Abstract
Several authors in bioethics literature have expressed the view that a whole brain conception of death is philosophically indefensible. If they are right, what are the alternatives? Some authors have suggested that we should go back to the old cardiopulmonary criterion of death and abandon the so-called Dead Donor Rule. Others argue for a pluralist solution. For example, Robert Veatch has defended a view that competent persons should be free to decide which criterion of death should be used to determine their death. However, there is very little data on people’s preferences about death determination criteria. We conducted online vignette-based survey with Latvian participants (N = 1416). The data suggest that the pluralist solution fits best with the way our study participants think about death determination—widely differing preferences concerning death determination criteria were observed. Namely, most participants choose one of the three criteria discussed in the literature: whole brain, higher brain, and cardiopulmonary. Interestingly, our data also indicate that study participants tend to prefer less restrictive criteria for determination of their own deaths than for determination of deaths of their closest relatives. Finally, the preferences observed in our sample are largely in accord with the Dead Donor Rule for organ procurement for transplantation.
Electronic supplementary material
The online version of this article (10.1007/s40592-020-00114-0) contains supplementary material, which is available to authorized users.
Keywords: Death, Death determination, Brain death, Organ transplantation
Introduction
Brain death is legally accepted as the criterion of death in many countries worldwide.1 Despite this wide consensus there are still many pockets of resistance in philosophy and in the medical community, and one might even argue, that there are even more dissenters now than there were about 20 or 30 years ago, when brain death started its way towards its legal recognition. Many philosophers have expressed the view that the concept of brain death is philosophically indefensible and therefore should be abandoned (Veatch 1993; Singer 1995; Truog 1997; Degrazia 2005). Peter Singer, for example, has pointed out that brain death is a conventional fiction and that although currently there is consensus about the concept, for various reasons it is unstable (1995, pp. 35–37).2 Seema Shah, Robert Truog and Franklin Miller have argued that death determination based on whole brain death is an “unacknowledged legal fiction that is used without full recognition of its falsity” (Shah et al. 2011, p. 721).3 This, however, raises difficult questions about the possibility of effective organ procurement and transplantation policy as the current practices in this area in many countries rely on the acceptance of the brain death criterion of death.
Several authors have come up with alternative suggestions about what should be done in this situation. Some authors (e. g. McMahan 2002; Glannon 2007) argue that instead of the whole brain death criterion we should accept the so-called higher brain criterion of death, i.e. assume that death should be determined as soon as irreversible loss of consciousness is diagnosed. Others argue for a slightly more complex solution. For example, Robert Truog (1997) suggests that we should return to the good old cardiorespiratory criterion of death and uncouple the link between organ transplantation and death.4 This means abandoning the so-called Dead Donor Rule—the principle that vital organs can be procured only from donors who are dead. The purpose of this move is to keep the current practice of organ procurement for transplantation, which we would have to change if we would simply go back to the cardiopulmonary concept of death without challenging the Dead Donor Rule.5
Furthermore, there are authors who argue that there is no reasonable hope to arrive at a consensus on the issue of death determination, because people have rather different intuitions about the matter and all philosophical conceptions advanced so far have problems of their own. Those authors defend the view, that determination of death is not a matter that can be decided by some medical facts about human organisms, but rather that it is a metaphysical and ethical choice, a decision that usually depends on the extent to which particular medical facts matter to people. Therefore, the only workable solution is to embrace pluralism about the criteria of death and to admit that people themselves should be allowed to choose the criteria that are used to determine their deaths. Views along these lines have been proposed by several authors (e. g. Lachs 1988; Sass 1992; Emanuel 1995; Bagheri 2007; Zeiler 2009), but to our knowledge the most elaborate account of this kind belongs to Robert Veatch (1989, 1999, 2019), Veatch and Ross (2016). According to Veatch, we have to tolerate different views that people have about death and to allow different groups to act on their opinions. Veatch proposes that people—while still competent—should be free within reason to choose the criteria under which they should be considered dead. As there are indefinite number of theoretically possible conceptions of death, there should be—for practical reasons—some limited set of choice alternatives. Veatch suggests that people should be offered to choose from the three plausible accounts that are discussed in bioethics literature, i.e., cardiopulmonary, whole-brain and higher brain. Furthermore, since for different reasons not everyone will make an explicit choice among the offered criteria of death, there must be a default position on death, so that it is clear for doctors and others how to proceed in such cases. Veatch proposes that the best candidate for that role is the currently widely accepted whole-brain conception. In cases where patients have not made their view on death clear while competent, the decision within certain limits should be made by the next of kin as it is done in other similar situations already.
Notwithstanding how the philosophical debate on this topic will unfold, the practicability of different suggestions should also be addressed. Prima facie, proposals that diverge less from popular preferences have a better chance of being successfully implemented as policies and the nature and distribution of these preferences is an empirical matter. Furthermore, some of philosophical theories in the market (e.g. pluralistic policy advocated by Veatch) imply that public preferences have a role in shaping the implementation of a given policy.
One thing to note is that there seems to be much public misunderstanding about medical and legal facts concerning death determination. A recent literature review indicates that “the existing data on public attitudes regarding brain death and organ transplantation reflect substantial public confusion” about medical and legal facts (Shah et al. 2015, p. 291). There are some important tendencies noted in the empirical literature, however. For example, research conducted in Japan and China (see Yang and Miller 2015, p. 216 for a brief overview) indicates a quite strongly pronounced support for a cardiopulmonary understanding of death. However, as far as we know, there are no studies in which participants had a possibility to explicitly indicate their own preferences concerning death determination criteria by choosing from a wide set of options. Another tendency of note is rather consistent public support for the Dead Donor Rule (see Dubois and Anderson 2006 for a review; but see Nair-Collins et al. 2014).
In this paper, we intend to contribute to this emerging literature on public preferences concerning death determination. There were three aims of the study. First, we wanted to gather some preliminary data on preferences concerning death determination criteria. We wanted to learn whether some potential criteria are more likely to be preferred than others. Second, we wanted to learn whether these preferences differ when we make the judgement about which criteria should be applied to ourselves and to our closest relatives. Third, we wanted to learn whether these preferences accord well with the Dead Donor Rule.
Study
Participants
The study questionnaire in Latvian was distributed via social networks Twitter and Facebook with a short request to complete the survey and share the link on their social network profiles. Within 3 days through which it was live, 1491 Latvian participants took part in it. After removing 3 participants for indicating age lower than 18 years old and another 72 participants for not providing answers to at least one of the four main measures, N = 1416 (67% females, 32% males, 1% chose ‘other/prefer not to answer’, 3 participants did not provide any answer; mean age: 35.1; SDage = 10.0; age range 18–81, 38 participants (2.7%) did not indicate their age).
Materials and procedure
To conduct the study, we developed a description of a process of dying. The description was developed in English and checked for medical accuracy by a medical doctor. Then the materials were translated into Latvian by one of the authors and checked for readability by a professional editor.
After receiving information on the nature of the study and providing their consent, participants read the following possible description of the process of dying, divided into numbered stages, from stages of increasing health deterioration (Stages 1 and 2) to a description of a corpse that already starts to decay (Stage 6). The remaining stages were designed to mimic conceptions of death discussed in bioethics literature. Stage 3 was designed to reflect the higher brain criterion of death, Stage 4—whole brain death criterion, Stage 5—cardiopulmonary criterion. This 6-stage description was always available for participants at the bottom of each page with measure.
The patient had fever and headaches for 3 days. The patient cannot tolerate bright light and noises. The patient is nauseous, and when he moves too fast he has vertigo. The doctor stuck a needle into the patient’s back to get some of the fluid in his brain and the results came back indicating inflammation. The doctor diagnosed meningitis.
The patient has been in the hospital for 3 days. First, in Neurology unit, but after a day he was transferred to the Intensive care unit. Patient’s memories of the recent past are fragmented, he has intense hallucinations. Medication is used to calm him down. In the ICU he is asleep most of the time. When he opens his eyes he cannot recognize the relatives. Sometimes when awake he mumbles random words or screams.
The patient’s state deteriorated rapidly. His brain herniated. Due to that the cerebral cortex of the brain stopped functioning. The patient is still breathing on his own and his heart beats, but he cannot feel anything or make himself move. The consciousness is irrevocably lost. The patient does not react to any attempts to talk to him. However, the patient responds to some stimuli: when the neurologist poured some ice-cold water into the patient’s ears and looked for his eyes to move, they did move. The patient is in this state for 2 weeks.
The patient’s brain stopped functioning. The patient is intubated and breathing is done by mechanical lung ventilator. If removed from it, the patient would not be able to breathe. The heart is beating, but medication is needed to sustain it. The patient does not move and does not feel anything. The patient no longer reacts to painful stimuli but some very basic reflexes remain: when the neurologist hits the knee with a little rubber hammer, the leg moves. The patient is in this state for 2 weeks.
The patient’s heart stopped and the patient was disconnected from the ventilator. The patient is not breathing, the body temperature starts to drop below 36 °C. The skin is becoming cold and grey. The patient is not responsive to any stimuli whatsoever.
After a day, the body is cold and stiff. The temperature is the same as the room temperature. The blood in blood vessels has pooled in the lower parts of the body due to gravity. The abdomen is distended because guts are starting to decay due to bacteria in there.
On the next page some additional background information was provided in order to make the study task more intelligible to the participants.
In different countries of the world, different criteria for the determination of death are used. For example, in some countries, death is declared after full brain death, while in others—when the heart no longer beats. In some countries, people have a right to choose, what criterion will be applied to them or to their relatives.
The following two pages contained questions on preferences for death determination. One concerning the self and the other concerning a close relative. The order of presentation of these two pages was randomized and participants were not allowed to come back to the previous page to change their responses. For both questions, participants had to choose a stage as numbered in the description of the process of dying.
The question about the self read:
Try to think about your own preferences concerning your death. Suppose that you also can end up in a situation that resembles the one described. (If you want to refresh your memory, description of the process of dying is repeated at the bottom of this page.) Please indicate the stage of the process of dying at which you would you prefer your own death to be stated.
While the question about the relative read:
Try to think about your preferences concerning the death of your closest relatives. Suppose that a close relative of yours can end up in a situation that resembles the one described. (If you want to refresh your memory, description of the process of dying is repeated at the bottom of this page.) Please indicate the stage of the process of dying at which you would prefer the death of your relative to be stated.
After answering questions about death determination, some additional background was provided on the next page concerning organ procurement for donation.
The time at which death is determined is also very important in the context of organ donation, since organs are suitable for transplantation only when they are not damaged. Most frequently, organs are procured for donation after complete death of the brain (Stage 4 in the description of the process of dying), but sometimes medical professionals wait till the heart stops beating (Stage 5), but in such cases it is necessary to procure the organs no later than five minutes after the heart stops beating.
The next two pages contained questions on preferences for organ procurement. One concerning the self and the other concerning a close relative. The order of presentation of these two pages was randomized and participants were not allowed to come back to the previous page to change their responses.
The question about the self read:
Try to think about your own preferences concerning organ donation. Suppose that you also can end up in a situation that resembles the one described. (If you want to refresh your memory, description of the process of dying is repeated at the bottom of this page.) Please indicate the stage of the process of dying at which you would prefer your organs to be procured for transplantation.
While the question about the relative read:
Suppose that a close relative of yours can end up in a situation that resembles the one described. (If you want to refresh your memory, description of the process of dying is repeated at the bottom of this page.) Please also suppose that your close relative expressed a wish to become an organ donor after they die. Please indicate the stage of the process of dying at which you would prefer the organs of your close relative to be procured for transplantation.
For both questions, participants had to choose a stage as numbered in the description of the process of dying. They were also allowed to choose additional option “I would not agree to organ donation in such case”.
Participants then provided information on their gender and age as well as whether they have studied philosophy and how often they practice religion and were thanked for participation.
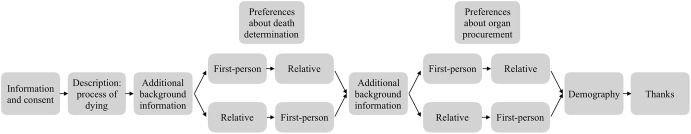
The study logic is depicted in Fig. 1. Full study materials in both English and Latvian as well as study data and additional analyses can be found online: https://osf.io/zadqv.
Fig. 1.
Study logic
Results
Since our measures asked to indicate a stage in the process of dying, we treat these responses as answers on ordinal scale, and thus run non-parametric tests.
Death determination, the main analysis
Mann–Whitney U test was performed in order to test for order effects. No differences in ranks were observed in either responses to the first person scenario (U = 250,121.0, Z = 0.068, p = 0.946, r = 0.00) or scenario about the relative (U = 242,333.5, Z = 1.149, p = 0.251, r = 0.03). Thus, all participants were pooled for related samples analysis.
Summary results about preferences concerning death determination criteria are displayed in Table 1.
Table 1.
Preferences of participants concerning stages of the dying process in which their death and death of their relatives should be stated (N = 1416)
| Stages | First-person | Relative | ||
|---|---|---|---|---|
| n | % | n | % | |
| 1 | 9 | 0.6 | 7 | 0.5 |
| 2 | 45 | 3.2 | 15 | 1.1 |
| 3 | 507 | 35.8 | 280 | 19.8 |
| 4 | 544 | 38.4 | 616 | 43.5 |
| 5 | 263 | 18.6 | 448 | 31.6 |
| 6 | 48 | 3.4 | 50 | 3.5 |
n indicates the number of participants choosing a given stage and % indicates the percent of participants choosing a given stage. Percentages may not add up to 100 due to rounding,
In both cases, top-3 most frequently chosen stages were 3, 4, and 5, with 4 being the most frequent (38.4% in first-person question and 43.5% in relative question).
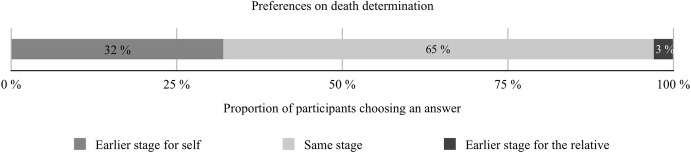
Wilcoxon Signed-ranks test indicated that participants were more often willing to choose a later stage for relatives than for themselves, Z = 17.74, p < 0.001, PSdep = 0.32. Looking in more detail, out of 1416 participants, 453 (32%) chose a later stage for determination of the relative’s death than their own death while only 41 (3%) chose an earlier stage for themselves. The remaining 922 (65%) preferred the same stage in both cases. Here and later in the paper we use probability of superiority estimation for dependent groups (PSdep) as a measure of effect size for Wilcoxon Signed-ranks tests, as recommended by Grissom and Kim (2014, pp. 114–115). PSdep = 0.32 means that there is 32% probability that within a randomly sampled pair of responses, the score for the relative will be higher than the score for oneself. These results are presented in Fig. 2.
Fig. 2.
Proportion of participants who prefer earlier stage for determination of death for themselves than for their relatives, same stage for both, and earlier stage for the relatives than for themselves. N = 1416
Additional analyses
For subsequent analyses that involve decisions concerning transplantation, 115 (8%) participants were removed since they chose “I would not agree to organ donation in such case” as an answer to at least one transplantation question (43 were opposed in first-person case; 21—in relative case; 51—in both). The reason for their exclusion is that leaving them in would not allow us to treat answers as choices on ordinal scale anymore.6
Information on choices indicated by the remaining participants (N = 1301) is presented in Table 2.
Table 2.
Preferences of participants concerning stages of dying process in which their death and death of their relatives should be stated and in which their and their relatives’ organs can be taken for transplantation (N = 1301)
| Stages | Death determination | Procurement | ||||||
|---|---|---|---|---|---|---|---|---|
| First-person | Relative | First-person | Relative | |||||
| n | % | n | % | n | % | n | % | |
| 1 | 8 | 0.6 | 6 | 0.5 | 3 | 0.2 | 3 | 0.2 |
| 2 | 40 | 3.1 | 13 | 1.0 | 20 | 1.5 | 9 | 0.9 |
| 3 | 484 | 37.2 | 263 | 20.2 | 281 | 21.6 | 143 | 11.0 |
| 4 | 509 | 39.1 | 584 | 44.9 | 770 | 59.2 | 811 | 62.3 |
| 5 | 227 | 17.4 | 400 | 30.7 | 217 | 16.7 | 326 | 25.1 |
| 6 | 33 | 2.5 | 35 | 2.7 | 10 | 0.8 | 9 | 0.7 |
n indicates the number of participants choosing a given stage and % indicates the percent of participants choosing a given stage. Percentages may not add up to 100 due to rounding
In all four cases, top 3 most frequently chosen stages were 3, 4, and 5, with 4 (whole brain death) being the most frequent (39.1% in first-person question, 44.9% in relative question, 59.2% in transplantation first-person case and 62.3% in transplantation relative case).
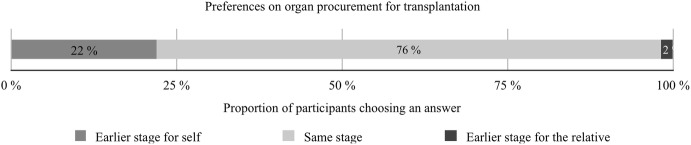
Transplantation
Out of 1301 participants, 281 (22%) chose a later stage for harvesting a relative’s organs than their own while only 31 (2%) chose a later stage for themselves. Remaining 989 (76%) preferred the same stage for both cases. A Wilcoxon Signed-ranks test indicated that participants were more often willing to choose a later stage for relatives than for themselves, Z = 13.61, p < 0.001, PSdep = 0.22. These results are presented in Fig. 3.
Fig. 3.
Proportion of participants who prefer earlier stage for harvesting organs for transplantation for themselves than for their relatives, same stage for both, and earlier stage for the relatives than for themselves. N = 1301
First-person case
Out of 1301 participants, 323 (25%) chose a later stage for harvesting their organs than for their death determination while 159 (12%) chose an earlier stage for harvesting their organs than for their death determination. The remaining 819 (63%) preferred the same stage for both cases. A Wilcoxon Signed-ranks test showed that participants were more often willing to choose a later stage for organ procurement than for death determination, Z = 7.61, p < 0.001, PSdep = 0.25.
Relative case
Out of 1301 participants, 239 (18%) chose a later stage for harvesting the organs of the relative than for death determination of the relative. 241 (19%) chose an earlier stage for organ procurement than for death determination. The remaining 821 (63%) preferred the same stage for both cases. A Wilcoxon Signed-ranks test indicated that there was no difference in relative case between time of death determination and time of organ procurement, Z = 0.065, p < 0.948.
Demographic effects
There were no notable demographic effects. Only some weak associations between preferences and gender, religiosity and age were observed (all correlation coefficients smaller than 0.15). For the analysis of demographic effects see online Supplementary materials.
Discussion
Preferences concerning death determination criteria
Looking at preferences for death determination, all three candidate criteria (cardiopulmonary; whole brain; higher brain) seem to have some support in our sample. The vast majority chose one of the three options that were designed to mimic death determination criteria familiar from the literature. This was true both for preferences concerning determination of their own death and for the death of their relatives. Stage 4 (whole brain death) was the most popular option for self (38.4%) and for relative (43.5%), but Stage 3 (higher brain death) was also a popular option (35.8% for self and 19,8% for relative). Stage 5 (cardiopulmonary death) was preferred by 18.6% for self and 31.6% for relative. If we agree—along with Veatch—that the distribution of the preferences is a good guide to which options should be in the choice-set while formulating a policy, then this result provides initial support for the idea of widening the set of criteria available for choice: not only whole brain death and cardiopulmonary death but also higher brain death should be in the choice-set.7 This is especially suggestive looking at preferences for the self where 40% of participants in our study opted for criteria that are less restrictive than the current legal standard (22% opted for more restrictive criteria).
Differences between first-person and relative cases
An interesting finding of the study is that participants tended to choose earlier stage in the process of dying for the determination of their own death than for the determination of death of their relative.
This has potential implications for situations in which relatives are entrusted to make a decision concerning which death determination criterion is to be applied: relatives may be inclined to choose a later stage for death determination than the patient herself would be inclined to choose, were she able to make a decision. This can be mitigated by encouraging people to write advance directives and putting more weight on them.
The same pattern was observed concerning the time at which organs are procured for transplantation. Participants tended to choose an earlier stage for themselves than for their relatives. This also can raise a similar concern in which relatives push for a later stage for organ procurement from their dying/dead relative than she herself would prefer, were she able to make a decision.
Dead Donor Rule
Concerning the Dead Donor Rule, the results are largely consistent with the rule: the vast majority of study participants prefer organs to be taken at the same stage at which death is declared or at a later stage. However, there also was a minority who exhibited a different pattern for themselves (12% of participants chose earlier stage for procurement of organs than for death determination) and also for the relatives (19%).
Limitations
Limitations of this study include the fact that participants were self-selected which prohibits us from drawing inferences about distribution of preferences in the whole Latvian population. Our data do not allow one to evaluate the precise distribution of preferences, but it is suggestive about general trends. Further research would be needed to provide more precise estimations. Another limitation is that only one description of the process of dying was used. Moreover, concerns can be raised that the process of death rarely if ever unfolds in the exact sequence of stages as in our description.8 Under realistic conditions we should not expect the process of dying to be structured in such a step-by-step manner. We acknowledge this as an important limitation of our study but we would still like to defend this methodological move. While clearly an idealized abstraction, this experimental set-up was decided a priori since our main interest was to find a way to measure differences in how ‘permissive’ or ‘restrictive’ criteria of death determination and an acceptable time for organ procurement that study participants are willing to apply. While we sacrifice some realism in choosing to operate with sequential description of the process of dying and, in consequence, an ordinal scale, we also gain quite a bit in simplicity and intuitiveness of exposition. Treating the scale as categorical would remove these benefits. One more limitation is that in order to make the study more intelligible to the participants we introduced some explanations that referred to current practices which may have had some anchoring effects. Data reported in this paper accord very closely with the data from a much smaller (N = 160) preliminary study we conducted with Lithuanian participants (Dranseika and Neiders 2018).
Conclusions
In this paper, we present empirical data from Latvia on preferences concerning death determination criteria. Our data give preliminary evidence that there are pronounced differences in public preferences about death determination. All three conceptions of death discussed in the bioethics literature were preferred by a considerable proportion of study participants. Moreover, our data also shows that the three conceptions of death that are suggested by Veatch as candidates for people to choose from are not entirely arbitrary—each had considerable number of supporters in our sample. In addition, since the whole brain criterion was the most frequently chosen answer, this would provide some preliminary evidence that—if default option is needed at all—this criterion would be most practicable as the default option. Also, as participants in most cases indicate that, provided that they have consented to donate their organs, the organs should be procured after their death is diagnosed, our data provide some support for the Dead Donor Rule, i.e., the data suggest that the rule fits well with the preferences observed in our sample. Last but not least, our study provides some evidence that people have a tendency to prefer an earlier stage for determination of death for themselves than for their relatives. This result underscores the importance of advance directives in establishing preferences concerning death determination criteria as the criterion preferred by a person might differ from the one that his or her relatives might choose, if that decision should be made when the person doesn’t have decision making capacity.
It might be objected, that from the evidence that people have certain beliefs there is no way to derive any normative conclusions about what kind of policies should be implemented. This is not the place to address this thorny issue as that would be a subject for another paper. However, if the question about the practicability of different proposals is addressed, then we think that our findings provide some initial evidence to support the pluralistic solution proposed by Veatch.9
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank Gunda Zvīgule-Neidere, MD for helping us with her medical knowledge in composing the vignette used in the study and Ivar Hannikainen and David Rodriguez-Arias for comments and suggestions. We are also grateful to the anonymous reviewers for suggestions how to improve the paper. Finally, we thank our participants without whom the study would not been possible.
Author contributions
IN and VD conceived the study and collected the data. VD analyzed the data. IN drafted the manuscript, with substantial contributions from VD. Both authors approved the final version of the manuscript.
Funding
The research was supported by Latvian Council of Science lzp-2019/1-0223.
Compliance with ethical standards
Conflict of interest
The authors report no conflict of interest.
Ethical approval
As in Latvia non-biomedical survey research is not subject to ethics review, we did not seek to obtain approval from a Human Research Ethics Committee. All procedures performed in studies involving human participants were in accordance with the national and institutional ethical standards and with the 1964 Helsinki declaration and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Although the criterion is widely accepted, diagnostic criteria that are used in different countries to detect brain death might differ. For further discussion see Wijdicks (2002).
In a similar vein Jeff McMahan has described brain death as an “an unstable compromise between those views that make the irreversible loss of the capacity for consciousness the criterion of human death and those that insist that the death of a human being, like the death of any other organism, consists in the irreversible loss of functional integrity by the organism” (McMahan, 1995, pp. 96–97).
This position is developed further and defended in (Miller and Truog 2012).
To be more precise, it should be noted that currently in considerable number of cases of transplantation organs are procured from individuals who fulfil the traditional criterion for death determination, i.e., from donors after circulatory death (DCD). For example, according to the latest report published by the EDQM in 2018, in the European Union there have been 11,325 actual deceased donors and 1785 of them were DCDs (Dominiguez-Gil, 2019, p. 19). We would like to thank David Rodriguez-Arias for bringing this to our attention.
Results concerning death determination preferences were nearly identical to those achieved in the full sample before 115 participants were removed. Analysis is presented in online Supplementary materials.
In discussing preferences concerning policies of death determination, it is important to draw a distinction between two types of preferences. First, there are preferences about which criterion of death determination a person would prefer for herself or her relatives. Second, there are preferences about which criterion of death determination a person would prefer to be introduced as a general rule for the whole of society (or whether the person would prefer a pluralistic policy wherein people are left free to choose a criterion for themselves). In this paper, we look only into the first type of preferences.
This concern was raised by an anonymous reviewer.
We agree with Lindauer (2019) who in a recent paper argues that normative concepts used in moral philosophy can be evaluated in terms of their fruitfulness in solving practical problems and one way to determine how fruitful a concept is might be determined by empirical research. Lindauer’s concept of “fruitfulness” seems to be very close to our understanding of practicability.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Bagheri A. Individual choice in the definition of death. Journal of Medical Ethics. 2007;33:146–149. doi: 10.1136/jme.2006.016014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degrazia D. Human Identity and Bioethics. Cambridge: Cambridge University Press; 2005. [Google Scholar]
- Dominiguez-Gil B. Newsettler Transplant. International Figures on Donation and Transplantation 2018. Strasbourg: European Directorate for the Quality of Medicines & HealthCare of the Council of Europe; 2019. [Google Scholar]
- Dranseika V, Neiders I. In defense of a pluralistic policy on the determination of death. Ethics & Bioethics. 2018;8(3–4):179–188. doi: 10.2478/ebce-2018-0016. [DOI] [Google Scholar]
- Dubois JM, Anderson EE. Attitudes towards death criteria and organ donation among healthcare personnel and the general public. Progress in Transplantation. 2006;16(1):65–73. doi: 10.1177/152692480601600113. [DOI] [PubMed] [Google Scholar]
- Emanuel LL. Reexamining death. The asymptotic model and a bounded zone definition. Hastings Center Report. 1995;25(4):27–35. doi: 10.2307/3562159. [DOI] [PubMed] [Google Scholar]
- Glannon W. Bioethics and the Brain. Oxford: Oxford University Press; 2007. [Google Scholar]
- Grissom RJ, Kim JJ. Effect Sizes for Research: Univariate and Multivariate Applications. Abingdon: Routledge; 2014. [Google Scholar]
- Lachs J. The element of choice in criteria of death. In: Zaner M, editor. Death: Beyond Whole-Brain Criteria. Dordrecht: Kluwer Academic Publishers; 1988. pp. 233–251. [Google Scholar]
- Lindauer M. Experimental philosophy and fruitfulness of normative concepts. Philosophical Studies. 2019 doi: 10.1007/s11098-019-01302-3. [DOI] [Google Scholar]
- McMahan J. The metaphysics of brain death. Bioethics. 1995;9(2):91–126. doi: 10.1111/j.1467-8519.1995.tb00305.x. [DOI] [PubMed] [Google Scholar]
- McMahan J. The Ethics of Killing. Problems at the Margins of Life. New York: Oxford University Press; 2002. [Google Scholar]
- Miller FG, Truog RD. Death, Dying, and Organ Transplantation. New York: Oxford University Press; 2012. [Google Scholar]
- Nair-Collins M, Green SR, Sutib AR. Abandoning the dead donor rule? A national survey of public view on death and organ donation. Journal of Medical Ethics. 2014;41(4):297–302. doi: 10.1136/medethics-2014-102229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sass H. Criteria for death: Self-determination and public policy. The Journal of Medicine and Philosophy. 1992;17:445–454. doi: 10.1093/jmp/17.4.445. [DOI] [PubMed] [Google Scholar]
- Shah S. Rethinking Brain Death as a Legal Fiction: Is the Terminology a Problem? Defining Death: Organ Transplantation and Fifty-Year Legacy of the Harvard Report on Brain Death, Special Report, Hastings Center Report. 2018;48(6):49–52. doi: 10.1002/hast.955. [DOI] [PubMed] [Google Scholar]
- Shah SK, Truog RD, Miller FG. Death and legal fictions. Journal of Medical Ethics. 2011;37:719–722. doi: 10.1136/jme.2011.045385. [DOI] [PubMed] [Google Scholar]
- Shah SK, Kasper K, Miller FG. A narrative review of the empirical evidence on public attitudes on brain death and vital organ transplantation: The need for better data to inform policy. Journal of Medical Ethics. 2015;41(4):291–296. doi: 10.1136/medethics-2013-101930. [DOI] [PubMed] [Google Scholar]
- Singer P. Rethinking Life and Death. The Collapse of Our Traditional Ethics. New York: St. Martin’s Press; 1995. [Google Scholar]
- Truog RD. Is it time to abandon brain death? Hastings Center Report. 1997;27(1):29–37. doi: 10.2307/3528024. [DOI] [PubMed] [Google Scholar]
- Veatch RM. Death, Dying, and the Biological Revolution. New Haven: Yale University Press; 1989. [Google Scholar]
- Veatch RM. The impending collapse of the whole-brain definition of death. The Hastings Center Report. 1993;23(4):18–24. doi: 10.2307/3562586. [DOI] [PubMed] [Google Scholar]
- Veatch RM. The conscience clause how much individual choice in defining death can our society tolerate? In: Younger SJ, Arnold RM, Schapiro R, editors. The Definition of Death Contemporary Controversies. Baltimore: The John Hopkins University Press; 1999. pp. 137–160. [Google Scholar]
- Veatch RM, Ross LF. Defining Death. The Case for Choice. Washington: Georgetown University Press; 2016. [Google Scholar]
- Veatch RM. Controversies in defining Death: a case for choice. Theoretical Medicine and Bioethics. 2019;40:381–401. doi: 10.1007/s11017-019-09505-9. [DOI] [PubMed] [Google Scholar]
- Wijdicks EFM. Brain death worldwide: accepted fact but no global consensus in diagnostic criteria. Neurology. 2002;58(1):20–25. doi: 10.1212/WNL.58.1.20. [DOI] [PubMed] [Google Scholar]
- Yang Q, Miller G. East-west differences in perception of brain death. Journal of bioethical inquiry. 2015;12(2):211–225. doi: 10.1007/s11673-014-9564-x. [DOI] [PubMed] [Google Scholar]
- Younger SJ. Defining death a superficial and fragile consensus. Archives of Neurology. 1992;49(5):570–572. doi: 10.1001/archneur.1992.00530290162028. [DOI] [PubMed] [Google Scholar]
- Zeiler K. Deadly pluralism? Why death-concept, death-definition, death-criterion and death-test pluralism should be allowed, even though it creates some problems. Bioethics. 2009;23(8):450–459. doi: 10.1111/j.1467-8519.2008.00669.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.