Abstract
Background:
The need for case-based learning in basic subjects is being recognized world over. Early clinical illustrations and actual clinical exposure enable students to associate basic science and real patient situations, probably increasing their retention of knowledge. The study was conducted to introduce an alternate method of teaching-learning in pharmacology in a large classroom setting to integrate pharmacology into clinical setting for better learning and understanding of the subject.
Methods:
Ninety-four students of second professional MBBS of a medical college in Punjab were divided into 2 groups and were taught a 2-hour topic in pharmacology using case-based learning (CBL) method and didactic lecture (DL) method using a crossover design. Their attendance and written test score at the end of teaching session were compared. Feedback from students and faculty was taken by prestructured questionnaires.
Results:
There was an increase in students’ attendance (P = .008) in CBL sessions but insignificant difference in their performance (P = .98) in the tests. Most (84%) of the students felt that CBL is a better method of teaching-learning than traditional DL. The teaching faculty felt that the students looked more interested and were themselves more motivated for the newer method of teaching.
Conclusions:
Case-based learning led to improvement in student motivation, satisfaction, and engagement. Most students and faculty accepted that CBL was an effective learning tool for pharmacology teaching in a large group setting and supported the incorporation of CBL into traditional DL teaching.
Keywords: Feedback, Pharmacology, Medical Education, Case based learning
Introduction
The teaching of pharmacology is a challenging task as it involves teaching of drugs and their kinetics and dynamics. Without any real-world application of this massive knowledge-bank in pharmacology, the undergraduate students are afraid of the subject due to the massive amount of data that have to be crammed and learned by rote memorization. Hence, an element of clinical correlation has to be brought into pharmacology teaching to promote easy comprehension of the subject.1
The introduction of problem-based, integrated student-centered medical curriculum demands active participation from the students and motivates them and facilitates self-directed learning.2 The Medical Council of India has also recommended the introduction of case-based learning (CBL) in basic medical subjects.3,4 It will be a challenge to implement the new curriculum across India, from training the faculty to adopting the novel teaching-learning (TL) methods, but most importantly to attempt a change in the conventional mind-set of the teachers and learners. Novel TL methods such as CBL, small group teaching, and bedside teaching are being introduced all over India, a small step toward sensitizing the faculty and students.5
Case-based learning is centered on a well-designed clinical problem through which students identify their learning requirements, make an enquiry, and correlate the theory and practice. Because of the active participation by students, it enhances the students’ ability to analyze and learn clinical application of the knowledge to treat a patient and can reflect on the educational experience gained through the cases/problems.6,7 The CBL encourages independent learning and deeper understanding of a particular topic and promotes life-long learning.2,8,9
There have been many studies to evaluate the small-group CBL learning.10-13 However, little research has been done on the educational benefits of CBL in a large group setting. This study was undertaken to introduce the students to an alternative method of learning (CBL) compared with the traditional one used (didactic lecture [DLs]) in a large classroom setting, to assess the students’ performance and acceptance of this modified teaching method, and to assess increased participation of students in CBL classes and the satisfaction and acceptance of the faculty with CBL as TL with the aim to improve student understanding and learning of the subject of pharmacology.
Methods
After approval from the Institutional Ethics Committee, the descriptive study was started in May 2016 for 5 months, in the Department of Pharmacology at a medical college in Punjab.
Planning
The study was planned in detail in a departmental meeting held in May 2016 with the head and whole faculty. The faculty was sensitized to the concept of CBL using problems and prescriptions. Subsequently, the faculty was made aware of the proposed intervention in the teaching method of students. Two topics which were to be taught to students using the proposed TL methods were finalized (drugs for acid peptic disorder [APD] and drugs for tuberculosis). Cases, problems, and prescriptions of the 2 finalized topics were prepared after focus group discussions involving all the faculty in the department and finalized. The students were also sensitized about the method and the topics 1 week before the class.
The feedback questionnaires for students and faculty were developed and validated by peer review. The student feedback questionnaire (Appendix 1) consisted of 12 questions on a 5-point Likert-type scale (1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, 5 = strongly agree). The questions were framed in such a way that yielded information regarding the use of DL and CBL in pharmacology classes and the context of understanding the mechanism of action and rationale of drugs. The faculty feedback questionnaire was prepared to know about their experiences and opinion about the new model method. The questionnaire had 7 questions on the 5-point Likert-type scale (Appendix 2). The students and the faculty who participated in the pilot study for questionnaire validation were excluded.
For the study, fourth semester MBBS professional students were taught topics of drugs for APD and anti-tubercular drugs using cases/problems and prescriptions for a duration of 2 hours for each topic. The total of 94 students was randomly divided into 2 groups: Group A and Group B. In Group A, 47 students were taught a 2-hour topic in pharmacology (drugs used in APD) using the case-based pharmacology (CBL) method (using prescriptions and problems as cases). In the method, a brief explanation was presented by the teacher, followed by an introduction of a clinical case scenario accompanied by questions addressing the objectives of that part of the lecture. (Students were asked to provide treatment on the basis of the case.) Group B had 47 students who were taught the same topic according to the routine DL method. In the next session, crossover of students was done and another 2-hour topic (drugs for tuberculosis) was taught by the CBL method and the traditional method (DL).
This was followed by a voluntary and anonymous prevalidated feedback questionnaire administered to all students. The feedback from the participating faculty was also obtained using a prevalidated feedback questionnaire. After 2 weeks of announcement, the students were given a written test of 40 marks (mixture of structured essay questions, short notes, and multiple-choice questions. The test paper was an equal mix of critical thinking–based and knowledge-based questions.
Data collection
The attendance during the sessions was noted and assessed. A written test was taken 2 weeks after the classes to evaluate the impact of the teaching methodology. The test score between the 2 groups (Group A and Group B) was compared and analyzed. The feedback from both students and faculty was taken and assessed.
Statistical analysis
The data collected were analyzed using parametric tests such as Student t test using Microsoft Excel 2010. A value of P < .05 was considered significant. Descriptive statistics was used to analyze the marks obtained, and the feedback questionnaires and results were expressed as percentage.
Results
A total of 94 students of second professional (fourth semester) MBBS were assessed in the 2 sessions. There were 42 men and 52 women, with an average age of 20.38 ± 0.852 years. The 2 groups were similar in all aspects (cross-over design) except the teaching method adopted for the 2 groups.
(a) Attendance in the sessions: On applying the t-unpaired test, there was significant difference (P = .008, t = 2.65) in attendance between the 2 groups (CBL vs DL), as shown in Figure 1.
(b) Outcome of the test: Regarding the marks obtained in the written test, on applying the t-unpaired test, there was no significant difference (P = .98) between the average marks scored by the students in the CBL and DL methods (Figure 2). However, on applying the t test on the detailed mark list (based on the type of questions asked), it was found that there was significant increase in marks obtained by students taught by CBL regarding questions which involved critical thinking (than the DL method). On the contrary, the knowledge-based questions showed significantly better results in the DL method than in the CBL method (Appendix 3).
(c) Perception of students regarding CBL: Feedback forms were offered to the students for voluntary and anonymous feedback, and all (100%) students gave their feedback (Figure 3). The students also mentioned some drawbacks of CBL: it made lectures slow and they required greater effort in the class, whereas many students suggested increasing the number of CBL sessions, asked for more cases, and were quite excited to answer the problems.
(d) Perception of faculty regarding CBL: The entire faculty involved in the study gave their feedback (Figure 4). Some of the suggestions given by the faculty included proper training of faculty for CBL by holding training sessions and to make a collection of cases, problems, and prescriptions for future use.
Figure 1.
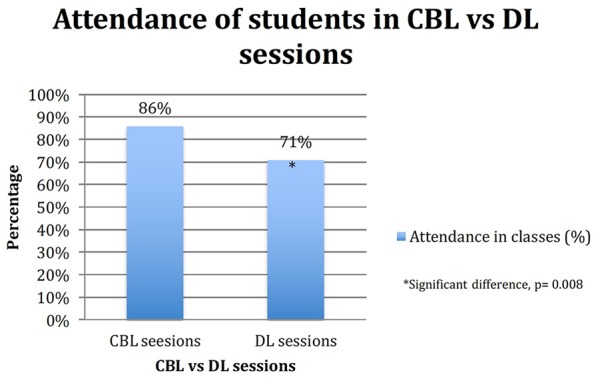
Attendance of students in the 2 groups in the sessions. CBL indicates case-based learning; DL, didactic lecture.
Figure 2.
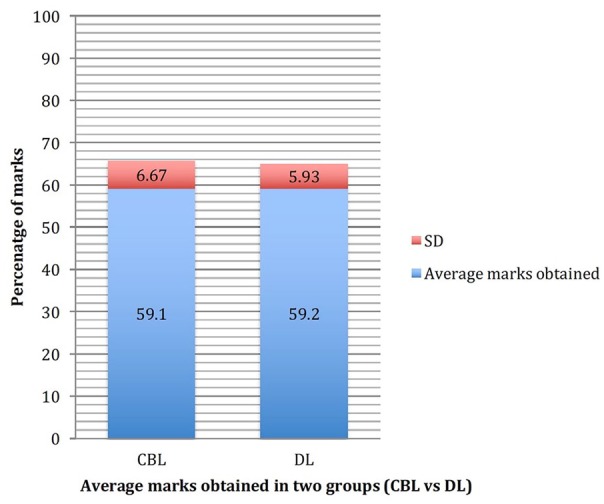
Marks obtained in written test by students of CBL vs DL groups. CBL indicates case-based learning; DL, didactic lecture.
Figure 3.
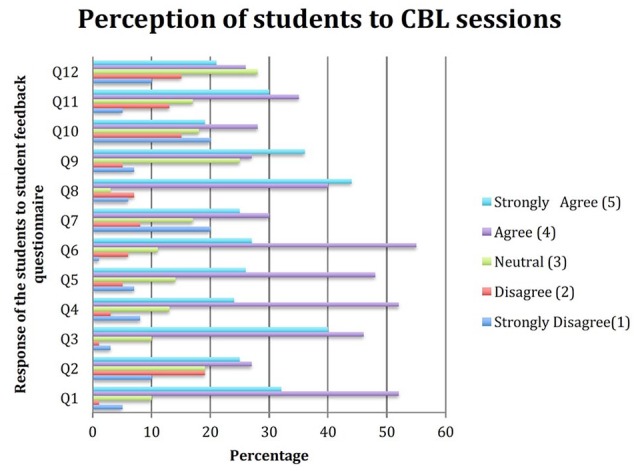
The response to the student feedback questionnaire (based on a 5-point Likert-type scale). Perception of students to CBL sessions. CBL indicates case-based learning.
Figure 4.
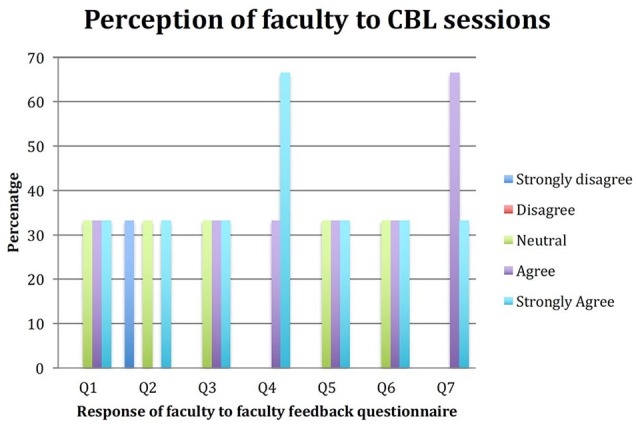
The response to the faculty feedback questionnaire (based on a 5-point Likert-type scale). Perception of faculty to CBL sessions. CBL indicates case-based learning.
Discussion
Pharmacology is a discipline more applicable and closer to clinical science; the design of learning cases and the incorporation of clinical relevance in them should be more obvious and easier to make. Recent studies indicate that CBL students are at least as successful in standardized tests and enjoy their learning more than conventional lecture–based learning students do.1,14 The improved attendance of students in our CBL sessions shows the students were motivated and interested to learn through CBL. The average marks obtained by 2 teaching methods were statistically insignificant. This indicates that the students found the CBL method as an engaging activity compared with the DL method. However, an insignificant difference in the marks obtained indicates no difference in retention of knowledge. Similar results were found by a study by Chilwant.15
There was no increase in marks obtained by the CBL method than the traditional DL method, but the students found the CBL much interesting and motivating. These results are similar to those studied by Michel et al,16 according to which a switch from lecture to CBL teaching of pharmacology does not occur at the expense of factual knowledge transmission. But the students rated generated interest in pharmacology and conveyed knowledge in pharmacology and understanding of medical questions higher than DL students.
The results of our study are comparable to the study done by Tayem in which CBL was found to be an effective learning tool for 82% of students and improved their level of preparation of exams (as stated by 75% of students), and 96% of students felt that the cases were appropriate to the lecture topics.8 For successful conduction of CBL, the role of the teacher was found to be very important by almost all of the students. In an interactive session like CBL, the role of teacher/facilitator is quite important as the subsequent discussion was dependent on the type of cases prepared.
In a comparative study conducted by Gupta et al,17 76% of the students found the CBL sessions to be better than theory lectures compared with 75% of students in our study. In our study, 74% of students believed that CBL sessions improved their concepts of pharmacology in clinical settings, as proved in a study by Gupta et al17 where 89% of students felt that the sessions reinforced the clinical aspects of the topics discussed. Only 50% of students in a study by Dube et al18 agreed that CBL improved ability to apply concepts of basic sciences to clinical situations. A similar study conducted in Bihar19 reported that 95% of students recommended CBL for next batches compared with only 37% of students in our study, and as many as 28% of students were neutral on this decision. Case-based learning promotes active involvement, increases attention and motivation, gives immediate feedback to teacher and student, and enhances the student’s learning by increasing the ability to synthesize and integrate the material in comparison with passive learners.19
A study concluded by Adiga and Adiga20 also clearly demonstrates stronger benefits of CBL in learning, such as an enhancement in academic locus, triggered motivation, achieving strategy, deep approaches, and deep-achieving approach to learning for the whole group. The results suggest that there are important cognitive benefits of the CBL approach. Case-based learning provides motivation for self-directed learning and helps to develop problem-solving skills. Only 50% of students in a study18 stated that CBL sessions would be helpful for final university exam preparation as against 65% in our study. All of the students agreed that learning of facts, diagnostic, and therapeutic skills was significantly enhanced by CBL sessions.18
A study done in medical school in Mexico also confirms our findings that students had an acceptable level of agreement in having carried out activities related to elaboration of knowledge, such as analyzing and answering questions, formulating hypothesis, and understanding the application of pharmacological knowledge.21 A study by Chilwant15 reported that 73% of students were motivated for self-study and 71% of students think that their performance in university examination will be better. Seventy-six percent of students were willing to replace conventional lectures with interactive lectures. These findings also support our present study, with 84% of students more motivated and 75% of students feeling that they will show a better performance in university exams.
Our faculty admitted that the whole experience was very motivating and it has improved their knowledge about newer TL methods. The faculty feedback was positive and so wanted to incorporate CBL for other important topics and combine it with traditional lectures methods, which are similar to the findings concluded by Dube et al.18
Student attendance has been recognized as a reliable parameter measuring student satisfaction with the learning process.22 The significant increase in attendance of students in CBL classes is similar to the CBL study reported by Klegeris and Hurren22 and Smith and Cook.23 The increase in attendance is a further proof of positive student impact and is attributed to the students’ interest to attend the class.
The limitations of the study were that only the short-term outcome was looked into. The long-term outcome, which is possible during internship and in the results of their PG exams, can be also assessed. Their prescribing skills can be assessed when they start practicing in their life. Evaluating students’ performance over 1 academic year with and without CBL could make an objective analysis of effectiveness of CBL. Also, the absent students were marked zero in the test. They were not excluded from the study because their feedback was taken regarding the methods of teaching. There is an inequality in the number of absent students from the 2 groups, which is a confounding factor for the results.
Conclusion
Case-based learning should be incorporated into our medical curriculum as a part of regular TL method for large group setting. The combination of both didactic lectures and case based learning would be an effective educational tool. Positive perceptions of students and faculty indicate the successful introduction of CBL in Basic Sciences Department like ours. Further studies aimed at assessing student learning, understanding, and retention of course content are needed to further justify implementation of this technique in courses that are delivered to large undergraduate classes.
Acknowledgments
The authors are thankful to the faculty and staff of the Department of Pharmacology at Gian Sagar Medical College, without whom this project would have been impossible to complete. They also acknowledge the guidance and help provided by the faculty of Medical Education Unit of CMC, Ludhiana.
Appendix
Appendix 1.
Questions in the student feedback questionnaire (based on a 5-point Likert-type scale).
| S. No | Questions |
|---|---|
| 1. | CBL was useful in the understanding of the topic |
| 2. | Didactic lectures were useful in the understanding of the topic |
| 3. | The problems given in the CBL were in the context of the topic under study |
| 4. | By virtue of CBL, the drugs could be better related to their basic mechanisms |
| 5. | CBL improved my ability to apply concepts of basic sciences to clinical situations |
| 6. | CBL helped me develop skills in identifying potential drug-related difficulties of the patient |
| 7. | CBL improved my learning skills better than didactic lectures |
| 8. | CBL made me motivated to learn more about the topic |
| 9. | There should be a judicious mixture of didactic lectures and CBL sessions for a better understanding of drugs |
| 10. | All CBL sessions should be preceded by didactic lectures to help with better understanding |
| 11. | Training in CBL sessions will help me in preparing you for the final university examination |
| 12. | CBL can be introduced as a new teaching-learning method for next batches |
| Any other suggestions/comments | |
Abbreviation: CBL, case-based learning.
Appendix 2.
Questions in the faculty feedback questionnaire (based on a 5-point Likert-type scale).
| S. No | Questions |
|---|---|
| 1. | Students were more involved, engaged, and interested in the session |
| 2. | CBL preparation took too much time |
| 3. | More faculty is required for proper implementation of CBL |
| 4. | CBL preparation requires more hard work. |
| 5. | CBL was very motivating and it has improved our knowledge about newer TL methods |
| 6. | Incorporate CBL for other important topics and combine it with traditional lecture methods |
| 7. | Will recommend this method of teaching for future batches |
| Any other suggestions/comments | |
Abbreviation: CBL, case-based learning; TL, teaching-learning.
Appendix 3.
Detailed marks obtained by 2 groups of students (MM: 40 marks).
| Group A (CBL method) |
Group B (DL method) |
|||
|---|---|---|---|---|
| Knowledge based (20 marks) |
Critical thinking based (20 marks) |
Knowledge based (20 marks) |
Critical thinking based (20 marks) |
|
| Average marks obtained | 10.67 ± 3.22 | 12.99 ± 3.72 | 12.69 ± 3.19 | 10.94 ± 2.97 |
| Percentage of marks | 26.7 | 32.5 | 31.73 | 27.34 |
| Standard error | 0.332 | 0.384 | 0.33 | 0.307 |
| Confidence level (95%) | 0.66 | 0.76 | 0.65 | 0.61 |
| Upper | 11.33 | 13.75 | 13.35 | 11.55 |
| Lower | 10.01 | 12.23 | 12.04 | 10.33 |
| P value | (CBL vs DL) P < .0001 |
(CBL vs DL) P < .0001 |
— | — |
Abbreviations: CBL, case-based learning; DL, didactic lecture.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: All the authors were involved in conception, literature review, drafting and revising of the manuscript. The final manuscript was approved by all the authors.
ORCID iD: Gurleen Kaur  https://orcid.org/0000-0001-8405-2913
https://orcid.org/0000-0001-8405-2913
References
- 1. Lau YT. Problem-based learning in pharmacology: a survey of department heads in Taiwan, China. Acta Pharmacol Sin. 2004;25:1238-1240. [PubMed] [Google Scholar]
- 2. Ghosh S. Combination of didactic lectures and case-oriented problem-solving tutorials toward better learning: perceptions of students from a conventional medical curriculum. Adv Physiol Educ. 2007;31:193-197. [DOI] [PubMed] [Google Scholar]
- 3. Medical Council of India. Regulations on Graduate Medical Education, 1997. Notification, Gazette of India, Part III, Sect. 4. 1997. Amended Upto Ma, 2018. https://www.mciindia.org/CMS/wp-content/uploads/2017/10/GME_REGULATIONS-1.pdf. Accessed February 12, 2020.
- 4. Competency based undergraduate curriculum for the Indian Medical Graduate. Alignment and Integration. https://www.mciindia.org/CMS/wp-content/uploads/2020/01/Alignment-and-Integration_03.10.2019.pdf. Accessed February 12, 2020. [PubMed]
- 5. Badyal DK. Pharmacology education in India: challenges ahead. Indian J Pharmacol. 2016;48:S3-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mahajan R, Badyal DK, Gupta P, Singh T. Cultivating lifelong learning skills during graduate medical training. Indian Pediatr. 2016;53:797-804. [DOI] [PubMed] [Google Scholar]
- 7. Kamat SK, Marathe PA, Patel TC, Shetty YC, Rege NN. Introduction of case based teaching to impart rational pharmacotherapy skills in undergraduate medical students. Indian J Pharmacol. 2012;44:634-638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tayem YI. The impact of small group case-based learning on traditional pharmacology teaching. Sultan Qaboos Univ Med J. 2013;13:115-120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. James H, Al Khaja KA, Sequeira RP. Effective use of real-life events as tools for teaching-learning clinical pharmacology in a problem-based learning curriculum. Indian J Pharmacol. 2015;47:316-321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Vora MB, Shah CJ. Case-based learning in pharmacology: moving from teaching to learning. Int J Appl Basic Med Res. 2015;5:S21-S23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hasamnis AA, Arya A, Patil SS. Case-based learning: our experience in clinical pharmacology teaching. J Pharm Bioallied Sci. 2019;11:187-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Singhal A. Case-based learning in microbiology: observations from a North West Indian Medical College. Int J Appl Basic Med Res. 2017;7:S47-S51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Thistlethwaite JE, Davies D, Ekeocha S, et al. The effectiveness of case-based learning in health professional education. A BEME systematic review: BEME Guide No. 23. Medical Teacher. 2012;34:e421-e444. [DOI] [PubMed] [Google Scholar]
- 14. Michel MC, Bischoff A, Jakobs KH. Comparison of problem-and lecture-based pharmacology teaching. Trends Pharmacol Sci. 2002;23:168-170. [DOI] [PubMed] [Google Scholar]
- 15. Chilwant KS. Comparison of two teaching methods, structured interactive lectures and conventional lectures. Biomed Res. 2012;23:363-366. [Google Scholar]
- 16. Michel MC, Bischoff A, Zu Heringdorf M, Neumann D, Jakobs KH., Problem- vs. lecture-based pharmacology teaching in a German medical school. Naunyn Schmiedebergs Arch Pharmacol. 2002;366:64-68. [DOI] [PubMed] [Google Scholar]
- 17. Gupta K, Arora S, Kaushal S. Modified case based learning: our experience with a new module for pharmacology undergraduate teaching. Int J Appl Basic Med Res. 2014;4:90-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dube SP, Ghadlinge MS, Mungal SU, Tamboli SB, Kulkarni MB. Students’ perception towards the problem based learning. IOSR-JDMS. 2014;13:49-53. [Google Scholar]
- 19. Kumar A, Vandana Aslami AN. Introduction of “case-based learning” for teaching pharmacology in a rural medical college in Bihar. Natl J Physiol Pharm Pharmacol. 2016;6:427-430. [Google Scholar]
- 20. Adiga S, Adiga U. Problem based learning—An approach to learning pharmacology in medical school. Biomed Res. 2010;21:43-46. [Google Scholar]
- 21. Marin-Campos Y, Mendoza-Morales L, Navarro-Hernandez JA. Students’ assessment of problems in a problem-based learning pharmacology course. Adv Health Sci Educ Theory Pract. 2004;9:299-307. [DOI] [PubMed] [Google Scholar]
- 22. Klegeris A, Hurren H. Impact of problem-based learning in a large classroom setting: student perception and problem-solving skills. Adv Physiol Educ. 2011;35:408-415. [DOI] [PubMed] [Google Scholar]
- 23. Smith M, Cook K. Attendance and achievement in problem-based learning: the value of scaffolding. Interdisc J Prob Based Learn. 2012;6:129-152. [Google Scholar]


