Abstract
Objectives
This study aims to examine litigation trends with thyroidectomies in the United States from 1984 to 2018.
Methods
We used the Westlaw legal database to collect data on the defendant, plaintiff, case demographics, alleged reasons for malpractice, additional complications, and case outcomes.
Results
The most common reason for litigation was vocal cord paralysis (51%, n = 28), with the majority ruling in favor of the defendant (64%, P = .042). Of those, 43% of cases (n = 12) were due to unilateral recurrent laryngeal nerve (RLN) injury, and 39% (n = 11) were due to bilateral RLN injury. Of the claims due to vocal cord paralysis that resulted in indemnity payment (36%), the majority included additional damages, such as lack of informed consent (30%) or subsequent damages from permanent tracheostomy (40%), which is usually a result of bilateral nerve paralysis.
Conclusion
RLN injury was the most common complication leading to trial, with most cases ruling in favor of the defense. However, most verdicts that favored the plaintiff or those that settled were due to subsequent damages from bilateral nerve paralysis, such as permanent tracheostomy. We encourage surgeons to consider a staged procedure in high-risk cases or cases with signal loss. There needs to be a bigger emphasis on informed consent in the training of surgeons. Surgeons should educate patients at high risk on potential surgical complications that may drastically affect their quality of life.
Keywords: medicolegal, thyroidectomy, malpractice, litigation, complications
Around 12% of the US population will develop a thyroid condition in their lifetime.1 These conditions include benign disorders such as goiter, hyperthyroidism, thyroiditis, Graves’ disease, and Hashimoto’s disease, and malignant ones, such as papillary, medullary, or anaplastic thyroid carcinoma. Surgical options for these conditions, particularly nodules and cancer, include thyroid lobectomy or total thyroidectomy. In the United States, the incidence of thyroid cancer has increased from 4.8 cases per 100,000 population in 1975 to 15.0 cases per 100,000 population in 2015.2 In addition to the increase in malignant thyroid conditions, benign conditions have been on the rise, leading to an increase in the total number of thyroidectomies performed.3-5 Although most complications following thyroidectomy are typically reversible, such as vocal cord paralysis (VCP) and hypocalcemia, there is a risk for permanent damage. Complications include unilateral VCP (0.85%), hypocalcemia (0.85%), hypothyroidism (0.77%), death (0.61%), and bilateral VCP (0.34%).6-9 The increase in thyroidectomies over the years, coupled with the serious complications, places physicians at significant risk for litigation, resulting in substantial cost and anguish.10
Medical malpractice lawsuits affect the state of health care and the patient’s well-being and influence how physicians conduct their practice.11 Previous literature has evaluated malpractice lawsuits in the hopes of educating and creating risk management approaches.4,12-14 Medical malpractice in thyroidectomies has been examined before; however, details regarding individual cases were not included in the analysis. The most recent review concluded that malpractice cases due to thyroidectomy are uncommon and do not result in indemnity payments. In addition, details regarding specialty training and type of paralysis (unilateral vs bilateral), as well as details regarding damages, were not included.10,14-16 Traditionally, general surgeons performed thyroidectomies, but in recent years, otolaryngologists have taken a larger role in the surgical procedure and management of thyroid disease.17,18
Our goal is to examine the litigation trends and risks involved with performing thyroidectomies and to provide risk mitigation strategies for physicians in both specialties.
Material and Methods
Data Source and Study Subjects
We conducted a retrospective study using data from the computerized legal database Westlaw (West Publishing Co, St Paul, Minnesota). Westlaw includes >40,000 databases and is one of the most advanced legal search engines in the United States. It consists of all federal and state court records that advance far enough for inclusion into publicly available records. Rules for inclusion in public records differ by jurisdiction. Most jurisdictions require reporting their verdict and settlements, while some do not and report only voluntarily submitted records, which the attorney has the option to do. If a case does not proceed far enough before reaching an out-of-court settlement, it will not be included in public records and therefore not included in Westlaw. Westlaw represents cases that have been evaluated by attorneys and deemed to be the most relevant and valuable due to precedent or content. We used a sample of Westlaw claims data that included the Medical Litigator database and Jury Verdicts and Settlements database. The search included all state and federal claims containing “thyroidectomy.” Out of 96 initial results, 41 cases were excluded ( Figure 1 ). Our study included 55 appropriate cases from 25 states from 1984 to 2018. The retrospective study was approved by the Institutional Review Board of the University of Texas Medical Branch at Galveston.
Figure 1.
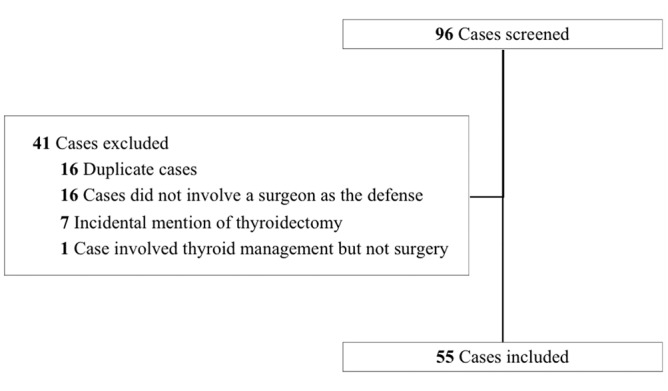
Selection of Westlaw database cases for analysis.
Variables and Study Outcomes
The defendant’s information included name, age, and sex, and the plaintiff’s information included name, specialty, and fellowship training. Additional information included the date, state, and county of the trial; diagnosis; procedure involved; damages and surgical complications; the defendant and plaintiff expert witnesses; and the final verdict, including the award size, amount of award demanded, and any settlement offers. All surgical complications and primary allegations for malpractice were collected. The cases were categorized on the basis of the most prominent injuries leading to litigation, including VCP, parathyroid injury, death, and progression of cancer. Less common injuries following thyroidectomy were grouped in an “other damages” category, which included wound-related injuries, coma, infection, emotional distress, and brachial plexus injury. Many operations resulted in additional medical complications reported in litigation, such as emotional distress, economic disparity, hematoma, permanent tracheostomy, and need for additional procedures. The cases were categorized by state. The incidence of litigate per state was calculated per the state’s current population.
Statistical Analyses
Descriptive statistics was presented as number and percentage for categorical data and mean (standard deviation) as well as median (first quartile, third quartile) for continuous data. For group comparison on categorical data, the chi-square test was applied, and the Fisher exact test was applied for data with an expected value <5. For group comparison on continuous data, the Wilcoxon 2-sample test (2 groups) or Kruskal-Wallis test (for 3 groups) was used. All analyses were conducted with SAS statistical software (version 9.4; SAS Institute Inc, Cary, North Carolina).
Results
Demographics
Fifty-five cases were found from 1984 to 2018. The majority (n = 23, 41%) were from 2000 to 2009 ( Table 1 ). Of the 55 cases, 15 (27.27%) were from 2010 to the present, 9 (16.36%) from 1990 to 1999, and 8 (14.54%) from 1980 to 1989. The age range was from 11 to 80 years, with a mean of 42 years. The majority of the plaintiffs were female (n = 50, 90.91%). The indications for surgery included benign disease (25.45%), thyroid dysfunction (18.18%), cancer (14.55%), or unknown conditions (41.8%). Benign disease included goiter, benign thyroid nodules, and cancer suspicion (25.45%). Thyroid dysfunction included inflammatory conditions, such as Graves’ disease, Hashimoto’s disease, thyroiditis, and hyperthyroidism (18.18%). Total thyroidectomy was the most performed procedure, as seen in 26 (47.27%) of 55 cases. The remaining procedures performed were a subtotal thyroidectomy in 7 cases (12.73%), lobectomy in 6 cases (10.91%), and unspecified thyroidectomy in 16 cases (29.09%).
Table 1.
Patient Characteristics (N = 55).
| Characteristics | No. of Patients | % |
|---|---|---|
| Age, y | ||
| 11-30 | 10 | 18.18 |
| 31-40 | 6 | 10.91 |
| 41-50 | 7 | 12.73 |
| 51-80 | 8 | 14.55 |
| Unknown | 24 | 43.64 |
| Sex | ||
| Male | 5 | 9.09 |
| Female | 50 | 90.91 |
| Indication | ||
| Benign diseasea | 14 | 25.45 |
| Thyroid dysfunctionb | 10 | 18.18 |
| Cancer | 8 | 14.55 |
| Unknown | 23 | 41.82 |
| Procedure | ||
| Total thyroidectomy | 26 | 47.27 |
| Subtotal thyroidectomy | 7 | 12.73 |
| Left lobectomy | 4 | 7.27 |
| Right lobectomy | 2 | 3.64 |
| Unspecified thyroidectomy | 16 | 29.09 |
| Primary damage | ||
| Vocal cord paralysis | 28 | 50.91 |
| Parathyroid injury | 7 | 12.73 |
| Death | 7 | 12.73 |
| Progression of cancer | 5 | 9.09 |
| Otherc | 8 | 14.55 |
| Procedure time | ||
| 1980-1989 | 8 | 14.55 |
| 1990-1999 | 9 | 16.36 |
| 2000-2009 | 23 | 41.82 |
| 2010-present | 15 | 27.27 |
| Regiond | ||
| Northeast | 10 | 18.18 |
| Midwest | 15 | 27.27 |
| South | 19 | 34.55 |
| West | 11 | 20.00 |
Goiter, thyroid nodules, and cancer suspicion.
Graves’ disease, Hashimoto’s disease, thyroiditis, and hyperthyroidism.
Wound injury, coma, infection, emotional distress, and brachial plexus injury.
US Census Bureau–designated regions: Northeast (CT, NJ, NY, PA), Midwest (IL, IN, KS, MI, MN, MO, OH), South (AL, DE, FL, KY, MD, MS, NC, OK, TX, VA, WV), and West (AZ, CA, WA).
Surgeon Information
Of the 55 cases studied, 49 had defendant specialty information ( Table 2 ). Of these 49 cases, the defendant was an otolaryngologist in 16 (28.57%) and a general surgeon in 33 (58.93%). Of the 33 cases against general surgeons, 3 (5.36%) had completed an endocrine fellowship; 3 (5.36%), an oncology fellowship; 2 (3.57%), a cardiothoracic fellowship; 1 (1.79%), a vascular fellowship; and 1 (1.79%), a head and neck fellowship. In 2 cases (3.57%), the defendant’s fellowship information was unknown. Of the 33 general surgeons, 21 (63.63%) did not have fellowship training. In this study, most litigation was against general surgeons who had not completed a fellowship training.
Table 2.
Specialty of Defendant.
| Specialty | No. of Cases | % |
|---|---|---|
| Otolaryngology | 16 | 28.57 |
| Unknown specialty | 6 | 10.71 |
| General surgery | 33 | 58.93 |
| No fellowship | 21 | 37.50 |
| Endocrine fellowship | 3 | 5.36 |
| Oncology fellowship | 3 | 5.36 |
| Cardiothoracic fellowship | 2 | 3.57 |
| Vascular fellowship | 1 | 1.79 |
| Head and neck fellowship | 1 | 1.79 |
| Unknown | 2 | 3.57 |
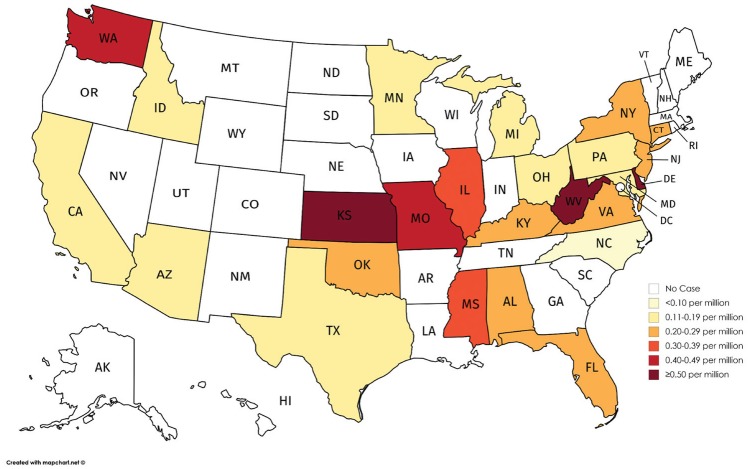
Geographic Distribution
The incidence of malpractice lawsuit was highest in the Southern states (39%), followed by the Midwestern states (27.27%; Table 1 , Figure 2 ). The Western states (20%) and the Northeastern states (18%) had the lowest incidence of malpractice lawsuits. VCP was the primary complication in 2 cases (18.18%) in the Northeast, 5 (45.45%) in the West, 10 (55.56%) in the South, and 11 (73.33%) in the Midwest (P = .0456).
Figure 2.
The rate of thyroidectomy malpractice cases reported per 1,000,000 state population from 1984 to 2018. Darker shades correspond to a higher number of cases.
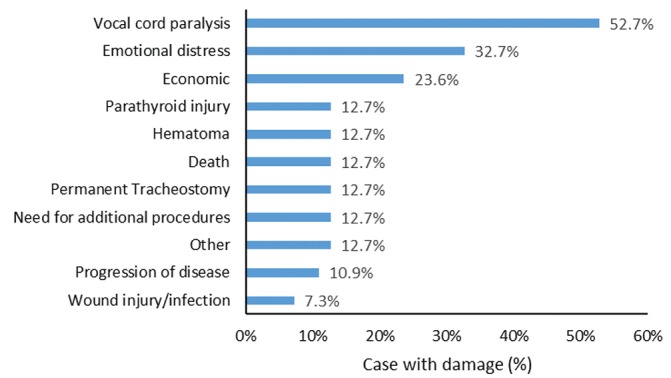
Damages
The most common complication leading to litigation was VCP (53%), followed by emotional distress (33%) and economic distress (24%; Figure 3 ). Many operations resulted in >1 damage leading to litigation; however, each case was categorized by the primary damage leading to litigation. The most common primary medical damage leading to litigation was VCP, in 28 of the 55 cases (50.91%; Table 1 ). This injury was reported as the primary damage in 7 cases (43.75%) treated by otolaryngologists and 17 (51.52%) by general surgeons ( Table 3 ). Of the 28 cases in which VCP was the primary damage, 12 were due to unilateral recurrent laryngeal nerve (RLN) injury, 11 to bilateral RLN injury, and 5 to an unknown RLN injury. Of the 12 unilateral RLN injuries, 3 cases were against otolaryngologists and 6 against general surgeons. Of the 11 bilateral RLN injuries, 1 case was against an otolaryngologist, 9 against general surgeons, and 1 against an unknown specialist. Of the 5 unknown RLN injuries, 3 cases were against otolaryngologists and 2 against general surgeons. Of the 9 cases of bilateral RLN injuries against general surgeons, 5 surgeons did not have fellowship training and 3 did. VCP was a complication reported in all age groups. The 31- to 40-year age group reported the highest incidence of VCP, in 4 of 6 cases (66.67%).
Figure 3.
Total damages reported in malpractice cases from thyroidectomies.
Table 3.
Association between Patient and Defendant Characteristics and Vocal Cord Paralysis (N = 55).
| Vocal Cord Paralysis, No. (%)a | |||
|---|---|---|---|
| Variable | With | Without | P Value |
| Age, y | .7922 | ||
| 11-30 | 4 (40.00) | 6 (60.00) | |
| 31-40 | 4 (66.67) | 2 (33.33) | |
| 41-50 | 3 (42.86) | 4 (57.14) | |
| 51-90 | 5 (62.50) | 3 (37.50) | |
| Unknown | 12 (50.00) | 12 (50.00) | |
| Sex | .1927 | ||
| Male | 1 (20.00) | 4 (80.00) | |
| Female | 27 (54.00) | 23 (46.00) | |
| Time of trial | .4544 | ||
| 1980-1989 | 6 (75.00) | 2 (25.00) | |
| 1990-1999 | 4 (44.44) | 5 (55.56) | |
| 2000-2009 | 12 (52.17) | 11 (47.83) | |
| 2010-2018 | 6 (40.00) | 9 (60.00) | |
| Surgeon specialty | .6101 | ||
| General surgery | 17 (51.52) | 16 (48.48) | |
| Otolaryngology | 7 (43.75) | 9 (56.25) | |
| Regionb | .0721 | ||
| Northeast | 2 (20.00) | 8 (80.00) | |
| Midwest | 11 (73.33) | 4 (26.67) | |
| South | 10 (52.63) | 9 (47.37) | |
| West | 5 (45.45) | 6 (54.55) | |
| Payment for plaintiff (n = 17) | .2685 | ||
| Mean (SD) | 2,156,128 (2,175,963) | 2,026,231 (4,173,401) | |
| Median (IQR) | 1,505,200 (402,823-3,797,000) | 295,000 (153,000-885,000) | |
| Payment for settlement (n = 7) | .3329 | ||
| Mean (SD) | 425,000 (282,843) | 2,305,000 (1,994,868) | |
| Median (IQR) | 425,000 (225,000-625,000) | 1,375,000 (1,300,000-4,100,000) | |
| Indemnity payment (n = 24) | .6394 | ||
| Mean (SD) | 1,809,902 (2,055,307) | 2,125,791 (3,458,612) | |
| Median (IQR) | 900,000 (309,645-2,594,000) | 817,500 (153,000-3,000,000) | |
Abbreviation: IQR, interquartile range.
Values are presented as No. (%) unless noted otherwise.
US Census Bureau–designated regions: Northeast (CT, NJ, NY, PA), Midwest (IL, IN, KS, MI, MN, MO, OH), South (AL, DE, FL, KY, MD, MS, NC, OK, TX, VA, WV), and West (AZ, CA, WA).
Other primary damages reported in litigation included progression of cancer, which was seen in 3 cases (18.75%) treated by otolaryngologists and 2 (6.06%) by general surgeons ( Table 4 ). Death was a complication in 3 cases (18.75%) treated by otolaryngologists and 3 (9.09%) by general surgeons. Parathyroid injury was an injury present in 1 case (6.25%) treated by an otolaryngologist and 5 (15.15%) by general surgeons. Less common and rare damages were included in the “other” category, as seen in 2 cases (12.50%) treated by otolaryngologists and 6 (18.18%) by general surgeons.
Table 4.
Association between Specialty and Primary Damages and Trial Outcome (n = 49).a
| Variable | General Surgery (n = 33) | Otolaryngology (n = 16) | P Value |
|---|---|---|---|
| Damage | .4682 | ||
| Vocal cord paralysis | 17 (51.52) | 7 (43.75) | |
| Parathyroid injury | 5 (15.15) | 1 (6.25) | |
| Death | 3 (9.09) | 3 (18.75) | |
| Progression of cancer | 2 (6.06) | 3 (18.75) | |
| Otherb | 6 (18.18) | 2 (12.50) | |
| Trial outcome | .7001 | ||
| Defense verdict | 18 (54.55) | 9 (56.25) | |
| Plaintiff verdict | 11 (33.33) | 4 (25.00) | |
| Settlement | 4 (12.12) | 3 (18.75) |
Values are presented as No. (%).
Wound injury (n = 3), coma (n = 2), infection (n = 1), emotional distress (n = 1), and brachial plexus injury (n = 1).
Verdict Outcome
The verdicts for the 55 cases included 31 (55.36%) in favor of the defense, 17 (30.36%) in favor of the plaintiff, and 7 (12.5%) settlements. In the 33 cases against general surgeons, there were 18 (54.55%) in favor of the defense, 11 (33.33%) in favor of the plaintiff, and 4 (12.12%) settlements. For the 16 cases reported against otolaryngologist, there were 9 (56.25%) in favor of the defense, 4 (25%) in favor of the plaintiff, and 3 (18.75%) settlements. The trial outcomes were similar between the specialties (P = .7001; Table 4 ).
In the cases that reported VCP as the primary damage, 18 (64.29%) ruled in favor of the defense and 8 (28.57%) in favor of the plaintiff, with 2 (7.14%) settlements. The majority of cases that closed with an indemnity payment included additional damages, such as lack of informed consent in 3 cases (30.00%) and permanent tracheostomy in 4 (40%). Cases that involved VCP as the primary damages were statistically more likely to be ruled in favor of the defense as opposed to the plaintiff (P = .0423). Out of the cases that reported parathyroid injury as the primary damage, 5 (71.43%) ruled in favor of the defense and 2 (28.57%) in favor of the plaintiff, with no settlements. In the cases that reported death as the primary damage, 3 (42.86%) ruled in favor of the defense, 4 (57.14%) ended in settlement, and 0 ruled in favor of the plaintiff. The progression of cancer was another primary damage, for which 2 (40%) cases ruled in favor of the defense, 3 (60%) cases ruled in favor of the plaintiff, and 0 cases ended in settlement. Injuries such as coma, infection, emotional distress, and brachial plexus injury and wound injury were placed in the “other” primary category. For this category, 3 cases (37.5%) ruled in favor of the defense, 4 (50%) ruled in favor of the plaintiff, and 1 (12.5%) case ended in a settlement ( Table 5 ).
Table 5.
Association between Primary Damages and Outcome (N = 55).a
| Primary Damage | Defense Verdict (n = 31) | Plaintiff Verdict (n = 17) | Settlement (n = 7) | P Value | P Value |
|---|---|---|---|---|---|
| Vocal cord paralysis | 18 (64.29) | 8 (28.57) | 2 (7.14) | .3507 | .0423b |
| Parathyroid injury | 5 (71.43) | 2 (28.57) | 0 (0.00) | .8524 | |
| Death | 3 (42.86) | 0 (0.00) | 4 (57.14) | .0033b | |
| Progression of cancer | 2 (40.00) | 3 (60.00) | 0 (0.00) | .3895 | |
| Otherc | 3 (37.50) | 4 (50.00) | 1 (12.50) | .4212 |
Values are presented as No. (%).
P < .05 (Fisher’s exact test).
Wound injury (n = 3), coma (n = 2), infection (n = 1), emotional distress (n = 1), and brachial plexus injury (n = 1).
Discussion
About 150,000 thyroidectomies are performed each year in the United States.19 Incidence of benign conditions and cancer of the thyroid requiring surgical intervention has increased in recent decades due to an aging population and an increase in diagnosis.5 Despite an increase in thyroidectomy procedures nationally,5 reported malpractice claims related to thyroidectomy were reported low, at 5.9 claims per 10,000 procedures.10 Most thyroidectomies in our study (43.6%) were performed for benign disease, including thyroid nodules, goiter, and thyroid dysfunction. This is likely due to improved diagnostic imaging and the resultant discovery of thyroid abnormalities, leading to an increase in surgery.5
The prevalence of thyroid disease is much higher in females than males, with 67% of thyroid disease occurring in females.20 Although thyroid diseases and surgery are more prevalent in the female population,20,21 the increased prevalence of thyroid disease in women does not account for the gender discrepancy in plaintiffs.22 Our study found that women (91%) were more likely than men to be the plaintiff. According to the Centers for Disease Control and Prevention, women are more likely to visit their doctor and seek treatment, which may account for the gender discrepancy.23
Regarding geographic variation of malpractice cases, the South had the highest incidence of total claims (33%), similar to what has been reported in the literature regarding malpractice claims in other specialties.15,24 The Northeast and the West, however, had the lowest incidence of malpractice cases related to thyroidectomy (20%). The geographic variation of malpractice cases may be a function of tort reform in the state, and other factors may play a role, such as state culture, additional cases not included in Westlaw, additional restrictions, and state supreme courts.25-27
In terms of the primary damage leading to the malpractice trials, VCP was the most common (54%). Despite being a known complication of thyroidectomy, it is still the most common complication leading to litigation.10,14-16,28 Litigation due to VCP mostly ruled in favor of the defense, in 18 of 28 cases (64.3%). However, out of the verdicts that favored the plaintiff (28.6%) or those that settled (7%), most were due to issues related to lack of informed consent (30%) or subsequent damages from permanent tracheostomy (40%), which is usually a result of bilateral nerve paralysis.
One of the most feared complications of thyroid surgery is bilateral nerve paralysis. In our study, we had a few individual examples of litigation involving bilateral VCP leading to devastating complications. For instance, a total thyroidectomy was performed on a 29-year-old woman that resulted in bilateral VCP, tracheostomy, speech, and respiratory problems. The patient had an additional procedure in which a nerve graft was attempted unsuccessfully. The verdict ruled in favor of the plaintiff with a sum of $1,175,000. Permanent tracheostomy is a devastating complication of bilateral RLN injury, which significantly affects a patient’s quality of life and expenditure of long-term supportive care. Patients at high risk of bilateral VCP should be particularly cautioned about potential life-changing sequelae if permanent tracheostomy is needed. Westlaw provides valuable information on individual malpractice cases. It is important to recognize what is important to the patient and to the jury.
Major debate exists among surgeons whether thyroid surgery should be staged in the setting of intraoperative RLN palsy or for high-risk cases, such as malignancy, retrosternal goiter, or Graves’ disease.29-33 The purpose of a staged thyroidectomy is to follow the patient postoperatively with laryngoscopy to establish vocal cord function before proceeding with completion surgery.33,34 In our study, of the 22 cases with VCP as the primary damage, 43% were due to unilateral RLN injury, and 39% were due to bilateral RLN injury. Most cases (6 of 11, 55%) with bilateral RLN injury resulted in permanent tracheostomy. We encourage surgeons to consider a staged procedure in high-risk cases or cases with signal loss. A staged or completion thyroidectomy can thus mitigate risks of not only a malpractice lawsuit but also the risk of losing the trial.32
Historically, thyroid disease has been managed by multiple specialties. Our study had 49 cases with defendant specialty information: 33 cases were against general surgeons and 16 against otolaryngologists. In addition, 14 of 16 (88%) cases against otolaryngologists occurred in the 2000-2020 period, coinciding with the increased role of the otolaryngologist in thyroid disease in recent decades.35 We found that the distribution of verdict outcome was similar between the defendant specialties. Saunders et al studied the National Inpatient Sample database and found that the majority (78%) of total thyroidectomies in the United States are performed by surgeons who focus <25% of their clinical practice on endocrine surgery.36 Loyo et al also identified a significant inverse relationship between surgeon volume and surgical complications and mortality in thyroidectomies.5 Further studies examining malpractice litigation and surgeon volume may be useful in the future.
Our study has several limitations. First, it is a database study; hence, the data are per the court record documentation, and accurate assessment of the medical status of the patients is not possible. Second, it was not possible to stratify the surgeons based on their case volumes or experience, since the information in that regard was limited. Third, while Westlaw consists of more medical malpractice cases than its competitors, there are still some limitations in the amount of cases that it provides. Westlaw consists of all federal and state court records that advance far enough for inclusion into publicly available records, which differs by jurisdiction. If a case does not proceed far enough before reaching a settlement, it will not be included in Westlaw. Consequently, we likely underestimated cases that were settled out of court before proceedings were initiated. However, many of the cases included in the Westlaw database are the written opinions of appellate courts. The appellate court decisions are critical to understanding a legal issue because these opinions determine how lower tribunals will decide similar issues in the future. Although Westlaw has limitations, it has been used in numerous medicolegal analyses across many specialties and has proved to be a tool in studying medical malpractice. Fourth, the geographic distribution analyzed does not account for the period of the legal database collection or the dynamic nature of each state’s litigation laws over time, as well as the underestimate of the total number of claims that are handled outside the courtroom.
This study highlights the patterns in thyroidectomy malpractice litigation in the United States from 1984 to 2018 and exemplifies an incremental increase in litigation over the last few decades. Despite being a known complication, RLN injury was the most common complication leading to trial, with most cases ruling in favor of the defense. However, the verdicts that settled or ruled in favor of the plaintiff were more likely a result of a lack of informed consent or bilateral VCP that ultimately led to permanent tracheostomy. We encourage surgeons to consider a staged procedure in high-risk cases or cases with signal loss. Surgeons should educate patients at high risk about potential complications that may drastically affect their quality of life.
Author Contributions
Megan L. Swonke, collected data, analyzed data, wrote article; Nasim Shakibai, collected data, wrote article; Mohamad R. Chaaban, designed study, revised article, concept and guidance.
Disclosures
Competing interests: None.
Sponsorships: None.
Funding source: None.
Acknowledgments
We acknowledge Lin-Na Chou, MS, statistician at the Department of Preventive Medicine and Community Health, The University of Texas Medical Branch, for assistance in statistical analysis of our data.
References
- 1. American Thyroid Association. General information/press room. https://www.thyroid.org/media-main/about-hypothyroidism/. Accessed May 20, 2018.
- 2. Reis LAG, Harkins D, Krapcho M, et al. SEER Cancer Statistics Review 1975-2003. Bethesda, MD: National Cancer Institute. [Google Scholar]
- 3. Ho TW, Shaheen AA, Dixon E, Harvey A. Utilization of thyroidectomy for benign disease in the United States: a 15-year population-based study. Am J Surg. 2011;201:570-574. [DOI] [PubMed] [Google Scholar]
- 4. Kern KA. Preventing the delayed diagnosis of breast cancer through medical litigation analysis. Surg Oncol Clin North Am. 1994;3:101-123. [Google Scholar]
- 5. Loyo M, Tufano RP, Gourin CG. National trends in thyroid surgery and the effect of volume on short-term outcomes. Laryngoscope. 2013;123(8):2056-2063. [DOI] [PubMed] [Google Scholar]
- 6. Vashishta R, Mahalingam-Dhingra A, Lander L, Shin EJ, Shah RK. Thyroidectomy outcomes: a national perspective. Otolaryngol Head Neck Surg. 2012;147(6):1027-1034. [DOI] [PubMed] [Google Scholar]
- 7. Bourrel C, Uzzan B, Tison P, et al. Transient hypocalcemia after thyroidectomy. Ann Otol Rhinol Laryngol. 1993;102(7):496-501. [DOI] [PubMed] [Google Scholar]
- 8. Ritter K, Elfenbein D, Schneider D, Chen H, Sippel RS. Hypoparathyroidism after total thyroidectomy: incidence and resolution. J Surg Res. 2015;197(2):348-353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sharma PK. Complications of thyroid surgery: practice essentials, overview, bleeding. Background, pathophysiology, etiology. https://emedicine.medscape.com/article/852184-overview. Published April 5, 2018. Accessed May 28, 2018.
- 10. Singer MC, Iverson KC, Terris DJ. Thyroidectomy-related malpractice claims. Otolaryngol Head Neck Surg. 2012;146(3):358-361. [DOI] [PubMed] [Google Scholar]
- 11. Mello MM, Studdert DM, Brennan TA. The new medical malpractice crisis. N Engl J Med. 2003;348(23):2281-2284. [DOI] [PubMed] [Google Scholar]
- 12. Kern KA. Medical malpractice involving colon and rectal disease: a 20-year review of United States civil court litigation. Dis Colon Rectum. 1993;36:531-539. [DOI] [PubMed] [Google Scholar]
- 13. Kern KA. Causes of breast cancer malpractice litigation: a 20-year civil court review. Arch Surg. 1992;127:542-547. [DOI] [PubMed] [Google Scholar]
- 14. Kern KA. Medicolegal analysis of errors in diagnosis and treatment of surgical endocrine disease. Surgery. 1993;114:1167-1174. [PubMed] [Google Scholar]
- 15. Abadin SS, Kaplan EL, Angelos P. Malpractice litigation after thyroid surgery: the role of recurrent laryngeal nerve injuries, 1989-2009. Surgery. 2010;148(4):718-723. [DOI] [PubMed] [Google Scholar]
- 16. Lydiatt DD. Medical malpractice and the thyroid gland. Head Neck. 2003;25(6):429-431. [DOI] [PubMed] [Google Scholar]
- 17. Ramsden JD, Johnson AP, Cocks HC, Watkinson JC. Who performs thryoidectomy: a review of current otolaryngological practice. Clin Otolaryngol Allied Sci. 2002;27(5):304-309. [DOI] [PubMed] [Google Scholar]
- 18. Terris DJ, Seybt MW, Siupsinskiene N, Gourin CG, Chin E. Thryoidectomy: changing patterns of practice. Laryngoscope. 2006;116(6):911-915. [DOI] [PubMed] [Google Scholar]
- 19. Al-Qurayshi Z, Robins R, Hauch A, Randolph GW, Kandil E. Association of surgeon volume with outcomes and cost savings following thyroidectomy: a national forecast. JAMA Otolaryngol Head Neck Surg. 2016;142(1):32-39. [DOI] [PubMed] [Google Scholar]
- 20. Tunbridge WMG, Evered DC, Hall R, et al. The spectrum of thyroid disease in a community: the Whickham Survey. Clinical Endocrinology. 1977;7(6):481-493. [DOI] [PubMed] [Google Scholar]
- 21. Rahbari R, Zhang L, Kebebew E. Thyroid cancer gender disparity. Future Oncol. 2010;6(11):1771-1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Chan WF, Lang BH, Lo CY. The role of intraoperative neuromonitoring of recurrent laryngeal nerve during thyroidectomy: a comparative study on 1000 nerves at risk. Surgery. 2006;140:866-872. [DOI] [PubMed] [Google Scholar]
- 23. Brett KM, Burt CW. Utilization of ambulatory medical care by women in the United States. Vital Health Stat. 2011;13(149):1-46. [DOI] [PubMed] [Google Scholar]
- 24. Thomas R, Gupta R, Griessenauer CJ, et al. Medical malpractice in neurosurgery: a comprehensive analysis. World Neurosurgery. 2018;110:e552-e559. [DOI] [PubMed] [Google Scholar]
- 25. Atkins A. Creating Minnesota: A History from the Inside Out. St Paul, MN: Minnesota Historical Society Press; 2008. [Google Scholar]
- 26. Sherman R, Moohr GS. Medical malpractice tort reform in Texas. Journal of Consumer and Commercial Law. 2009;12:142-150. [Google Scholar]
- 27. Talaska RJ, Brown C, Spencer AK. Texas medical malpractice: the plaintiff’s perspective. Advocate. 2016;77. [Google Scholar]
- 28. Dralle H, Sekulla C, Haerting J, et al. Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery. 2004;136(6):1310-1322. [DOI] [PubMed] [Google Scholar]
- 29. Randolph GW, Dralle H, Abdullah H, et al. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope. 2011;121(suppl 1):S1-S16 [DOI] [PubMed] [Google Scholar]
- 30. Dralle H, Sekulla C, Lorenz K, Thanh PN, Schneider R, Machens A. Loss of the nerve monitoring signal during bilateral thyroid surgery. BJS. 2012;99(8):1089-1095. [DOI] [PubMed] [Google Scholar]
- 31. Sadowski SM, Soardo P, Leuchter I, Robert JH, Triponez F. Systematic use of recurrent laryngeal nerve neuromonitoring changes the operative strategy in planned bilateral thyroidectomy. Thyroid. 2013;23(3):329-333. [DOI] [PubMed] [Google Scholar]
- 32. Goretzki P, Schwarz K, Brinkmann J, Wirowski D, Lammers B. The impact of intraoperative neuromonitoring (IONM) on surgical strategy in bilateral thyroid diseases: is it worth the effort? World J Surg. 2010;34(6):1274-1284. [DOI] [PubMed] [Google Scholar]
- 33. Christoforides C, Papandrikos I, Polyzois G, Roukounakis N, Dionigi G, Vamvakidis K. Two-stage thyroidectomy in the era of intraoperative neuromonitoring. Gland Surgery. 2017;6(5):453-463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Calò PG, Medas F, Conzo G, et al. Intraoperative neuromonitoring in thyroid surgery: is the two-staged thyroidectomy justified? Int J Surg. 2017;41:S13-S20. [DOI] [PubMed] [Google Scholar]
- 35. Chambers KJ, Bhattacharyya N. The increasing role of otolaryngology in the management of surgical thyroid disorders. Laryngoscope. 2013;123(12):3239-3242. [DOI] [PubMed] [Google Scholar]
- 36. Saunders BD, Wainess RM, Dimick JB, Doherty GM, Upchurch GR, Gauger PG. Who performs endocrine operations in the United States? Surgery. 2003;134(6):924-931. [DOI] [PubMed] [Google Scholar]