluated within orthopaedics and have been recorded for a variety of common procedures, including total knee, shoulder, and hip arthroplasties.2,6,19,21,24,30,56
There are approximately 2 million arthroscopic knee surgeries performed annually in the United States.55 Despite their prevalence, postoperative opioid usage after arthroscopic procedures of the knee, hip, and shoulder have not been investigated in great detail. The volume of arthroscopic procedures performed in the United States has been increasing rapidly and contributes to a significant portion of common orthopaedic procedures.17 Most notably, hip arthroscopy has risen markedly, with as high as a 25-fold increase within the past decade.4,8,10,33,57 Arthroscopic procedures of the shoulder have also become more prevalent. In fact, the incidence of arthroscopic rotator cuff repair (RCR) has increased by as much as 600% in recent years.7,15,28,29,51 Knee arthroscopy and related procedures such as anterior cruciate ligament reconstruction (ACLR), meniscal repair, and partial meniscectomy have also continued to grow in volume.22,23,25,32,36,40,50,60
Despite the growing use of knee, shoulder, and hip arthroscopy, there is a paucity of information regarding postoperative opioid prescribing patterns and use after arthroscopic procedures. This systematic review aims to examine and summarize the trends in prescribing practices and postoperative opioid consumption among patients undergoing sports medicine procedures. As a secondary objective, this review also intends to determine the existing patient awareness surrounding appropriate opioid disposal practices.
Methods
We conducted a systematic review in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.43
Search Strategy
Two investigators independently performed a systematic search of the electronic databases MEDLINE, EMBASE, and PubMed. A keyword search was performed, which included a combination of the following medical subject headings: arthroscopy, sports medicine, opioids, and related synonyms (eg, opiates). Additional studies were discovered by searching the reference lists of eligible studies. The search was performed from database inception to the second week of December 2018.
Eligibility Criteria
Studies were eligible for inclusion if they examined (1) patients undergoing arthroscopic shoulder, hip, or knee arthroscopy and related procedures (eg, ACLR, tibial tubercle osteotomy [TTO]); (2) described postoperative opioid prescribing patterns; and/or (3) evaluated opioid consumption rates. Articles were excluded if there were less than 10 study participants or they did not report patient-specific data.
Study Selection and Data Extraction
Two independent reviewers screened the titles and abstracts from our initial search and extracted relevant data from all eligible studies into a standardized collection form using spreadsheet software. Data collected included general study information (eg, author, year of publication, level of evidence), study population data (eg, sample size, mean age, patient sex), and outcome measures used (eg, morphine milligram equivalent [MME] prescribed, MME used, MME left over, prescription duration, refill rate).
Assessment of Risk of Bias in Eligible Studies
The overall quality of each eligible study was evaluated with the Methodological Index for Non-Randomized Studies (MINORS).58 The MINORS criteria is a validated tool used to assess the methodological quality of nonrandomized studies, including those that are comparative and noncomparative. Each of the 12 items included in the MINORS criteria is given a score of 0, 1, or 2, resulting in a maximum score of 16 and 24 for noncomparative and comparative studies, respectively.58
Statistical Analysis
Descriptive statistics were calculated with continuous data presented as weighted means with corresponding standard deviations and categorical data as frequencies with percentages. Quantity of opioids prescribed, used, and left over were converted to MMEs for standardized reporting using an accepted conversion table from the Centers for Medicare & Medicaid Services.46 For studies that did not report the mean or standard deviation, the median and interquartile range were used to impute these values using a well-established statistical technique described by Hozo et al.26
Results
Literature Search
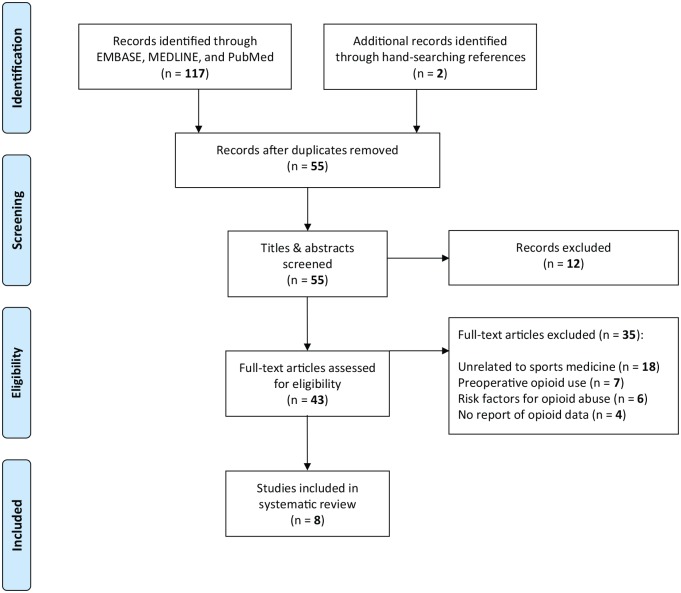
Our electronic literature search generated 119 studies for review. After removing duplicates, 55 studies were screened according to their titles and abstracts. Eight studies9,16,34,48,53,54,62,67 were deemed eligible for inclusion after full-text review (Figure 1).
Figure 1.
Flow diagram summarizing the literature search, screening, and selection process using PRISMA (Preferred Reporting Items for Systematic Meta-Analyses) guidelines.
Study Characteristics
A total of 8 studies including 816 patients with a mean age of 43.8 years were eligible for inclusion. Detailed characteristics of each study are displayed in Table 1. Three studies16,34,53 examined opioid-prescribing habits and use among patients undergoing arthroscopic shoulder procedures, including RCR,16,34,53 Bankart repair,34 superior labrum anterior to posterior repair,34 and distal clavicle resection/subacromial decompression.34 There were 4 studies16,48,62,67 that evaluated opioid-prescribing practices and consumption after arthroscopic procedures of the knee, including meniscal surgery (repair or partial meniscectomy),16,48,62,67 ACLR,48,62 TTO,48,62 and medial patellofemoral ligament (MPFL) reconstruction.48,62 Two studies reported on opioid use after hip arthroscopy.9,54 Among the 8 eligible studies, opioid-prescribing patterns,9,16,34,48,53,54,62,67 opioid consumption,9,16,53,54,62,67 refill rates,9,34,48,53,54,62,67 and opioid disposal education were evaluated.16,34,53,54,62
Table 1.
General characteristics of eligible studies
| First Author (Year) | LOE | Sample Size, N | Male: Female | Age, y, Mean (SD) | Procedure, n | MME Prescribed, Mean (SD) | MME Used, Mean (SD) | MME Leftover, % | Refill Rate, n/Total (%) | Aware of Methods for Disposal of Opioids, % | Nonopioid Sources of Pain Management |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cunningham (2018)9 | 4 | 73 | 18:55 | 36.5 (11.3) | Hip arthroscopy + labral repair (72)/acetabuloplasty (73)/femoroplasty (68)/microfracture (3) | 618 (316) | 251 (60.9) | 59 | 11/73 (15) | NR | Perioperative: • ± Peripheral nerve block Postoperative: • Acetaminophen • Naproxen • ± Gabapentin/pregabalin • ± Meloxicam/indomethacin |
| Fujii (2018)16 | 4 | 53 | NR | NR | Shoulder arthroscopy + RCR (23) | 425 (124.5) | 192 (131.3) | 55 | NR | 18 | Perioperative: • NR |
| Knee arthroscopy + meniscal surgery (30) | 190 (112.5) | 156 (112.5) | 18 | Postoperative: • Acetaminophen • Naproxen |
|||||||
| Kumar (2017)34 | 4 | 100 | 74:26 | 48 (14) | Shoulder arthroscopy + RCR (50)/SLAP repair (19)/Bankart repair (11)/DCR ± SAD (20) | 531 (380) | 339 (NR) | 36 | 11/100 (14) | 25 | Perioperative: • Peripheral nerve block Postoperative: • Acetaminophen |
| O’Neill (2014)48 | 4 | 100 | 41:59 | 42 (9.7) | Knee arthroscopy + meniscal surgery (63) + ACLR (25)/TTO (4)/patellar tendon debridement (2)/ROH (2)/other (4) | 50 (0) | NR | NR | 40/100 (40) | NR | Perioperative: • Spinal anesthesia Postoperative: • Acetaminophen |
| Sabatino (2018)53 | 4 | 146 | 100:46 | 60.6 (9.7) | Shoulder arthroscopy + RCR (146) | 778 (447) | 599 (666) | 23 | 47/146 (32) | 44 | Perioperative: • NR Postoperative: • NR |
| Selley (2018)54 | 4 | 23 | 7:16 | 42 (15) | Hip arthroscopy + labral repair + acetabuloplasty ± femoroplasty (23) | 600 (0) | 134 (174) | 78 | 0/23 (0) | 35 | Perioperative: • Intra-articular injection (morphine) • Acetaminophen/Celebrex Postoperative: • Acetaminophen • Naproxen |
| Tepolt (2018)62 | 4 | 100 | 44:56 | 17.5 (3.5) | Knee arthroscopy + ACLR (47)/TTO (6)/MPFLR (7)/meniscal surgery (18)/other (22) | 382 (93.8) | 124 (100.5) | 68 | 1/100 (1) | 52 | Perioperative: • Peripheral nerve block (femoral or sciatic) • Acetaminophen/Ketorolac Postoperative: • Acetaminophen • Naproxen • Diazepam |
| Wojahn (2018)67 | 4 | 221 | 114:107 | 46.2 (10.3) | Knee arthroscopy + meniscal repair (13)/partial meniscectomy (170)/chondroplasty (19)/debridement (5)/loose body removal (14) | 181 (200) | 130 (156.7) | 28 | 13/221 (6) | NR | Perioperative: • Peripheral nerve block (1.4%) • Intra-articular injection (56%) • Portal site injection (44%) Postoperative: • NSAID (60%) |
ACLR, anterior cruciate ligament reconstruction; DCR, distal clavicle resection; LOE, level of evidence; MME, milligram morphine equivalents; MPFLR, medial patellofemoral ligament reconstruction; NR, not reported; NSAID, nonsteroidal anti-inflammatory drug; RCR, rotator cuff repair; ROH, removal of hardware; SAD, subacromial decompression; SLAP, superior labrum anterior to posterior; TTO, tibial tubercle osteotomy.
Opioid Prescribing Practices
Among the 3 studies16,34,53 (195 patients) that evaluated opioid-prescribing practices after arthroscopic shoulder procedures, a mean of 610 MMEs were prescribed. Four studies16,48,62,67 (451 patients) examined the amount of opioids provided after knee arthroscopy, with a mean of 197 MMEs prescribed postoperatively. Patients who underwent hip arthroscopy (2 studies9,54; 96 patients) were prescribed a mean of 613 MMEs. See Table 2 for a complete comparison of standard opioid formulations prescribed after shoulder, knee, and hip arthroscopy.
Table 2.
Comparison of standard opioid formulations prescribed after arthroscopic procedures of the shoulder, knee, and hip
| Shoulder Arthroscopy | Knee Arthroscopy | Hip Arthroscopy | |
|---|---|---|---|
| Mean MME prescribed | 610 | 197 | 613 |
| Oral codeine—30-mg tablets, n | 136 | 44 | 136 |
| Oral hydrocodone—5-mg tablets, n | 122 | 40 | 123 |
| Oral oxycodone—5-mg tablets, n | 81 | 26 | 82 |
| Oral hydromorphone—2-mg tablets, n | 76 | 25 | 77 |
MME, milligram morphine equivalent.
Postoperative Opioid Consumption
Across all arthroscopic shoulder procedures (3 studies16,34,53; 195 patients), a mean of 418 MMEs were consumed postoperatively, leaving 31% of prescribed opioids unused. Similarly, a mean of 131 MMEs were used after knee arthroscopy and related procedures (3 studies16,62,67; 351 patients), leaving 34% of the prescribed opioid. Last, patients who underwent hip arthroscopy (2 studies9,54; 96 patients) consumed an average of 223 MMEs, resulting in 64% of the prescribed opiods remaining. A comparison of mean opioid consumption after common arthroscopic procedures of the shoulder, knee, and hip is illustrated in Table 3.
Table 3.
Comparison of mean opioid consumption after common arthroscopic procedures of the shoulder, knee, and hip
| Shoulder Arthroscopy |
Knee Arthroscopy |
Hip Arthroscopy |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| RCR | SLAP Repair | Bankart Repair | DCR/SAD | ACLR | Meniscal Surgery | TTO | MPFLR | Labral Repair + Acetabuloplasty ± Femoroplasty ± Microfracture | |
| Sample size | 145 | 19 | 11 | 20 | 47 | 294 | 6 | 7 | 96 |
| Mean MME used | 471 | 344 | 175 | 238 | 155 | 126 | 128 | 138 | 223 |
| Oral codeine—30-mg tablets, n | 105 | 76 | 39 | 53 | 34 | 28 | 28 | 31 | 50 |
| Oral hydrocodone—5-mg tablets, n | 94 | 69 | 35 | 48 | 31 | 25 | 26 | 28 | 45 |
| Oral oxycodone—5-mg tablets, n | 63 | 46 | 23 | 32 | 21 | 17 | 17 | 18 | 30 |
| Oral hydromorphone—2-mg tablets, n | 59 | 43 | 22 | 30 | 19 | 16 | 16 | 17 | 28 |
ACLR, anterior cruciate ligament reconstruction; DCR, distal clavicle resection; MME, milligram morphine equivalent; MPFLR, medial patellofemoral ligament reconstruction; RCR, rotator cuff repair; SAD, subacromial decompression; SLAP, superior labrum anterior to posterior; TTO, tibial tubercle osteotomy.
Duration of Opioid Use
Three studies54,62,67 reported on duration of opioid use postoperatively after arthroscopic procedures of the hip54 and knee.62,67 All studies reported that more than half of patients discontinued opioid use within 3 days of surgery. Tepolt et al62 found that approximately 70% of patients ceased to take opioids 3 days after knee arthroscopy and related procedures such as ACLR, TTO, and MPFL reconstruction.
Opioid Disposal
Five studies16,34,53,54,62 reported whether patients received instructions regarding opioid disposal or had prior knowledge of appropriate disposal methods. Of the 348 patients evaluated, only 36% of patients had received preoperative instruction or were aware of the proper means by which to dispose of leftover opioids.
Refill Rate
Among patients undergoing arthroscopic shoulder procedures (2 studies34,53; 227 patients), 26% requested at least 1 refill of their opioid prescription, while 13% and 12% received a refill after knee (3 studies48,62,67; 421 patients) and hip (2 studies9,54; 96 patients) arthroscopic procedures, respectively.
Study Quality
The quality of eligible studies was evaluated using the MINORS criteria (see Appendix 1, available in the online version of this article).58 All included studies were noncomparative. The mean MINORS score for eligible studies was 12.1 (SD, 1.1) or 75% (12/16). All studies had a score of 10 or higher. Only 1 study48 among those eligible reported an unbiased assessment of study endpoint.
Discussion
The current systematic review demonstrated that patients undergoing shoulder, knee, and hip arthroscopic procedures were overprescribed opioids postoperatively and often had more than one-third of the prescribed opioid remaining. Despite this, only 36% of patients had received counsel or had prior knowledge of appropriate methods of opioid disposal. Last, although the majority of patients received more opioids than they utilized, 1 in 4 patients undergoing an arthroscopic shoulder procedure received at least 1 refill.
Our finding that opioids are commonly overprescribed after arthroscopic procedures of the shoulder, knee, and hip is not unique to sports medicine. In fact, the overprescription of opioid medications has also been reported within the foot and ankle,42 upper extremity,31 and arthroplasty27 literature. Our results are also consistent with findings from large national63 and insurance68 claims database studies, which have observed an increase in mean MME prescribed after knee arthroscopy over an 8-year time period.68 Welton et al65 recently surveyed 170 members of the American Shoulder and Elbow Society (ASES) regarding pain management strategies after RCR and found that surgeons prescribed a mean of 462.5 MMEs postoperatively. This amount is consistent with the mean of 471 MMEs consumed among the pooled cohort of patients undergoing RCR noted in this study.
Because of the growing concern for opioid misuse and abuse, there has been an increased focus on developing strategies aimed at safer opioid prescribing practices (Table 4).35,37,59 One such strategy is to adhere to procedure-specific opioid prescribing guidelines, whereby surgeons provide the lowest dose and shortest duration regimen needed for adequate pain control after a specific operative intervention.35 For instance, Overton et al49 utilized a 3-step modified Delphi method to develop opioid prescribing guidelines for 20 common procedures within 8 surgical specialties, including orthopaedics.59 They recommended a maximum of 10, 20, and 20 tablets of oxycodone 5 mg (75, 150, and 150 MMEs) for arthroscopic partial meniscectomy, ACLR, and RCR, respectively. Although the aforementioned recommendations may fall short of the mean MMEs consumed by patients who underwent RCR (471 MMEs) in the current study, multiple opioid prescriptions for smaller individual amounts has been advocated by some to limit opioid excess.9
Table 4.
Strategies and recommendations for safe opioid prescribing
| Strategies and Recommendations (Level of Evidence) | |
|---|---|
| Preoperative | (1) Assess for history of opioid use, dependence, tolerance, and
risk factors for opioid-related morbidity and mortality prior to
surgery (4) (2) Educate patients regarding expectations of pain using in-office handouts/video advising patients on pain control through the postinjury, preoperative, and postoperative phases of care (1) |
| Perioperative | (1) Multimodal analgesia including regional anesthetics (1) |
| Postoperative | (1) Multimodal analgesia including regional anesthetics
(1) (2) Procedure-specific prescribing (3) (3) Provide patients with several opioid prescriptions for smaller individual amounts (2) (4) Provide patients with explicit instructions on appropriate opioid safekeeping and disposal guidelines (3) (5) Consider opioid contract (5) |
Another strategy utilized to alleviate perioperative pain and reliance on opioids is multimodal analgesia, which employs analgesics from different classes and administration sites (ie, oral, intravenous, regional) to improve pain relief and limit analgesic-related side effects.13,35 Several studies have noted decreased postoperative opioid consumption after arthroscopic procedures among patients treated with multimodal analgesia in the perioperative period.13,14,41 Commonly used medications include nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, alpha-II agonists (eg, clonidine), cyclooxygenase-2 inhibitors, gabapentinoids, N-methyl-d-aspartate receptor agonists (eg, ketamine), magnesium, liposomal bupivacaine, and corticosteroids.1,11,12,20,44,47,64 Among 170 ASES members recently surveyed regarding pain management, 88% reported using a regional nerve block for RCR, while less than 40% and 20% used NSAIDs and acetaminophen, respectively, during the perioperative period.65
More recently, there has been a growing emphasis placed on preoperative patient education of opioid use, adverse effects, and abuse. This stems from the results of a randomized controlled trial with a 2-minute narrated video and handout detailing the risks of opioid use and abuse to 68 patients undergoing arthroscopic RCR. This group consumed 42% fewer opioids and was 2.2 times more likely to discontinue opioid medications compared with the control group at the 3-month follow-up.61
Our finding that only 36% of patients received postoperative instruction or had prior knowledge of appropriate methods to dispose of opioids is concerning. Similar findings have been reported in other areas of orthopaedics.3,31 Among 1416 patients undergoing upper extremity surgery, only 5.3% received instruction on opioid disposal postoperatively.42 A systematic review to quantify how postoperative opioids were used, stored, and disposed of after surgery found that 3 of 4 patients stored opioids in unlocked locations, and less than 30% planned to or actually disposed of unused prescription opioids.3 Less than 10% employed a disposal method recommended by the Food and Drug Administration (ie, return to pharmacy/drug take-back or flushing medication down sink/toilet).3
Despite the excessive prescription of opioids reported in the current study, 1 in 4 patients received a refill after arthroscopic shoulder surgery. Patients who were using opioids within 3 months prior to an arthroscopic RCR were 3 times more likely to still require opioids 3 months postoperatively.66 Gil et al18 utilized insurance claims data to examine risk factors for prolonged opioid use among opioid-naïve patients undergoing arthroscopic shoulder procedures. They reported that a cumulative preoperative opioid dose of >743 MMEs (99 tablets of 5 mg oxycodone), a history of suicidal ideation/self-harm, alcohol dependence/abuse, a mood or anxiety disorder, female sex, and a chronic pain disorder were all significant predictors of prolonged opioid use.18
The current review has a number of limitations. First, the majority of studies failed to report on preoperative opioid use among eligible patients, which is a known predictor of prolonged opioid use postoperatively and may have acted as a confounder.18,66 Second, multimodal analgesia protocols are commonly used during arthroscopic procedures of the shoulder, knee, and hip; however, the adjunctive medications that were used during the perioperative period varied across the included studies. Third, the current review was unable to provide information regarding the mean number of days opioid medications were required for each procedure, as this information was not available from the eligible studies. Additionally, there was considerable variation in the parameters chosen to report opioid consumption among the included studies. For example, some studies reported either average or median amounts of opioid tablets consumed postoperatively; as such, these values were converted to average MMEs to standardize and pool the data. Last, very few studies commented on preoperative strategies used to educate patients on appropriate opioid use, and even fewer described safe opioid disposal practices.
Conclusion
Our investigation suggests that clinicians are overprescribing opioid medications after common sports medicine procedures, with more than one-third of prescribed opioids remaining in excess. Appropriate risk stratification tools and evidence-based recommendations for pre-, peri-, and postoperative pain management strategies after arthroscopic procedures need to be developed, which may help curb the growing opioid crisis.
Supplemental Material
Supplemental material, Appendix for Opioid Use After Common Sports Medicine Procedures: A Systematic Review by Ujash Sheth, Mitesh Mehta, Fernando Huyke, Michael A. Terry and Vehniah K. Tjong in Sports Health: A Multidisciplinary Approach
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Arumugam S, Lau CS, Chamberlain RS. Use of preoperative gabapentin significantly reduces postoperative opioid consumption: a meta-analysis. J Pain Res. 2016;9:631-640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bedard NA, Pugely AJ, Westermann RW, Duchman KR, Glass NA, Callaghan JJ. Opioid use after total knee arthroplasty: trends and risk factors for prolonged use. J Arthroplasty. 2017;32:2390-2394. [DOI] [PubMed] [Google Scholar]
- 3. Bicket MC, Long JJ, Pronovost PJ, Alexander GC, Wu CL. Prescription opioid analgesics commonly unused after surgery: a systematic review. JAMA Surg. 2017;152:1066-1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bonazza NA, Homcha B, Liu G, Leslie DL, Dhawan A. Surgical trends in arthroscopic hip surgery using a large national database. Arthroscopy. 2018;34(6):1825-1830. [DOI] [PubMed] [Google Scholar]
- 5. Chen JH, Humphreys K, Shah NH, Lembke A. Distribution of opioids by different types of Medicare prescribers. JAMA Intern Med. 2016;176:259-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Clarke H, Page G, McCartney C, et al. Pregabalin reduces postoperative opioid consumption and pain for 1 week after hospital discharge, but does not affect function at 6 weeks or 3 months after total hip arthroplasty. Br J Anaesth. 2015;115:903-911. [DOI] [PubMed] [Google Scholar]
- 7. Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL. National trends in rotator cuff repair. J Bone Joint Surg Am. 2012;94:227-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Colvin AC, Harrast J, Harner C. Trends in hip arthroscopy. J Bone Joint Surg Am. 2012;94:e23. [DOI] [PubMed] [Google Scholar]
- 9. Cunningham D, Lewis B, Hutyra C, Nho S, Olson S, Mather R. Prospective, observational study of opioid use after hip arthroscopy for femoroacetabular impingement syndrome. Arthroscopy. 2018;34:1488-1497.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cvetanovich GL, Chalmers PN, Levy DM, et al. Hip arthroscopy surgical volume trends and 30-day postoperative complications. Arthroscopy. 2016;32:1286-1292. [DOI] [PubMed] [Google Scholar]
- 11. Doleman B, Read D, Lund JN, Williams JP. Preventive acetaminophen reduces postoperative opioid consumption, vomiting, and pain scores after surgery: systematic review and meta-analysis. Reg Anesth Pain Med. 2015;40:706-712. [DOI] [PubMed] [Google Scholar]
- 12. Eckhard L, Jones T, Collins JE, Shrestha S, Fitz W. Increased postoperative dexamethasone and gabapentin reduces opioid consumption after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2019;27:2162-2172. [DOI] [PubMed] [Google Scholar]
- 13. Elkassabany NM, Wang A, Ochroch J, Mattera M, Liu J, Kuntz A. Improved quality of recovery from ambulatory shoulder surgery after implementation of a multimodal perioperative pain management protocol. Pain Med. 2019;5:1012-1019. [DOI] [PubMed] [Google Scholar]
- 14. Ellis TA, 2nd, Hammoud H, Merced PD, et al. Multimodal clinical pathway with adductor canal block decreases hospital length of stay, improves pain control, and reduces opioid consumption in total knee arthroplasty patients: a retrospective review. J Arthroplasty. 2018;33:2440-2448. [DOI] [PubMed] [Google Scholar]
- 15. Frank RM, Chalmers PN, Moric M, Leroux T, Provencher MT, Romeo AA. Incidence and changing trends of shoulder stabilization in the United States. Arthroscopy. 2018;34:784-792. [DOI] [PubMed] [Google Scholar]
- 16. Fujii MH, Hodges AC, Russell RL, et al. Post-discharge opioid prescribing and use after common surgical procedure. J Am Coll Surg. 2018;226:1004-1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Garrett WE, Jr, Swiontkowski MF, Weinstein JN, et al. American Board of Orthopaedic Surgery Practice of the Orthopaedic Surgeon: part-II, certification examination case mix. J Bone Joint Surg Am. 2006;88:660-667. [DOI] [PubMed] [Google Scholar]
- 18. Gil JA, Gunaseelan V, DeFroda SF, Brummett CM, Bedi A, Waljee JF. Risk of prolonged opioid use among opioid-naive patients after common shoulder arthroscopy procedures. Am J Sports Med. 2019;47:1043-1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Grace TR, Khanna K, Choo KJ, et al. The influence of preoperative opioid use on inpatient opioid requirements and discharge prescriptions after primary shoulder arthroplasty. J Shoulder Elbow Surg. 2018;27:1572-1579. [DOI] [PubMed] [Google Scholar]
- 20. Gürkan Y, Yörükoğlu HU, Is˛ık E, Kus˛ A. The effect of ibuprofen on postoperative opioid consumption following total hip replacement surgery. Turk J Anesthesiol Reanim. 2019;47:31-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Haas SB, Premkumar A, Lovecchio FC, et al. Characterization of postoperative opioid consumption and disposal patterns after total knee arthroplasty with a novel mobile phone text messaging platform. Orthop Proc. 2018;100-B(suppl 12):65. [Google Scholar]
- 22. Hancock KJ, Westermann RR, Shamrock AG, Duchman KR, Wolf BR, Amendola A. Trends in knee articular cartilage treatments: an American Board of Orthopaedic Surgery Database Study. J Knee Surg. 2019;32:85-90. [DOI] [PubMed] [Google Scholar]
- 23. Herzog MM, Marshall SW, Lund JL, Pate V, Mack CD, Spang JT. Trends in incidence of ACL reconstruction and concomitant procedures among commercially insured individuals in the United States, 2002-2014. Sports Health. 2018;10:523-531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ho E, Doherty M, Thomas R, Attia J, Oldmeadow C, Clapham M. Prescription of opioids to post-operative orthopaedic patients at time of discharge from hospital: a prospective observational study. Scand J Pain. 2018;18:253-259. [DOI] [PubMed] [Google Scholar]
- 25. Howard DH. Trends in the use of knee arthroscopy in adults. JAMA Intern Med. 2018;178:1557-1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Huang PS, Copp SN. Oral opioids are overprescribed in the opiate-naive patient undergoing total joint arthroplasty. J Am Acad Orthop Surg. 2019;27:e702-e708. [DOI] [PubMed] [Google Scholar]
- 28. Iyengar JJ, Samagh SP, Schairer W, Singh G, Valone FH, Feeley BT. Current trends in rotator cuff repair: surgical technique, setting, and cost. Arthroscopy. 2014;30:284-288. [DOI] [PubMed] [Google Scholar]
- 29. Jensen AR, Cha PS, Devana SK, et al. Evaluation of the trends, concomitant procedures, and complications with open and arthroscopic rotator cuff repairs in the Medicare population. Orthop J Sports Med. 2017;5:2325967117731310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kelly JS, Opsha Y, Costello J, Schiller D, Hola ET. Opioid use in knee arthroplasty after receiving intravenous acetaminophen. Pharmacotherapy. 2014;34(suppl 1):22S-26S. [DOI] [PubMed] [Google Scholar]
- 31. Kim N, Matzon JL, Abboudi J, et al. A prospective evaluation of opioid utilization after upper-extremity surgical procedures: identifying consumption patterns and determining prescribing guidelines. J Bone Joint Surg Am. 2016;98:e89. [DOI] [PubMed] [Google Scholar]
- 32. Kim S, Bosque J, Meehan JP, Jamali A, Marder R. Increase in outpatient knee arthroscopy in the United States: a comparison of National Surveys of Ambulatory Surgery, 1996 and 2006. J Bone Joint Surg Am. 2011;93:994-1000. [DOI] [PubMed] [Google Scholar]
- 33. Kremers HM, Schilz SR, Van Houten HK, et al. Trends in utilization and outcomes of hip arthroscopy in the United States between 2005 and 2013.J Arthroplasty. 2017;32:750-755. [DOI] [PubMed] [Google Scholar]
- 34. Kumar K, Gulotta LV, Dines JS, et al. Unused opioid pills after outpatient shoulder surgeries given current perioperative prescribing habits. Am J Sports Med. 2017;45:636-641. [DOI] [PubMed] [Google Scholar]
- 35. Labrum JT, 4th, Ilyas AM. The opioid epidemic: postoperative pain management strategies in orthopaedics. JBJS Rev. 2017;5:e14. [DOI] [PubMed] [Google Scholar]
- 36. Lisik JP, Dowsey MM, Petterwood J, Choong PF. Review of knee arthroscopic practice and coding at a major metropolitan centre. ANZ J Surg. 2017;87:380-384. [DOI] [PubMed] [Google Scholar]
- 37. Lovecchio F, Derman P, Stepan J, et al. Support for safer opioid prescribing practices: a catalog of published use after orthopaedic surgery. J Bone Joint Surg Am. 2017;99:1945-1955. [DOI] [PubMed] [Google Scholar]
- 38. Makary MA, Overton HN, Wang P. Overprescribing is major contributor to opioid crisis. BMJ. 2017;359:J4792. [DOI] [PubMed] [Google Scholar]
- 39. Manchikanti L, Helm S, 2nd, Fellows B, et al. Opioid epidemic in the United States. Pain Physician. 2012;15 3suppl:eS9-eS38. [PubMed] [Google Scholar]
- 40. McCormick F, Harris JD, Abrams GD, et al. Trends in the surgical treatment of articular cartilage lesions in the United States: an analysis of a large private-payer database over a period of 8 years. Arthroscopy. 2014;30:222-226. [DOI] [PubMed] [Google Scholar]
- 41. McLaughlin DC, Cheah JW, Aleshi P, Zhang AL, Ma CB, Feeley BT. Multimodal analgesia decreases opioid consumption after shoulder arthroplasty: a prospective cohort study. J Shoulder Elbow Surg. 2018;27:686-691. [DOI] [PubMed] [Google Scholar]
- 42. Merrill HM, Dean DM, Mottla JL, Neufeld SK, Cuttica DJ, Buchanan MM. Opioid consumption following foot and ankle surgery. Foot Ankle Int. 2018;39:649-656. [DOI] [PubMed] [Google Scholar]
- 43. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mont MA, Beaver WB, Dysart SH, Barrington JW, Del Gaizo DJ. Local infiltration analgesia with liposomal bupivacaine improves pain scores and reduces opioid use after total knee arthroplasty: results of a randomized controlled trial.J Arthroplasty. 2018;33:90-96. [DOI] [PubMed] [Google Scholar]
- 45. Morris BJ, Mir HR. The opioid epidemic: impact on orthopaedic surgery. J Am Acad Orthop Surg. 2015;23:267-271. [DOI] [PubMed] [Google Scholar]
- 46. National Center for Injury Prevention and Control. CDC compilation of benzodiazepines, muscle relaxants, stimulants, zolpidem, and opioid analgesics with oral morphine milligram equivalent conversion factors, 2016. version. Atlanta, GA: Centers for Disease Control and Prevention; 2016. [Google Scholar]
- 47. Nielsen RV, Fomsgaard JS, Nikolajsen L, Dahl JB, Mathiesen O. Intraoperative S-ketamine for the reduction of opioid consumption and pain one year after spine surgery: a randomized clinical trial of opioid-dependent patients. Eur J Pain. 2019;23:455-460. [DOI] [PubMed] [Google Scholar]
- 48. O’Neill DF, Webb Thomas C. Less is more: limiting narcotic prescription quantities for common orthopedic procedures. Phys Sportsmed. 2014;42:100-105. [DOI] [PubMed] [Google Scholar]
- 49. Overton HN, Hanna MN, Bruhn WE, et al. Opioid-prescribing guidelines for common surgical procedures: an expert panel consensus. J Am Coll Surg. 2018;227:411-418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Parker BR, Hurwitz S, Spang J, Creighton R, Kamath G. Surgical trends in the treatment of meniscal tears: analysis of data from the American Board of Orthopaedic Surgery Certification Examination Database. Am J Sports Med. 2016;44:1717-1723. [DOI] [PubMed] [Google Scholar]
- 51. Riff AJ, Frank RM, Sumner S, et al. Trends in shoulder stabilization techniques used in the United States based on a large private-payer database. Orthop J Sports Med. 2017;5:2325967117745511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Rudd RA, Aleshire N, Zibbell JE, Gladden RM. Increases in drug and opioid overdose deaths—United States, 2000-2014. Am J Transplant. 2016;16:1323-1327. [DOI] [PubMed] [Google Scholar]
- 53. Sabatino MJ, Kunkel ST, Ramkumar DB, Keeney BJ, Jevsevar DS. Excess opioid medication and variation in prescribing patterns following common orthopaedic procedures. J Bone Joint Surg Am. 2018;100:180-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Selley R, Butler B, Johnson DL, Cogan C, Terry MA, Tjong V. A prospective pilot study in hip arthroscopy: how many opiates should we prescribe for pain? 2018 World Congress of Regional Anesthesia & Pain Medicine https://epostersonline.com/ASRAWORLD18/node/1163. Accessed March 25, 2020. [Google Scholar]
- 55. Siemieniuk RAC, Harris IA, Agoritsas T, et al. Arthroscopic surgery for degenerative knee arthritis and meniscal tears: a clinical practice guideline. BMJ. 2017;357:j1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Sing DC, Barry JJ, Cheah JW, Vail TP, Hansen EN. Long-acting opioid use independently predicts perioperative complication in total joint arthroplasty. J Arthroplasty. 2016;31(9 suppl):170-174.e1. [DOI] [PubMed] [Google Scholar]
- 57. Sing DC, Feeley BT, Tay B, Vail TP, Zhang AL. Age-related trends in hip arthroscopy: a large cross-sectional analysis. Arthroscopy. 2015;31:2307-2313.e2. [DOI] [PubMed] [Google Scholar]
- 58. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological Index for Non-Randomized Studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73:712-716. [DOI] [PubMed] [Google Scholar]
- 59. Soffin EM, Waldman SA, Stack RJ, Liguori GA. An evidence-based approach to the prescription opioid epidemic in orthopedic surgery. Anesth Analg. 2017;125:1704-1713. [DOI] [PubMed] [Google Scholar]
- 60. Suchman KI, Behery OA, Mai DH, Anil U, Bosco JA. The demographic and geographic trends of meniscal procedures in New York State: an analysis of 649,470 patients over 13 years. J Bone Joint Surg Am. 2018;100:1581-1588. [DOI] [PubMed] [Google Scholar]
- 61. Syed UAM, Aleem AW, Wowkanech C, et al. Neer Award 2018. The effect of preoperative education on opioid consumption in patients undergoing arthroscopic rotator cuff repair: a prospective, randomized clinical trial.J Shoulder Elbow Surg. 2018;27:962-967. [DOI] [PubMed] [Google Scholar]
- 62. Tepolt FA, Bido J, Burgess S, Micheli LJ, Kocher MS. Opioid overprescription after knee arthroscopy and related surgery in adolescents and young adults. Arthroscopy. 2018;34:3236-3243. [DOI] [PubMed] [Google Scholar]
- 63. Thiels CA, Anderson SS, Ubl DS, et al. Wide variation and overprescription of opioids after elective surgery. Ann Surg. 2017;266:564-573. [DOI] [PubMed] [Google Scholar]
- 64. VanWagner MJ, Krebs NM, Corser W, Johnson CN. Liposomal bupivacaine reduces opioid consumption and length of stay in patients undergoing primary total hip arthroplasty. Hip Int. 2019;29:276-281. [DOI] [PubMed] [Google Scholar]
- 65. Welton KL, Kraeutler MJ, McCarty EC, Vidal AF, Bravman JT. Current pain prescribing habits for common shoulder operations: a survey of the American Shoulder and Elbow Surgeons membership. J Shoulder Elbow Surg. 2018;27(6S):S76-S81. [DOI] [PubMed] [Google Scholar]
- 66. Westermann RW, Anthony CA, Bedard N, et al. Opioid consumption after rotator cuff repair. Arthroscopy. 2017;33:1467-1472. [DOI] [PubMed] [Google Scholar]
- 67. Wojahn RD, Bogunovic L, Brophy RH, et al. Opioid consumption after knee arthroscopy. J Bone Joint Surg Am. 2018;100:1629-1636. [DOI] [PubMed] [Google Scholar]
- 68. Wunsch H, Wijeysundera DN, Passarella MA, Neuman MD. Opioids prescribed after low-risk surgical procedures in the United States, 2004-2012. JAMA. 2016;315:1654-1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Appendix for Opioid Use After Common Sports Medicine Procedures: A Systematic Review by Ujash Sheth, Mitesh Mehta, Fernando Huyke, Michael A. Terry and Vehniah K. Tjong in Sports Health: A Multidisciplinary Approach