Abstract
Background
The effect of steroid use on outcomes in patients with cardiac arrest (CA) remains controversial. We systematically reviewed the literature to investigate whether steroid use after CA increased the return of spontaneous circulation (ROSC) rate and survival to discharge in patients with CA.
Methods
PubMed, Embase, CNKI, and the Cochrane Central Register of Controlled Trials were searched for randomized controlled trials (RCTs) and observational studies on the effect of steroid use on outcomes in adults with CA. The outcomes were ROSC and survival to discharge.
Results
Seven studies (four RCTs and three observational studies) were included. Pooled analysis suggested that steroid use was associated with increased ROSC in patients with CA. Steroid use was significantly associated with survival to discharge, which was a consistent finding in RCTs and observational studies. Subgroup analysis based on the time of drug administration (during cardiopulmonary resuscitation [CPR] vs. after CA) showed that steroid use during CPR and after CA were significantly associated with an increased rate of ROSC and survival to discharge.
Conclusion
Current evidence indicates that steroid use after CA could increase ROSC and survival to discharge in patients with CA. However, high-quality and adequately powered RCTs are warranted.
Keywords: Steroids, cardiac arrest, meta-analysis, return of spontaneous circulation, survival, cardiopulmonary resuscitation
Introduction
Cardiac arrest (CA) is a worldwide health problem, with an estimated annual incidence of 295,000 in the USA.1 Survival of patients after CA is very low.2 Patients who die after cardiopulmonary resuscitation (CPR) may have an inadequate adrenal response.3 Other studies have shown that relative adrenal insufficiency is common in patients with CA.4–6 Adrenal insufficiency is associated with poor outcome and increased mortality.
Several studies suggest that steroid use after CA could improve the return of spontaneous circulation (ROSC) rates and long-term survival.7,8 However, Tsai et al.8 conducted a prospective, nonrandomized, open-label clinical trial to examine the effect of hydrocortisone on out of hospital cardiac arrest (OHCA) outcomes. They found no significant difference in the rate of survival to discharge between the hydrocortisone and non-hydrocortisone groups.9 To date, studies reporting the effect of steroid use on outcomes after CA have showed conflicting results. Thus, it is necessary to examine the effectiveness of steroid administration in various medical facilities. In the present study, we conducted a systematic meta-analysis to investigate the association between steroid use and outcome in CA patients.
Materials and methods
Literature search and selection criteria
This study was conducted and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.10 PubMed, Embase, CNKI, and the Cochrane Central Register of Controlled Trials were searched based on the search strategy from 1 January 2000 to 1 March 2019. The search strategy was as follows: (“cardiac arrest” OR “heart arrest” OR “ventricular fibrillation” OR “cardiopulmonary resuscitation” OR “CA” OR “CPR”) AND (“steroid” OR “glucocorticoids” OR “adrenal cortex hormones” OR “hydrocortisone” OR “methylprednisolone” OR “dexamethasone”). We applied language restrictions of Chinese and English. Two independent investigators performed the initial search, deleted duplicate records, screened the titles and abstracts for relevance, and identified each as excluded or requiring further assessment. We included studies that were relevant to our PICO search strategy. The US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov; March 2019) and World Health Organization International Clinical Trials Registry Platform (WHO ICTRP) (apps.who.int/trialsearch/; March 2019) were searched for unpublished and ongoing studies, and the OpenGrey database (www.opengrey.eu; March 2019) was searched for grey literature. The reference sections from all studies that were retained during data extraction were searched as well as recent meta‐analyses and reviews on the topic (to March 2019). We also scanned conference proceedings from the American Society of Regional Anesthesia, European Society of Regional Anaesthesia, European Society of Anaesthesiology, and American Society of Anesthesiology up to 2019.
Studies meeting the following criteria were included: (1) population: adult patients with CA, with no exclusion for the cause of CA, and thus, trauma patients were among some of the included studies; (2) intervention: steroid use after CA; (3) comparison: no steroid use; (4) outcome: ROSC and survival to discharge; and (5) design: randomized controlled trials (RCTs) and observational studies (prospective or retrospective cohort studies). In accordance with the CPR guidelines, epinephrine was used in both the experimental and control groups, and thus, in both study types, experimental groups received both drugs (steroids and epinephrine) and control groups received epinephrine. In addition, each group may have received other drugs such as vasopressin. We excluded case reports, case series, review articles, and non-human studies.
Data extraction and quality assessment
Data extraction was performed by Q.Z. and confirmed independently by B.L. The following information was extracted from each study: first author, year of publication, country, study design, patient characteristics, number of patients enrolled, intervention, and outcome data. When the same patients were reported in several publications, we retained only the largest study to avoid duplication of the information. Discrepancies were resolved by discussion between the two investigators. The primary outcome was ROSC. The secondary outcome was survival to discharge. Two reviewers (Q.Z. and B.L.) independently assessed the methodological quality of each study using the Newcastle–Ottawa scale11 for prospective studies and the Cochrane Collaboration tool for RCTs.11
The GRADE approach
The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach was applied to provide an overall assessment of the evidence relating to all of the outcomes. A summary of findings was developed using the GRADEpro software (ims.cochrane.org/revman/other-resources/gradepro).
Statistical analysis
Review Manager (version 5.3; Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) was used for statistical analysis. Differences were expressed as the relative risk (RR) with the 95% confidence interval (CI). Heterogeneity across studies was tested using the I2 statistic, which is a quantitative measure of inconsistency across studies. Studies with an I2 statistic of 25% to 50% were considered to have low heterogeneity, those with an I2 statistic of 50% to 75% were considered to have moderate heterogeneity, and those with an I2 statistic of >75% were considered to have high heterogeneity. Considering the large clinical heterogeneity of included patients, a random effects model was used to explain the substantial clinical heterogeneity between studies. Potential publication bias was assessed by visual assessment of constructed funnel plots. A p-value <0.05 was considered to be significant. This study did not receive or require ethics approval and informed consent was not required because it was a meta-analysis.
Results
Study search and selection
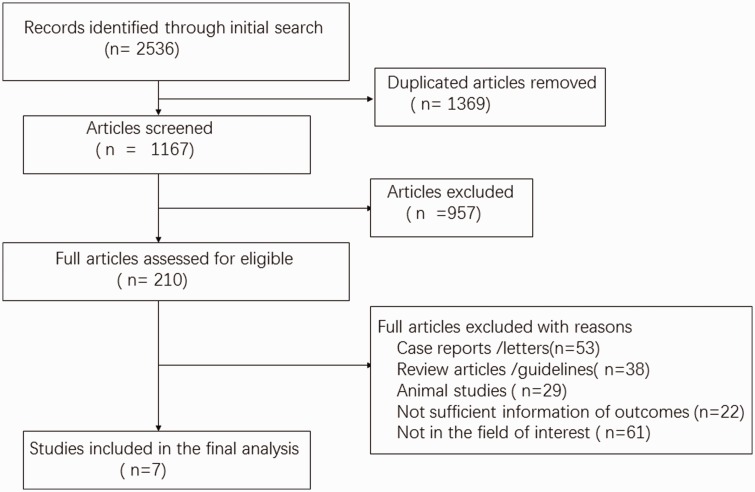
A flowchart of our search strategy and the reasons is shown in Figure 1. After identification and screening, 210 full-text studies were read for further evaluation and, among them, 203 were excluded because they did not report predefined outcomes or meet our inclusion criteria. Finally, seven studies were included in our analysis.
Figure 1.
Flowchart of the search strategy.
Study characteristics and quality
The main characteristics of the included studies are shown in Table 1, and the outcome data from each included study are shown in Table 2. We included seven studies7,8,12–16 in our analysis. These studies were published between 2001 and 2019. Among the included studies, three studies7,8,12 were published in English, and among these three studies, the steroid group received a combination of steroids with vasopressin and/or epinephrine. The other four studies were published in Chinese.13–16 Two studies8,12 were cohort studies, and the other five studies were RCTs.7,13–16 Among these studies, Zhang et al.13 used steroids and epinephrine in the steroid group, while the other studies used steroids in combination with atropine and epinephrine. Overall, there were 9414 patients included in the meta-analysis (3647 patients in the steroid group and 5767 patients in the non-steroid group).
Table 1.
Baseline characteristics of the included studies.
| Study | Year | Country/ Region | Study Design | Cause of CA | Age | Gender (male) | Endpoint | Epinephrine dosage | Vasopressin | Range year | Finding |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Tsai et al. | 2019 | Taiwan | Retrospective observational single centre | Nontraumatic OHCA, IHCA | Steroid 67.66 y; Non-steroid 67.51 y | Steroid 59.19%; Non-steroid 59.5% | Survival to discharge, 1-year survival | Steroid 5.68±5.27; Non-steroid 5.72±5.23 | Steroid 0.35%; Non-steroid 0.4% | 2004–2011 | Steroid use was associated with better survival to hospital discharge |
| Zhang et al. | 2015 | China mainland | RCT Single centre | Nontraumatic OHCA, IHCA | 65.7±19.6 y | 35% | ROSC, Survival to discharge | Steroid 9.03; Non-steroid 9.05 | – | 2011–2014 | Glucocorticoid use during CPR was associated with ROSC |
| Niimura et al. | 2017 | Japan | Retrospective observational single centre | OHCA | Steroid 51.43± 14.17 y; Non-steroid 51.30±13.19 y | Steroid 62%; Non-steroid 73% | Survival to discharge, ROSC | – | Steroid 8%; Non-steroid 1% | January 2005 and May 2014 | The results demonstrate a correlation between hydrocortisone administration and the high rate of survival to discharge. |
| Mentzelopoulos et al. | 2013 | Greece | RCT single centre | OHCA, IHCA | Steroid 63.2 y; Non-steroid 62.8 y | Steroid 63.8%; Non-steroid 73.1% | Survival to discharge, ROSC | – | – | September 1, 2008, to October 1, 2010 | Combined vasopressin–epinephrine and methylprednisolone during CPR resulted in improved survival to hospital discharge |
| Yang et al. | 2002 | China mainland | RCT, single centre | OHCAIHCA | 26–76 y | Steroid 57%; Non-steroid 52% | ROSC | – | – | – | Combined vasopressin–epinephrine and methylprednisolone during resuscitation improved ROSC |
| Mu et al. | 2014 | China mainland | Retrospective observationalSingle centre | Nontraumatic OHCA | – | – | ROSC | – | – | October 2004 to July 2005 | Administration of hydrocortisone during resuscitation, particularly within 6 minutes after ED arrival, may be associated with improved ROSC rate in OHCA patients |
| Wei et al. | 2001 | China mainland | RCT, single centre | Nontraumatic OHCA, IHCA | – | – | – | – | Combined vasopressin–epinephrine and methylprednisolone during CPR improved ROSC |
RCT, randomized controlled trial; ROSC, return of spontaneous circulation; OHCA, out of hospital cardiac arrest; IHCA, in hospital cardiac arrest.
Table 2.
Outcome data from included studies.
|
Survival to discharge |
ROSC |
|||
|---|---|---|---|---|
| Study | Steroid | Non-steroid | Steroid | Non-steroid |
| Tsai et al. (2019) | 828/3248 | 618/3248 | N | N |
| Mentzelopoulos et al. (2013) | 18/130 | 7/138 | 109/130 | 91/138 |
| Niimura et al. (2017) | 10/46 | 214/1771 | 15/61 | 325/2172 |
| Zhang et al. (2015) | 7/50 | 2/50 | 31/50 | 8/50 |
| Mu et al. (2014) | N | N | 18/31 | 19/47 |
| Yang et al. (2002) | N | N | 32/42 | 26/42 |
| Wei et al. (2001) | N | N | 65/85 | 42/71 |
ROSC, return of spontaneous circulation.
Quality assessment
The risk of bias of the RCTs ranged from low to high (two were low, two were medium, and one was high). Sources with a high risk of bias included sequence generation, allocation concealment, and other potential threats to validity. All five RCTs had a low risk for blinding of participants, personnel, and outcome assessors. A low risk of selective outcome reporting was achieved in five RCTs. A high risk of specific methodology for allocation concealment was described in three RCTs. A low risk of sequence generation was found in two RCTs. Based on the Newcastle-Ottawa Scale to assess the risk of bias in the cohort studies, two studies were rated as having a total score of >5, indicating a low risk of bias. Two studies7,16 achieved low risk, two studies13,15 achieved medium risk, and one study14 achieve high risk.
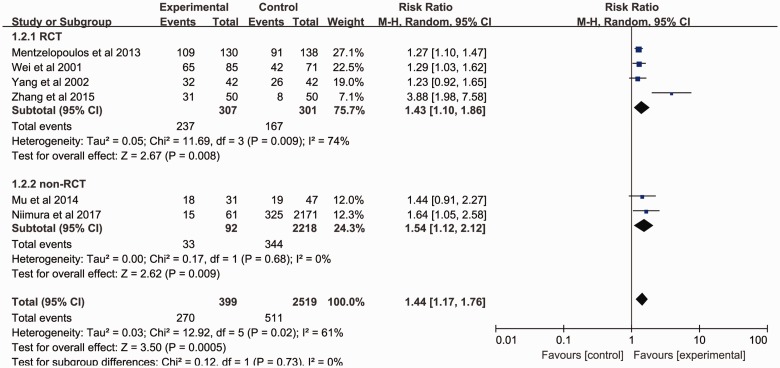
Primary outcome: ROSC
Six studies7,12–16 examined the association between steroid use and ROSC. Among these six studies, four studies were RCTs and two were cohort studies. The overall effect size (RR 1.44; 95%CI 1.17–1.76; P = 0.02) demonstrated a significant association between steroid use and ROSC. A subgroup analysis (RCTs vs. cohort studies) was also conducted. RCTs and cohort studies both revealed a significant association between steroid use and ROSC (RCT: RR 1.43; 95%CI: 1.10–1.86, P = 0.008; cohort studies: RR 1.54; 95%CI 1.12–2.12, P = 0.009). There was no significantly statistical heterogeneity between the subgroups based on a test of interaction (I2 = 0; Figure 2).
Figure 2.
Forest plot of the pooled effects of steroid use on ROSC in cardiac arrest patients.
df, degrees of freedom; M-H, Mantel–Haenszel; Experimental, steroid group; control, non-steroid group.
A subgroup analysis based on the time of steroid administration (during CPR vs. after CA) showed that steroid use during CPR was significantly associated with an increased rate of ROSC (RR 1.64; 95% CI 1.05–2.58, P < 0.005). Steroid use after CA was also significantly associated with an increased rate of ROSC (RR 1.42; 95% CI 1.13–1.77, P < 0.0001). One study [12] reported drug administration during CPR and five studies7,13–16 reported drug administration after CPR for the ROSC. Two studies7,12 reported drug administration during CPR and two studies8,13 reported drug administration after CPR for the result of survival to discharge.
Secondary outcomes: Survival to discharge
Four studies7,8,12,13 reported the association between steroid use and the outcome survival to discharge. When the four groups were pooled together (Figure 3), the effect size analysis (RR 1.67; 95% CI 1.16–2.40, P < 0.005) indicated that steroid use was significantly associated with an increased rate of survival to discharge. A subgroup analysis suggested that steroid use was associated with a significantly increased rate of survival to discharge in both the RCTs (RR, 2.89; 95% CI, 1.39–6.03, P = 0.005) and the observational studies (RR, 1.36; 95% CI, 1.21–1.52, P < 0.0001).
Figure 3.
Forest plot of the pooled effects of steroid use on survival to discharge in cardiac arrest patients.
df, degrees of freedom; M-H, Mantel–Haenszel; Experimental, steroid group; control, non-steroid group.
Subgroup analysis based on the time of drug administration (during CPR vs after CA) showed that use of steroid during CPR was significantly associated with increased rate of survival to discharge (RR 2.16; 95% CI 1.33–3.49, P < 0.05), use of steroid after CA was significantly associated with increased rate of survival to discharge (RR 1.35; 95% CI 1.23–1.48, P < 0.05).
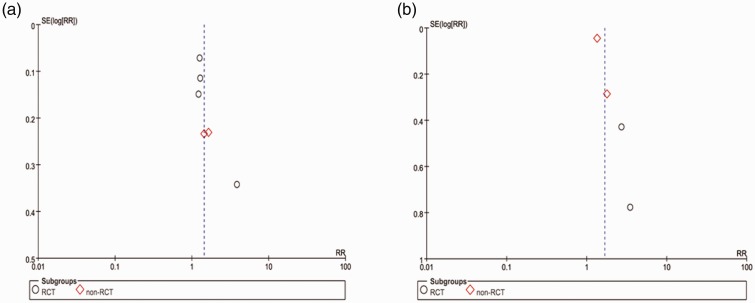
Publication bias
For the meta-analysis of the effect of steroid use on ROSC, there was no evidence of significant publication bias based on inspection of the funnel plot (Figure 4).
Figure 4.
a: Funnel plot of the effects of steroid use on ROSC in cardiac arrest patients. b: Funnel plot of the effects of steroid on survival to discharge in cardiac arrest patients.
GRADEpro summary of findings
The quality of evidence was assessed for ROSC and survival to discharge and there was no difference in the risk of bias for these parameters.
Discussion
This meta-analysis compares steroid use with placebo/no steroid use. In this study, we found that steroid use compared with no steroid use was associated with an improved ROSC rate and survival to discharge in patients with CA.
Various studies have shown that steroid supplementation during CPR may be beneficial by maintaining hemodynamic stability and enhancing myocardial function, thereby improving ROSC rates.17,18
The recovery of ROSC in CA patients leads to the global ischemia–reperfusion (I/R) injury, which includes excess free radical production, systemic inflammatory response, and an activated apoptosis pathway.19,20 Studies have shown that a low serum cortisol level was associated with unstable hemodynamics after ROSC and a shorter survival duration.21 Steroids also help to maintain cardiovascular stability by inhibiting catecholamine reuptake and the enhancing vascular response to vasopressors.22 The use of vasopressors increase the plasma cortisol concentration by improving perfusion to the adrenal cortex and medulla,17 which in turn helps to maintain vascular tone and enhance the effects of administered vasopressors.7
CA causes severe shock, and the interruption of blood flow leads to disruption of oxygen and metabolic substrate delivery, which affects every system including the immune system. CA patients present with a “sepsis-like” syndrome, which is characteristic of the high levels of circulating cytokines and the presence of endotoxin in plasma.19 Immune dysregulation is an important feature of OHCA patients after ROSC.19 Steroids could work through both immunologic and hemodynamic mechanisms, and steroids modulate the systemic inflammatory response.23 Previous animal studies have shown that steroids may preserve myocardial function and improve arterial reactivity.24,25 They also help to maintain cardiovascular stability by inhibiting catecholamine reuptake, enhancing vascular response to vasopressors, and decreasing nitric oxide-mediated vasodilation.22,26 Steroids have been reported to decrease oxidative stress,27 which was increased after CA.28 Previous studies have shown that myocardial apoptosis and lymphocyte apoptosis occur after CA.29,30 However, steroids could reduce apoptosis,31 and thus ameliorate post-resuscitation myocardial dysfunction.32 CA also leads to cerebral injury,33 and studies have shown that steroids could reduce cerebral injury.34 Steroids modulate the immune system, and they could theoretically affect the post-CA inflammatory response.
In this study on the effects of steroid use on ROSC in CA patients, the overall heterogeneity was low, but the subgroup heterogeneity (RCTs vs. cohort studies) was high. The effect of steroid use on survival to discharge was investigated in this meta-analysis, and the total heterogeneity was high, but the subgroup heterogeneity (RCTs vs. cohort studies) was low. The difference between RCTs and cohort studies may explain the heterogeneity. Thus, it is critical to improve the methodological quality of observational studies in future research. Among the included studies, the combination of steroids with different drugs and the drug dose may lead to substantial clinical heterogeneity. Additionally, further studies are required to uncover potential mechanisms of steroids in CA. However, more well-designed, randomized, double-blind, placebo-controlled trials are required.
Limitations
First, our analysis did not show an association between the steroid dose and clinical outcomes. A high degree of clinical heterogeneity may weaken the stability of the conclusions. Harmful effects of steroid use were not considered in our study, which may influence the clinical outcomes. Second, we included RCTs and observational studies. Observational studies have a high risk of selection bias and confounding by indication. Third, there are many types of steroids that are administered at various dosages. These may lead to the heterogeneity in a meta-analysis, but the included studies did not report these data, and additional subgroup analyses were not possible. Fourth, the largest study included in the present analysis was Tsai et al.,8 which enrolled more patients than the all remaining studies combined. However, the primary outcome of the present analysis did not include that study. This may have led to bias in the primary outcome.
Conclusion
Current evidence indicates that steroid use increases the rate of ROSC and survival to discharge in patients with CA. Steroid use may remain an acceptable option for patients with CA; however, high-quality and adequately powered RCTs are warranted.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD
Chunsheng Li https://orcid.org/0000-0002-3161-4457
References
- 1.Soar J, Maconochie I, Wyckoff MH, et al. 2019 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations: Summary From the Basic Life Support; Advanced Life Support; Pediatric Life Support; Neonatal Life Support; Education, Implementation, and Teams; and First Aid Task Forces. Circulation 2019; 140: e826–e880. [DOI] [PubMed] [Google Scholar]
- 2.Sasson C, Rogers MA, Dahl J, et al. Predictors of survival from out-of-hospital cardiac arrest: A systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes 2010; 3: 63–81. [DOI] [PubMed] [Google Scholar]
- 3.O’Brien CE, Santos PT, Reyes M, et al. Association of diastolic blood pressure with survival during paediatric cardiopulmonary resuscitation. Resuscitation 2019; 143: 50–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hekimian G, Baugnon T, Thuong M, et al. Cortisol levels and adrenal reserve after successful cardiac arrest resuscitation. Shock 2004; 22: 116–119. [DOI] [PubMed] [Google Scholar]
- 5.Kim JJ, Hyun SY, Hwang SY, et al. Hormonal responses upon return of spontaneous circulation after cardiac arrest: A retrospective cohort study. Crit Care 2011; 15: R53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pene F, Hyvernat H, Mallet V, et al. Prognostic value of relative adrenal insufficiency after out-of-hospital cardiac arrest. Intensive Care Med 2005; 31: 627–633. [DOI] [PubMed] [Google Scholar]
- 7.Mentzelopoulos SD, Malachias S, Chamos C, et al. Vasopressin, steroids, and epinephrine and neurologically favorable survival after in-hospital cardiac arrest: A randomized clinical trial. JAMA 2013; 310: 270–279. [DOI] [PubMed] [Google Scholar]
- 8.Tsai MS, Chuang PY, Huang CH, et al. Postarrest steroid use may improve outcomes of cardiac arrest survivors. Crit Care Med 2019; 47: 167–175. [DOI] [PubMed] [Google Scholar]
- 9.Tsai MS, Huang CH, Chang WT, et al. The effect of hydrocortisone on the outcome of out-of-hospital cardiac arrest patients: A pilot study. Am J Emerg Med 2007; 25: 318–325. [DOI] [PubMed] [Google Scholar]
- 10.Knobloch K, Yoon U, Vogt PM. Preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement and publication bias. J Craniomaxillofac Surg 2011; 39: 91–92. [DOI] [PubMed] [Google Scholar]
- 11.Zhao L, Li C, Liu B, et al. The association of gasping and outcome, in out of hospital cardiac arrest: A systematic review and meta-analysis. Resuscitation 2015; 97: 7–12. [DOI] [PubMed] [Google Scholar]
- 12.Niimura T, Zamami Y, Koyama T, et al. Hydrocortisone administration was associated with improved survival in Japanese patients with cardiac arrest. Sci Rep 2017; 7: 17919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang F, Yang ZJ, Shen J, et al. Adrenaline combined with methylprednisolone sodium succinate Cardiopulmonary resuscitation. Chinese Clinical Medicine 2015; 22: 670–671. http://med.wanfangdata.com.cn/Paper/Detail?id=PeriodicalPaper_zglcyx201505026&dbid=WF_QK. [Google Scholar]
- 14.Yang GL, Li CX. Clinical study on comprehensive medication for cardiopulmonary cerebral resuscitation. National Coal Industry Medical Journal 2002; 5: 379–380. http://med.wanfangdata.com.cn/Paper/Detail?id=PeriodicalPaper_zgmtgyyxzz200204065&dbid=WF_QK. [Google Scholar]
- 15.Mu CJ, Li WQ, Zhou YM, et al. Hydrocortisone sodium succinate for cardiopulmonary resuscitation the influence of patient prognosis. Chinese Journal of Integrated Traditional and Western Medicine 2014; 21: 229–231. http://med.wanfangdata.com.cn/Paper/Detail?id=PeriodicalPaper_zgzxyjhjjzz201403030&dbid=WF_QK. [Google Scholar]
- 16.He WX, Hong Z. Application of high-dose adrenaline combined with aminophylline, of clinical study of cardiopulmonary cerebral resuscitation with dexamethasone. Chinese Emergency Medicine 2001; 21: 224–225. http://med.wanfangdata.com.cn/Paper/Detail?id=PeriodicalPaper_zgjjyx200104016&dbid=WF_QK. [Google Scholar]
- 17.Kornberger E, Prengel AW, Krismer A, et al. Vasopressin-mediated adrenocorticotropin release increases plasma cortisol concentrations during cardiopulmonary resuscitation. Crit Care Med 2000; 28: 3517–3521. [DOI] [PubMed] [Google Scholar]
- 18.Lindner KH, Haak T, Keller A, et al. Release of endogenous vasopressors during and after cardiopulmonary resuscitation. Heart 1996; 75: 145–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adrie C, Adib-Conquy M, Laurent I, et al. Successful cardiopulmonary resuscitation after cardiac arrest as a “sepsis-like” syndrome. Circulation 2002; 106: 562–568. [DOI] [PubMed] [Google Scholar]
- 20.Tsai MS, Huang CH, Tsai CY, et al. Ascorbic acid mitigates the myocardial injury after cardiac arrest and electrical shock. Intensive Care Med 2011; 37: 2033–2040. [DOI] [PubMed] [Google Scholar]
- 21.Schultz CH, Rivers EP, Feldkamp CS, et al. A characterization of hypothalamic-pituitary-adrenal axis function during and after human cardiac arrest. Crit Care Med 1993; 21: 1339–1347. [DOI] [PubMed] [Google Scholar]
- 22.Oppert M, Schindler R, Husung C, et al. Low-dose hydrocortisone improves shock reversal and reduces cytokine levels in early hyperdynamic septic shock. Crit Care Med 2005; 33: 2457–2464. [DOI] [PubMed] [Google Scholar]
- 23.van Leeuwen HJ, van der Bruggen T, van Asbeck BS, et al. Effect of corticosteroids on nuclear factor-kappaB activation and hemodynamics in late septic shock. Crit Care Med 2001; 29: 1074–1077. [DOI] [PubMed] [Google Scholar]
- 24.Liakopoulos OJ, Teucher N, Muhlfeld C, et al. Prevention of TNFalpha-associated myocardial dysfunction resulting from cardiopulmonary bypass and cardioplegic arrest by glucocorticoid treatment. Eur J Cardiothorac Surg 2006; 30: 263–270. [DOI] [PubMed] [Google Scholar]
- 25.Mansart A, Bollaert PE, Giummelly P, et al. Effects of dexamethasone and L-canavanine on the intracellular calcium-contraction relation of the rat tail artery during septic shock. Am J Physiol Heart Circ Physiol 2006; 291: H1177–H1182. [DOI] [PubMed] [Google Scholar]
- 26.Matsumura M, Kakishita H, Suzuki M, et al. Dexamethasone suppresses iNOS gene expression by inhibiting NF-kappaB in vascular smooth muscle cells. Life Sci 2001; 69: 1067–1077. [DOI] [PubMed] [Google Scholar]
- 27.Hall ED. Neuroprotective actions of glucocorticoid and nonglucocorticoid steroids in acute neuronal injury. Cell Mol Neurobiol 1993; 13: 415–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nagase M, Sakurai A, Sugita A, et al. Oxidative stress and abnormal cholesterol metabolism in patients with post-cardiac arrest syndrome. J Clin Biochem Nutr 2017; 61: 108–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xiao HL, Zhao LX, Yang J, et al. Imbalance of angiotensin-converting enzymes affects myocardial apoptosis during cardiac arrest induced by acute pulmonary embolism in a porcine model. Int J Mol Med 2019; 43: 1575–1584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gu W, Zhang Q, Yin W, et al. Caspase-3-mediated splenic lymphocyte apoptosis in a porcine model of cardiac arrest. Am J Emerg Med 2014; 32: 1027–1032. [DOI] [PubMed] [Google Scholar]
- 31.Bishopric NH, Andreka P, Slepak T, et al. Molecular mechanisms of apoptosis in the cardiac myocyte. Curr Opin Pharmacol 2001; 1: 141–150. [DOI] [PubMed] [Google Scholar]
- 32.Wynsen JC, Preuss KC, Gross GJ, et al. Steroid-induced enhancement of functional recovery of postischemic, reperfused myocardium in conscious dogs. Am Heart J 1988; 116: 915–925. [DOI] [PubMed] [Google Scholar]
- 33.Hou X, Li C, Gu W, et al. Effect of Shenfu on inflammatory cytokine release and brain edema after prolonged cardiac arrest in the swine. Am J Emerg Med 2013; 31: 1159–1164. [DOI] [PubMed] [Google Scholar]
- 34.Katz L, Vaagenes P, Safar P, et al. Brain enzyme changes as markers of brain damage in rat cardiac arrest model. Effects of corticosteroid therapy. Resuscitation 1989; 17: 39–53. [DOI] [PubMed] [Google Scholar]