Abstract
Study Design:
Retrospective cohort study.
Objectives:
Discectomy alone or discectomy with fusion have been 2 polarized options in the management of large lumbar disc herniations presenting with leg-dominant pain in young patients. The objective of the study was to evaluate the outcomes of discectomy in young patients with large central lumbar disc herniation (CLDH) presenting with predominant leg pain.
Material and Methods:
Young patients (<45 years) presenting with predominant leg pain and MRI confirmed diagnosis of CLDH between April 2007-January 2017 were included in the study. All patients underwent tubular microdiscectomy. Outcomes of surgery were evaluated using visual analogue score (VAS) for leg and back pain, Oswestry Disability Index (ODI), and Macnab’s criteria.
Results:
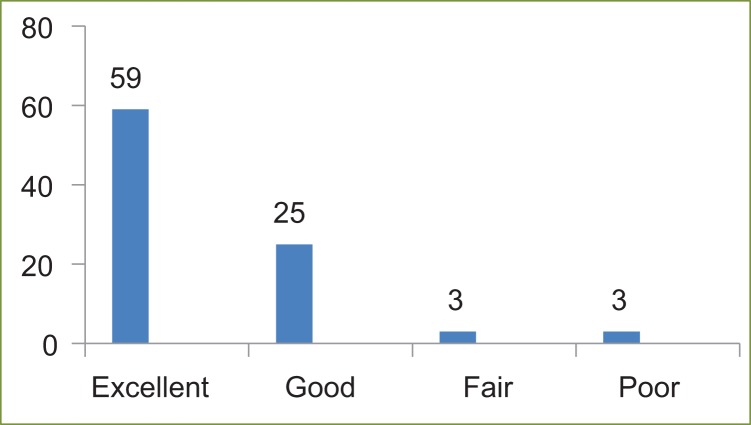
Ninety patients fulfilled the inclusion criteria. The mean age of patients was 34.9 years (range 19-45 years). Mean follow-up was 5.09 years (range 2-10 years). The incidence of CLDH in young adults was 30% and incidence among all “operated” lumbar disc herniations was 15.9%. The mean VAS for leg pain improved from 7.48 ± 0.9 to 2.22 ± 0.84 (P < .05) and the mean ODI changed from 60.53 ± 7.84 to 18.33 ± 6.20 (P < .05). Fifty-nine patients (65.6%) reported excellent, 25 patients (27.8%) reported good, 3 patients each (3.3%) as fair and poor outcomes respectively.
Conclusion:
Discectomy alone for CLDH with predominant leg pain is associated with high success rate and low need for a secondary surgical procedure. Patient selection in terms of leg-dominant pain may be the main attribute for lower incidence of recurrence, postoperative back-pain, and instability needing a secondary procedure. Minimally invasive discectomy may provide an added advantage of preserving normal spinal anatomy, thus minimizing the need for primary spinal fusion in these patients.
Keywords: central lumbar disc herniation (CLDH), lumbar disc herniation, tubular microdiscectomy, minimally invasive spine surgery, spine surgery, microdiscectomy, sciatica
Introduction
Central lumbar disc herniation (CLDH) is defined as a disc protrusion, extrusion or sequestration with the apex located in the midline of the spinal canal with a maximum deviation of the apex from the midline of 10% to each side.1 There are no clear definitions of large central disc herniations based on canal cross-section diameter. The closest definition and description has been attempted by Barlocher et al.1 These authors have categorized them into extrusion or sequestration of disc occupying more than 50% of the sagittal intraspinal diameter and contained central herniation occupying less than 50%.1 The other closer definition have been provided by Fardon et al2 under NASS (North American Spine Society) guidelines.2 The large central disc herniations belong to the “Central Zone” as per the descriptions of disc fragment migration in terms of anatomical landmarks.2
CLDHs have certain unique and controversial features. The incidence of CLDH is lower than the more common posterolateral herniations.1 Central lumbar disc herniations have varied presentations, are nonresponsive to conservative management and in due course require surgery for satisfactory results.3 Although a universal phenomenon; interestingly there is limited literature with regard to the description and optimal surgical options for CLDH. The guidelines for patients presenting with predominant back pain or predominant leg pain are different.4 Discectomy alone or discectomy with fusion is still a matter of controversy for such large herniated discs.5 Multiple surgical approaches have been described for retrieval of the disc fragments.1,6-8
Postoperative outcomes of CLDH is not only poorer than the other more common forms of disc herniation, but they also differ remarkably among different studies.1,6-8 This could be due to varied inclusion and exclusion criteria and varied treatment options, making it a mixed bag where oranges were compared with apples. Maybe there is a need for classification of patients with CLDH based on their dominant presenting symptoms and the delineation of factors associated with poor outcomes. These factors may differ in patients with back-dominant and leg-dominant pain and if so, can be considered while deciding surgical approach. In patients with lumbar disc herniations presenting with leg-dominant pain, tubular microdiscectomy has consistently proven to be an effective surgery.9,10 However, literature supporting the feasibility and outcomes of tubular microdiscectomy for large CLDH is negligible.
The aim of this study was to evaluate the clinical outcomes of discectomy in young patients suffering from CLDH with predominant leg pain.
Materials and Methods
This retrospective study was conducted in a single tertiary-care institution. All patients that were operated for CLDH between April 2007 and January 2017 were reviewed. The inclusion criteria for patients in this study were (1) young adults (<45 years) presenting with predominant leg pain (radicular symptoms), (2) flexion dominant pain (sitting/bending forward), (3) with or without associated back pain (nondominant), (4) magnetic resonance imaging (MRI) confirmed diagnosis, and (5) minimum 2-year follow-up.
The exclusion criteria included: (1) predominant back pain with or without radicular symptoms, (2) associated stenosis and segmental instability as predominant cause of pain as determined by preoperative clinical and radiological assessment, (3) extension-dominant pain (neurogenic claudication), (4) cases with multilevel disc involvement, recurrent disc herniation and previous surgery of lumbar spine.
The study is approved by institutional review board (approval vide BHIRB7840), Bombay Hospital and Medical Research Centre.
In all cases, the MRIs were analyzed by the lead author and certified radiologist. Central disc herniation type was categorized as described by Barlocher et al.1
Operative Approach
The lead author operated on all patients of CLDH. The patient was positioned on a radiolucent table in prone position with bolsters below the chest and the iliac crest keeping the abdomen free, head end raised, and pressure points well padded. The surgeon stood on the side of patient’s presenting symptoms; in cases with bilateral symptoms surgeon stood on the side with more severe symptoms. All patients were approached unilaterally. Using lateral fluoroscopy imaging, on the ipsilateral side, a 20G spinal needle was inserted all the way down till the lamina or the interlaminar space, such that the trajectory of the needle bisected the involved disc space. The needle was inserted 0.8 to 1 cm lateral to the midline. Once the location was confirmed on the image intensifier, 10 cm3 of diluted bupivacaine 0.5% was injected to provide preemptive analgesia. A 2-cm long (for the 18-mm METRX tube) or a 1.8-cm long (16-mm tube) vertical incision was then taken over the skin centered over the spinal needle. Gradual dilation of the intermuscular plane was then conducted using the serial dilators of increasing diameters. The respective tubular retractor was docked at the involved disc space and secured with the flexible-arm assembly system and the precise localization was confirmed with the image intensifier (Figure 1). The procedure was performed using an operating microscope. After clearing the soft tissues, laminotomy and flavectomy were performed. Nerve root was identified and mobilized to expose the herniated disc. Removal of the herniated disc was performed using disc forceps and the nerve root was freed all around using a nerve hook and Penfield dissector. Annulotomy was done in cases of contained herniations; the disc space was then probed using a nerve hook and the herniated fragments retrieved. As per the requirements of a particular case, based on the symptomatology and the MRI location of the fragments, the opposite side (by gradually wanding the tubular retractor) axilla as well as the shoulder of the nerve root and the anterior aspect of the dura was probed for hidden fragments. The surgical wound was then closed in 2 layers with absorbable sutures after removal of the tubular retractor and adequate hemostasis. All patients were mobilized after 4 to 6 hours of extubation. Patients were discharged on postoperative day 1.
Figure 1.
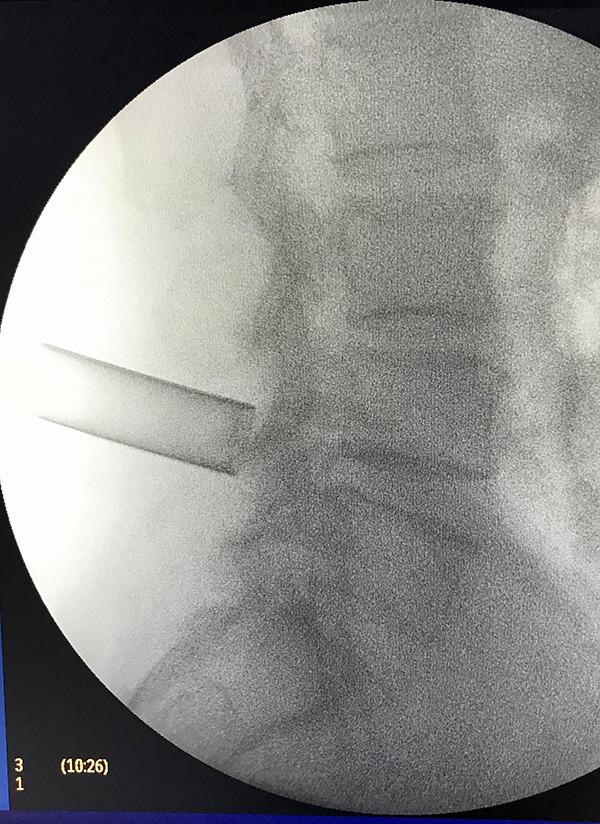
An 18-mm tube docked at L4-L5 level.
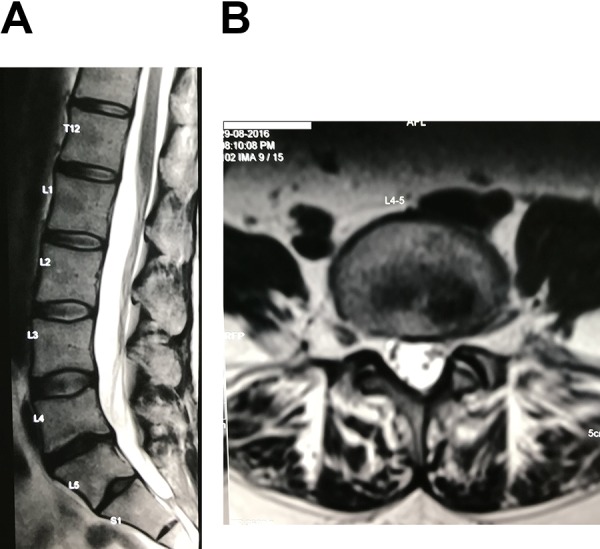
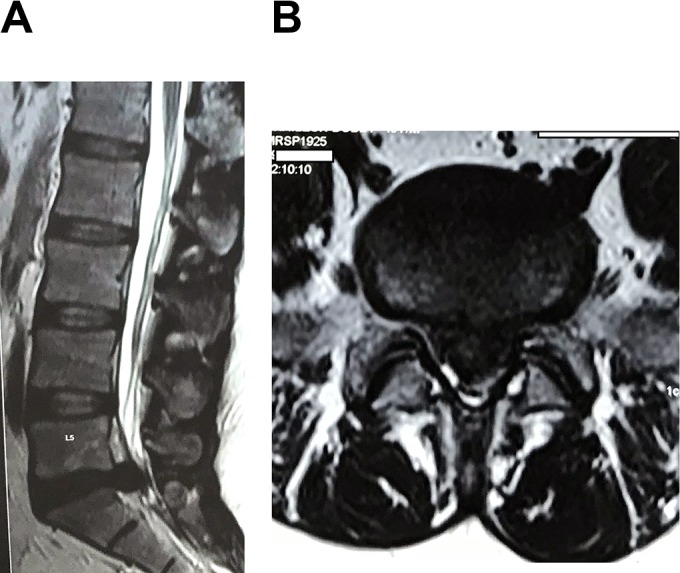
Figure 2a and b shows the sagittal and axial images, respectively, of 37-year-old woman with L4-L5 CLDH. Figure 3a and b shows the postoperative sagittal and axial images, respectively, of the same patient. Figure 4a and b shows the sagittal and axial images, respectively, of a 34-year-old male patient with L5-S1 CLDH with near complete obliteration of spinal canal.
Figure 2.
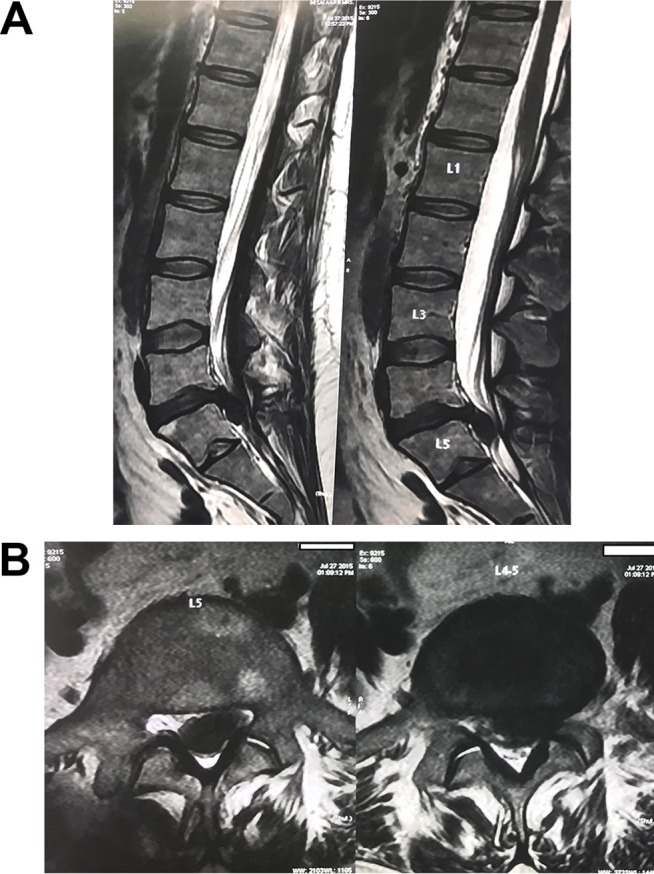
(a) Sagittal magnetic resonance image (MRI) of a 37-year-old woman with L4-L5 caudally migrated central lumbar disc herniation (CLDH). (b) Axial MRI of same patient showing large central disc herniation.
Figure 3.
(a) Postoperative sagittal magnetic resonance image (MRI) of the same patient as in Figure 1. (b) Postoperative axial MRI of the same patient showing adequate decompression and complete removal of herniated fragment.
Figure 4.
(a) Sagittal magnetic resonance image (MRI) of a 34-year-old man with L5-S1 central lumbar disc herniation (CLDH). (b) Axial MRI of the same patient showing central disc herniation nearly obliterating the spinal canal.
Outcome Measures
The patients were followed up at intervals of 1 week, 6 weeks, 3 months, 6 months, 12 months, 2 years, and every year thereafter. The patients were assessed by visual analogue scale (VAS) for leg pain, VAS for back pain, and Oswestry Disability Index (ODI) questionnaire. Statistical analysis was performed to examine interobserver reliability. Cohen’s kappa statistic test was 0.889 for the 2 examiners, which demonstrated high reproducible accuracy in categorizing central disc herniation on MRI. Continuous variables are expressed using mean and standard deviation. Kolmogorov-Smirnov test was used as test for normality. VAS for leg pain and ODI scores followed normal distribution of data; hence, paired t test was used to test the statistical significance of the change in the mean values of pre- and postoperative parameters. VAS for back pain did not fall under the normal distribution of data, hence Wilcoxon signed rank test was used. All statistical analysis was performed using IBM SPSS software version 20.0. A probability value of P < .05 was considered statistically significant.
Results
Ninety patients fulfilled our inclusion criteria. Two patients presented with cauda equina syndrome and 1 with foot drop. The mean age of patients was 34.9 years (range 19-45 years) and the male to female ratio was 1.6:1. Mean body mass index of our patients was 23.82 kg/m2 (range 21-27.6 kg/m2) (Table 1). Mean follow-up was 5.09 years (range 2-10 years). Mean duration of surgery was 50 minutes (range 20-90 minutes) and average blood loss was 30 mL (range 20-100 mL). Fifteen patients were lost to follow-up. The mean VAS scale for leg pain improved from 7.48 ± 0.9 to 2.22 ± 0.84 (P < .05), mean VAS scale for back pain improved from 3.90 ± 1.07 to 2.40 ± 1.17 (P < .05). The mean ODI scores changed from 60.53 ± 7.84 to 18.33 ± 6.20 (P < .05) (Table 2). Paired-sample t test and Wilcoxon signed rank tests were used to compare the variability in range of follow-up of patients and it yielded statistically significant results (Tables 3 and 4).
Table 1.
Demographics and Descriptive Characteristics of the Study Cohort.
| Patient demographics | N = 90 |
|---|---|
| Male:female | 1.6 (55):1 (35) |
| Age, years, mean (range) | 34.9 (19-45) |
| BMI, kg/m2, mean (range) | 23.82 (21-27.6) |
| Follow-up, years, mean (range) | 5.09 (2-10) |
| Level of disc herniation | |
| L3-L4 | 5 |
| L4-L5 | 51 |
| L5-S1 | 34 |
| Preoperative neurological deficits | 3 (2 CES; 1 foot drop) |
| Intraoperative complications | Incidental durotomy (n = 4) |
| Reoperation rates | 3.3% (n = 3) |
Abbreviation: BMI, body mass index; CES, cauda equina syndrome.
Table 2.
Mean Preoperative and Postoperative VAS (leg and back), ODI Scores, and P Values.
| Preoperative, Mean (SD) [95% CI] | Postoperative, Mean (SD) [95% CI] | P | |
|---|---|---|---|
| VAS (leg pain) | 7.48 (0.9) [7.113-7.853] | 2.22 (0.84) [1.88-2.56] | <.05 |
| VAS (back pain) | 3.90 (1.07) [3.469-4.33] | 2.40 (1.17) [1.93-2.87] | <.05 |
| ODI scores | 60.53 (7.84) [57.35-63.70] | 18.33 (6.20) [15.82-20.84] | <.05 |
Abbreviations: VAS, visual analogue score; ODI, Oswestry disability index; SD, standard deviation; CI, confidence interval.
Table 3.
Mean Difference in Preoperative to Postoperative Scores and P Value.
| Paired-Samples Test | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Paired Differences | t | df | Significance (2-tailed) | ||||||
| Mean | SD | SEM | 95% CI of the Difference | ||||||
| Lower | Upper | ||||||||
| Pair 1 | VAS leg (preop) − VAS leg (postop) | 5.258 | .924 | .098 | 5.064 | 5.453 | 53.715 | 89 | .000 |
| Pair 2 | ODI (preop) − ODI (postop) | 41.820 | 10.098 | 1.070 | 39.693 | 43.947 | 39.071 | 89 | .000 |
| Pair 3 | VAS back (preop) − VAS back (postop) | 1.371 | 1.004 | .106 | 1.159 | 1.582 | 12.876 | 89 | .000 |
Abbreviations: VAS, visual analogue score; ODI, Oswestry disability index; preop, preoperative; postop, postoperative; SD, standard deviation; SEM, standard error of the mean; CI, confidence interval.
Table 4.
Mean Improvement in VAS for Back Pain Scores and P Values
| Ranks | ||||
|---|---|---|---|---|
| N | Mean Rank | Sum of Ranks | ||
| VAS back (postop) − VAS back (preop) | Negative ranks | 80a | 42.11 | 3327.00 |
| Positive ranks | 4b | 39.75 | 159.00 | |
| Ties | 6c | |||
| Total | 90 | |||
| Test Statisticsd | ||||
| VAS Back (Postop) − VAS Back (Preop) | ||||
| Z | −7.365e | |||
| Asymptotic significance (2-tailed) | .000 | |||
Abbreviations: VAS, visual analogue score; preop, preoperative; postop, postoperative.
a VAS back (postop) < VAS back (preop).
b VAS back (postop) > VAS back (preop).
c VAS back (postop) = VAS back (preop).
d Wilcoxon signed rank test.
e Based on positive ranks.
Patient Satisfaction
Fifty-nine patients (65.6%) reported as excellent, 25 patients (27.8%) reported good, 3 patients (3.3%) reported as fair, and 3 patients (3.3%) as poor outcomes as per Macnab’s criteria (Figure 5). Overall, 93.4% had satisfactory outcome. Neurologically affected patient with foot drop improved completely and patients with cauda equina improved significantly in terms of useful muscle power and bladder and bowel continence. Patients with poor outcome (3.3%) required a secondary surgical procedure in terms of fusion.
Figure 5.
Clinical outcomes according to Macnab’s criteria.
Complications
There were 4 cases of incidental dural tear in the series and all were minor tears. These tears were managed successfully by masterly inactivity and watertight closure (due to inherent quality of technique there is no dead space formation to encourage collection of cerebrospinal fluid).
Discussion
The surgical management of lumbar disc herniations is dictated by various factors such as (1) symptomatology, (2) morphological location, as well as (3) the technical capability of the ease or difficulty of accessing the herniated fragment/s. In terms of symptomatology, while there are no strict guidelines, generally “leg-dominant pain” is successfully managed with discectomy.4,11 This is generally the treatment of choice with the more common “posterolateral herniations.” However, in a patient with “leg-dominant pain,” the situation becomes complicated in cases with large central disc herniations because factors (2) and (3) come into play. Morphologically, central large herniations are associated with higher incidences of recurrence, postoperative instability and low back pain and this is related to the associated larger annular defect as well large void created in the anterior column.1,6,7,12 Hence, there is a tendency to perform discectomy and interbody fusion in such cases.4 Again, technical difficulty in decompression of the nerve roots and the dural sac in the presence of large central disc herniations that occupy a large part of the spinal canal may lay foundation for a more aggressive step such as a facetectomy to avoid dural and neurological injuries. Such a situation would dictate a fusion procedure at the same time of discectomy in the fear of seeding post-operative instability.
Interestingly, apart from Barlocher at al,1 studies devoted to large central disc herniation are very few in literature. Studies related to outcomes of central large herniations are a mixed bag without any emphasis on symptomatology.1,6-8 The results of discectomy in these studies are associated with a low satisfaction rate.1,6-8 This could be a result of varied inclusion criteria in these studies. Patients with CLDHs present variedly with unilateral/bilateral radicular symptoms with or without back pain and few present with features of cauda equina syndrome.1,6-8 Surgical management options have ranged from discectomy with unilateral/ bilateral laminotomy or central laminotomy, hemilaminectomy, laminectomy and segmental fusion.1,6-8 There is still a lack of consensus on the appropriate surgical approach. Even the incidence in these studies varies widely.1,6-8
In the current study, the frequency of CLDH in young adults was 30% and incidence was 15.9% of all “operated’’ lumbar disc herniations over a period of 10 years across all the age-groups. The cutoff age of 45 years was considered to include only the younger adults who would probably lie in the first 2 stages (“disc degeneration” and “phase of instability”) of the Kirkaldy-Willis theory of disc degeneration.13 This group (<45 years) would be a challenge to treat with discectomy alone, especially in the presence of large herniations, without rendering the segment unstable and manifestation of its consequences. On the contrary, subject >45 years of age would probably have reached the “stabilization phase” and the resultant segmental stability would naturally protect the segment from complications such as recurrence, postoperative instability and back pain. This study evaluated the outcomes of discectomy in patients with CLDH presenting with “predominant leg pain” only.
Successful postoperative outcome in the current study was 93.4%. Successful postoperative surgical outcome in the previously published series ranged from 18% to 68%.1,6-8 McGuire and Amundson7 reported successful outcome in only 18% of patients using a central or bilateral laminotomy approach; moreover, 82% of their patients required a subsequent fusion procedure later. Knop-Jergas et al6 reported fair or poor postoperative outcomes in 52% of patients by laminotomy/partial laminectomy with discectomy. Barlocher et al1 reported successful outcome in 68% of patients using unilateral or bilateral fenestration with discectomy. However, as discussed earlier, these studies1,6-8 are no proper comparison groups to evaluate the success rate, as they considered a mixed bag of patients with large central herniations without mentioning the predominant symptoms.
The need for distinction of “predominant leg pain” from “predominant back pain” is relevant clinically. The outer annulus and the posterior longitudinal ligament (PLL) are known to be richly innervated by nociceptive fibers.14 The higher recurrence rate in previous studies was attributed to large annular tears, annular incompetence, higher degree of the internal disc disruption and the destabilized PLL.6,12,15-18 Walker et al7 noted that persistent back pain in patients with CLDH was due to destabilized PLL leading to greater segmental instability. Hence, we assume that the sequence of higher disc disruption, large annular tear, and destabilized PLL associated with CLDH may be significant in patients presenting with predominant back pain as presenting complaint. However, this may not be the case with patients with predominant leg pain.
Recurrence of symptoms was seen in 6.6% (6 patients) of the current study population; three patients were managed conservatively and the rest (3.3%) required a secondary surgical procedure. The recurrence rate in this study is much lower as compared with previous studies1,6-8 and could be attributed mainly to appropriate selection of patients with predominant leg pain as well as the virtues of minimally invasive unilateral approach. This has been echoed in a previous study where Hussein et al19 noted excellent long-term outcomes using tubular microdiscectomy in large uncontained lumbar disc herniations and opined that tubular microdiscectomy preserves the anatomy of the spine without compromising its stability leading to decreased incidence of low back pain. Surgical violation in open lumbar discectomy with muscle and ligaments stripping, dissection, and excessive cauterization influence the stabilization and coordination system in the innervation area of the dorsal nerve roots of the spinal nerves, and could aggravate segmental instability and cause an incidence of 11% to 15% postoperative disabling low back pain.20-23
As noted in this study, not all CLDH are inherently unstable as described in the past. Treatment needs to be individualized according to the predominant complaints of the patient. One can achieve excellent outcomes with discectomy alone (with proper patient selection) and can avoid more invasive and expensive procedures like fusion. Tubular microdiscectomy is feasible and can adequately decompress large CLDH. With the added advantage of being a minimally invasive procedure and preservation of normal spine anatomy tubular microdiscectomy contributes to the successful outcome.
Although cost utility assessment was not a formal part of this study, the clinical and cost implications of performing a tubular microdiscectomy versus open discectomy/fusion for the same indication warrants discussion. In this study using the outlined selection criteria, the majority of patients underwent a day surgery procedure. The advantages of tubular microdiscectomy over conventional discectomy include smaller incisions, lesser tissue trauma, better cosmesis, early ambulation, lesser postoperative pain, lesser blood loss, shorter hospital stay, shorter time to return to work, and thus lesser cost of treatment. Another measure of success of this technique is reflected by the patient’s ability to return early to the previous job. Foley and Smith24 reported a mean return to work time of 17.6 days proving its cost-effectiveness. The unit’s protocol is to allow patients to resume work after 2 weeks following surgery.
Limitations of the Study
An ideal study would have been to analyze the outcomes of discectomy in all situations, irrespective of whether the pain is predominantly in the back or the leg and then compare the outcomes. However, there have been studies done earlier on such sets of patients with a mixed bag of symptoms revealing poor outcomes. With the unit’s protocol for management of patients of CLDH with predominant back pain being discectomy and fusion (transforaminal lumbar interbody fusion), this study was designed to particularly assess the outcomes of discectomy in those patients of CLDH with predominant leg pain.
Conclusion
Discectomy alone for CLDH with predominant leg pain is associated with a high success rate and a low need for a secondary surgical procedure. Patient selection in terms of leg-dominant pain may be the main attribute for lower incidence of recurrence, postoperative back pain and instability needing a secondary procedure. Minimally invasive discectomy (tubular microdiscectomy) may provide an added advantage of preserving normal spinal anatomy and thus minimizing the need for primary spinal fusion in patients of CLDH with predominant leg pain.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Sandeep Tapashetti, MS (Ortho), DNB(Ortho)  https://orcid.org/0000-0003-0705-3319
https://orcid.org/0000-0003-0705-3319
References
- 1. Barlocher CB, Krauss JK, Seiler RW. Central lumbar disc herniation. Acta Neurochir (Wein). 2000;142:1369–1374. [DOI] [PubMed] [Google Scholar]
- 2. Fardon DF, Williams AL, Dohring EJ, Murtagh FR, Rothman SLG, Sze GK. Lumbar disc nomenclature: version 2.0: recommendations of the combined task forces of the North American Spine Society, the American Society of Spine Radiology and the American Society of Neuroradiology. Spine J. 2014;14:2525–2545. [DOI] [PubMed] [Google Scholar]
- 3. Sutheerayongprasert C, Paiboonsirijit S, Kuansongtham V, Anuraklekha S, Hiranyasthiti N, Neti S. Factors predicting failure of conservative treatment in lumbar-disc herniation. J Med Assoc Thai. 2012;95:674–680. [PubMed] [Google Scholar]
- 4. Wang JC, Dailey AT, Mummaneni PV, et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 8: lumbar fusion for disc herniation and radiculopathy. J Neurosurg Spine. 2014;21:48–53. [DOI] [PubMed] [Google Scholar]
- 5. Satoh I, Yonenobu K, Hosono N, Ohwada T, Fuji T, Yoshikawa H. Indication of posterior lumbar interbody fusion for lumbar disc herniation. J Spinal Disord Tech. 2006;19:104–108. [DOI] [PubMed] [Google Scholar]
- 6. Knop-Jergas BM, Zucherman JF, Hsu KY, DeLong B. Anatomic position of a herniated nucleus pulposus predicts the outcome of lumbar discectomy. J Spinal Disord. 1996;9:246–250. [PubMed] [Google Scholar]
- 7. Walker JL, Schulak D, Murtagh R. Midline disk herniations of the lumbar spine. South Med J. 1993;86:13–17. [DOI] [PubMed] [Google Scholar]
- 8. McGuire RA, Amundson GM. The outcome of surgically treated L4/5 central disc herniation. Orthopaedic Association of the English-Speaking World: Combined Meeting. J Bone Joint Surg Br. 1992;74:280. [Google Scholar]
- 9. Wu X, Zhuang S, Mao Z, Chen H. Microendoscopic discectomy for lumbar disc herniation: surgical technique and outcome in 873 consecutive cases. Spine (Phila Pa 1976). 2006;31:2689–2694. [DOI] [PubMed] [Google Scholar]
- 10. Garg B, Nagraja UB, Jayaswal A. Microendoscopic versus open discectomy for lumbar disc herniation: a prospective randomised study. J Orthop Surg (Hong Kong). 2011;19:30–34. [DOI] [PubMed] [Google Scholar]
- 11. Dewing CB, Provencher MT, Riffenburgh RH, Kerr S, Manos RE. The outcomes of lumbar microdiscectomy in a young, active population: correlation by herniation type and level. Spine (Phila Pa 1976). 2008;33:33–38. [DOI] [PubMed] [Google Scholar]
- 12. Carragee EJ, Han MY, Suen PW, Kim D. Clinical outcomes after lumbar discectomy for sciatica: the effects of fragment type and annular competence. J Bone Joint Surg Am. 2003;85:102–108. [PubMed] [Google Scholar]
- 13. Kirkaldy-Willis WH, Farfan HF. Instability of lumbar spine. Clin Orthop Relat Res. 1982;(165):110–123. [PubMed] [Google Scholar]
- 14. Crock HV. Observations on the management of failed spinal operations. J Bone Surg Br. 1976;58:193–199. [DOI] [PubMed] [Google Scholar]
- 15. Ohshima H, Hirano N, Osada R, Matsui H, Tsuji H. Morphologic variation of lumbar posterior longitudinal ligament and the modality of disc herniation. Spine (Phila Pa 1976). 1993;18:2408–2411. [DOI] [PubMed] [Google Scholar]
- 16. Loughenbury PR, Wadhwani S, Soames RW. The posterior longitudinal ligament and peridural (epidural) membrane. Clin Anat. 2006;19:487–492. [DOI] [PubMed] [Google Scholar]
- 17. Wiltse LL, Fonseca AS, Amster J, Dimartino P, Ravessoud FA. Relationship of the dura, Hofmann’s ligaments, Batson’s plexus, and a fibrovascular membrane lying on the posterior surface of the vertebral bodies and attaching to the deep layer of the posterior longitudinal ligament. An anatomical, radiologic, and clinical study. Spine (Phila Pa 1976). 1993;18:1030–1043. [DOI] [PubMed] [Google Scholar]
- 18. Daghighi MH, Pouriesa M, Maleki M, et al. Migration patterns of herniated disc fragments: a study on 1,020 patients with extruded lumbar disc herniation. Spine J. 2014;14:1970–1977. [DOI] [PubMed] [Google Scholar]
- 19. Hussein M, Abdeldayem A, Mattar MM. Surgical technique and effectiveness of microendoscopic discectomy for large uncontained lumbar disc herniations: a prospective, randomized, controlled study with 8 years of follow-up. Eur Spine J. 2014;23:1992–1999. [DOI] [PubMed] [Google Scholar]
- 20. Lewis PJ, Weir BKA, Broad RW, et al. Long-term prospective study of lumbosacral discectomy. J Neurosurg. 1987;67:49–54. [DOI] [PubMed] [Google Scholar]
- 21. Salenius P, Laurent LE. Results of operative treatment of lumbar disc herniation. A survey of 886 patients. Acta Orthop Scand. 1977;48:630–634. [DOI] [PubMed] [Google Scholar]
- 22. Weber H. Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine (Phila Pa 1976). 1983;8:131–140. [PubMed] [Google Scholar]
- 23. Hanley EN, Jr, Shapiro DE. The development of low-back pain after excision of a lumbar disc. J Bone Joint Surg Am. 1989;71:719–721. [PubMed] [Google Scholar]
- 24. Perez-Cruet MJ, Foley KT, Isaacs RE, et al. Microendoscopic lumbar discectomy: technical note. Neurosurgery. 2002;51(5 suppl):S129–S136. [PubMed] [Google Scholar]