Abstract
Background
Caesarean rates increased in different parts of the world, rising from 20% to 33% in the USA and from 40% to 55% in Brazil between 1996 and 2011; however, there was no reduction in morbimortality rates. Several factors have been suggested as responsible for this increase, such as health judicialisation, fear of the painful process on the patients’ part and reduction of medical training in vaginal delivery and labour complications. It is urgent to reverse this process and, therefore, a model of actions was created with the intention of engaging the team in order to reduce caesarean rates in a Brazilian hospital.
Methodology
The model was based on the following actions: encouragement of labour analgesia; execution of written reports of any cardiotocographic examination; plan-do-study-act cycles for nursing orientations about the positions that favour pregnant women during labour; creation of a birth induction form; monthly feedback with physicians and nurses on caesarean rates achieved; verification of the caesarean rate by medical staff with individual feedback; daily round of medical coordination for case discussions; disclosure of caesarean rates on hospital posters; and constant dissemination of literature with strategies to reduce caesarean delivery. This plan of action started in January 2016. The mean caesarean section rate in the 31 months preceding the interventions (period A) was then compared with the 31 subsequent months (period B).
Results
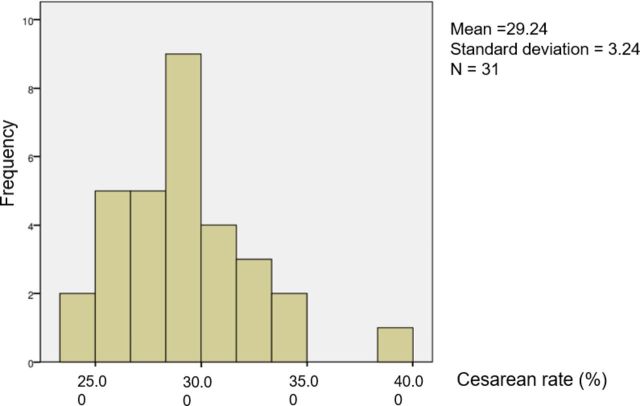
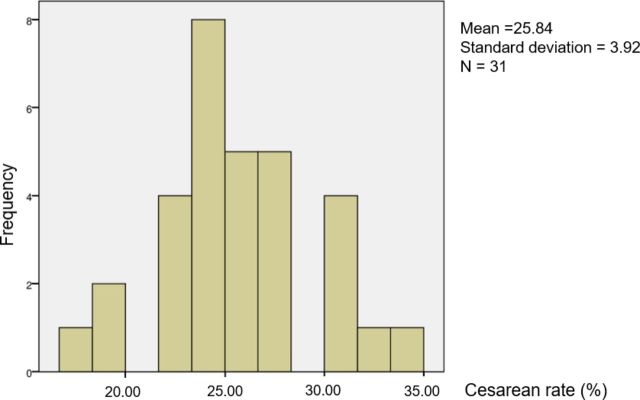
Both periods presented caesarean rates with normal distribution. The mean caesarean rate was 29.24% (range: 38.69%–23.89%, SD 3.24%) vs 25.84% (range: 17.96%–34.97%, SD 3.92%, p<0.05), respectively, for periods A and B.
Conclusion
After the implementation of the plan of action, there was a reduction in caesarean rates in this hospital.
Keywords: obstetrics and gynecology, healthcare quality improvement, cesarean delivery, patient safety, quality improvement
Introduction
Overall rates of caesarean sections have shown a substantial increase over the years. In the USA, for example, there was an increase from just over 20% in 1996 to almost 33% in 2011.1 In Brazil, a country with very high rates of caesarean section births, the situation was even more critical, with an increase from 40% to almost 55% in the same period for both the public and private systems. However, considering only the private health system, the values exceeded 80%.2
The clinical benefits of this practice cannot be proven, as the increase in caesarean sections was not accompanied by a reduction in neonatal mortality and morbidity.3 These data, added to the risks involved in the procedure, reveal that caesarean sections are being overused. Unnecessary caesarean sections increase the risk of maternal death by 3.7 times and the risk of amniotic embolism by almost 5 times, for example. In addition, they promote respiratory issues in the new-born and anomalous insertions of the placenta in subsequent pregnancies.1
Besides that, caesarean sections are associated with higher rates of admission of new-borns to neonatal intensive care units, longer hospital stays and greater use of human resources for assistance found in this type of delivery.4 5 For American Medicaid, the costs involved in a caesarean section, including prenatal, childbirth and postnatal care are on average US$13 590 per event, while for vaginal deliveries this cost is about US$9131, meaning 30% lower.6
It is difficult to establish what led to the current indiscriminate use of caesarean sections, but some factors include the judicialisation of health, the fear of a painful process by patients and a reduction in vaginal delivery training. Regardless of these factors, there is a challenge to reduce these indices, not neglecting the necessary use of the procedure which should occur in 15%–18% of cases, including when there is placenta previa or fetal distress.7 Work models centred on the physician, which occur in countries such as Brazil, may also be one of the factors involved as this makes the assistance more interventionist.8
Thus, there is a worldwide concern on how to reverse this process. One of the main examples is the initiative of the Institute for Healthcare Improvement, which in partnership with Hospital Israelita Albert Einstein and Agência Nacional de Saúde Suplementar (ANS—a national governmental agency that regulates the Brazilian health system), launched Programa Parto Adequado, aiming to change this reality there. Similarly, in 2012, the American College of Obstetricians and Gynaecologists published strategies for safe reduction in first caesarean sections.9
Among the main strategies described for the reduction of caesarean sections are those that involve the understanding of what are the abnormal evolutions of labour (dystocia), especially in its last stage, which decreases the probability of vaginal birth. Consequently, the diagnostic method and proper management of these conditions are essential.10–14
Likewise, the use of assisted vaginal delivery techniques, that is, forceps and vacuum extraction, is described as a way of reducing caesarean rates, although its use has been decreasing over time. In the USA in 1992, approximately 12% of vaginal births required assisted vaginal delivery techniques, which decreased to 7.5% in 2006, a period in which there was an increase in caesarean sections.15 Moreover, the use of forceps and vacuum extractors is not associated with higher risks of neonatal mortality or intracranial haemorrhage when compared with caesarean section.10 Even though these procedures are considered safe, they are not routinely applied during medical residency training. Therefore, such training needs to be reinstated, especially with advances in realistic simulation.12
As fetal distress is one of the most common causes of caesarean sections, the analysis of systematised vitality is considered fundamental for reducing the number of procedures. Generally, this analysis is performed through the intermittent auscultation of fetal heartbeats and by periodic cardiotocography examination, which is a graphical record of fetal beats and uterine activity over time. Thus, presenting protocols that govern the use of these tools as well as their interpretation and subsequent conduct are actions that are also proposed to reduce caesarean rates.9
Finally, we can also mention strategies suggested in literature to increase vaginal births: establishing the maximum estimated fetal weight accepted to allow normal birth, incentivating the practice of labour induction and encouraging and training for vaginal birth in twins in which the first fetus is cephalic, because in these cases, the risks do not seem to be greater than in single pregnancies.13–16
New diagnostic tools are needed with objective criteria for indications of birth by caesarean section. One issue is disseminating information to the team that provides birth assistance and encouraging a change in behaviour required to reduce caesarean sections.
With this objective, an action model was created with the aim of engaging birth teams to reduce the rate of caesarean sections in a Brazilian hospital (Hospital Geral de Itapecerica da Serra).
Methodology
This study was designed using the SQUIRE 2.0 guidelines (Standards for Quality Improvement Reporting Excellence), which was validated internationally by the scientific community.
Scenario and participants
A plan of action to improve caesarean section rates was established in January 2016 at the General Hospital of Itapecerica da Serra, which is part of the public health system, located in the state of São Paulo, Brazil. This service has approximately 200 births per month and is a reference hospital for high-risk pregnancies in the region. All pregnant women who gave birth at the hospital from June 2013 to July 2018 were included in the study.
The participants were the entire care team in the maternity ward, including doctors, nurses, nursing technicians and coordinators. They were duly guided and trained so that they could put the action plan into practice.
Intervention
First, in order to engage the whole team with the aim of reducing the rate of caesarean sections, several meetings with the leaders of each sector at the General Hospital of Itapecerica da Serra. These were held to clarify the importance of the objective in improving the maternal-fetal care, as well as the importance of each person’s role in the change process.
The plan involved a group of actions that were initially designed by the coordinators based on literature research and inspired by other successful similar experiences.17–20 During the process of execution, all actions were improved with the experience and knowledge of the team, which included the doctors, nurses, nursing technicians, coordinators and even the pregnant women who went into labour in General Hospital of Itapecerica da Serra in that period. To make this possible, a monthly meeting was established with the leadership team to assess difficulties and review protocols.
During the initial analysis of the caesarean rates in the hospital, it was noticed that even though the service had a team of anaesthetists on standby, a short number of vaginal deliveries happened with anaesthesia. In order to understand why it happens, doctors, nurses and puerperal patients were called. To our surprise, while the majority of the healthcare group had the belief that anaesthesia harms the evolution for a normal delivery, most patients did not even know that it was possible to deliver without such pain. Besides that, one of the mothers’ main distress in relation to delivery is the fear of pain, which sometimes makes them beg for a caesarean section. It is known that an effective epidural analgesia is associated with a prolonged second stage of labour, but this is not associated with an increase in adverse maternal or neonatal outcomes21 Moreover, the labour analgesia increases maternal satisfaction, which helps to spread the benefits of vaginal delivery and contributes with the goal to reduce caesarean sections.22
For that reason, one of the first actions carried out was to encourage labour analgesia by raising the awareness of the care team as well as guiding and disclosing the possibility of delivery with less pain to the patients since hospital admission. For that, posters about labour analgesia were placed on the hospital information board.
Another action put into effect was nursing training on the positions that favour fetal rotation and descent, as well as encouraging pregnant women during labour. This was done through a plan-do-study-act cycle, which is a scientifically validated method for healthcare quality improvement.23 24 The nurse leader planned training based on scientific literature concerning the different positions that help women during labour. Then, an explanation about all these positions was given to one chosen nurse and it was applied in several labours for 3 days. Feedback from the nurse in training, as well as from the women in labour was given in order to improve the techniques. One barrier raised at this stage was the parturient’s fear of causing harm to the baby when they took certain positions. This was solved by performing a periodic check of the fetal heartbeat every 15 min during the first stage of labour and every 5 min during the second stage of labour, when the cervical dilation is complete (10 centimetres), until the delivery of the neonate.25 Another resolution adopted was the creation of written reports of any cardiotocographic examination that was performed either by the physician or by the nursing staff, which allowed labour to be attended more safely. These reports were included in the medical records and were audited monthly by a medical record committee.
Finally, all the other maternity nurses were trained on mothers’ positions and were encouraged to empower the pregnant women to move during the labour process in order to support easier and safer births. Besides that, a team of experts from the hospital joined to create a protocol of birth induction based on the latest evidence from literature and adapted it for their reality. It was thought after an observation that an expressive number of indications for caesarean in our service were due to overrated failure of induction. A form was designed and disclosed to the whole team in order to encourage the doctors, nurses and even the patients to complete the whole cycle of induction of labour before declaring its failure.
The coordinators also implemented monthly feedback to physicians and nurses on the caesarean section rates achieved in the previous month. They also verified these rates with the medical team, through individual feedback. After that, they disclosed the data and exposed it on posters in the hospital.
Furthermore, a daily medical coordination round was introduced to check the hospitalised pregnant women and discuss the critical cases with the team. Besides that, literature dissemination with strategies to reduce caesarean sections and new concepts in obstetrics were performed in monthly scientific meetings. Moreover, a recycling course was offered to the whole team annually in order to improve techniques (eg, operative vaginal delivery) and update knowledge.
Measurements and data analysis
Once this action plan was defined, the analysis was divided into two periods to compare the caesarean section rates, with period A comprising of the 31 months prior to the adopted actions and period B comprising of the 31 months subsequent to the adopted actions.
The groups were compared regarding the average age of the participants, average gestational age, average birth weight, percentage of multiple pregnancies and sex of the infants. The neonatal outcome was also compared between the groups through 5 min Apgar scores.
The monthly caesarean section rates in each period were then individually subjected to visual analysis of histograms, and the Shapiro-Wilk test was performed using IBM SPSS Statistics Subscription software (11–2018) to verify data normality. Normal distributions were considered tests with p>0.05.
Next, the caesarean section rates for both periods were compared using two independent sample t-tests for equality of mean. A difference was considered significant when the two-tailed p was less than 0.05.
Results
The main characteristics of the studied population divided by periods A and B are summarised in table 1. Regarding maternal age, more than 80% of women were between 19 and 29 years of age in both groups.
Table 1.
Studied population divided by age group, type of pregnancy, fetus gender, 5 min Apgar score, fetal birth weight and gestational age at birth in both study periods (A and B)
| Period A | Period B | |
| n (%) | n (%) | |
| Age group (years) | ||
| <18 | 918 (15.14%) | 694 (11.51%) |
| 19–29 | 3375 (55.68%) | 3398 (56.33%) |
| 30–39 | 1561 (25.75%) | 1726 (28.61%) |
| >40 | 207 (3.42%) | 214 (3.55%) |
| Type of pregnancy | ||
| Singleton | 5854 (96.58%) | 5837 (96.77%) |
| Twin | 207 (3.42%) | 192 (3.18%) |
| Trigeminal | 0 (0.00%) | 3 (0.05%) |
| Fetus gender | ||
| Male | 3172 (52.33%) | 3039 (50.38%) |
| Female | 2887 (47.63%) | 2993 (49.62%) |
| Ignored | 2 (0.03%) | 0 (0.00%) |
| 5th minute Apgar score | ||
| <7 | 85 (1.40%) | 97 (1.61%) |
| ≥7 | 5975 (98.58%) | 5928 (98.28%) |
| Uninformed | 1 (0.02%) | 7 (0.12%) |
| Fetal birth weight | ||
| <1500 g | 135 (2.22%) | 128 (2.2%) |
| 1500–2499 g | 661 (10.98%) | 670 (11.1%) |
| >2500 g | 5261 (86.80%) | 5234 (86.77%) |
| Gestational age at birth | ||
| <37 weeks | 838 (13.82%) | 851 (14.12%) |
| >37 weeks | 5177 (85.42%) | 5151 (85.39%) |
| Ignored | 46 (0.76%) | 30 (0.50%) |
For both groups, approximately 96% of pregnancies were singleton, and slightly more than 50% were male fetuses. Regarding neonatal outcomes assessed by 5 min Apgar scores, there was no significant difference between groups.
In terms of weight and gestational age at birth, in both groups, more than 80% of fetuses were full-term and weighed more than 2500 g.
For period A, the mean caesarean section rate was 29.24%, with a median of 28.9%, ranging from 23.89% to 38.69%, and a SD of 3.24%. For period B, the mean caesarean section rate was 25.84%, with a median of 25.70%, ranging from 17.96% to 34.97% and a SD of 3.92%. Figures 1 and 2, in the form of histograms, corroborate the normal distribution in both groups.
Figure 1.
Histogram of the temporal distribution of caesarean rates in period A.
Figure 2.
Histogram of the temporal distribution of caesarean rates in period B.
Although the graphs show a clear normal distribution of values and the groups have an n>30, which allows application of the central limit theory, the Shapiro-Wilk test was applied to numerically confirm the normal distribution of the data in both groups. The values found for group A and group B were 0.954 and 0.960, respectively.
Given that the data for the two groups had a normal distribution, the two independent sample t-tests were used to verify if there was a significant difference in mean between the periods. The results are provided in table 2. Note that the difference in mean between the groups was statistically significant (p<0.001), considering an acceptable error of less than 5% (p<0.05).
Table 2.
Statistical comparison of caesarean rates between period A and B
| Caesarean rates | ||
| Period A | Period B | |
| Mean (%) | 29.2369 | 25.8364 |
| Median (%) | 28.9100 | 25.7009 |
| Variance (%) | 10.466 | 15.358 |
| Standard deviation (%) | 3.23514 | 3.91891 |
| Observations | 31 | 31 |
| T-test | P<0.001 | |
Additionally, in the same period, there was an increase in the rate of labour analgesia from 9.37% on average in period A to 17.09% on average in period B. Similarly, the two independent sample t-tests to determine mean differences indicated a statistically significant difference with a p value less than 0.05 (p<0.001) (table 3).
Table 3.
Statistical comparison of labour analgesia rates between period A and B
| Labour analgesia | ||
| Period A | Period B | |
| Mean (%) | 9.3707 | 17.0981 |
| Median (%) | 9.3700 | 16.47 |
| Variance (%) | 15.1226 | 34.4926 |
| Standard deviation (%) | 3.8887 | 5.873 |
| Observations | 31 | 31 |
| T-test | P<0.01 | |
Discussion
As initially explained, caesarean section rates have been increasing worldwide, and this increase is a major concern in countries where the rates are historically high, as in Brazil.1 2 In these cases, a vicious cycle tends to form because with reduced vaginal births, there is less training and practical experience in procedures relate to that delivery method, perpetuating caesarean sections. This phenomenon can be observed through the smaller number of instrumentalised vaginal births over time.11
The peculiarities of delivery assistance models, including within the same country, hinder general actions to reduce caesarean sections. However, in a study by Vogt et al, multidisciplinary care of pregnant women during labour improves the labour experience and reduces caesarean section rates.8 For this reason, in the model developed in this study, it was decided for nurses to be those responsible for the rates achieved by disseminating and applying feedback from the results to them. One goal was to increase their skills in monitoring labour, especially during the expulsive period because prolonged delivery and cephalopelvic disproportion are among the main indications of operative delivery.7 11 26
The sustainability of the plan of action was also addressed as the actions themselves would end up without long-term improvements. Consequently, new protocols of induction of labour and fetal monitoring during labour were included in the medical record so nurses and doctors need to fill it for all deliveries. These data are monthly audited through a 10% sampling by a medical record committee. That also applies to cardiotocography analysis by nurses and doctors, who must sign the examination.
Besides that, the head nurse personally supervises the conduct around 5% of deliveries performed by the nurses of her team and reports to the hospital management in order to bring difficulties and propose improvements. Considering that an important limitation of a quality improvement intervention in practice is the engagement of the team, we believe that individual feedbacks and that close attention to everyone’s performance ensures the perpetuity of these actions.
Additionally, a strong motivation for our team to follow the rules is that the correct filling of the medical records is part of our professional’s performance evaluation. The increase in the number of caesarean sections (currently over 30%, but periodically reviewed) also leads to a reduction in financial transfers to the Hospital by the State, and that can be extended to the professionals involved.
The low disclosure of Zhang’s studies, which broke Friedman’s partogram paradigm as a more appropriate form of childbirth care, was considered a contributing factor for high caesarean section rates.11 For this reason, the disclosure of new scientific concepts among the teams most likely made them more lenient to the slower progression of cervical dilatation.
Notwithstanding, the daily rounds and case discussion with the multidisciplinary team also served as guiding principles for cases where traditionally a more plausible option would be caesarean section. For instance, this applied to macrosomic fetuses, functional dystocia and a prolonged expulsion phase, although with an evolution time slower than that acceptable by the ACOG.1 8–11 Besides that, the rounds and discussion played roles in standardising and updating the interpretation of cardiotocography, with a likely influence on the classification of fetal distress.
Performing cardiotocographic examinations in written form on a medical record for subsequent auditing results in a detailed and very objective assessment of the required data, with a more assertive orientation of the adopted approach, especially due to the established learning curve.27
A study by Stoll et al that included more than 3600 women in eight countries from different cultures (Australia, Canada, Chile, England, Germany, New Zealand, Australia and Iceland) showed that fear of pain is one of the main reasons for caesarean section preference.28 In an attempt to mitigate this problem, the proposed model included the expansion of the use of labour analgesia and notably, its increase was accompanied by an increase in vaginal delivery rates. Educational campaigns for pregnant women regarding their rights to pain relief played a crucial role.
Unfortunately, it was not possible to assess the impact of each action in isolation in the present model, but the data show their effectiveness together, especially considering that the two study samples were similar and comparable. Team turnover did not impact the caesarean section rate until the implementation of the cited measures, which leads us to the conclusion that such measures most likely generated reliable results.
For monetary reasons, it was not possible to test this action plan using realistic simulation. However, realistic simulation would allow for training and resumption of actions that are currently less frequent in obstetric practice, such as operative vaginal delivery and external cephalic inversions. In addition, it provides greater training to midwives because it presents excellent practice for the management of complications associated with vaginal delivery.29 30
It should be noted that perinatal outcomes, assessed by the 5 min Apgar score, remained unchanged with the increase in vaginal delivery rates. This means that the increased use of this method met the safety requirements and that caesarean sections were most likely performed without being required.
Footnotes
Contributors: RN conceived and designed the improvement actions and wrote the manuscript. RDSF and RSA implemented the planned actions and wrote the manuscript. CATD analysed the data.
Funding: The authors themselves funded this research.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article.
References
- 1.American College of Obstetricians and Gynecologists (College), Society for Maternal-Fetal Medicine, Caughey AB, et al. Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol 2014;210:179–93. 10.1016/j.ajog.2014.01.026 [DOI] [PubMed] [Google Scholar]
- 2.Ministério da Saúde / DATASUS Brazilian Health Unic System Department of Informatics [internet homepage – accessed in June 2019]. Available: http://www2.datasus.gov.br/DATASUS/index.php?area=02
- 3.Gregory KD, Jackson S, Korst L, et al. Cesarean versus vaginal delivery: whose risks? whose benefits? Am J Perinatol 2012;29:7–18. 10.1055/s-0031-1285829 [DOI] [PubMed] [Google Scholar]
- 4.Leite ACP, Araujo Júnior E, Helfer TM, et al. Comparative analysis of perinatal outcomes among different typesof deliveries in term pregnancies in a reference maternity of Southeast Brazil. Ceska Gynekol 2016;81:54–7. [PubMed] [Google Scholar]
- 5.Etringer AP, Pinto MFT, Gomes M. Análise de custos dA atenção hospitalar AO parto vaginal E cesariana eletiva para gestantes de risco habitual no Sistema Único de Saúde. Ciênc. saúde coletiva 2019;24. [DOI] [PubMed] [Google Scholar]
- 6.Truven Health Analytics The cost of having a baby in the United States, 2013. Available: http://transform.childbirthconnection.org/wp-content/uploads/2013/01/Cost-of-Having-aBaby-Executive-Summary.pdf
- 7.Molina G, Weiser TG, Lipsitz SR, et al. Relationship between cesarean delivery rate and maternal and neonatal mortality. JAMA 2015;314:2263–70. 10.1001/jama.2015.15553 [DOI] [PubMed] [Google Scholar]
- 8.Vogt SE, Silva KSda, Dias MAB. Comparison of childbirth care models in public hospitals, Brazil. Rev Saude Publica 2014;48:304–13. 10.1590/s0034-8910.2014048004633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spong CY, Berghella V, Wenstrom KD, et al. Preventing the first cesarean delivery: summary of a joint Eunice Kennedy Shriver National Institute of child health and human development, Society for Maternal-Fetal medicine, and American College of obstetricians and Gynecologists workshop. Obstet Gynecol 2012;120:1181–93. 10.1097/aog.0b013e3182704880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Werner EF, Janevic TM, Illuzzi J, et al. Mode of delivery in nulliparous women and neonatal intracranial injury. Obstet Gynecol 2011;118:1239–46. 10.1097/AOG.0b013e31823835d3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Powell J, Gilo N, Foote M, et al. Vacuum and forceps training in residency: experience and self-reported competency. J Perinatol 2007;27:343–6. 10.1038/sj.jp.7211734 [DOI] [PubMed] [Google Scholar]
- 12.Little SE, Edlow AG, Thomas AM, et al. Estimated fetal weight by ultrasound: a modifiable risk factor for cesarean delivery? Am J Obstet Gynecol 2012;207:309.e1–309.e6. 10.1016/j.ajog.2012.06.065 [DOI] [PubMed] [Google Scholar]
- 13.Lee HC, Gould JB, Boscardin WJ, et al. Trends in cesarean delivery for twin births in the United States: 1995-2008. Obstet Gynecol 2011;118:1095–101. 10.1097/AOG.0b013e3182318651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barrett JF, Hannah ME, Hutton EK, et al. A randomized trial of planned caesarean or vaginal delivery for twin pregnancy: twin birth study Collaborative group. N Engl Med 2013;369:1295–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Srinivas SK, Epstein AJ, Nicholson S, et al. Improvements in US maternal obstetrical outcomes from 1992 to 2006. Med Care 2010;48:487–93. 10.1097/MLR.0b013e3181d68840 [DOI] [PubMed] [Google Scholar]
- 16.Powell J, Gilo N, Foote M, et al. Vacuum and forceps training in residency: experience and self-reported competency. J Perinatol 2007;27:343–6. 10.1038/sj.jp.7211734 [DOI] [PubMed] [Google Scholar]
- 17.Torres JA, Domingues RMSM, Sandall J, et al. Caesarean section and neonatal outcomes in private hospitals in Brazil: comparative study of two different perinatal models of care. Cad Saude Publica 2014;30 Suppl 1:S1–12. 10.1590/0102-311x00129813 [DOI] [PubMed] [Google Scholar]
- 18.Borem P, Ferreira JBB, da Silva UJ, et al. [Increasing the percentage of vaginal birth in the private sector in Brazil through the redesign of care model]. Rev Bras Ginecol Obstet 2015;37:446–54. 10.1590/SO100-720320150005264 [DOI] [PubMed] [Google Scholar]
- 19.Kingdon C, Downe S, Betran AP. Women's and communities' views of targeted educational interventions to reduce unnecessary caesarean section: a qualitative evidence synthesis. Reprod Health 2018;15:130. 10.1186/s12978-018-0570-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kingdon C, Downe S, Betran AP. Non-Clinical interventions to reduce unnecessary caesarean section targeted at organisations, facilities and systems: a qualitative evidence synthesis of stakeholders' views. PLoS One 2018;13:e0203274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Turner J, Flatley C, Kumar S. Epidural use in labour is not associated with an increased risk of maternal or neonatal morbidity when the second stage is prolonged. Aust N Z J Obstet Gynaecol 2019;12 10.1111/ajo.13045 [DOI] [PubMed] [Google Scholar]
- 22.Lim G, Facco FL, Nathan N, et al. A review of the impact of obstetric anesthesia on maternal and neonatal outcomes. Anesthesiology 2018;129:192–215. 10.1097/ALN.0000000000002182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leis JA, Shojania KG. A primer on PDSA: executing plan-do-study-act cycles in practice, not just in name. BMJ Qual Saf 2017;26:572–7. 10.1136/bmjqs-2016-006245 [DOI] [PubMed] [Google Scholar]
- 24.Knudsen SV, Laursen HVB, Johnsen SP, et al. Cuality of care? A systematic review of reported effects and methodological rigor in plan-do-study-act projects. BMC Health Serv Res 2019;19:683. 10.1186/s12913-019-4482-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.American College of Obstetricians and Gynecologists ACOG practice Bulletin No. 106: intrapartum fetal heart rate monitoring: nomenclature, interpretation, and general management principles. Obstet Gynecol 2009;114:192–202. 10.1097/AOG.0b013e3181aef106 [DOI] [PubMed] [Google Scholar]
- 26.Begum T, Rahman A, Nababan H, et al. Indications and determinants of caesarean section delivery: evidence from a population-based study in Matlab, Bangladesh. PLoS One 2017;12:e0188074. 10.1371/journal.pone.0188074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Devane D, Lalor J. Midwives' visual interpretation of intrapartum cardiotocographs: intra- and inter-observer agreement. J Adv Nurs 2005;52:133–41. 10.1111/j.1365-2648.2005.03575.x [DOI] [PubMed] [Google Scholar]
- 28.Stoll KH, Hauck YL, Downe S, et al. Preference for cesarean section in young nulligravid women in eight OECD countries and implications for reproductive health education. Reprod Health 2017;14:116. 10.1186/s12978-017-0354-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dupuis O, Moreau R, Silveira R, et al. A new obstetric forceps for the training of junior doctors: a comparison of the spatial dispersion of forceps blade trajectories between junior and senior obstetricians. Am J Obstet Gynecol 2006;194:1524–31. 10.1016/j.ajog.2006.01.013 [DOI] [PubMed] [Google Scholar]
- 30.Crofts JF, Lenguerrand E, Bentham GL, et al. Prevention of brachial plexus injury-12 years of shoulder dystocia training: an interrupted time-series study. BJOG 2016;123:111–8. 10.1111/1471-0528.13302 [DOI] [PubMed] [Google Scholar]