Abstract
Context:
Cardiovascular diseases cause 17 million deaths annually worldwide, of which hypertension is responsible for 9.4 million and a 7% burden of disease. High blood pressure is responsible for 45% of deaths from heart disease and 51% of deaths from stroke.
Objective:
The aim of this systematic review and meta-analysis was to quantify the effect of isometric resistance training on systolic, diastolic, and mean arterial blood pressure (SBP, DBP, and MAP, respectively) values in normotensive adult participants.
Data Sources:
This study was registered with the PROSPERO database. Eligible studies were identified after performing a systematic search within the following databases: PubMed, Scielo, BioMed Central, Clinical Trials, EMBASE, Cochrane Central Register of Controlled Trials, and EBSCO.
Study Selection:
Randomized controlled trials that categorized participants as normotensive according to the guidelines of the American Heart Association and the American College of Cardiology were included.
Study Design:
Systematic review with meta-analysis.
Level of Evidence:
Level 1.
Data Extraction:
Data related to participant characteristics, exercise programs, level of evidence, risk of bias, Consensus on Exercise Reporting Template, and outcomes of interest were systematically reviewed independently by 2 authors.
Results:
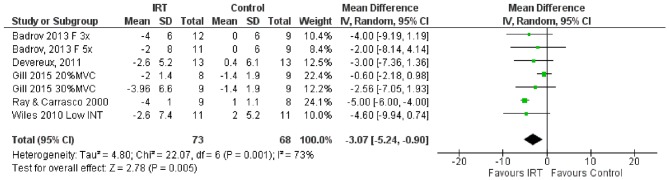
A total of 6 randomized controlled trials were included. The following reductions in blood pressure (compared with the control group) were generated by isometric resistance training: SBP (mean difference [MD], −2.83 mm Hg; 95% CI, −3.95 to −1.72; P < 0.00001), DBP (MD, −2.73; 95% CI, −4.23 to −1.24; P = 0.0003), and MAP (MD, −3.07; 95% CI, −5.24 to −0.90; P = 0.005).
Conclusion:
It appears that isometric resistance training reduces SBP, DBP, and MAP in normotensive young adults in a statistically significant and clinically relevant manner. This type of exercise could be considered effective in preventing arterial hypertension.
Keywords: hypertension, blood pressure management, primary prevention, meta-analysis, static resistance training
Currently, cardiovascular diseases cause 17 million deaths annually worldwide, of which hypertension is responsible for 9.4 million and a 7% burden of disease. High blood pressure (BP) is responsible for 45% of deaths from heart disease and 51% of deaths from stroke.27 There was also an upward trend in cases of hypertension. Thus, in 1980, approximately 600 million adults older than 25 years had high BP, and by 2008, this number had grown to 1 billion adults.26 In general, the prevalence of hypertension is higher in low- and middle-income countries compared with high-income countries, and the number of undiagnosed, uncontrolled, and untreated patients with hypertension is higher in low-income countries due to weaknesses in their health care systems.26 Nonetheless, there are several highly evidence-based strategies and recommendations proposed for mitigating the impact of hypertension from important organizations around the world, including the American College of Cardiology, American Heart Association, European Society of Cardiology, and the European Society of Hypertension.22,25
Increasing weekly physical activity, reducing weight, and reducing smoking and alcohol consumption together with a healthy diet are strategies that generate significant clinically important reductions in BP (~2 to ~10 mm Hg).22,25,27 Particularly, a decrease of 2 to 3 mm Hg in systolic or diastolic BP (SBP or DBP, respectively) generates important reductions on the mortality risk caused by cardiovascular disease and all other causes. There is, nevertheless, an association between physical activity and hypertension, as that found in a cohort study from 2018, which showed a 28% chance of developing hypertension if the individual was physically inactive.21 Likewise, the likelihood of a sedentary person suffering high BP nearly doubles.21 However, the body of evidence on the effects of isometric resistance training (IRT) in normotensive, prehypertensive, and hypertensive individuals is growing.2,4,9,10,13,20 Thus, a systematic review and meta-analysis that included randomized controlled trials in which IRT was performed in normal and hypertensive adults concluded that this form of training has the potential to significantly reduce BP and suggested it as a complementary treatment method.9 In general, this meta-analysis reported a significant reduction in SBP, DBP, and mean arterial BP (MAP) (–5.20, –3.91, and –3.33 mm Hg, respectively).9 Another systematic review that quantified the effects of IRT on SBP, DBP, and MAP in normal and hypertensive adults concluded that the magnitude of the effect on their results was greater than that previously reported in aerobic or dynamic resistance training.2
In general, there is a large body of scientific evidence related to the effect of IRT on BP levels. Mainly, the current state of science is limited to systematic reviews of randomized controlled trials in pre- and hypertensive patients.2,4,9,10,13,20 Nevertheless, there is still uncertainty about the reductions generated by IRT on SBP, DBP, and MAP due to the heterogeneity of the results reported by these studies.2,4,9,10,13,20
Particularly, in the preliminary searches, we did not find systematic reviews and meta-analyses that reported, in their main analysis, on the effects of IRT on BP values of normotensive participants with current recommendations from the American Heart Association and the American College of Cardiology.22 Therefore, the aim of this systematic review and meta-analysis was to quantify the effect of IRT on SBP, DBP, and MAP values in normotensive adult participants.
Methods
This systematic review and meta-analysis was performed subject to the criteria and recommendations of the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement.12 This study was registered with the PROSPERO database on November 13, 2018.
Study Selection
The studies included in this systematic review met the following criteria: (1) randomized controlled trials (RCTs), (2) adult participants (age >18 years), (3) normotensive participants (SBP <120 mm Hg and DBP <80 mm Hg), and (4) main outcome BP. Studies among pregnant women and studies currently in development were excluded from this review.
Search Strategy
Potentially eligible studies were identified after performing a systematic search on the following databases: PubMed, Scielo, BioMed Central, Clinical Trials, EMBASE, Cochrane Central Register of Controlled Trials, EBSCO, the gray literature, and journals related to the area. No restrictions on language or publication timeline were applied. The search strategy used keywords, Medical Subject Headings (MeSH), and Boolean connectors, including: isometric exercise OR isometric strength training OR isometric resistance training OR handgrip AND blood pressure OR arterial blood pressure OR arterial tension AND adults normotensive OR normotensives AND randomized clinical trials OR randomized controlled trials OR clinical study OR clinical trials. Furthermore, references of studies were reviewed to further identify randomized controlled trials that met the inclusion criteria.
Data Extraction and Risk of Bias Assessment
Data related to participant characteristics, exercise programs, and outcomes of interest were systematically reviewed independently (Table 1). This information went into a database created by each author in Microsoft Excel 2016. Two authors separately assessed the risk of bias of the studies using the Cochrane Collaboration tool for risk of bias (Version 5.1.0).7 We rated each criterion as low, high, or unclear risk of bias.
Table 1.
Characteristics of included studies
| Study and Country | Participants | Duration, wk | Frequency | Exercise Training Characteristics |
|---|---|---|---|---|
| Badrov et al, 2013,1 Canada | CG: F 9 EG IHG Fx 3: F 12 EG IHG Fx 5: F 11 |
8 | EG IHG Fx 3: 3d EG IHG Fx 5: 5d |
4 × 2-minute nondominant handgrip contractions at 30% MVC; 4-minute recovery between sets |
| Devereux et al, 2011,5 United Kingdom | CG: M 13 EG: M 13 |
4 | 3 d/wk | 4 × 2-minute bilateral leg extension isometric contractions at 95% HR peak; 3-minute recovery between sets |
| Gill et al, 2015,6 USA | CG: M 4 and F 14 EG 23% MVC: M 4 and F 4 EG 34% MCV: M 2 and F 7 |
3 | 3 d/wk | EG 23% MVC: 4 × 2-minute bilateral leg extension isometric
contractions at 23% MVC; 3-minute recovery between
sets EG 34% MVC: 4 × 2-minute bilateral leg extension isometric contractions at 34% MVC; 3-minute recovery between sets |
| Howden et al, 2002,8 United Kingdom | CG: M 5 and F 3 EG Handgrip: M 6 and F 2 |
5 | 3 d/wk | 4 × 2-minute bilateral arm flexion isometric contractions at 30% MVC; 3-minute recovery between sets |
| Ray and Carrasco, 2000,17 USA | CG: 8 mixed EG: 9 mixed |
5 | 4 d/wk | 4 × 3-minute dominant handgrip contractions at 30% MVC; 5-minute recovery between sets |
| Wiles et al, 2010,24 United Kingdom | CG: M 11 EG Low INT: M 11 |
8 | 3 d/wk | 4 × 2-minute bilateral leg extension isometric contractions at 10% MVC; 2-minute recovery between sets |
CG, control group; EG, experimental group; F, female; Fx, training frequency; HR peak, heart rate peak; IHG, isometric handgrip; IRT, isometric resistance training; low INT, low intensity; M, male; mixed, both sexes; MVC, maximal voluntary contraction.
Reporting of Exercise Interventions in the Isometric Resistance Training Programs
We used the Consensus on Exercise Reporting Template (CERT) tool to evaluate the completeness of the reports of interventions with exercise.18,19 “CERT has the potential to increase clinical uptake of effective exercise programs, enable research replication, reduce research waste, and improve patient outcomes.”18
Studies Included in the Review
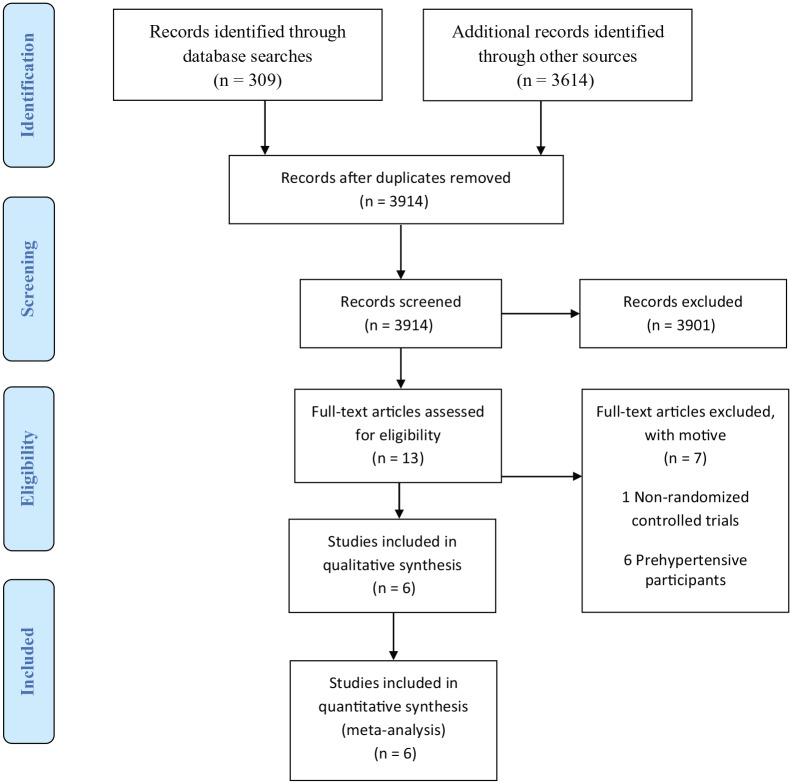
In total, 3923 references were obtained from the search, of which 309 came from scientific databases such as PubMed, Scielo, BioMed Central, Clinical Trials, EMBASE, Cochrane Central Register of Controlled Trials, and EBSCO. A total of 3614 studies were identified in journals and the gray literature. After eliminating duplicates and screening by title and abstract, a total of 13 articles remained for full-text reading (Figure 1).
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart.
Data Synthesis
The main outcome variables for this study were SBP, DBP, and MAP.
Statistical Analysis
For continuous outcomes, we recorded group size, mean values, and standard deviations for each group compared in the included studies. Pooled effects were calculated using an inverse-variance model, and the data were pooled to generate a mean difference (MD) in millimeters of mercury (mm Hg) with corresponding 95% confidence intervals (CIs). All studies for each outcome reported data in the same units, so we were able to pool all studies regardless of whether they reported change data or final data. Significance was set at P < 0.05. Statistical heterogeneity was evaluated using the I2 statistic and classified according to the Cochrane Handbook7: negligible heterogeneity, 0% to 40%; moderate heterogeneity, 30% to 60%; substantial heterogeneity, 50% to 90%; and considerable heterogeneity, 75% to 100%. A fixed-effects model was used if heterogeneity was low (I2 < 50%); otherwise, a random-effects model was used. All analyses were performed by a single reviewer using Review Manager Version 5.316 and checked against the data extracted by 1 author.
Results
Six studies were included in the qualitative and quantitative analysis, with a total of 8 intervention groups and 139 normotensive adult participants (intervention group, n = 81; control group, n = 58).1,5,6,8,17,24 Particularly, 2 intervention groups were excluded due to reported ranges for prehypertension mean SBP at baseline (high-intensity intervention group: mean ± SD SBP, 121.5 ± 4.6 mm Hg24; knee extension intervention group: mean ± SD SBP, 121 ± 9.6 mm Hg8). On the other hand, 5 studies used a parallel design1,6,8,17,24 while the remainder used a crossover design.5 Three of the 6 studies included participants of both sexes,6,8,17 2 included only men,5,24 and 1 article reported the inclusion of only women.1 In general, studies reported how they measured BP. Five studies reported that they measured BP using automated brachial oscillometry.1,5,8,17,24 One study measured BP using an automated sphygmomanometer6 (Table 1).
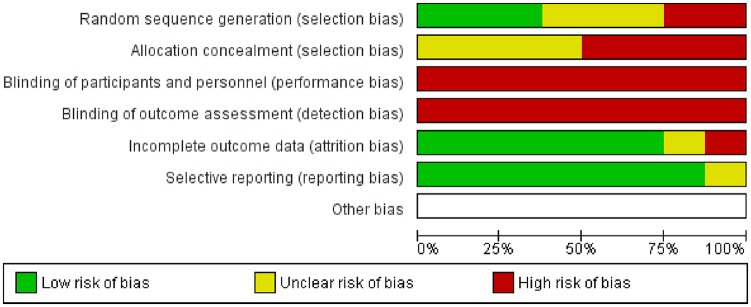
Risk of Bias Assessment
The studies included in this systematic review had a high risk of bias with reference to random sequence generation, allocation concealment, and blinding of outcome assessment. Only 2 studies reported performing random sequence generation.1,24 The 6 RCTs included did not perform blinding of participants and study personnel, neither did they report blinding of outcome assessors.1,5,6,8,17,24 Three studies did not describe allocation concealment,1,5,17 and the remaining 3 were determined to have an unclear risk of bias6,8,24 (Figure 2).
Figure 2.
Risk of bias presented as a percentage across all included studies.
Reporting of Exercise Interventions in the IRT Programs
According to the CERT tool, the RCTs included in this study scored an average of 9 on a scale of 0 to 16, which evaluates the completeness of reporting of interventions with exercise. Specifically, studies described the instrument used to perform the IRT (manual dynamometry and isokinetic dynamometer) and clearly detailed the frequency, intensity, time, and type (FITT) of intervention.1,5,6,8,17,24 In general, only 2 studies described exercise supervision and qualifications of the person supervising the intervention.1,6 Two articles reported adverse events.1,8 Four of the 6 RCTs described performing IRT progression.5,8 Only 2 studies reported measuring exercise adherence.1,24 Finally, 2 studies reported that the intervention was carried out as planned.1,24
Quantitative Analysis
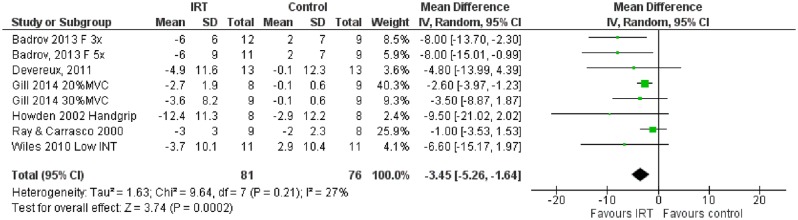
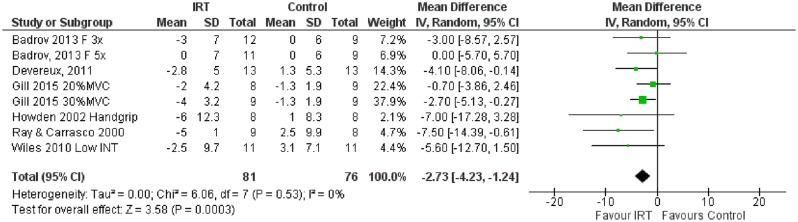
The effects of IRT on SBP, DBP, and MAP are shown in Figures 3, 4, and 5, respectively. Significant and substantial heterogeneity existed in MAP results (P = 0.001; I2 = 73%). For SBP there was negligible, non–statistically significant heterogeneity (P = 0.21;I2 = 27%), In particular, consistent results were reported for DBP (P = 0.53; I2 = 0%). IRT statistically and significantly decreased SBP (MD, –2.83 mm Hg; 95% CI, –3.95 to −1.72; P < 0.00001), DBP (MD, –2.73 mm Hg; 95% CI, –4.23 to −1.24; P = 0.0003), and MAP (MD, –3.07 mm Hg; 95% CI, –5.24 to −0.90; P = 0.005) compared with the control group.
Figure 3.
Effect of isometric resistance training (IRT) on systolic blood pressure (mm Hg).
Figure 4.
Effect of isometric resistance training (IRT) on diastolic blood pressure (mm Hg).
Figure 5.
Effect of isometric resistance training (IRT) on mean arterial pressure (mm Hg).
Discussion
The aim of this systematic review and meta-analysis was to quantify the effect of isometric resistance training on the values of SBP, DBP, and MAP in normotensive adult participants. The main results of this research report that IRT generated clinically relevant and statistically significant reductions on SBP (–2.83 mm Hg; P < 0.00001), DBP (–2.73 mm Hg; P = 0.0003), and MAP (–3.07 mm Hg; P = 0.005) in normotensive adult participants. However, substantial heterogeneity was reported for MAP, and we suggest being cautious with the interpretation of this result.
In general, cohort studies and clinical guidelines report that a reduction of 2 mm Hg in SBP reduces the risk of death by stroke by 6%, by coronary heart disease by 4%, and by all causes by 3%.23 Likewise, a reduction of 2 mm Hg DBP reduces the prevalence of hypertension by 17% and, furthermore, reduces the incidence of stroke-related events by 15% and the incidence of coronary heart disease by 6%.3
To our knowledge, this is the first systematic review with a subsequent meta-analysis that investigates the effects of IRT on BP values in normotensive participants according to current recommendations from the American Heart Association and the American College of Cardiology.22 Previously, systematic reviews reported results from subgroup analyses that described significant reductions in SBP, DBP, and MAP in participants classified as normotensive by the guidelines at that time.2,9,10,13,20 Nevertheless, our results show lower magnitudes of BP reductions than those previously reported.2,4,9,10,13,20 This could be specifically due to the strong association reported that IRT generates reductions of greater magnitude in medicated hypertensive patients.14
On the other hand, the articles included in this research had a wide patient age range (18-35 years) and included participants of both sexes. In accordance with our results, the body of current scientific evidence reports that IRT reduces BP values in normotensive and hypertensive patients younger than 45 years.9,13 With regard to sex, prior research showed that IRT lowers BP by a similar magnitude in normotensive and hypertensive men and women.2,4,9,10,13,20
In particular, the included RCTs describe different types of accessories for performing IRT in the upper and lower kinetic chain. These results suggest that performing IRT with handgrips or isokinetic dynamometry appears to generate statistically significant reductions in SBP, DBP, and MAP. A sample of the above is the inclusion in other meta-analysis of studies using handgrips, isokinetic dynamometers, and body weight exercises, which reported significant decreases in BP.2,4,9,10,13,20 Additionally, the articles included in this systematic review used similar IRT doses or protocols (FITT): 4 sets of 2 minutes at 10% to 34% of maximal voluntary contraction (MVC) or their equivalents in electromyography or peak heart rate, with a recovery time between sets of 2 to 5 minutes, performed 3 to 4 times a week over 3 to 8 weeks. By comparing the scientific evidence that investigates the effects of IRT on BP, the dose described above is the most commonly used by primary and secondary research.2,4,9,10,11,13,15,20 Furthermore, a wide range of intensities (5%-50% MVC) can be used during IRT to generate clinically relevant and statistically significant reductions of SBP, DBP, and MAP in normotensive adult participants. Finally, we currently know an efficient and safe IRT dose for lowering BP in normotensive young adult patients.2,9,10,13,20
One of the strengths of this systematic review and meta-analysis is the absence of statistical heterogeneity in the DBP result (I2 = 0%; negligible heterogeneity). By contrast, a systematic review in 2014 showed substantial heterogeneity as well as statistical significance regarding the DBP reductions generated by IRT in normotensive participants (I2 = 74%; P = 0.0003).2 Likewise, another meta-analysis reported substantial heterogeneity in findings of DBP in normotensive participants, although it did not achieve statistical significance (I2 = 64%; P = 0.06).10
Limitations
There were several potential limitations to this meta-analysis, which should be kept in mind: (1) the RCTs that were part of this study have methodological problems and high risk of bias; (2) nonreporting or allocation concealment issues; (3) participant knowledge of interventions as well as unblinded outcome assessment; (4) our meta-analyses included studies with a low number of participants; (5) the overall number of studies that met the inclusion criteria is small; and (6) BP is a parameter with multifactorial affectation, in consequence, other factors such as nutrition and the consumption of stimulants like caffeine may affect it and have not been included in the analysis. Because this has not been accounted for in the selected studies, this could mean a potential limitation when interpreting our results. We therefore recommend caution regarding the interpretation of the results presented in this study.
Conclusion
It appears that IRT reduces SBP, DBP, and MAP in normotensive young adults in a statistically significant and clinically relevant manner. We therefore suggest that this type of exercise (specifically isometric leg extension and handgrip exercises) be considered effective therapy for preventing arterial hypertension. The efficiency of this intervention is limited to brief time periods. Because of this, long-term effects (minimum 1 year) should be investigated.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Badrov MB, Bartol CL, Dibartolomeo MA, Millar PJ, McNevin NH, McGowan CL. Effects of isometric handgrip training dose on resting blood pressure and resistance vessel endothelial function in normotensive women. Eur J Appl Physiol. 2013;113:2091-2100. [DOI] [PubMed] [Google Scholar]
- 2. Carlson DJ, Dieberg G, Hess NC, Millar PJ, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis. Mayo Clin Proc. 2014;89:327-334. [DOI] [PubMed] [Google Scholar]
- 3. Cook NR, Cohen J, Hebert PR, Taylor JO, Hennekens CH. Implications of small reductions in diastolic blood pressure for primary prevention. JAMA Intern Med. 1995;155:701-709. [PubMed] [Google Scholar]
- 4. Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. 2013;2:e004473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Devereux GR, Wiles JD, Swaine I. Markers of isometric training intensity and reductions in resting blood pressure. J Sports Sci. 2011;29:715-724. [DOI] [PubMed] [Google Scholar]
- 6. Gill KF, Arthur ST, Swaine I, et al. Intensity-dependent reductions in resting blood pressure following short-term isometric exercise training. J Sports Sci. 2015;33:616-621. [DOI] [PubMed] [Google Scholar]
- 7. Higgins JPT, Green S, eds. Manual Cochrane de revisiones sistemáticas de intervenciones. Cochrane Collaboration; 2011. [Google Scholar]
- 8. Howden R, Lightfoot JT, Brown SJ, Swaine IL. The effects of isometric exercise training on resting blood pressure and orthostatic tolerance in humans. Exp Physiol. 2002;87:507-515. [DOI] [PubMed] [Google Scholar]
- 9. Inder JD, Carlson DJ, Dieberg G, McFarlane JR, Hess NCL, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis to optimize benefit. Hypertens Res. 2016;39:89-94. [DOI] [PubMed] [Google Scholar]
- 10. Jin YZ, Yan S, Yuan WX. Effect of isometric handgrip training on resting blood pressure in adults: a meta-analysis of randomized controlled trials. J Sports Med Phys Fitness. 2017;57:154-160. [DOI] [PubMed] [Google Scholar]
- 11. Lawrence MM, Cooley ID, Huet YM, Arthur ST, Howden R. Factors influencing isometric exercise training-induced reductions in resting blood pressure. Scand J Med Sci Sports. 2015;25:131-142. [DOI] [PubMed] [Google Scholar]
- 12. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62:e1-e34. [DOI] [PubMed] [Google Scholar]
- 13. López-Valenciano A, Ruiz-Pérez I, Ayala F, Sánchez-Meca J, Vera-Garcia FJ. Updated systematic review and meta-analysis on the role of isometric resistance training for resting blood pressure management in adults. J Hypertens. 2019;37:1320-1333. [DOI] [PubMed] [Google Scholar]
- 14. Millar PJ, Bray SR, McGowan CL, MacDonald MJ, McCartney N. Effects of isometric handgrip training among people medicated for hypertension: a multilevel analysis. Blood Press Monit. 2007;12:307-314. [DOI] [PubMed] [Google Scholar]
- 15. Millar PJ, McGowan CL, Cornelissen VA, Araujo CG, Swaine IL. Evidence for the role of isometric exercise training in reducing blood pressure: potential mechanisms and future directions. Sports Med. 2014;44:345-356. [DOI] [PubMed] [Google Scholar]
- 16. The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen, Denmark: The Nordic Cochrane Centre, The Cochrane Collaboration; 2014. [Google Scholar]
- 17. Ray CA, Carrasco DI. Isometric handgrip training reduces arterial pressure at rest without changes in sympathetic nerve activity. Am J Physiol Heart Circ Physiol. 2000;279:H245-H249. [DOI] [PubMed] [Google Scholar]
- 18. Slade SC, Dionne CE, Underwood M, Buchbinder R. Consensus on Exercise Reporting Template (CERT): explanation and elaboration statement. Br J Sports Med. 2016;50:1428-1437. [DOI] [PubMed] [Google Scholar]
- 19. Slade SC, Dionne CE, Underwood M, et al. Template (CERT): modified Delphi. Phys Ther. 2016;96:1514-1524. [DOI] [PubMed] [Google Scholar]
- 20. Smart NA, Way D, Carlson D, et al. Effects of isometric resistance training on resting blood pressure: individual participant data meta-analysis. J Hypertens. 2019;37:1927-1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Werneck AO, Oyeyemi AL, Gerage AM, et al. Does leisure-time physical activity attenuate or eliminate the positive association between obesity and high blood pressure? J Clin Hypertens. 2018;20:959-966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice. J Am Coll Cardiol. 2018;71(6):1269-1324. [DOI] [PubMed] [Google Scholar]
- 23. Whelton PK, He J, Appel LJ, et al. Primary prevention of hypertension: clinical and public health advisory from the National High Blood Pressure Education Program. JAMA. 2002;288:1882-1888. [DOI] [PubMed] [Google Scholar]
- 24. Wiles JD, Coleman DA, Swaine IL. The effects of performing isometric training at two exercise intensities in healthy young males. Eur J Appl Physiol. 2010;108:419-428. [DOI] [PubMed] [Google Scholar]
- 25. Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. J Hypertens. 2018;36:1956-2041. [DOI] [PubMed] [Google Scholar]
- 26. World Health Organization. A Global Brief on Hypertension: Silent Killer, Global Public Health Crisis. Geneva, Switzerland: World Health Organization; 2013. [Google Scholar]
- 27. World Health Organization. Global Status Report on Noncommunicable Diseases 2014. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]