Abstract
For both education and practice, the dissemination of the Joint Commission of Pharmacy Practitioner’s Patient Care Process for Pharmacists has heightened attention to the need for a defined care process for pharmacists. Yet, when one compares this framework with those described in other disciplines, what makes it specific to pharmacy? Graduates must establish their unique role in patient care management among the health care team. Therefore, it is essential that pharmacy educators prepare students to contribute uniquely and communicate articulately about those contributions. This involves intentionally teaching an explicit clinical assessment process and a recognized taxonomy for communicating medication-related needs. In addition, educators must: ensure integration of patient care frameworks unique to pharmacists in curricula, commit to critical evaluation of care process instruction, and partner with external stakeholders to establish the distinct contributions of pharmacists to team-based care.
Keywords: patient care, care process, pharmacy education
INTRODUCTION
A dentist, a pilot, and a pastry chef walk into a bar and the bartender asks, “What common trait brings the three of you together today?” While this might sound like the beginning of a cocktail party joke, there is no witty punchline to follow. Instead, the question the bartender poses is serious. What do these three professionals have in common? The answer has important implications for academic pharmacy and the profession as a whole.
The Academy needs greater consistency, specificity, and intentionality in terms of teaching a common patient care process1 across all points of pharmacist training across all pharmacy schools. The dentist, pilot, and pastry chef all have a defined “practice” or way of accomplishing their work that is intentional and provides the foundation for consistent outcomes and stakeholder recognition. A dentist is trained to apply a defined and consistent assessment process, starting each examination on the same tooth and working in the same direction. A patient will experience this process no matter who their provider, which contributes to their trust in the discipline, not just in the individual practitioner. Airline pilots have a pre-flight checklist that they review prior to each flight, in the same way, in the same order. The lead and co-pilot may not know each other, but they will implicitly understand their roles, expectations, and how to communicate with each other as they prepare a flight for departure. A pastry chef knows the importance of following the same recipes, using the same ingredients, following the same procedures in the same order to get the same results time and time again. Customer satisfaction (and that of the food critic who may unexpectedly stop by) is rooted in the ability to provide consistency day in and day out, even when the pastry chef is on vacation and another chef is responsible for preparing the desserts in his or her absence.
Lack of consistency in the implementation of the pharmacist’s patient care process (PPCP) is a detriment to the profession’s ability to demonstrate value. Consistency in practice starts in pharmacy school. Is the patient care work of a pharmacist any less important than that of the dentist, pilot, or pastry chef? Should our stakeholders (ie, patients, health care colleagues, health plans) experience differences in consistency or quality from individual practitioners of our profession? Standards that ensure consistency create trust in the experience a patient will have with a practitioner. We need to have internal standards that others can recognize. We see pilots walking through the airport with their bags of flight manuals, and we trust that they each subscribe to a process that will get us safely to our destination every single time.
As educators, we must ask ourselves: If a patient sees two pharmacists, will those pharmacists apply the same care process? Could that patient perceive inconsistency in the approach between pharmacists, causing them to question the specific role they play in health care? Will both pharmacists achieve the same positive outcomes through their clinical service, repeatedly, over many patient care encounters? We need to hold ourselves accountable for preparing graduates who can deliver care consistently, and we should expect others to hold educators accountable as well.
Teaching the General PPCP is Not Enough
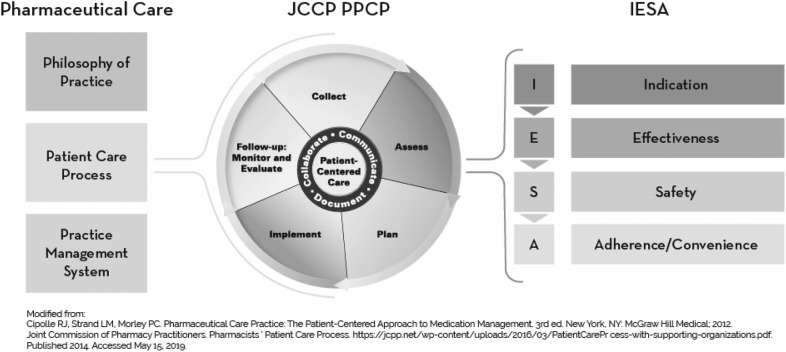
The PPCP’s basic, five-step framework is not distinctly unique to pharmacists. Collect, assess, plan, implement, and follow-up is the general process of care for all health professions.2-5 Of course the clinical work of a pharmacist is different than that of a physician or nurse. The care process becomes specific to pharmacy when it is driven by a philosophy of practice and supported by a practice management system7 where addressing all of a patient’s medication-related needs is the central purpose of the pharmacist’s work6,7 (Figure 1). In addition, it is made specific by a unique assessment process and a taxonomy that a pharmacist applies to define a patient’s mediation-related needs.
Figure 1.
Relationship Between Professional Practice Elements, The Patient Care Process, and Pharmacy’s Distinct Assessment Process
The assessment process and taxonomy are components of a “usable innovation.” Implementation science (ie, the study of methods that influence the integration of evidence-based interventions into practice) tells us that, a usable innovation must establish “essential functions” that define the practice and “operational definitions” for each of the essential functions.8 The essential functions and operational definitions are vital for the innovation to be taught, learned, and applied in a manner that consistently produces the intended outcome(s).8 Research applying the usable innovation framework to comprehensive medication management resulted in the definition outlined in The Patient Care Process for Delivering Comprehensive Medication Management (CMM): Optimizing Medication Use in Patient-Centered, Team-Based Care Settings.9 This work builds on the efforts of JCPP1 and other scholars.7,10 The operational definitions outline with specificity the thought process and actions a pharmacist will apply when carrying out the five steps of the PPCP. Readers should review the “operational definition” of a pharmacist’s assessment process in this resource and consider the following: To what degree are your faculty, staff, preceptors, and students consistently applying and teaching this process? To what extent is this nomenclature employed in your didactic and experiential teaching? For example, when a student is reviewing a patient’s medication needs, are they not only reviewing their existing medications but also ensuring that there is not an unmet indication (operational definition “2b” of the referenced document)?
As we see in the operational definition, the pharmacist’s assessment is rooted in the IESA (indication, effectiveness, safety, adherence/convenience) framework, which indicates the thought process used to determine that each medication is indicated, effective, and safe, and that the patient has the ability to adhere to the medication.7,11 This explicit assessment of each medication for indication, effectiveness, safety, and adherence is a unique contribution of the pharmacist. In addition, it is critical to creating consistency and affirming pharmacy’s value to the health care system. When approaching a patient’s medications, students need to use the IESA framework and be held accountable for this assessment process. It is this thought process that ensures a thorough and accurate review of a patient’s medication-related needs, just like a pilot’s pre-flight checklist ensures nothing is overlooked before a flight departs for its destination.
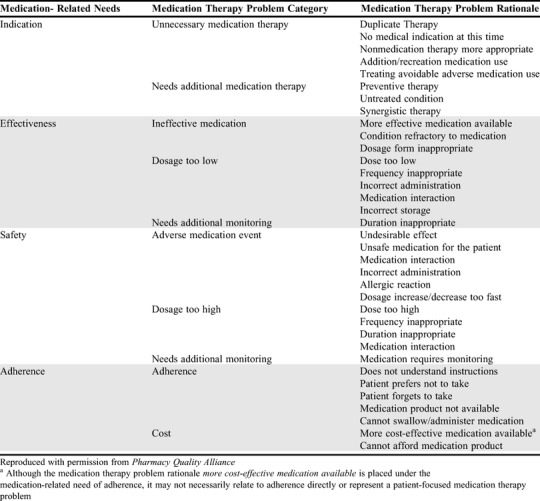
As a component of the PPCP process, a taxonomy is needed to define and communicate medication therapy problems. Along with the assessment process, this taxonomy establishes the uniqueness of the pharmacist’s contribution to quality of care. The Medication Therapy Problem Framework11 (MTPF, which is explicitly aligned with the IESA framework) has been adopted by the Pharmacy Quality Alliance (PQA) (Table 1). The PQA is a national entity whose mission is optimizing health by advancing the quality of medication use. The profession should view the PQA’s actions to promote this framework as affirming a standard of practice. Again, when you review this framework, consider the degree to which your faculty, staff, preceptors, and students consistently apply and teach this framework in didactic, simulated or experiential learning settings.
Table 1.
Medication Therapy Problem Categories Framework for Pharmacy Quality Alliance Measures
Education as a Foundation for Expanding Roles for Pharmacists
As payment models shift to reward services that improve health and lower costs, new roles for pharmacists require demonstrating value to payers, executives, and teams. Thus, a fundamental question is whether the patient care services of pharmacists produce value in health care. We anticipate that most readers would assume that, yes, the clinical services of pharmacists produce value. However, a 2014 systematic review by Viswanathan and colleagues involving 44 studies focused on measuring the impact of clinical services provided by pharmacists concluded that the answer to this question is “maybe.”18 The reason? They found that, across the 44 studies reviewed, the specific intervention delivered by pharmacists was either unstated or lacked specificity. The authors concluded, “New research, regardless of specific focus, will likely continue to find inconsistent results until underlying sources of heterogeneity [in practice specificity] are accounted for.” This finding was similar to that identified in a separate systematic review.19
Expanded employment opportunities for pharmacists will be realized if stakeholders believe that three key specifics are true: the care delivered by pharmacists has a significant positive impact on health care quality and costs; this care is accomplished via a service that is distinct to pharmacists and unable to be delivered by another health care provider at a lower price point; and the care process of pharmacists that creates value is consistently delivered across all settings and situations. Schools and colleges of pharmacy should provide the foundation that will establish these “truths.” We must commit to rigor and discipline in instruction across all facets of our curricula and in the expectations that we set for faculty and preceptors.
Committing to Honesty While Reflecting on Curricular and Instructional Design
In considering our teaching related to the PPCP, we must resist the urge to assume or say, “we are already doing this,” a phrase that has been stated countless times over the past two decades by both academics and practitioners. The issue of consistency in care is too important to avoid critical consideration of current instructional efforts. Accreditation Council for Pharmaceutical Education (ACPE) Standard 10.8 requires schools to prepare students “to provide patient-centered collaborative care as described in the Pharmacists’ Patient Care Process model endorsed by the Joint Commission of Pharmacy Practitioners.”12 However, there is no established expectation for the process and methods a school uses to achieve this standard. Recent publications suggest that action is being taken. Several papers have described methods schools are using to incorporate the PPCP within their curricula.13-17 However, it is unclear to what degree schools have addressed the teaching and assessed competency with IESA and the MTPF, which are the unique elements of the pharmacists’ patient care process.
Every school must critically and honestly examine its curriculum and its instructional strategies and question the degree to which it consistently teaches a patient care process unique to pharmacists. To place the importance of this analysis into context, consider the following:
If a school of dentistry was not consistently preparing its graduates to assess patients in a consistent man ner, what would be the actions of that school’s accrediting body? A citation would likely occur and a requirement for resolution and reporting would be levied.
What would be the actions of an airline if one of its pilots was identified as inconsistently applying stan dard flight procedures? If competency was not quickly established, sanctions, remediation and ul timately dismissal would be expected.
What are the implications for a pastry chef who dem onstrates inconsistency in their product? They might be demoted to an assistant role or terminated. If they were the owner of the establishment, reduced revenues may potentially lead to closure of the business.
For these three practitioners (the dentist, the pilot, and the pastry chef), the stakes are high. A lack of performance or inconsistent instruction within the core of the discipline could result in the type of actions that might discontinue their role within their profession. Again, we ask, is the patient care work of pharmacists any less important than that of the work of the dentist, pilot, or pastry chef? Should the ramifications of inconsistent practice or instruction be any less severe for pharmacists or pharmacy educators? At each college and school, we must discuss and debate our responses to the following questions:
In our core curriculum, where, how, and how well do we explicitly teach and assess students in their use of the IESA assessment process? Are we assured that each student determines the indication; effective ness; safety; and adherence of each medication for each patient?
Where, how, and how well do we explicitly teach and assess students in the classification, documentation, and communication of the outcomes of their clinical assessment using the MTP Framework?
To what degree are students applying the IESA assessment process and the MTPF in their education experience, including didactic, simulation, and experiential education? Are they used early and often in the curriculum?
What evidence do we have that our preceptors role model this assessment process and expect students to apply it?
What evidence do we have that pharmacy students are consistently assessing using IESA and communicat ing problems using MTRF (ie, demonstrating the unique contributions of pharmacists) on interprofes sional teams?
As the demands of the health care environment esca late, can employers fully depend on receiving a graduate that consistently delivers care, and there fore, consistently delivers value, to the health care team?
The credibility of the profession is at stake. If we cannot produce graduates who can consistently deliver care and value to the team, then we must consider whether society should continue to invest in the pharmacy practice and education.
CONCLUSION
The next time you visit the dentist, board an airplane, or enjoy a well-prepared dessert, take a moment to recall that the trust, safety, and enjoyment inherently produced by the respective practitioners of these services does not occur by chance. There is a rigor to the discipline and training held by each of these individuals that produces the positive outcome you experience and the sense of value you assign to their work. Our graduates are entering a health care system where expectations for the skills and expertise of pharmacists are growing. If we send these graduates into that environment without a foundation that prepares them to consistently apply a unique care process, academic pharmacy will have failed in its primary opportunity to influence the health of patients. The Academy must embrace and promote the standards for rigor and quality that will drive the profession’s ability to thrive in a changing health care environment. In embracing our responsibility to develop the most well-prepared workforce poised to manage the medication needs of patients and our society, we must also seek learnings from across our programs, share our own successes, and join a shared commitment to lead the work of adopting the critical components of a care process unique to pharmacists. There is an imperative to establish a community of learning across schools and colleges in order to accelerate adoption and spread of instructional efforts that produce consistency among graduates.
REFERENCES
- 1.Joint Commission of Pharmacy Practitioners. Pharmacists ’ Patient Care Process. 2014. https://jcpp.net/wp-content/uploads/2016/03/PatientCareProcess-with-supporting-organizations.pdf. Accessed May 22, 2019.
- 2.American Nurses Association. The Nursing Process. https://www.nursingworld.org/practice-policy/workforce/what-is-nursing/the-nursing-process/. Accessed April 14, 2020.
- 3.Writing Group of the Nutrition Care Process/Standardized Language Committee. Nutrition Care Process and Model Part I: The 2008 Update. J Am Diet Assoc. 2008;108(7):1113-1117. [DOI] [PubMed] [Google Scholar]
- 4.Lacey K, Pritchett E. Nutrition care process and model: ADA adopts road map to quality care and outcomes management. J Am Diet Assoc. 2003;103(8):1061-1072. [DOI] [PubMed] [Google Scholar]
- 5.American Physical Therapy Association. Guidelines: Physical Therapy Documentation of Patient/Client Management. 2009. https://www.apta.org/uploadedFiles/APTAorg/About_Us/Policies/BOD/Practice/DocumentationPatientClientMgmt.pdf. Accessed April 14, 2020.
- 6.Pestka DL, Sorge LA, McClurg MR, Sorensen TD. The philosophy of practice for comprehensive medication management: Evaluating its meaning and application by practitioners. Pharmacother J Hum Pharmacol Drug Ther. 2018;38(1):69-79. [DOI] [PubMed] [Google Scholar]
- 7.Cipolle RJ, Strand LM, Morley PC. Pharmaceutical Care Practice: The Patient-Centered Approach to Medication Management Services. 3rd ed. New York, NY: McGraw Hill Professional; 2012. [Google Scholar]
- 8.Fixsen D, Blase K, Metz A, Van Dyke M. Implementation Science. In: Wright J, ed. International Encyclopedia of the Social and Behavioral Sciences. 2nd ed. Oxford, UK: Elsevier Ltd; 2015:695-702. [Google Scholar]
- 9.Roth McClurg M, Sorensen TD, Carroll J, et al. . The Patient Care Process for Delivering Comprehensive Medication Management (CMM): Optimizing Medication Use in Patient-Centered, Team-Based Care Settings. C Primary Care Res Team. 2018. http://www.accp.com/cmmcareprocess. Accessed April 14, 2020.
- 10.Patient-Centered Primary Care Collaborative. The Patient-Centered Medical Home: Integrating Comprehensive Medication Management to Optimize Patient Outcomes Resource Guide. 2012. www.pcpcc.org/sites/default/files/media/medmanagement.pdf. Accessed April 14, 2020.
- 11.Pharmacy Quality Alliance. Medication Therapy Problem Categories Framework for PQA Measures. https://www.pqaalliance.org/assets/Measures/PQA%20MTP%20Categories%20Framework.pdf. Accessed April 14, 2020.
- 12.Accreditation Council for Pharmacy Education. Accreditation Standards and Key Elements for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. 2015. https://www.acpe-accredit.org/pdf/Standards2016FINAL.pdf. Accessed April 14, 2020.
- 13.Cooley J, Lee J. An operationalization of the Pharmacists’ Patient Care Process at on public college of pharmacy. Am J Pharm Educ. 2017;82(2):Article 6301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kolar C, Hager KD, Losinski V. Beyond the pharmacists’ patient care process: cultivating patient care practitioners by utilizing the pharmaceutical care framework. Inov Pharm. 2017;8(3):Article 7. [Google Scholar]
- 15.Hager KD, Kolar C, Janke KK. Concept mapping, reflective writing, and patchwork text assessment in a first-year pharmaceutical care course. Curr Pharm Teach Learn. 2016;8(4):492-500. [Google Scholar]
- 16.Gonyeau MJ, DiVall M, Conley MP, Lancaster J. Integration of the Pharmacists’ Patient Care Process (PPCP) into a comprehensive disease management course Series. Am J Pharm Educ. 2018;82(5):Article 6311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rivkin A. Thinking clinically from the beginning: early introduction of the pharmacists’ patient care process. Am J Pharm Educ. 2016;80(10):Article 164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Viswanathan M, Kahwati LC, Golin CE, et al. . Medication therapy management interventions in outpatient settings. JAMA Intern Med. 2015;175(1):76-87. [DOI] [PubMed] [Google Scholar]
- 19.Greer N, Bolduc J, Geurkink E, et al. . Pharmacist-led chronic disease management: a systematic review of effectiveness and harms compared with usual care. Ann Intern Med. 2016;165(1):30. [DOI] [PubMed] [Google Scholar]