Abstract
Objectives
Other than age, diabetes is the largest contributor to overall healthcare costs and reduced life expectancy in Europe. This paper aims to more exactly quantify the net impact of diabetes on different aspects of healthcare provision in hospitals in England, building on previous work that looked at the determinants of outcome in type 1 diabetes (T1DM) and type 2 diabetes (T2DM).
Setting
NHS Digital Hospital Episode Statistics (HES) in England was combined with the National Diabetes Audit (NDA) to provide the total number in practice of people with T1DM/T2DM.
Outcome measures
We compared differences between T1DM/T2DM and non-diabetes individuals in relation to hospital activity and associated cost.
Results
The study captured 90% of hospital activity and £36 billion/year of hospital spend. The NDA Register showed that out of a total reported population of 58 million, 2.9 million (6.5%) had T2DM and 240 000 (0.6%) had T1DM. Bed-day analysis showed 17% of beds are occupied by T2DM and 3% by T1DM. The overall cost of hospital care for people with diabetes is £5.5 billion/year. Once the normally expected costs including the older age of T2DM hospital attenders are allowed for this fell to £3.0 billion/year or 8% of the total captured secondary care costs. This equates to £560/non-diabetes person compared with £3280/person with T1DM and £1686/person with T2DM. For people with diabetes, the net excess impact on non-elective/emergency work is £1.2 billion with additional estimated diabetes-related accident & emergency attendances at 440 000 costing the NHS £70 million/year. T1DM individuals required five times more secondary care support than non-diabetes individuals. T2DM individuals, even allowing for the age, require twice as much support as non-diabetes individuals.
Conclusions
This analysis shows that additional cost of provision of hospital services due to their diabetes comorbidities is £3 billion above that for non-diabetes, and that within this, T1DM has three times as much cost impact as T2DM. We suggest that supporting patients in diabetes management may significantly reduce hospital activity.
Keywords: general diabetes, health economics, public health, hospital
Strengths and limitations of the study.
We were able to look at national level data across nearly 5500 general practitioner practices in relation to hospital activity. The analysis covered more than 90% of hospital costs in England.
Any conclusions drawn must account for the fact that our findings are based on association, not definite causation.
Inherent in this real-world analysis methodology are potential confounding factors that are inherent in any retrospective study. Nevertheless, our design was such as to minimise the potential impact of such factors.
INTRODUCTION
Other than age, diabetes is the largest contributor to overall healthcare costs and reduced life expectancy in Europe.1 People with type 1 (T1DM) and type 2 (T2DM) diabetes require much higher levels of hospital support than their non-diabetes counterparts. Healthcare provision in hospital can be broken down into four main areas: (1) planned/elective including day-case admissions (Planned), (2) emergency/non-elective admissions (Emergency), (3) accident & emergency (A&E) attendances and (4) outpatient consultations/attendances (Outpatient). Each of these different classes must be managed appropriately by clinicians and hospital administrators, and the relevance of diabetes to this planning may be different.
The National Diabetes Inpatient Audit2 has shown that 18% of all hospital beds on any 1 day are occupied by people who have a diagnosis of diabetes2 compared with a 7% prevalence of all diabetes in the adult population of England. This may significantly overstate the impact of the condition as over 90% of people with diabetes have T2DM, which generally occurs much later in life so that the cohort is significantly older than the general population—as such, their normal healthcare requirements would increase significantly with age.
NHS Digital publishes the general practitioner (GP) practice patient register split into age groups and can provide practice level extracts from Hospital Episode Statistics (HES) of the amount of different practice activities for people who have a recorded diagnosis of T1DM or T2DM and those that do not have such a diagnosis.3 The National Diabetes Audit (NDA) publishes the numbers and ages of people with either T1DM or T2DM in each practice4 also split into age groups. Other practice characteristics such as ethnicity, social deprivation and location are also publicly available.5
The NHS in England publishes a significant amount of data at a GP practice level and we have previously described the impact of a variety of population, service and prescribing factors on outcomes.6 7 We have previously looked at the determinants of outcome in T1DM and T2DM in GP practices in England.6 7 It was felt that this approach could be used to quantify and so adjust for the effect of age on different services that are provided in hospital to T2DM individuals and therefore achieve a much more accurate evaluation of the actual net cost of diabetes, including all associated comorbidities to the health service.
AIMS
This paper aims to more exactly quantify the net impact of diabetes on the different aspects of healthcare provision in hospitals in England.
At GP practice level, we took the allocation of the different elements of hospital costs associated with the diagnosis of either T2DM or T1DM while adjusting for the difference in the T2DM age profile from the general population. We wished to use this analysis to provide a clearer focus for diabetes services to determine which elements of care they can focus on, in order to improve outcomes. Specifically, we compared differences between T1DM/T2DM and non-diabetes individuals in relation to hospital activity and the associated costs.
METHODS
Individual patients who had a diagnosis of either T1DM or T2DM and their age and practice code were identified within the NHS Digital HES data for 2016_2017 and 2017_2018. The sum of annual activity of the different services, including emergency, elective, A&E and outpatient care, was then extracted from the NHS Digital HES for each general practice for all those patients with a diagnosis of T1DM or T2DM and the non-diabetes individuals in 2017_2018. Emergency and elective activity were shown as totals for the number of unique patients, admissions, overall bed-days and the total national tariff charged, while only the number of unique patients and total attendances were provided for outpatient and A&E activity. The completeness of data was checked by looking at the national totals for the year reported within the reference costs.
The actual total population of T1DM and T2DM individuals and their age groups at the GP practice level was taken from NHS Digital NDA.4 Public Health England publishes the patient numbers and age profile of each GP practice from this total. The age profile for non-diabetes patients was calculated by subtracting the total diabetes population.
The demographic and location data for each practice including social deprivation, population density (urban/rural), Latitude (Northerliness) were taken from the Office of National Statistics (ONS).5 The % minority ethnicity was also determined.
The total overall hospital costs for each practice in each of the three classes (T1DM, T2DM and non-diabetes) were calculated by adding the provided total elective and non-elective tariff charges to the Outpatient and Accident & Emergency attendances each multiplied by the national overall average cost/attendance taken from the 2017–2018 national reference costs.
For each of the T1DM, T2DM and non-diabetes population: Total Hospital Costs=Total recorded Elective Tariff Charges+Total recorded Non-Elective Tariff Charges+Total recorded Outpatient Attendances×Average annual Outpatient tariff cost/attendance+Total recorded Accident & Emergency attendances×average cost/attendance (both taken from the 2017–2018 national reference costs).
The number of practices included in the study was limited to those for which all the data sets were available plus if there were more than 200 T2DM patients or more than 20 T1DM patients on their register (5468 GP practices).
Practices that identify people earlier in the course of their T2DM increase their numbers and pro-rata this reduces the associated average hospital costs/person, to include for this a ‘T2DM %case identification’ factor was calculated. Our statistical model took account of this and linked the actual recorded T2DM register as % of the total practice population to the practice age, gender, ethnicity, social disadvantage, latitude and main long-term condition disease prevalence. Based on this statistical model, an expected level of T2DM could be predicted. The difference between the predicted and actual T2DM prevalence was taken as the local practice % case identification. This factor was not required for T1DM as the onset of that condition is more clearly delineated, so all people with this condition can be more easily identified.
Patient and public involvement statement
It was not appropriate or possible to involve patients or the public in this work given that we used general practice level summated data and related hospital outcome statistics.
Statistics
A stepwise multiple regression model was created using Excel with Analyse-it add-in linking as outcome level of hospital activity of each class/head of population for T1DM and T2DM at GP practice level to the:
The same measure for the non-diabetes population.
% of non-diabetes population age >75.
% of either T1DM or T2DM.
% case identification (T2DM).
Population density (pop/sq km)
% black and minority ethnicity (BME).
Practice size.
% prevalence of T2DM.
Latitude.
To remove the effect of the age difference between T2DM and non-diabetes population on the cost impact of diabetes, the regression coefficient was applied to the difference between % on patients over 75 in T2DM and the non-diabetes population, to give a ‘net’ T2DM disease impact on each of the activities and cost levels including:
Overall costs.
Emergency admissions, bed days and tariff.
Elective admissions, day case, bed days and tariff.
A&E attendances.
Outpatient attendances.
To highlight the impact of the condition, the activity/person for T1DM and T2DM was also shown as a ratio to the non-diabetes activity/person.
As diabetes can have many wide-ranging health impacts, establishing the overall additional all-cause hospital costs of diabetes on top of expected normal healthcare needs is difficult. Using a practice population-based approach allows us to allow for confounding factors such as age and disease identification. However, it remains a statistical analysis relying on large amounts of data entered during clinical treatments so it will contain normal administrative errors. Nevertheless, it is hoped that both the scale of these data capturing over 160 million episodes and as these errors can be either over or under-reported that the outcomes should correspond to the actual values.
RESULTS
The study (see table 1) captured around 90% of the hospital activity data for England in 2017/2018. The missing 10% could be explained by the difference in definitions between the different analyses (ie, outpatient attendances and episodes which include more than one attendance). The tariff difference between the reference known costs of hospital T1DM/T2DM management and extracted HES of just under £7 billion could relate to other commercial costs or activities not captured within the HES data extraction.
Table 1.
Data captured in study
| 2017_2018 | Reference costs | Extracted HES | Captured |
| Organisation providing returns | 152 | ||
| Bed days | 26 462 497 | 25 932 385 | 98% |
| Tariff charged | £26 219 369 965 | £19 392 269 892 | 74% |
| Outpatient attendance | 87 714 235 | 119 758 272 | 137% |
| A&E attendances | 19 950 458 | 20 737 416 | 104% |
A&E, accident & emergency; HES, Hospital Episode Statistics.
The NDA Register showed that out of a total population of 56 million in England, 2.9 million (6.5%) had T2DM and 270 000 (0.7%) had T1DM. The bed-day analysis confirmed that 17% of beds were occupied by T2DM and 3% by T1DM at a total of 20%, on average, of bed occupancy similar to that reported in the National Inpatient Audit.2
The National average reference 2017_2018 costs/event for both consultant and non-consultant-led outpatient appointments is £125/attendance.8 The national average reference costs for the variety of A&E attendances including all the activities were £160/attendance.8
Included into the study (table 2) were practices for which there was enough data and to reduce the impact of single hander practice outliers and decrease the variance only practices with more than 200 T2DM patients were included in the estimation of age impact. This removed 18% of practices and 6% of the T2DM population.
Table 2.
Scope of study
| 2017_2018 | Practices | Population | NDA T2 | NDA T1 | |||
| Total | 7255 | 59 005 024 | 2 914 825 | 243 090 | |||
| Complete data | 6676 | 92% | 55 924 632 | 95% | 2 835 540 | 97% | 236 025 |
| T2>200 | 5468 | 75% | 51 352 503 | 87% | 2 656 850 | 91% | |
NDA, National Diabetes Audit.
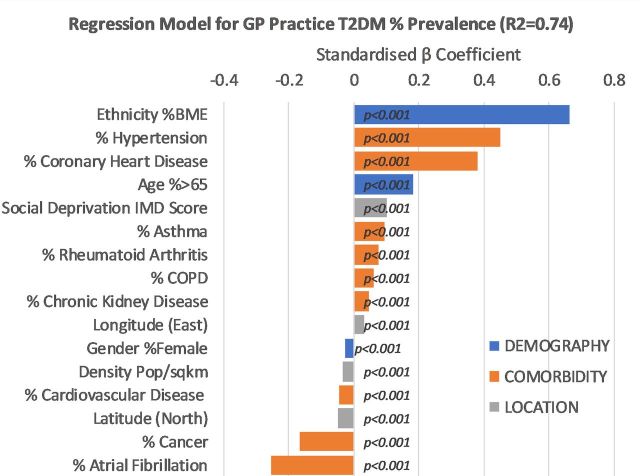
The results of the expected prevalence calculation are shown in figure 1. GP practices with a higher proportion of black and minority ethnicity (BME) ethnicity individuals, people with hypertension and coronary artery disease plus an older age profile had higher proportions of T2DM individuals. The statistical model based on these factors accounted for 74% of the variation in T2DM prevalence across GP practices in England. Higher proportions of BME individuals, individuals with a history of hypertension, coronary artery disease and aged 65 or over have the strongest association with higher T2D prevalence. A ‘T2DM Case Identification’ for each practice was then calculated from the actual prevalence of T2 divided by the expected value.
Figure 1.
T2DM identification. Statistical model linking % of T2DM to chosen practice factors. Factors contributing related to higher T2DM prevalence are on the right of the figure. BME, black and minority ethnicity; COPD, chronic obstructive pulmonary disease; GP, general practitioner; T2DM, type 2 diabetes.
Figure 2A shows the age profile (proportion at a particular age) of non-diabetes, T1DM and T2DM in the England general population. For T2DM, the age distribution is considerably different from the non-diabetes population, while the T1DM age distribution is close to the non-diabetes population. The figure also shows the proportion of over 65 within each of these diagnostic categories (T1DM, T2DM and non-diabetes) for hospital attendees. For hospital attendees, the proportion of admissions in the over 65 age for T2DM at 66% was much higher than for non-diabetes individuals at 22% and T1DM at 15%.
Figure 2.
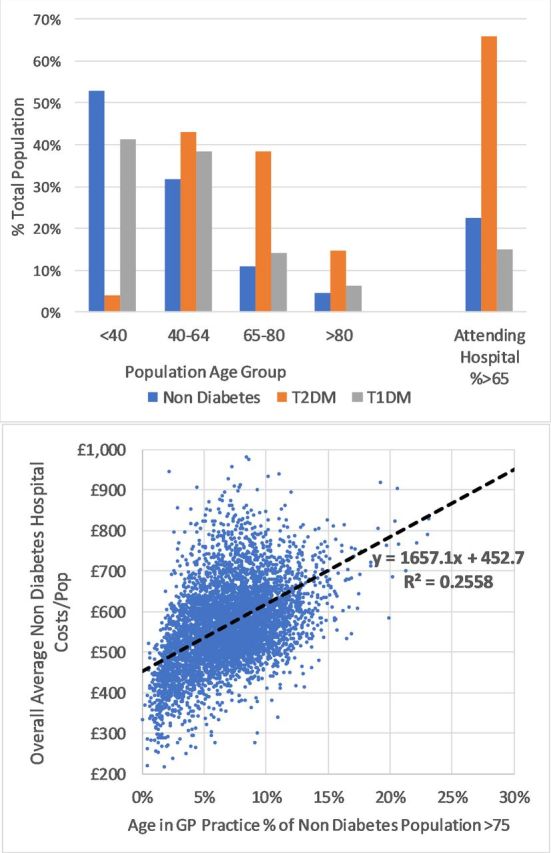
(A) Age distribution (proportion at a particular age) in the general population by diabetes type and proportion aged >65 years in hospital patients. (B) Impact in practices non-diabetes population of age% >75 years old on total hospital costs/non-diabetes population. GP, general practitioner; T1DM, type 1 diabetes; T2DM, type 2 diabetes.
The age profile data showed that across all GP practices in England, for non-diabetes, 7% of people were aged >75 years, and for people with T2DM, 26% were age >75 years old.
Figure 2B shows the variation of total hospital costs by the proportion of people on the GP list >75 years old. The univariate linear regression based on GP practice level total costs of hospital activity versus age profile of the practice shows that if 7% of people were aged >75 years in the GP practice, that the expected total non-diabetes population costs would be expected to be £568/person. However, if the figure was 26% of people aged >75 years, then the equivalent non-diabetes population costs would rise to £884/person. This univariant analysis suggests that the increased age of T2DM people accounts for up to £316/person of the cost difference.
Multivariate regression analysis for T2DM hospital costs
Figure 3A–3E shows the results from five of the multivariate regression models used to link the level of cost and activity/T2DM person to the main drivers from the practice and levels for the non-diabetes populations including the age of both non-diabetes and T2DM%>75.
Figure 3.
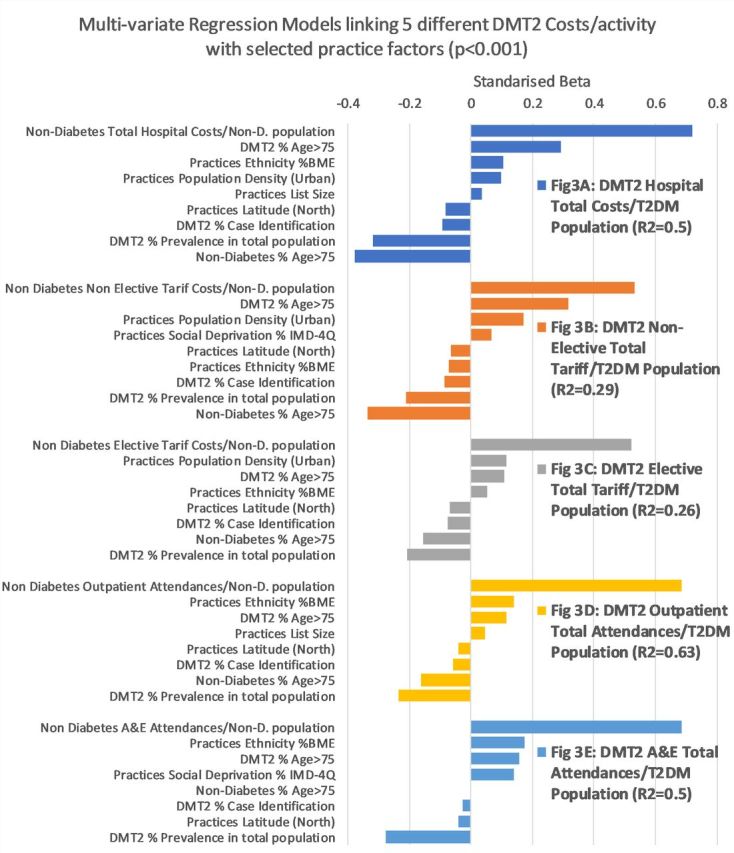
(A–E) The results from five multivariate regression models linking to selected practice factors for T2DM-related hospital activity. A&E, accident & emergency; BME, black and minority ethnicity; T2DM, type 2 diabetes.
Overall hospital costs/various practice populations were normally distributed with skew and kurtosis factors for non-DM=0.06 and 1.7; T2DM=0.8 and 2.2 and T1DM=1.6 and 2.7, mostly within the ±2 acceptable range.
The variation captured in each model was between 0.26 and 0.63. The regression analysis shows that the main driver for T2DM diabetes service costs and activity are as follows:
Equivalent service costs for the non-diabetes population.
Age%>75 of the T2DM population.
For the factors associated with lower T2DM hospital costs:
Prevalence %T2DM.
Age% >75 of the non-diabetes population.
T2DM% case identification.
Minor factors that had variable effects included:
Social deprivation.
Practice size.
T2DM prevalence.
%BME ethnicity.
Northerly latitude.
Population density (urban/rural).
Similar patterns were seen across hospital total costs, non-elective costs, elective costs, outpatient total attendances and A/E total attendances.
To extrapolate the level of the age effect contained within the T2DM activity and costs, the multiple regression coefficient for the proportion of T2DM individuals aged >75 years was taken for each measure from the analysis and applied to the difference between the T2DM value of 26% >75 years vs 7% of the non-diabetes population >75 years old. The age-related impact on T2DM total acute costs difference/person is £300/person. This was similar to the £316 calculated by the univariant analysis.
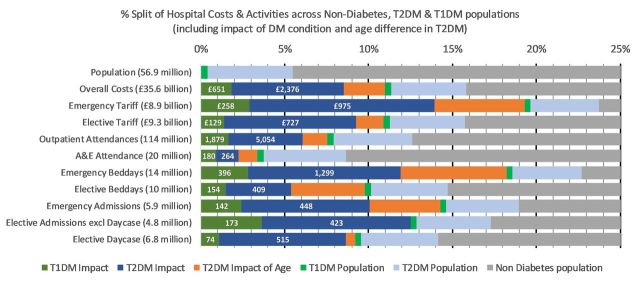
Figure 4 highlights the relation of the diagnosis of T1DM and T2DM with the percentage of total hospital activity. While the numbers of T1DM are 0.42% and T2DM are 5.06% of the total background population, having allowed for the normal needs and influence of age, the net diabetes impact as a condition is 8.5% of hospital costs of the NHS (T1DM 1.8%+T2 DM 6.7%). In making up this net total, 13.9% are for emergency costs (T1DM 2.9%+T2 DM 11%), 9.2% are for elective costs (1.4% T1DM+7.8% T2DM), 6% are for outpatient attendances (1.6%T1DM+4.4%T2 DM) and 2.2% are for A&E attendances (0.9% T1DM and 1.3% T2DM). Overall patients with diabetes are taking 19.3% of bed days, but after allowing for normal needs and age related, then the additional consumption is 11.9% of emergency beds (2.8%T1DM+9.1%T2 DM) and 5.4% elective beds (1.5%T1DM+3.9%T2 DM).
Figure 4.
Comparison of hospital activity between non-diabetes and T1DM (split by the impact of population and condition) and T2DM (split by impact population, age, and condition). A&E, accident & emergency; T1DM, type 1 diabetes; T2DM, type 2 diabetes.
Table 3 provides an overview of the costs of diabetes including the impact of age on T2DM. £35.6 billion/year of hospital spending is included in this analysis. This accounts for 66% of £53.7 billion total hospital income in England in 2017/2018, with the overall cost of hospital care for people with diabetes being £5.6 billion/year. Once the normally expected costs including the older age of T2DM, hospital attenders are allowed for this fell to £3.0 billion/year or 8% of the total captured secondary care costs. Of this, £0.65 billion or 21% of the age-adjusted diabetes spend came from the additional treatment provided to T1DM individuals who were only 8% of the total diabetes population. This equates to £560/non-diabetes person compared with £3280/person with T1DM and £1686/person with T2DM (of this £300 is associated with the age difference so the net impact on hospital costs is £826/person).
Table 3.
Results: The numbers and activities associated with 6791 GP practices that had provided both HES activity and NDA data
| Population,000 | Total | Non-diabetes | T1DM | T2DM | T2 age adjust | Net T1DM* | Net T2DM incl age | DM Imp† % Total |
T1 as % DM | Multiple of non-diabetes unit | |
| 56 915 | 53 796 | 239 | 2880 | T1 | T2 age adjusted | ||||||
| Hospital spend (£ million): | |||||||||||
| Non-elective tariff | £8859 | £6756 | £288 | £1815 | −£479 | £258 | £975 | 14% | 21% | 9.6 | 3.7 |
| Elective tariff | £9270 | £7809 | £164 | £1297 | −£140 | £129 | £739 | 9% | 15% | 4.7 | 2.8 |
| Outpatient (@£125 each) | £14 305 | £12 503 | £291 | £1511 | −£210 | £235 | £632 | 6% | 27% | 5.2 | 1.9 |
| A&E (@£160 each) | £3159 | £2885 | £42 | £232 | −£35 | £29 | £42 | 2% | 41% | 3.2 | 1.3 |
| TOTAL | £35 593 | £29 953 | £784 | £4855 | −£864 | £651 | £2388 | 9% | 21% | 5.9 | 2.5 |
| Admissions & bed days:,000 | |||||||||||
| Non-elective bed-days | 14 204 | 10 980 | 445 | 2779 | −892 | 396 | 1299 | 12% | 23% | 9.1 | 3.2 |
| Non-elective Adm‡ | 5853 | 4742 | 163 | 948 | −246 | 142 | 448 | 10% | 24% | 7.7 | 2.8 |
| Elective bed-days | 10 462 | 8924 | 194 | 1345 | −457 | 154 | 409 | 5% | 27% | 4.9 | 1.9 |
| Elective Adm ON§ | 4774 | 3949 | 191 | 635 | 17 | 173 | 441 | 13% | 28% | 10.9 | 3.1 |
| Elective Adm DC¶ | 6799 | 5858 | 74 | 866 | −37 | 48 | 515 | 8% | 9% | 2.9 | 2.6 |
| Length of stay (LOS) days: | % of Non-D | ||||||||||
| Non-elective LOS | 2.43 | 2.32 | 2.72 | 2.93 | 2.72 | 2.69 | 118% | 116% | |||
| Elective LOS | 2.19 | 2.26 | 1.01 | 2.12 | 1.01 | 1.36 | −55% | −40% | |||
| Attendances:,000 | |||||||||||
| Outpatient | 114 439 | 100 024 | 2324 | 12 091 | −1,682 | 1879 | 5054 | 6% | 27% | 4.8 | 1.9 |
| A&E | 19 742 | 18 034 | 260 | 1448 | −219 | 180 | 264 | 2% | 41% | 3.1 | 1.3 |
*Net=Total after taking away non-diabetes costs and age factor.
†Imp=Impact of additional resources for DM.
‡Adm=Admissions.
§ON=Overnight.
¶DC=Daycase.
T1DM individuals required 5.9 times as much secondary care activity as non-diabetes individuals. For T2DM, having allowed for the age difference there is 2.5 times secondary care activity as non-diabetes individuals. The main area for these costs difference was the emergency/non-elective care with 9.6 times the non-diabetes level for T1DM and 3.7 times non-diabetes level for T2DM. The elective treatment costs were 4.7 times for T1DM and 2.8 times higher for T2DM than for non-diabetes.
Total inpatient tariff charges
The total admission tariff charges for people with diabetes is £3.5 billion/year. £2.1 billion is for non-elective/emergency and £1.4 billion elective work. Of this, £0.9 billion would be chargeable for average non-diabetes activity plus £0.6 billion can be associated with the older age of the T2DM. Therefore, the total net additional costs are £2 billion/year—this splits as £0.4 billion T1DM (£1620/person) and £1.6 billion T2DM (£595/person).
For the non-diabetes population, non-elective/emergency tariff charges are 46% of the total admission charges. For people with diabetes, the net excess impact on non-elective/emergency work is £1.2 billion or 60% of the total net excess; this splits as £3090/person T1DM and net £340/person/T2DM.
Bed occupancy
The recorded 24.7 million bed days is equivalent to 67 577 fully occupied beds; of these, 13 047 or 19.3% were taken by people with either T1DM or T2DM. Of these, 6858 beds occupied (10%) can be explained by the expected health requirements of older age people. The remaining 6183 (9.1% of total) can be considered a direct consequence of the additional comorbidities associated with diabetes. Of these, 1645 (26% of DM excess total) excess beds are occupied by T1DM.
Closer examination of beds occupied by patients admitted in non-elective/emergency circumstances revealed that out of the total 38 914 fully occupied beds, 8832 (22.6%) were occupied by people with diabetes, and allowing for the expected 4576 normal and older age, the excess in emergency is 4256 beds—these are 11% of the total non-elective beds and 68% of the overall excess diabetes beds. It is also worth noting that 1174 of the excess non-elective beds are taken by T1DM people, making up 70% of the total 1645 T1DM excess beds.
Length of stay: excluding day cases
An average length of stay (LOS) for both elective overnight and emergency admissions can be calculated by dividing their total bed days for both T1DM and T2DM (age-adjusted) by their total number of overnight admissions for T1DM and T2DM (age-adjusted). These values can then be compared with the two different LOSs for the non-diabetes population.
The non-elective LOS for both T1DM and T2DM are only around 10% longer than non-diabetes, so most of the higher non-elective or emergency bed occupancy in diabetes must come from an increased rate of admission rather than LOS.
The elective LOS data are intriguing with the average overnight elective LOS for T1DM is at 1.0 day/person around 50% of the non-diabetes. For T2DM at 1.46 days/person, LOS is 62% of the non-diabetes LOS. This suggests that these patients are receiving higher numbers of planned short overnight admissions across a number of specialities, to treat some of the consequences of their condition.
Elective day case
The evidence shows that elective day-case admissions for both T2DM (age-adjusted) and T1DM are around 2.5 times the level of the non-diabetes patients. This will include day case podiatry procedures, ophthalmology and dialysis day-case attendances. This suggests that the increase in diabetes-associated comorbidities does also increase the amount of elective treatment levels that people with diabetes require.
Outpatient attendances
There was a big difference between the additional number of outpatient attendances that a person with T1DM patients showed at 4.8 times the non-diabetes attendances compared with the 1.8 times for T2DM. This might be due to the larger number of ongoing checks are being given to people with T1DM for eye, foot and renal complication management. The total additional outpatient attendances provided to people with diabetes to cover all the consequences of their condition was estimated at 6.9 million or 6% of all outpatient attendances. At an estimated average reference cost of £125/attendance, this costs the NHS total £825 million/year.
A&E attendances
A&E attendances for T1DM were 3.1 times higher and T2DM 1.3 times higher than non-diabetes. The total additional estimated diabetes related A&E attendances at 440 000 was 2% of all the A&E attendances in England in 2017/2018. At an average cost of £160/attendance, this costs the NHS a total of £70 million/year.
DISCUSSION
There has been much discussion about the true cost of diabetes and its complications to the NHS. There is already significant investment in managing the 3.2 million people identified with diabetes. The spend on glycaemic control medication alone in 2017_2018 was over £1 billion. This analysis shows that additional costs of provision of hospital services due to their diabetes comorbidities is £3 billion above those for non-diabetes and that within this T1DM have three times as much cost impact as T2DM. We have not included other forms of diabetes such as maturity onset diabetes of the young (MODY) or secondary diabetes in our analysis, as the numbers of people with these conditions are likely to be quite low at individual GP practices and coding of diagnosis is likely to vary.
In order to account for the variable rate of identification of T2DM across GP practices, we have:
In the hospital data captured activity for all those patients whose hospital record as having diagnosis diabetes at any visit during the previous 2 years.
In the practice data captured local total local populations having records of diabetes diagnosis.
In the latter, there will be an identification gap as practices will overdiagnose or underdiagnose compared with average. This gap will make those practices costs/head relatively higher or lower and so we make it clear that some of these costs may be due to overdiagnosis/underdiagnosis.
Also by calculating and bringing this identification gap into the age impact calculation, we remove this potential confounder from age impact.
In 2012, Hex et al9 in ‘Estimating the current and future costs of Type 1 and Type 2 diabetes in the UK, including direct health costs and indirect societal and productivity costs’ estimated the total secondary care costs at £7.7 billion with excess in-patient days at a cost £1.8 billion, of which 99% was on T2DM. Marion Kerr in ‘Inpatient Care for People with Diabetes: The Economic Case for Change for Insight Health Economics’ November 201110 estimated the additional impact at £573 million–£686 million. Neither of these previous analyses took account of the age distribution difference between T2DM individuals and the non-diabetes population as we have done here.
Hex et al8 also indicated that less than 25% of that diabetes treatment cost relates to the costs of management of diabetes, with the rest being accounted for by the costs of treating the complications of diabetes, which in one sense could be seen as ‘adverse events’. Another factor highlighted in this paper is that the indirect costs of diabetes are considerably higher than the direct costs and many relate to a cost to the individual with diabetes or to their carers. Cost estimates for productivity and social costs are often opportunity costs, such as time lost that could be spent on other activities.9 Furthermore, one quarter of care home residents in the UK have T2DM.11 Access issues, where there are frailty and mobility problems preventing routine GP or hospital appointment visits, can result in services being quite variable in delivery from one area to another.12
An International Diabetes Federation study13 showed that people with diabetes have medical costs that are two to three times more than age-matched and sex-matched patients without diabetes, that is, that if the average healthcare cost per person without diabetes is $1000 (£787), for a similar person with diabetes the cost will be $2000-$3000. These figures are not dissimilar to those reported in our study—of £560/non-diabetes person compared with £1810/person with diabetes. The significant excess of non-elective and elective activity and costs for T1DM individuals is indicative of the complexities of management of this condition and is related to the fact that many people with T1DM do not achieve target glycaemic control with hypoglycaemia, a frequent cause of hospital A/E attendance.14
There is also large pressure on hospital beds and especially with emergency admissions. That 11% of emergency beds are occupied by patients being admitted through the direct consequences their diabetes and 27% of these are T1DM shows that supporting patients in managing their diabetes remains a clear focus for primary care with T1DM remaining a very important aspect. LOS as reported here is also a factor and this can be impacted significantly by effective deployment of diabetes specialist nurses on wards.15
The total additional outpatient attendances provided to people with diabetes to cover all the consequences of their condition was estimated at 6.9 million or 6% of all outpatient attendances. This might be due to the larger number of ongoing checks that are being given to people with T1DM for eye, foot and renal complication management and to many people with T1DM. This also highlights a possible opportunity to deliver more of these services in the community rather than in the hospital for these patients.
The higher number of elective day-case, elective and A/E attendances likely are a consequence of management of diabetes complications and comorbidities in both T1DM and T2DM.
We acknowledge that we have not analysed ways in which the hospital costs of diabetes could be reduced. We know that people with diabetes are constantly managing their condition on a daily basis but may only come into contact with healthcare professionals a couple of times a year. Therefore, education programmes that give people the knowledge and motivation to manage their condition have value. For people with T1DM, Dose Adjustment Normal Eating (DAFNE)16 is an education course that trains people to estimate the carbohydrate in each meal and to inject the right dose of insulin. A cost-effectiveness analysis17 based on economic data from randomised control trials on DAFNE and similar programmes in Germany and Austria shows very good results. A 7-year follow-up on UK patients who went on a DAFNE course showed that their glycaemic control remained better than a similar group who had not been on the course.18 Over 10 years, structured treatment and teaching programmes save £2200 per patient. The majority of the savings arose from avoiding dialysis and foot ulceration.
Education for people with T2DM is also cost-effective. Data from a leading education programme, X-PERT, show the costs are outweighed by savings in cardiovascular and diabetes medication.19 A systematic review rated X-PERT as very cost-effective.20 Another major education programme, Diabetes Education and Self Management for Ongoing and Newly Diagnosed (DESMOND),21 is also effective with the key benefits being reductions in weight and smoking rate.22
In our recent papers,6 7 we showed that access to expert patient programmes can result in significant improvements in glycaemia control as can informed choice of diabetes medication. If achieved, such improvements in glycaemia could have the potential to reduce hospital costs in the longer term.
Healthcare systems influence a broad range of treatment decisions, both directly, via implemented policies/guidelines, and indirectly through the impact of shorter duration of clinical appointments and patients’ perceptions of their healthcare needs. We hope that this paper will be helpful to those who direct policy in healthcare both in the UK and elsewhere in the world.
CONCLUSION
People with diabetes have a significant impact on hospital activity including management of diabetes-related complications. They are admitted more often especially as emergencies and stay on average for longer. People with T1DM, although 10% of the people with diabetes have more than threefold the impact of T2DM, so require more special attention. However, people with T2DM have a wider range of comorbidities and so can be more complex.
While not a conclusion that we can draw directly from our analysis, it is possible that improved management of T1DM and T2DM in primary care in terms particularly of measures to prevent the longer term development of complications may reduce the level of hospital activity and hospital costs. The role of the secondary care specialist team in supporting primary care and ensuring that most people with diabetes are being well managed, not just focussing on the smaller in number hardest to treat group will be a key factor in improving primary care management outcomes will be critical in this endeavour.
Supplementary Material
Footnotes
Contributors: MS, MD and AH conceived the study. MS collected the data. MS and MLu conducted the data analysis. MS, MLi, MD, AF, CD, MG, RG, SGA, GR and AH all contributed to the writing of the paper. SGA, GR, RG, AF and MG provided an overview of the manuscript.
Funding: The relevant HES data were extracted from NHS Digital Hospital Episode Statistics by Wilmington Healthcare and provided by NAPP Pharmaceuticals. AH as the corresponding author affirms that this is an honest, accurate and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Disclaimer: Dissemination to specific participants will not be possible as all data was anonymised and at a GP practice level.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research.
Patient consent for publication: Not required.
Ethics approval: As we used publicly available and general practitioner level data, with no individual patient data, it was not necessary to seek ethics approval for this study.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available in a public, open access repository. In most cases, publicly available data were used for the analysis. The Hospital Episode Data and filtration by Patient Diagnosis can be obtained through a suitable NHS Digital data research application (https://digital.nhs.uk/services/data-access-request-service-dars).
References
- 1.Who global report on diabetes, 2016. Available: https://apps.who.int/iris [Accessed 31 May 2019].
- 2.National diabetes inpatient audit, 2018. Available: http://content.digital.nhs.uk/diabetesinpatientaudit [Accessed 25 May 2019].
- 3.NHS Digital HES data. Available: https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/hospital-episode-statistics [Accessed 21 May 2019].
- 4.National diabetes audit, 2018. Available: http://content.digital.nhs.uk/diabetesinpatientaudit [Accessed 25 May 2019].
- 5.HERC Yorkshire and the number public health Observatory data, 2018. Available: https://www.herc.ox.ac.uk/health_datasets/.data./yorkshire-and-the-humber-public-health-observatory-indicator-search-tool [Accessed 26 May 2019].
- 6.Heald AH, Livingston M, Malipatil N, et al. Improving type 2 diabetes mellitus glycaemic outcomes is possible without spending more on medication: lessons from the UK national diabetes audit. Diabetes Obes Metab 2018;20:185–94. 10.1111/dom.13067 [DOI] [PubMed] [Google Scholar]
- 7.Heald AH, Livingston M, Fryer A, et al. Route to improving type 1 diabetes mellitus glycaemic outcomes: real-world evidence taken from the National diabetes audit. Diabet Med 2018;35:63–71. 10.1111/dme.13541 [DOI] [PubMed] [Google Scholar]
- 8.NHS Improvement 2017_18 Hospital Service Reference costs Available: https://improvement.nhs.uk/resources/reference-costs/#rc1718
- 9.Hex N, Bartlett C, Wright D, et al. Estimating the current and future costs of Type 1 and Type 2 diabetes in the UK. including direct health costs and indirect societal and productivity costs York Health Economics Consortium Ltd, University of York, Diabetic medicine 2012;29:855–62. [DOI] [PubMed] [Google Scholar]
- 10.Inpatient care for people with diabetes: the economic case for change Marion Kerr insight health economics. Available: https://www.diabetes.org.uk/resources-s3/2017-1_1.pdf [Accessed 14 Jun 2019].
- 11.The Kings Found Available: www.kingsfund.org.uk/sites/default/files/field/field_document/managing-people-long-term-conditions-gp-inquiry-research-paper-mar11.pdf [Accessed 23 May 2019].
- 12.Good clinical practice guidelines for care home residents with diabetes, 2010. Available: http://www.diabetes.org.uk/About_us/Position-statements-recommendations/Care-recommendations/Good-clinical-practice-guidelines-for-care-home-residents-with-diabetes [Accessed 25 May 2019].
- 13.Zhang W, et al. Economic impact of diabetes in diabetes atlas fourth edition. Brussels: International Diabetes Federation, 2009. http://www.idf.org/sites/default/files/Economic_impact_of_Diabetes.pdf [Google Scholar]
- 14.Wang H, Donnan PT, Leese CJ, et al. Temporal changes in frequency of severe hypoglycemia treated by emergency medical services in types 1 and 2 diabetes: a population-based data-linkage cohort study. Clin Diabetes Endocrinol 2017;3:7. 10.1186/s40842-017-0045-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Diabetes Times Available: https://diabetestimes.co.uk/diabetes-nurses-group-celebrates-anniversary-2/ [Accessed 23 June 2019].
- 16.Lawton J, Rankin D, Cooke D, et al. Patients' experiences of adjusting insulin doses when implementing flexible intensive insulin therapy: a longitudinal, qualitative investigation. Diabetes Res Clin Pract 2012;98:236–42. 10.1016/j.diabres.2012.09.024 [DOI] [PubMed] [Google Scholar]
- 17.Shearer A, Bagust A, Sanderson D, et al. Cost-Effectiveness of flexible intensive insulin management to enable dietary freedom in people with type 1 diabetes in the UK. Diabet Med 2004;21:460–7. 10.1111/j.1464-5491.2004.01183.x [DOI] [PubMed] [Google Scholar]
- 18.Gunn D, Mansell P. Glycaemic control and weight seven years after DAFNE structured education in type 1 diabetes. Diabetic Medicine 2012;29:807–12. [DOI] [PubMed] [Google Scholar]
- 19.Deakin T. The diabetes pandemic: is structured education the solution or an unnecessary expense? Practical Diabetes 2011;28:1–14. 10.1002/pdi.1635 [DOI] [Google Scholar]
- 20.Jacobs-van der Bruggen MAM, van Baal PH, Hoogenveen RT, et al. Cost-Effectiveness of lifestyle modification in diabetic patients. Diabetes Care 2009;32:1453–8. 10.2337/dc09-0363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gillett M, Dallosso HM, Dixon S, et al. Delivering the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: cost effectiveness analysis. BMJ 2010;341:c4093. 10.1136/bmj.c4093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davies MJ, Heller S, Skinner TC, et al. Effectiveness of the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: cluster randomised controlled trial. BMJ 2008;336:491–5. 10.1136/bmj.39474.922025.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.