Abstract
Background
Innovation is important to improve patient care, but few studies have explored the factors that initiate change in healthcare organizations.
Methods
As part of the European project EPICE on evidence-based perinatal care, we carried out semi-structured interviews (N = 44) with medical and nursing staff from 11 randomly selected neonatal intensive care units in 6 countries. The interviews focused on the most recent clinical or organizational change in the unit relevant to the care of very preterm infants. Thematic analysis was performed using verbatim transcripts of recorded interviews.
Results
Reported changes concerned ventilation, feeding and nutrition, neonatal sepsis, infant care, pain management and care of parents. Six categories of drivers to change were identified: availability of new knowledge or technology; guidelines or regulations from outside the unit; need to standardize practices; participation in research; occurrence of adverse events; and wish to improve care. Innovations originating within the unit, linked to the availability of new technology and seen to provide clear benefit for patients were more likely to achieve consensus and rapid implementation.
Conclusions
Innovation can be initiated by several drivers that can impact on the success and sustainability of change.
Introduction
Innovation was defined as “the intentional introduction and application within a role, group or organisation, of ideas, processes, products or procedures new to the relevant unit of adoption”,1 regardless of the time elapsed since development or availability in the marketplace. In the healthcare field, innovations typically include new services, ways of working or technologies directed at improving the health outcomes, cost-effectiveness, administrative efficiency, or user’s experience.2,3 According to Greenhalgh et al.,3 an important element of healthcare innovation is implementation “by planned and coordinated actions”.
Implementing innovation, including the abandoning of ineffective or obsolete practices,4 is crucial to improve the effectiveness and safety of health care.5 However, “invention is hard but dissemination is even harder”,6 and the slow or uneven adoption of innovation has been frequently reported.6,7
Theoretical models of change7 have identified different primary catalysts for the adoption of innovation including the recognition of the need to change, as indicated by “unfreezing the target behaviour” in Lewin’s change theory8 or “establishing a sense of urgency” in Kotter’s eight-step process;9 the innovation characteristics in Rogers’ diffusion theory;10 and the balance between benefits and costs of adoption according to the risk-based framework.11 Focussing on implementation, the Consolidated Framework for Implementation Research (CFIR) has provided a comprehensive and pragmatic structure to promote theory development and effectiveness verification across multiple contexts.12 However, studies providing empirical data about the factors that initiate change in healthcare organizations or the relation between the origin of innovation and the success of implementation are few.13
We carried out a qualitative study with physicians and nurses to explore how clinical or organizational innovations are introduced and implemented in neonatal intensive care units (NICUs), a setting characterized by extreme patient fragility, complex technological environment, highly specialized multidisciplinary personnel. This paper focusses on the initial motive for change, broadly defined as the reasons, goals or events that started the process leading to actual clinical or organizational innovation.
Methods
This study is part of the “Effective Perinatal Intensive Care in Europe” project (EPICE, https://epiceproject.eu) on the use of evidence-based interventions in perinatal care in 19 regions of 11 European countries.14 For this study, we involved one region from each country with resources to carry out qualitative interviews and analysis: the Eastern region in Denmark, Ile-de-France in France, Hesse in Germany, Lazio in Italy, Northern Region in Portugal and East Midlands in the UK. In each region, we stratified the NICUs according to academic status (yes/no) to ensure variability in terms of organization and policies of care, resources, involvement in research and training. We then randomly selected two NICUs per region within these strata. In each NICU, we interviewed two physicians and two nurses with experience of at least 3 years clinical work in that unit. Priority was given to staff with involvement or interest in evidence-based medicine. We focused on physicians and nurses because the presence of other professionals (e.g. physiotherapists, psychologists) in NICU teams may vary between countries. Additionally, these professionals are often attached to different hospital units and provide only consulting or part-time work in NICU. We had no explicit refusals. However, in Denmark, only one unit was able to schedule the interviews within the study period.
The study was approved by the Ethics Committees in all regions. Signed informed consent by informants was obtained except in Denmark and France, where the Committees waived the requirement.
Data collection
We carried out 44 individual semi-structured interviews in local language, focussing on the most recent clinical or organizational innovation introduced in the unit regarding care of very preterm infants (VPT, <32 weeks of gestation). We broadly referred to the theory of organizational change outlined by Pettigrew,15 emphasizing the categories of content (“what has changed”), context (inner and outer) and process of change, including the actions, reactions and interactions of the various interested parties. We developed an interview guide to ensure standardization across units and interviewers. The guide followed a chronological order starting with the content of the change and the main initial motive, or driver, for introducing it; the planning, dissemination and implementation phases; compliance and perceived benefits of the innovation. Pilot interviews carried out in Italy, France, Portugal and UK and discussions within the study team were used to finalize the guide. A 2-day training workshop was held for interviewers to standardize the conduct of the interviews and methods of transcribing and analysing the data.
Interviews were carried out by appointment at the informant’s hospital, and were recorded and fully transcribed anonymously.
Data analysis
We used thematic analysis to identify the patterns across the dataset (“themes”) relevant to the description and motives for change.16 The analysis was performed in two stages to address the challenges of our multilingual sample. Firstly, at regional level each interviewer carried out an initial coding of the raw data using a common scheme based on the interview guide and supplemented with additional codes emerging from the data and shared within the coding team. The coded text was then translated into English for the second stage of analysis, which was carried out at the coordinating centre in Italy by E.F. and M.C. E-mail discussions between the interviewers and the Italian team were used to check the interpretation of results.
Similar themes continued to emerge in all NICUs after the first half of the interviews, indicating saturation.
The analyses were performed using the NVivo10 software (QSR International, Australia).
Results
The characteristics of NICUs and informants are presented in Tables 1 and 2, respectively. The 11 selected NICUs were diverse with respect to structural and functional organization, including number of cots and admissions, provision of specialized services, and use of protocols and guidelines. Most informants (n = 35) were females. The mean interview duration differed by profession (34 min for physicians and 44 for nurses) and country, with longer interviews in the UK and Italy.
Table 1.
Characteristics of the participating NICUs (n = 11).
| Size, type of patients and night/weekend staffing | |
| Official number of intensive care cots (median, range) | 9 (3–13) |
| Number of annual admissions (median, range) | 511 (436–1083) |
| Annual number of babies requiring mechanical ventilation (median, range) | 96 (32–399) |
| Admission of older babies/children (n, %) | 4 (36) |
| Staff on-call available to come to the unit on week nights (n, %) | 7 (64) |
| Staff on-call available to come to the unit on weekend nights (n, %) | 7 (64) |
| Staff on-call available to come to the unit on weekend days (n, %) | 7 (64) |
| Specialized procedures and services in NICU hospital (yes) | |
| High frequency ventilation (n, %) | 11 (100) |
| Inhaled nitric oxide therapy (n, %) | 9 (82) |
| Neonatal surgery (n, %) | 9 (82) |
| PDA surgery (n, %) | 7 (64) |
| Human milk bank (n, %) | 6 (55) |
| ROP treatment (n, %) | 5 (45) |
| Neurosurgery (n, %) | 5 (45) |
| Renal dialysis (n, %) | 4 (36) |
| Use of protocols/guidelines in NICU | |
| Breastfeeding and human milk use (n, %) | 11 (100) |
| ROP screening (n, %) | 11 (100) |
| PDA treatment (n, %) | 10 (91) |
| Brain ultrasound screening protocol (n, %) | 10 (91) |
| Follow-up of very preterm infants (n, %) | 10 (91) |
| Surfactant use (n, %) | 9 (82) |
| Oxygen saturation targets (n, %) | 9 (82) |
| Use of mechanical ventilation (n, %) | 8 (73) |
| Hypothermia prevention in the delivery room (n, %) | 7 (64) |
| Use of CPAP (n, %) | 7 (64) |
| Use of postnatal corticosteroids (n, %) | 6 (55) |
| ROP treatment (n, %) | 6 (55) |
| Use of caffeine to prevent BPD (n, %) | 6 (55) |
| Developmental care (n, %) | 6 (55) |
| PDA prophylaxis (n, %) | 5 (45) |
| Use of erythropoietin (n, %) | 5 (45) |
| Withdrawal or withholding of treatment for extremely preterm babies (n, %) | 4 (36) |
| Use of vitamin A to prevent BPD (n, %) | 2 (18) |
| Use of probiotics (n, %) | 1 (9) |
| Care of parents | |
| Free parental visiting (24h/day) (n, %) | 6 (55) |
| Routine skin-to-skin care (n, %) | 9 (82) |
BPD bronchopulmonary dysplasia, CPAP continuous positive airways pressure, PDA patent ductus arteriosus, ROP retinopathy of prematurity
Table 2.
Demographic and professional characteristics of informants.
| Denmark | France | Germany | Italy | Portugal | UK | Total | ||
|---|---|---|---|---|---|---|---|---|
| n. | n. | n. | n. | n. | n. | n. | % | |
| Gender | ||||||||
| Male | 1 | 2 | 2 | 1 | 1 | 2 | 9 | 20.5 |
| Female | 3 | 6 | 6 | 7 | 7 | 6 | 35 | 79.5 |
| Age (years) | ||||||||
| 30–39 | 0 | 3 | 0 | 0 | 4 | 0 | 7 | 15.9 |
| 40–49 | 1 | 3 | 3 | 6 | 1 | 4 | 18 | 40.9 |
| ≥50 | 3 | 2 | 5 | 2 | 3 | 4 | 19 | 43.2 |
| Directive role (yes)a | ||||||||
| Physicians | 1 | 3 | 2 | 0 | 1 | 2 | 9 | 40.9 |
| Nurses | 1 | 1 | 2 | 1 | 1 | 3 | 9 | 40.9 |
| Total years of experience in Neonatal Intensive Care: mean (SD) | ||||||||
| Physicians | 20.0 (−) | 17.5 (8.8) | 18.5 (9.1) | 22.5 (9.1) | 17.5 (8.7) | 18.0 (5.0) | 18.9 (7.4) | |
| Nurses | 22.5 (4.9) | 13.0 (9.5) | 29.3 (7.4) | 20.8 (3.2) | 14.5 (8.3) | 23.8 (6.4) | 20.4 (8.6) | |
| Total years of experience in this unit: mean (SD) | ||||||||
| Physicians | 19.0 (−) | 10.5 (3.9) | 17.8 (8.2) | 20.8 (11.1) | 15.0 (9.1) | 14.3 (4.3) | 15.8 (7.6) | |
| Nurses | 20.0 (1.4) | 9.3 (6.4) | 28.5 (6.2) | 13.8 (7.5) | 13.8 (8.9) | 22.3 (9.0) | 17.7 (9.4) | |
| Length of interview (min): mean (SD) | ||||||||
| Physicians | 28 (4) | 28 (2) | 19 (3) | 43 (13) | 37 (14) | 45 (16) | 34 (13) | |
| Nurses | 38 (6) | 33 (18) | 39 (20) | 48 (9) | 36 (10) | 67 (25) | 44 (20) | |
aRow proportions
Table 3 shows the reported innovations. For physicians, the most frequently reported changes concerned ventilation, followed by feeding and nutrition, and by infant care and pain management. This latter was the most frequently reported by nurses, who also discussed the care of parents.
Table 3.
Topics of the changes reported by the informants.
| Physicians | Nurses |
|---|---|
| Ventilation (n. 9): | Infant care and pain management (n. 6): |
| Initial infant stabilization through non-invasive ventilation | Establishment of the kangaroo care method (n. 2) |
| Introduction of Targeted Tidal Volume ventilation | Change of infant bathing schedule |
| Use of High Flow Nasal Cannula for ventilation weaning | Introduction of kinaesthetic infant handling |
| Introduction of high-flow nasal cannula oxygen (Optiflow) | Review of discharge procedure for the Neonatal Unit |
| Use of RAM cannulas for CPAP | Neonatal pain assessment and treatment guideline |
| Increase of oxygen saturation limits for ventilated infants (up to 95%) (n. 3) | Ventilation (n. 5): |
| Protocol for improvement of trainees’ intubation skills | Use of new fastening system for ventilated babies (CPAP) |
| Enteral and parenteral feeding/nutrition (n. 6): | Guideline for adjusting neopuff according to ventilator settings |
| Change of feeding schedule (n. 2) | Development of protocol for difficult intubation cases |
| Lowering GA for use of raw customized maternal milk (from ≥32 to ≥28 weeks | Introduction of Targeted Tidal Volume ventilation |
| Use of fresh maternal milk (versus frozen) | Use of apnoea monitoring element in Infant Flow System |
| Request of parenteral nutrition bags before birth, based on anticipated baby birthweight (n. 2) | Enteral feeding/nutrition (n. 4): |
| Infant care and pain management (n. 3): | Use of fresh maternal milk (n.2) |
| Establishment of protocol for kangaroo care | Feeding with raw and customized milk since 28 weeks gestation (n. 2) |
| Pain assessment and treatment based on use of pain scales | Care of parents (n.2): |
| Transfer from incubator to open cot | Increased parental involvement in infant care |
| Neonatal infections (n. 2): | Protocol for first communication with parents at the time of NICU admission |
| Implementation of NICE guidelines for neonatal sepsis | Other (n. 5): |
| Guideline for vancomycin dosing and monitoring | Management of umbilical catheter |
| Other (n. 2): | Heart disease screening: preductal and postductal saturation |
| Pharmacological treatment of PDA | Mandatory documented daily inspection of the unit resuscitation equipment |
| Guideline for the treatment of umbilical granuloma | New administration rules after change of drug name and producer |
| Introduction of NICE guidelines on phototherapy |
GA gestational age, PDA patent ductus arteriosus, CPAP continuous positive pressure ventilation, NICE National Institute for Health and Care Excellence
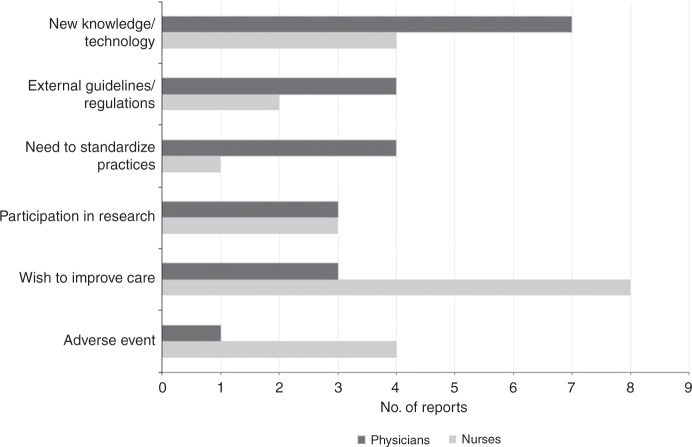
Six “themes” emerged from the data in relation to the initial main motive for change (Fig. 1). Again, nurses were more likely to report care-related motives, while physicians appeared more sensitive to the availability of new knowledge and technology.
Fig. 1.
Main reported motives for change by profession.
Availability of new knowledge or technology
Findings in scientific literature, attendance at conferences and informal opportunities to exchange information with colleagues were reported as main triggers for change by seven physicians and four nurses.
The idea has emerged from the literature. Since some years we have managed respiratory distress in very premature infants in a fairly systematic way by intubation and surfactant administration. And then new randomised trials appeared in the literature showing that stabilization of these infants by non-invasive ventilation could avoid intubation and unnecessary administration of surfactant, because these children did not need it. […] So it’s a real change of practice. (Physician/France/9)
New staff arriving from other hospitals were also a source of innovative ideas, and often took the lead in promoting implementation:
…we’ve been aware that other units had been using a different mode of infant ventilation and also this consultant came from a unit where that was being used. So we were sort of fairly happy that it’s not going to do any harm and might have the potential to do some good. […] This consultant I mentioned actually took ownership of it, did produce a guideline. (Physician/UK/25)
The availability of innovative technology, such as new equipment, was a very strong driver for change:
A very recent change that, I really believe, has modified quite a bit our management, both for physicians and nurses, are the RAM cannulas for nasal ventilation. They allow us to use a high flow and apply pressure both during inspiration and expiration. […] The previous system was more powerful, but more aggressive. (Physician/France/14)
While most of the new technology mentioned concerned ventilation, other types of equipment were also reported:
…as now there is an easy-to-use machine that allows us to analyse every time the lipid, protein and carbohydrate content [of mother’s milk], well we do it, everything is analysed and we will know exactly what we are doing. Because we know that maternal milk is perfect for preemies, but it does not exactly meet the needs of the premature baby. Thus we give what is called a fortifier. (Physician/France/35)
Considering the advantages of a technology and obtaining the resources to acquire it may take time, but its adoption seems to raise little resistance, and benefit from easy implementation:
We had attended a conference as a team and looked at the equipment, and thought that it would be something really good. […] We spoke to the representatives there and had a quote, and decided that this was something we were going to buy. (Physician/UK/1)
Thus if one finds something easier at the technical level, which seems as effective, one wants to use it. That’s it. (Physician/France/14)
Guidelines and regulations from outside the NICU
Change may be motivated by factors external to the unit, such as a new guideline or regulation issued by official agencies:
So with NICE, they get a national launch and when they come out, you are told by commissioners that you need… you need to find a way to meet this guideline. And then we would usually adapt the national guideline into a local policy. (Physician/UK/38)
Because there is a regulation on the use of breast milk that is very clear and very strict and does not allow the use of raw frozen-thawed milk within a hospital service. It is possible at home but not in the hospital because of obvious bacteriological reasons and so, there you go, it was imperative that we follow the rules and not be outside of bounds. (Physician/France/13).
The guidelines produced by scientific or professional groups seem to be more acceptable that those issued by official agencies, particularly when some of the staff had been involved in the process:
…a [hospital] pediatric pain group was created, including the various sub-specialties at the level of paediatrics. I am the coordinator of the group, myself and nurse X, the nurses are obviously involved, in fact they are the ones who are with the children and carry out the pain assessment and administer the medications, basically. (Physician/Portugal/18)
For the NICU, this was
… an opportunity to bring some things up to date, things which were being done but there was no proper protocol. (Physician/Portugal/18)
In contrast, guidelines issued by official agencies were viewed as more bureaucratic, and possibly less appropriate to the unit patients and care. They appeared to encounter more resistance, particularly when there was disagreement about the strength of the evidence:
So one of the difficulties with NICE guidelines is that they come out with a government stamp on them saying you must do it and you must audit them. But actually sometimes the evidence on which the guideline is based is quite weak. And ultimately it comes down to expert opinion. (Physician/UK/38)
Need to standardize practices
The decision to standardize practices generally arose within the unit team, aiming at more consistent and homogeneous care:
There was a need for a common framework. (Nurse/Italy/17)
Even issues considered common knowledge could benefit from standardization, as was the case with actions in response to vancomycin blood level monitoring:
We did know, that you must react. Everyone knew that, but it wasn’t standardized. Now it’s rather precise, regardless of who is working, whether it’s weekend or night or whatever, the reaction is always exactly the same. (Physician/Germany/10)
The need for a common approach was felt especially in case of rapid staff turnover, or because of new professionals joining the unit:
Now every morning we have the physiotherapists […]. Therefore also this part, which was not included in the old protocol, had to have relevance, and we all had to standardize our approach to the children. (Nurse/Italy/17)
Modification of the characteristics of the patients admitted to NICU was mentioned as a motive to revise policies:
Also the type of patients change, they are becoming smaller and smaller… the 23 weekers were only in the mind of God, now they survive, therefore clearly you have to update progressively, as both research and type of patients lead you to adapt some parts. (Physician/Italy/34)
Participation in research
The experience of participating in a study requiring modification of usual routines was the main driver leading to the establishment of a structured protocol for kangaroo skin-to-skin maternal care:
There were many reasons that motivated it, one of them—and this was very important—was that we are part of a project which is called CARE. So we took advantage of this situation to say that we would like our unit to be part of this change and we went ahead with it. (Physician/Portugal/19)
In Italy, participation in an intervention study to increase parental presence in NICU led to the establishment of a new routine for the first communication with the parents:
Before, in case of a new neonatal admission, we were busy only with the baby. Now we go to talk to the parents, we reassure them and tell them that as soon as the baby has stabilized, they will be able to enter [the NICU]. (Nurse/Italy/24)
In Germany, study participation led to the development of an educational protocol identifying the situations when endotracheal intubation could be performed by trainees:
Well, we had taken part in a study, a study on intubation, and in that framework we thought, good now, we’ll thoroughly reorganise it, so that there are guidelines. (Physician/Germany/39)
In one case only the reported research, a randomized clinical trial to identify the lowest baby’s weight for safe transition from incubator to open cot, was designed by the informant and carried out within the unit itself:
Therefore, now I can tell parents that we transfer the infants to open cots because [our study] showed that this is beneficial, without side effects, and shortens the hospital stay by about one week. (Physician/Italy/40)
One definite advantage of research participation is the opportunity to test a new policy before adoption and experience its benefits. With reference to the CARE project mentioned before, the informant said:
People understood the importance, and stopped saying what a bore, we have to do this. […] For example we now do ventricular drainage with the baby in the Kangaroo position, something that we had never done before, and we have very good results. Also with venipuncture, and you can see a decrease in level of pain, because we have the levels of pain measured on a scale. We feel this is very beneficial. (Physician/Portugal/19)
Nevertheless, when the change involves, as in this case, organizational modifications requiring compliance by the whole team and the parents, implementation can still be challenging:
It’s a process which is a bit different, and [initially] the medical staff weren’t really motivated. I mean one thing is a new ventilator, a new ventilation strategy, and then you have all the scientific enthusiasm inherent to intensivists. As long as there is the money to buy the ventilators, there’s a meeting, and if there is agreement they move forward and the process is established and everyone follows along, the parents have no word in it, nor the nurses, they just have to adapt to it. Whereas here, there is involvement of all staff, it is different and very interesting, at least from my point of view. (Portugal/Physician/19)
Occurrence of an adverse event
Adverse events, and the urgency to prevent similar cases in the future, were reported as rare but highly emotionally charged triggers leading to the change of unit practices:
This change occurred because we diagnosed late, late a baby who was in hospital with aortic coarctation…In other words, there was an error in our work. […] I think that it was because of this urgent case that [the cardiac screening] was implemented from one day to the next. It had to be done. (Nurse/Portugal/37)
While describing the newly introduced daily mandatory inspection of the resuscitation equipment at the labour ward, documented and signed by the nurse in charge, the informant reported about:
…a suction device that actually didn’t work, the device was faulty, it just didn’t build up any suction and you would have noticed that if you had checked it beforehand. So that happened in a situation with an emergency caesarean section where we really came in at the same time as the patient. […] We discussed, how do you do that, how do others do that, how can we match that? And then we said, okay, it’s got to be a daily check. (Nurse/Germany/36)
Adverse events appeared to prompt immediate change even when unrelated to identified clinical errors:
…the one that springs to mind that is probably the most recent is a guideline on difficult intubation. What prompted it initially was… we actually had an incident where a baby was very difficult to reintubate. And when we looked at the incident in detail, we identified that we hadn’t got a guideline on the difficult to manage airway. […] What was interesting when we wrote the guideline was that what had been done during the incident was what the guideline said we should do. (Nurse/UK/11)
Interestingly, the nurse commented on the value of guidelines precisely for infrequent events:
It isn’t a circumstance that is going to happen often, but then I feel that those are particularly the occasions you need guidelines for. Obviously for things you do day-in day-out, it’s perhaps less important, because you know what you’re doing all the time. Whereas something that happens less often, it’s always useful to have a guideline to refer to. (Nurse/UK/11)
Improvement of care
Improvement of care was explicitly identified as the main motive for change by three doctors and eight nurses. Two physicians from the same NICU mentioned the importance of starting personalized parenteral nutrition since the first hours after birth:
…this nutrition prevents the babies from entering a catabolic state, which is what happens when they are born and so, it is fundamental that we stop the catabolic state, right, and try to nourish them from the first day. (Physician/Portugal/42)
This aim conflicted with the opening hours of the hospital pharmacy, that would not prepare parenteral nutrition bags unless ordered before 2 pm:
…and so, all newborns who were born outside of those hours had to receive [only] basic fluid therapy until the next day. (Physician/Portugal/42)
Additionally, parenteral bags could only be ordered with reference to a specific, legally identified individual:
And here the problem is that legally the baby only exists after it is born. (Physician/Portugal/28)
The change that was implemented involved ordering a parenteral bag “in anticipation”:
So we ended up by speeding things a little and planning ahead and making requests for babies, who aren’t yet identified with a file number, by using only the mother’s identity and the baby’s predicted weight. (Physician/Portugal/28)
And then that bag is adjusted in terms of the rhythm of perfusion for the infant who is born in the meantime. There, it’s something new. (Physician/Portugal/42)
The nurses focussed on the importance of care, and on the appropriate handling of the fragile very preterm babies:
At the beginning of last year we discussed that we would like to introduce kinaesthetics into our care practices. […] It’s not that anyone ever felt that we weren’t handling the children correctly, rather we just wanted to improve because the children stay in our wards for a very, very long time. We wanted to do something good for the children, and we noticed that we treat them differently from our medical colleagues. So, we have a medical colleague who always positions the children semi-upright, because he says that’s good for their breathing. Then you come to one of these little cots and you see that the infant is in this position but is sliding down and being held up by the air tubes. Breathing improves, no question about that, but you need to give the child a support, some security, so the baby doesn’t have the feeling, oh God, what do I do now? (Nurse/Germany/15)
Improvement of patient care may also be achieved by increasing parents’ involvement and empowerment:
We chose our focal points that we want to communicate to the parents. We really pushed the advice for breastfeeding, reinforced skills in feeding and handling the infants. Our experience was, the more skilled the parents are, the more they can contribute to the care. (Nurse/Germany/12)
Discussion
This study provides, from the perspective of the healthcare staff, an overview of the type of clinical and organizational innovations introduced in the NICUs and of the main factors that motivated the decision to change. Consistently with our initial question, some of the innovations described referred to the same topic. However, the relative frequency of selection varied by professional role, with ventilation at the top of the physicians’ list while issues of infant and parental care were more prominent among nurses.
We found that the introduction of innovative policies or treatments in NICUs can be triggered by several factors. Some were external to the unit, such as the publication of a new law or official guideline in need of implementation. Others were internal, arising from a reflection on own clinical experience promoted by reading the literature, attending conferences, participation in research, or as reaction to an adverse event. While external triggers were generally backed-up by formal assessment of scientific evidence, this was not always the case for changes that originated from staff personal experience and observations. This dichotomy seems to mirror two views of evidence-based medicine: the rigorous identification of scientific evidence with results of randomized clinical trials and meta-analyses only, versus the broader view including other sources of evidence such as different study designs, clinical experience, interactions with peers and patients, and “pragmatic science” methods of learning.17–19
In our study, pragmatic methods and clinical experience were used to promote organizational changes especially in areas where formal scientific evidence was lacking or controversial. They were more often used by nurses, because of their special interest in the patient perspective and, possibly, the relative paucity of experimental evidence in nursing.20,21 However, clinical experience is effective only when accompanied by the other three elements of the Kolb’s experiential learning cycle,22 namely reflective observation, conceptualization and experimentation. The development, reported by one of our informants, of a randomized trial based on the initial observation of a declining trend of babies’ weight at transfer to open cots, with its final finding of safe shortening of hospital stay, was a perfect example of the application of the cycle as well as demonstration of the complementarity between EBM and quality improvement methods.19
We found that the type of motivation to change influenced the speed of implementation and staff compliance. Innovations arising within the NICU team, out of personal experiences and exchanges with colleagues, new information from the literature or participation in research, appeared to lead to smoother and possibly quicker implementation. An extreme example of internal trigger was the occurrence of an adverse event, where the emotional burden led to immediate action and widely shared consensus about the necessary change. This finding confirms the learning potential for staff after an adverse event, which is at the root of audit initiatives such as incidence reporting, case analyses and mortality statistics conferences for the NICU or all hospital staff.23,24
The nature of the innovation was also relevant. Technological innovations, such as new drugs or equipment, offer the promise of improving care within limited resources and without need for complex reorganization of unit routines. In contrast, changes requiring policy reorganization, coordination across disciplines and agreement by all components of the team remain challenging, and may take more time to gain consensus.25 However, glamour and underlying commercial interests may foster the adoption of new technologies even before evidence of benefit and cost-effectiveness is established. Preliminary testing to the same standards of other innovations is absolutely necessary.26,27
The active participation of the unit staff in the development of the new policy, or at least in the decision to adopt it, appeared crucial to increase compliance. Changes imposed completely from outside, such as mandatory regulations or official guidelines issued by ad hoc agencies, raised more frequent criticism and resistance, particularly when the strength of the evidence was considered controversial. An additional important issue was the opportunity to test the innovation before adoption, as was the case for participating in a research project on kangaroo care, highlighting the importance of clinical research not only in generating new knowledge but also as learning experience for participants. Finally, the presence of a staff member with personal interest and expertise in the specific field of change was the third element that emerged as important for successful implementation.
This study has strengths and limitations. To our knowledge, this is the first study providing an overview of the factors that trigger change and promote the introduction of clinical and organizational innovation in NICUs. The study benefited from the EPICE mixed-method design as we based our research hypothesis on quantitative data showing variable uptake of a range of evidence-based interventions by region.14 However, our decision to focus on the process of change allowed any unit to participate, as the interview contents were not contingent on use of a specific intervention. We did not provide a pre-set definition of innovation, allowing a better understanding of what constitutes innovation for the medical and nursing professionals. The choice of discussing a real experience, identified as the most recent, aimed to avoid theoretical discussions and prevent the selection of the most successful event. The inclusion of a maximum of eight interviews per country inhibited a full analysis of country-level specificities. Nonetheless, many of the themes emerged in multiple contexts, suggesting broader application.
Conclusions
The findings of our study can contribute to inform strategies aimed at fostering successful implementation of the intended change and staff compliance. Whether the change originates within the NICU or from outside, it is advisable to involve all the staff concerned in its uptake, including listening to objections and criticisms and proposals for local adaptation. In case of innovation promoted by official agencies, early partnering with professional associations may be important. Clinical audits represent a powerful opportunity for change, particularly when carried out with a nonjudgemental, pragmatic attitude. Regular literature review meetings can promote the transfer of scientific findings into clinical practice. Actual participation in research studies can be an effective way to test innovations before adoption and monitor the outcomes. Overall, these strategies may represent interesting research hypotheses to be tested in future studies.
Along with the established role of evidence-based methods to assess the value of innovative interventions, qualitative research can contribute to a better understanding of the circumstances and conditions that foster the development, dissemination and implementation of clinical innovations.
Acknowledgements
We are grateful to all the physicians and nurses who participated in the interviews and shared their experiences with us. We thank Nikola Jeck for carrying out the interviews in Germany. The EPICE project was funded by the European Union's Seventh Framework Programme [FP7/2007−2013] (grant no. 259882). In Portugal, this study was also funded by FEDER through the Operational Programme Competitiveness and Internationalization and from the Foundation for Science and Technology—FCT (Portuguese Ministry of Science, Technology and Higher Education), under the Unidade de Investigação em Epidemiologia—Instituto de Saúde Pública da Universidade do Porto (EPIUnit) (POCI-01-0145-FEDER-006862; ref.UID/DTP/04750/2013) and the Ph.D. Grant SFRH/BD/111794/2015 (Carina Rodrigues), co-funded by the FCT and the POCH/FSE Program.
Author contributions
M.C. designed the study, drafted the study protocol, coordinated data analyses and prepared the manuscript. E.F. coordinated data acquisition and analyses across the participating regions, carried out and transcribed the interviews in Italy and performed the overall second-stage data analyses. C.R., E.S.D., R.F.M. and M.B. participated in the finalization of the study protocol and materials, supervised data acquisition in their region and contributed to the manuscript for important aspects related to the interpretation of results and the discussion. A.F.M., A.L., J.W., A.H. carried out and transcribed the interviews in their region and performed first-stage data analyses; they contributed to the paper as regards the validity of data reporting and interpretation. I.C. prepared and maintained the quantitative database of the study, prepared the tables and figure, and performed the literature review. J.Z. initiated and coordinated the EPICE project, participated in the definition of this study aims, protocol and instrument, and substantially contributed to the manuscript for important aspects. All authors have read and approved the final version of the manuscript.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.West, M. A. The social psychology of innovation in groups. In: Innovation and Creativity at Work: Psychological and Organizational Strategies (eds West, M. A. & Farr, J. L.) 309−333 (John Wiley & Sons, Oxford, UK, 1990).
- 2.Länsisalmi H, Kivimäki M, Aalto P, Ruoranen R. Innovation in healthcare: a systematic review of recent research. Nurs. Sci. Q. 2006;19:66–72. doi: 10.1177/0894318405284129. [DOI] [PubMed] [Google Scholar]
- 3.Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82:581–629. doi: 10.1111/j.0887-378X.2004.00325.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Prasad V, Ioannidis JP. Evidence-based de-implementation for contradicted, unproven, and aspiring healthcare practices. Implement. Sci. 2014;9:1. doi: 10.1186/1748-5908-9-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Balas EA, Chapman WW. Road map for diffusion of innovation in health care. Health Aff. (Millwood) 2018;37:198–204. doi: 10.1377/hlthaff.2017.1155. [DOI] [PubMed] [Google Scholar]
- 6.Berwick DM. Disseminating innovation in health care. JAMA. 2003;289:1969–75. doi: 10.1001/jama.289.15.1969. [DOI] [PubMed] [Google Scholar]
- 7.Donaldson NE, Rutledge DN, Ashley J. Outcomes of adoption: measuring evidence uptake by individuals and organizations. Worldviews Evid. Based Nurs. 2004;1:S41–51. doi: 10.1111/j.1524-475X.2004.04048.x. [DOI] [PubMed] [Google Scholar]
- 8.Lewin K. Field Theory in Social Science. New York, NY: Harper & Row; 1951. [Google Scholar]
- 9.Kotter JP. Leading change. Why transformation efforts fail. Harv. Bus. Rev. 2007;85:92–107. [Google Scholar]
- 10.Rogers EM. Diffusion of Innovation. 1st edn. New York, NY: Free Press of Glencoe; 1962. [Google Scholar]
- 11.Panzano PC, Roth D. The decision to adopt evidence-based and other innovative mental health practices: risky business? Psychiatr. Serv. 2006;57:1153–61. doi: 10.1176/ps.2006.57.8.1153. [DOI] [PubMed] [Google Scholar]
- 12.Damschroder LJ, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement. Sci. 2009;4:50. doi: 10.1186/1748-5908-4-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stevens B, Lee SK, Law MP, Yamada J, Canadian Neonatal Network EPIC Study Group. A qualitative examination of changing practice in Canadian neonatal intensive care units. J. Eval. Clin. Pr. 2007;13:287–94. doi: 10.1111/j.1365-2753.2006.00697.x. [DOI] [PubMed] [Google Scholar]
- 14.Zeitlin J, et al. Use of evidence based practices to improve survival without severe morbidity for very preterm infants: results from the EPICE population based cohort. BMJ. 2016;354:i2976. doi: 10.1136/bmj.i2976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pettigrew AM. Context and action in the transformation of the firm. J. Manag. Stud. 1987;24:649–70. doi: 10.1111/j.1467-6486.1987.tb00467.x. [DOI] [Google Scholar]
- 16.Guest G. Applied Thematic Analysis. Thousand Oaks, CA: Sage Publications; 2012. [Google Scholar]
- 17.Berwick DM. Broadening the view of evidence-based medicine. Qual. Saf. Health Care. 2005;14:315–6. doi: 10.1136/qshc.2005.015669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baker GR. Strengthening the contribution of quality improvement research to evidence based health care. Qual. Saf. Health Care. 2006;15:150–1. doi: 10.1136/qshc.2005.017103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Salter KL, Kothari A. Knowledge ‘translation’ as social learning: negotiating the uptake of research-based knowledge in practice. BMC Med. Educ. 2016;16:76. doi: 10.1186/s12909-016-0585-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Profetto-McGrath J, Smith KB, Hugo K, Taylor M, El-Hajj H. Clinical nurse specialists' use of evidence in practice: a pilot study. Worldviews Evid. Based Nurs. 2007;4:86–96. doi: 10.1111/j.1741-6787.2007.00086.x. [DOI] [PubMed] [Google Scholar]
- 21.Yarcheski A, Mahon NE, Yarcheski TJ. A descriptive study of research published in scientific nursing journals from 1985 to 2010. Int. J. Nurs. Stud. 2012;49:1112–21. doi: 10.1016/j.ijnurstu.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 22.Kolb DA. Experiential Learning Experience as a Source of Learning and Development. Englewood Cliffs, NJ: Prentice Hall; 1984. [Google Scholar]
- 23.Snijders C, et al. Specialty-based, voluntary incident reporting in neonatal intensive care: description of 4846 incident reports. Arch. Dis. Child Fetal Neonatal Ed. 2009;94:F210–5. doi: 10.1136/adc.2007.135020. [DOI] [PubMed] [Google Scholar]
- 24.de Feijter JM, de Grave WS, Muijtjens AM, Scherpbier AJ, Koopmans RP. A comprehensive overview of medical error in hospitals using incident-reporting systems, patient complaints and chart review of inpatient deaths. PLoS ONE. 2012;7:e31125. doi: 10.1371/journal.pone.0031125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bradley EH, Schlesinger M, Webster TR, Baker D, Inouye SK. Translating research into clinical practice: making change happen. J. Am. Geriatr. Soc. 2004;52:1875–82. doi: 10.1111/j.1532-5415.2004.52510.x. [DOI] [PubMed] [Google Scholar]
- 26.Bloom SL, Leveno KJ. Unproven technologies in maternal-fetal medicine and the high cost of US health care. JAMA. 2017;317:1025. doi: 10.1001/jama.2017.1218. [DOI] [PubMed] [Google Scholar]
- 27.Godlee F. Putting innovation to the test. BMJ. 2017;359:j5539. doi: 10.1136/bmj.j5539. [DOI] [Google Scholar]