In critically ill mechanically ventilated patients, ventilator-associated pneumonia (VAP) is the most common iatrogenic pulmonary infection. Diagnosis of VAP is challenging, potentially leading to delayed treatment or overuse of antimicrobials [1]. The impact of VAP on clinical outcomes has been thoroughly investigated [2], but remains a matter of controversy. Indeed, various trials that showed reduction of VAP failed to demonstrate improved clinical outcomes. In addition, the association between VAP and mortality is uncertain, since risk of VAP is time-dependent and patient needs to survive at least until VAP onset, limiting clear extrapolation of mortality risks. Studies attempting to control for these confounding biases have demonstrated VAP attributable mortality slightly higher than 10% [3]. Irrespective of methodological limitations, substantial body of evidence has been produced in this field and a questionable drive to achieve zero-VAP rates has grown in the past decade. This editorial provides a critical viewpoint on the zero-VAP contradiction, and summarizes controversies surrounding pharmacological and non-pharmacological interventions to reduce VAP rates.
Zero-VAP
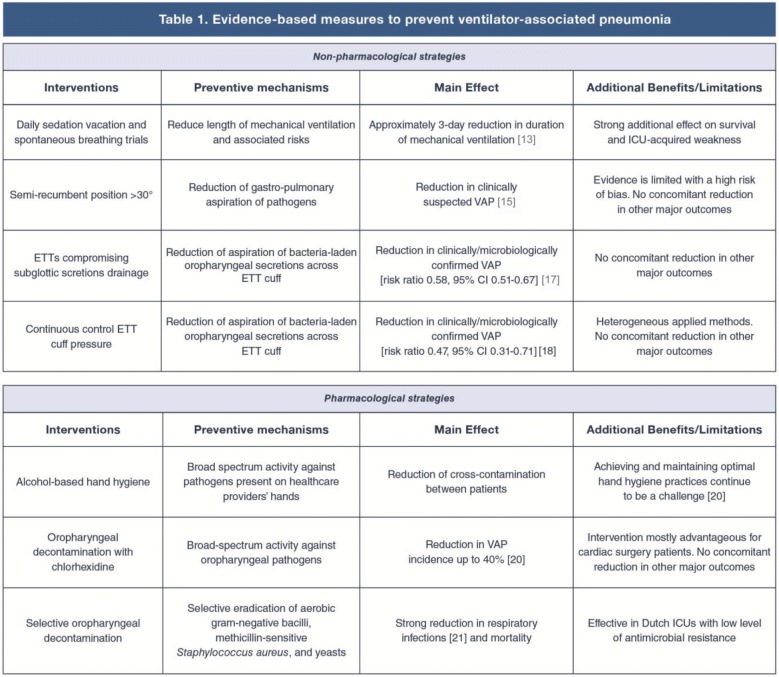
VAP has been increasingly considered as a fully preventable iatrogenic complication and used for benchmark and quality measure, in the context of pay-for-performance programs. This has led to overemphasized reduction in VAP incidence, specifically in North America. Indeed, in the latest National Healthcare Safety Network report, VAP rates between 0 and 4 per 1000 ventilation-days were described [4], while around the same period, Europeans were reporting an incidence density higher than 8 [5]. International administrators and healthcare policy makers strongly endorsed the “zero-VAP” approach, motivating nation-wide efforts [6], but overlooking its fundamental limitations. First, several promising interventions that reduced VAP risks, did not concurrently curtail secondary outcomes or even use of antibiotics (Table 1), questioning their clinical impact. Second, reliable and accurate diagnostic methods are crucial to corroborate eradication of a preventable disease. To date, a gold-standard to diagnose VAP is still inaccessible and we rely on multiple unspecific assays to score the risk of VAP. The newly proposed definitions of VAP, namely infection-related ventilator condition [8], did not noticeably improve accuracy of VAP diagnosis [7]. This results in easy manipulation of surveillance figures [8], specifically when quality standards or accreditations are needed. More importantly, diagnostic hurdles raise legitimate concerns on the overall evidence in this field of investigation. Indeed, substantial reduction of VAP has been frequently demonstrated by single-centre studies, using before–after designs, heterogeneous diagnostic methods and lacking concealment of interventions [9]. Finally, long-term implementation of strategies to avoid VAP is challenging, requires frequent monitoring of adherence and reinforcements, but even when methodically strategized, adherence rates not greater than 80% have been achieved [10], implying that sizeable compliance could be an unfeasible goal.
Table 1.
Evidence-based measures to prevent ventilator-associated pneumonia
ETT endotracheal tube, VAP ventilator-associated pneumonia, ICU intensive care unit, CI confidence interval
Preventive bundles
Various individual measures have proven efficacy in the prevention of VAP (Table 1), but when these measures are concomitantly applied, risks of VAP are further reduced. Meta-analyses on the implementation of VAP bundles showed that simple interventions, applied in a coordinated way as a part of a ventilator bundle care not only reduce VAP, but might also improve survival [11]. Nonetheless, as mentioned in previous paragraphs, those studies often applied inadequate methods and overlooked potential confounding factors, such as secular temporal trends in VAP incidence or regression to the mean. In addition, disagreement still exists on the most efficient and feasible bundle, since previous studies differed in the number and types of interventions, while it is known that individual components unequally impact outcomes [12].
Non-pharmacological measures
Endotracheal intubation is a main risk factor for VAP, since patients aspirate orogastric pathogens across the endotracheal tube (ETT) cuff, specifically when they are placed in the supine horizontal position. Therefore, reducing the time of intubation, through daily sedation vacation [13] and spontaneous breathing trials [14] are tenable preventive measures. Positioning the patient with the head of the bed elevated > 30° reduces aspiration and clinically confirmed VAP [15], but quality of evidence supporting this intervention is poor, and the optimal angulation of the head of the bed is still uncertain. The Gravity-VAP trial showed that the lateral-Trendelenburg position (LTP) could further reduce VAP, specifically in patients with healthy lungs upon intubation, but LTP feasibility appeared challenging [16]. To date, only ETTs comprising aspiration of subglottic secretions [17] reduced VAP by more than 50%, but substantial benefits were mostly corroborated in cardiac surgery patients. Avoiding ETT cuff deflation could further decrease pulmonary infections, as demonstrated by the use of devices that continuously control cuff pressure [18]; however, diverse machines have been used across available studies and consistent lack of benefits in secondary outcomes has been reported.
Pharmacological measures
It is firmly established that contact precautions, including hand hygiene with alcohol-based solutions, are pivotal in reducing transmission of drug-resistant pathogens [19]. These measures are endorsed by the most prominent international health agencies to reduce incidence of all nosocomial infections. Following endotracheal intubation, oropharyngeal flora shifts to a predominance of aerobic Gram-negative pathogens and Staphylococcus aureus. Thus, modulation of orogastric colonization has been a central strategy in the prevention of VAP. Various concentrations of chlorhexidine, up to 2%, have been used to hinder oropharyngeal growth of pathogens [20], specifically in cardiac surgery ICU patients. Importantly, in recent years, arguments have been raised against the use of chlorhexidine, due to associated increased mortality. These findings could be anecdotal or imply extensive pulmonary aspiration of chlorhexidine, specifically in patients in the semi-recumbent position; thus, experimental/clinical corroboration is needed. Several investigators have also recommended selective digestive or oropharyngeal decontamination (SDD/SOD) to maximize eradication of gastrointestinal Gram-negative bacteria. SDD/SOD have been principally applied in Dutch ICUs, with lower prevalence of multi-drug resistant pathogens. In those settings, SDD/SOD have consistently reduced incidence of respiratory infections [21] and mortality. Potential rebound colonization and increased antibiotic resistance have been a serious concern. Indeed, even in Dutch ICUs, rising ceftazidime resistance was documented. Interestingly, a recent study [22] evaluating SDD/SOD effects on bloodstream infections was conducted in ICUs with high prevalence of antibiotic-resistance. Mortality was not affected by the interventions, while antibiotic resistance did not vary throughout the study periods.
In conclusion, although a variety of studies have demonstrated reduction in VAP, certainty of evidence in this field of investigation is still limited, due to the lack of reliable diagnostic methods, disagreement on VAP burden and substantial inconsistency, heterogeneity and risk of bias of available studies. In conclusion, we call attention to the crucial need of innovative diagnostic markers and application of improved research methods to advance this field and precisely corroborate efficacy of interventions in reducing VAP.
Compliance with ethical standards
Conflicts of interest
Sebastiano Maria Colombo and Andrea Catalina Palomeque do not have conflict of interest related to this manuscript. Gianluigi Li Bassi, in the past 5 years, received grant funding, through his affiliated institution from Fisher and Paykel, Bayer AG and Theravance Biopharma.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Torres A, Niederman MS, Chastre J, et al. International ERS/ESICM/ESCMID/ALAT guidelines for the management of hospital-acquired pneumonia and ventilator-associated pneumonia: guidelines for the management of hospital-acquired pneumonia (HAP)/ventilator-associated pneumonia (VAP) of the European Respiratory Society (ERS), European Society of Intensive Care Medicine (ESICM), European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and Asociación Latinoamericana del Tórax (ALAT) Eur Respir J. 2017 doi: 10.1183/13993003.00582-2017. [DOI] [PubMed] [Google Scholar]
- 2.Rello J, Ollendorf DA, Oster G, et al. Epidemiology and outcomes of ventilator-associated pneumonia in a large US database. Chest. 2002;122:2115–2121. doi: 10.1378/chest.122.6.2115. [DOI] [PubMed] [Google Scholar]
- 3.Melsen WG, Rovers MM, Groenwold RH, et al. Attributable mortality of ventilator-associated pneumonia: a meta-analysis of individual patient data from randomised prevention studies. Lancet Infect Dis. 2013;13:665–671. doi: 10.1016/S1473-3099(13)70081-1. [DOI] [PubMed] [Google Scholar]
- 4.Dudeck MA, Weiner LM, Allen-Bridson K, et al. National Healthcare Safety Network (NHSN) report, data summary for 2012, device-associated module. Am J Infect Control. 2013;41:1148–1166. doi: 10.1016/j.ajic.2013.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martin-Loeches I, Povoa P, Rodríguez A, et al. Incidence and prognosis of ventilator-associated tracheobronchitis (TAVeM): a multicentre, prospective, observational study. Lancet Respir Med. 2015;3:859–868. doi: 10.1016/S2213-2600(15)00326-4. [DOI] [PubMed] [Google Scholar]
- 6.Álvarez-Lerma F, Palomar-Martínez M, Sánchez-García M, et al. Prevention of ventilator-associated pneumonia: the multimodal approach of the Spanish ICU “Pneumonia Zero” Program. Crit Care Med. 2018;46:181–188. doi: 10.1097/CCM.0000000000002736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Klein Klouwenberg PMC, van Mourik MSM, Ong DSY, et al. Electronic implementation of a novel surveillance paradigm for ventilator-associated events: feasibility and validation. Am J Respir Crit Care Med. 2014 doi: 10.1164/rccm.201307-1376OC. [DOI] [PubMed] [Google Scholar]
- 8.Magill SS, Klompas M, Balk R, et al. Developing a new, national approach to surveillance for ventilator-associated events. Crit Care Med. 2013;41:2467–2475. doi: 10.1097/CCM.0b013e3182a262db. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Klompas M. Is a ventilator-associated pneumonia rate of zero really possible? Curr Opin Infect Dis. 2012;25:176–182. doi: 10.1097/QCO.0b013e3283502437. [DOI] [PubMed] [Google Scholar]
- 10.Landelle C, Nocquet Boyer V, Abbas M, et al. Impact of a multifaceted prevention program on ventilator-associated pneumonia including selective oropharyngeal decontamination. Intensive Care Med. 2018;44:1777–1786. doi: 10.1007/s00134-018-5227-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pileggi C, Mascaro V, Bianco A, et al. Ventilator bundle and its effects on mortality among ICU patients. Crit Care Med. 2018;46:1167–1174. doi: 10.1097/CCM.0000000000003136. [DOI] [PubMed] [Google Scholar]
- 12.Klompas M, Li L, Kleinman K, et al. Associations between ventilator bundle components and outcomes. JAMA Intern Med. 2016;176:1277–1283. doi: 10.1001/jamainternmed.2016.2427. [DOI] [PubMed] [Google Scholar]
- 13.Kress JP, Pohlman AS, O’Connor MF, Hall JB. Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med. 2000;342:1471–1477. doi: 10.1056/NEJM200005183422002. [DOI] [PubMed] [Google Scholar]
- 14.Girard TD, Kress JP, Fuchs BD, et al. Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (awakening and breathing controlled trial): a randomised controlled trial. Lancet. 2008;371:126–134. doi: 10.1016/S0140-6736(08)60105-1. [DOI] [PubMed] [Google Scholar]
- 15.Wang L, Li X, Yang Z, et al. Semi-recumbent position versus supine position for the prevention of ventilator-associated pneumonia in adults requiring mechanical ventilation. Cochrane Database Syst Rev. 2016;1:CD009946. doi: 10.1002/14651858.CD009946.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li Bassi G, Panigada M, Ranzani OT, et al. Randomized, multicenter trial of lateral Trendelenburg versus semirecumbent body position for the prevention of ventilator-associated pneumonia. Intensive Care Med. 2017;43:1572–1584. doi: 10.1007/s00134-017-4858-1. [DOI] [PubMed] [Google Scholar]
- 17.Caroff DA, Li L, Muscedere J, Klompas M. Subglottic secretion drainage and objective outcomes: a systematic review and meta-analysis. Crit Care Med. 2016;44:830–840. doi: 10.1097/CCM.0000000000001414. [DOI] [PubMed] [Google Scholar]
- 18.Nseir S, Lorente L, Ferrer M, et al. Continuous control of tracheal cuff pressure for VAP prevention: a collaborative meta-analysis of individual participant data. Ann Intensive Care. 2015 doi: 10.1186/s13613-015-0087-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boyce JM. Current issues in hand hygiene. Am J Infect Control. 2019;47S:A46–A52. doi: 10.1016/j.ajic.2019.03.024. [DOI] [PubMed] [Google Scholar]
- 20.Klompas M. Oropharyngeal decontamination with antiseptics to prevent ventilator-associated pneumonia: rethinking the benefits of chlorhexidine. Semin Respir Crit Care Med. 2017;38:381–390. doi: 10.1055/s-0037-1602584. [DOI] [PubMed] [Google Scholar]
- 21.Liberati A, D’Amico R, Pifferi S, et al. Antibiotic prophylaxis to reduce respiratory tract infections and mortality in adults receiving intensive care. Cochrane Database Syst Rev. 2009 doi: 10.1002/14651858.CD000022.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wittekamp BH, Plantinga NL, Cooper BS, et al. Decontamination strategies and bloodstream infections with antibiotic-resistant microorganisms in ventilated patients: a randomized clinical trial. JAMA. 2018;320:2087–2098. doi: 10.1001/jama.2018.13765. [DOI] [PMC free article] [PubMed] [Google Scholar]