Abstract
Purpose
Air pollutant exposure constitutes a serious risk factor for the emergence or aggravation of (existing) pulmonary disease. The impact of pre-intensive care ambient air pollutant exposure on the duration of artificial ventilation was, however, not yet established.
Methods
The medical records of 2003 patients, admitted to the intensive care unit (ICU) of the Antwerp University Hospital (Flanders, Belgium), who were artificially ventilated on ICU admission or within 48 h after admission, for the duration of at least 48 h, were analyzed. For each patient’s home address, daily air pollutant exposure [particulate matter with an aerodynamic diameter ≤ 2.5 µm (PM2.5) and ≤ 10 µm (PM10), nitrogen dioxide (NO2) and black carbon (BC)] up to 10 days prior to hospital admission was modeled using a high-resolution spatial–temporal model. The association between duration of artificial ventilation and air pollution exposure during the last 10 days before ICU admission was assessed using distributed lag models with a negative binomial regression fit.
Results
Controlling for pre-specified confounders, an IQR increment in BC (1.2 µg/m3) up to 10 days before admission was associated with an estimated cumulative increase of 12.4% in ventilation duration (95% CI 4.7–20.7). Significant associations were also observed for PM2.5, PM10 and NO2, with cumulative estimates ranging from 7.8 to 8.0%.
Conclusion
Short-term ambient air pollution exposure prior to ICU admission represents an unrecognized environmental risk factor for the duration of artificial ventilation in the ICU.
Electronic supplementary material
The online version of this article (10.1007/s00134-020-05999-3) contains supplementary material, which is available to authorized users.
Keywords: Air pollution, Intensive care, Artificial ventilation, Mechanical ventilation, Critical care
Take-home message
| Short-term ambient particulate and gaseous air pollution exposure prior to ICU admission significantly prolongs the duration of mechanical ventilation irrespective of preexisting lung disease or ICU admission diagnosis. This finding suggests that optimizing air quality could influence ICU-related morbidity. |
Introduction
The usual outdoor traffic-related air polluting suspects comprise gaseous (e.g., nitrogen dioxide (NO2)) and particulate pollutants generated by combustion processes. Particulate matter (PM) is a heterogenic mixture of solid and liquid particles of organic and inorganic substances, drifting in the air. Mostly, sulfate, nitrates, ammonia, sodium chloride, black carbon, mineral dust and water are present, though heavy metals, polycyclic aromatic hydrocarbons, bacteria, viruses and even pollen can also be found [1]. Relevant to human health, inhalable particles are categorized by aerodynamic diameter: equal or less than (≤) 10 µm (PM10), ≤ 2.5 µm (PM2.5) or ≤ 0.1 µm (PM0.1). Black carbon (BC), a component of PM2.5 formed through incomplete combustion processes, is often used—in addition to NO2—as a proxy of traffic-related air pollution.
The smaller the particle, the deeper the penetration in the respiratory system, leading to inflammatory reactions on the alveolar level, resulting in cytotoxicity and possible mutagenesis [2, 3]. As such, ambient air pollution constitutes a serious risk factor not only for the emergence of respiratory infections, but also for the development of reduced pulmonary function and/or aggravation of existing pulmonary disease (e.g., asthma, cystic fibrosis, chronic obstructive pulmonary disease [COPD]) [4–7].
In analogy with the recent finding that patient pre-admission medical and sociodemographic characteristics (e.g., medication use, immune status, frailty) can influence the course and outcome and even the degree of respiratory failure during intensive care unit (ICU) admission [8–10], we investigated the association between short-term exposure to residential ambient air pollution and the duration of mechanical ventilation in ICU patients.
Methods
A detailed description of the methods is provided in an electronic supplement.
Study population
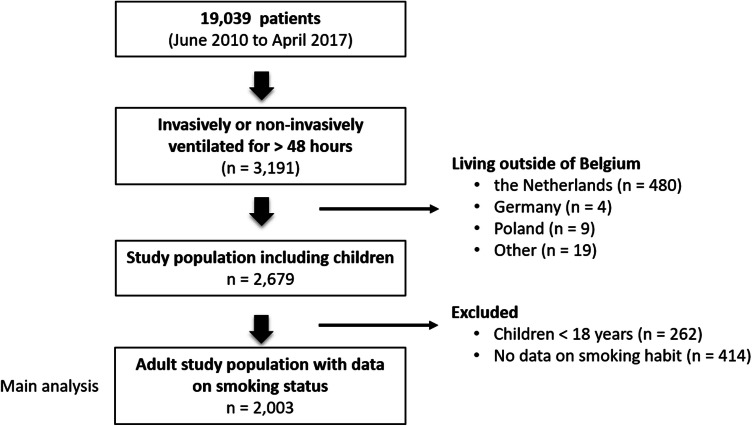
We conducted a large-scale cohort study in the 45-bed tertiary ICU of the Antwerp University Hospital (Flanders, Belgium). Medical records of 19,039 patients, admitted from June 6, 2010, up to and including April 15, 2017, were analyzed for all modes of artificial (invasive and noninvasive) ventilation within 48 h of admission. Clinical data were primarily retrieved from the patient data management system (PDMS) (Metavision, iMDsoft, Düsseldorf, Germany), while personal information (e.g., smoking status) was retrieved from other medical records. Our study was approved by the ethical committee of the University of Antwerp/Antwerp University Hospital (AIRPOLLUTIC trial, 17/12/162). A total of 3191 patients were mechanically ventilated within the first 48 h of admission for the duration of at least 48 h. After exclusion of patients living outside of Belgium (n = 512), removal of patients with no data on smoking status (n = 414) and elimination of children (< age 18 years) (n = 262), our final study population comprised 2003 patients (Fig. 1).
Fig. 1.
Flowchart depicting the selection procedure of patients admitted to the intensive care unit of the Antwerp University Hospital located in Belgium between June 6, 2010, and April 15, 2017
We obtained relevant demographic and clinical data in every patient and used the Simplified Acute Physiology Score (SAPS3) as a validated score for severity of illness [11]. We also obtained information on APACHE IV [12]. Ventilation duration was calculated by summing the duration (in hours) of all consecutive (invasive and noninvasive) ventilation episodes during the same ICU admission and was rounded to the nearest number of whole days.
Ambient air pollution exposure assessment
Residential addresses were geocoded with ArcGIS 10 software. Residential PM2.5, PM10, BC and NO2 exposure levels (µg/m3) were modeled for each patient’s address using a high-resolution spatiotemporal model [13]. The model takes into account land cover data obtained from satellite images (CORINE land cover data set) and pollution data from fixed monitoring stations in combination with a dispersion model [14]. We calculated the daily concentrations of air pollutants at the patient’s residential address up to 10 days before admission (lag0 to lag10, with lag0 representing the day of admission). For a sensitivity analysis, we calculated the annual average air pollution levels (as a proxy for long-term exposure).
Statistical analysis
Short-term health effects of environmental stressors may become apparent only a few or more days after exposure, implying that exposures during several days (lags) before the effect on human health should be considered. Instead of testing associations with lagged exposures in separate models, distributed lag (nonlinear) models [DL(N)Ms] provide a flexible methodology to capture the temporal pattern of the association by entering different lags in one and the same model. The primary study outcome was the duration of ventilation in days. The association between ventilation duration and air pollution exposure was investigated by negative binomial regression, using a separate model for each of the four pollutants. Potential delayed effects of air pollution on ventilation duration up to 10 days before ICU admission (lag0 to lag10) were allowed by using DLNMs [15], with lag0 representing the day of admission, lag1 the day before admission and so on. The exposure–response function was modeled using a natural cubic spline with 5 df. Seasonality and long-term trends were modeled using a natural cubic spline of time (day of the study period) with 6 df per year. Models were additionally adjusted for indicator variables for day of the week and for known determinants of duration of ventilation such as sex, age (modeled with a natural cubic spline with 3 df), BMI (kg/m2), disease severity (SAPS3), smoking status (non-smoker/active smoker), origin of the patient before ICU admission (emergency department/other) and admission diagnosis (non-respiratory/respiratory non-infectious respiratory infectious).
In a secondary analysis, we adjusted our models for APACHE IV. In an effort to account for exposure misclassification in patients who were admitted to the hospital some days before ICU admission (e.g., 6 days at home, 4 days in the hospital, then ICU admission), we performed an analysis where we combined the daily exposure values derived at the home address with the daily exposure values derived at the hospital. Alternatively, we excluded patients coming from another hospital ICU to account for possible exposure misclassification (resulting in n = 1755). In another secondary analysis, we accounted for possible confounding due to respiratory comorbidities by excluding all patients with preexisting lung disease including COPD and asthma (resulting in n = 1672) and by excluding all patients with preexisting respiratory and neuromuscular comorbidities (n = 1463). We then further restricted the study population to patients who left the ICU alive (n = 1027) to account for early death. Finally, to differentiate between short- and long-term effects, we added annual average air pollution levels (as a proxy for long-term exposure) to our main model. Reported estimates represent the lag-specific and cumulative (lag0–10 days) percentage change (with 95% confidence intervals [CI]) in ventilation duration for an interquartile range (IQR) increase in air pollution exposure. All analyses were performed with the statistical software R (R Foundation for Statistical Computing, Vienna, Austria) using the “dlnm” package [16].
Results
Population characteristics
Demographic and clinical characteristics of the 2003 adult patients are summarized in Table 1. 48.3% of our study population were 65 years or older. There were more men (65.3%) than women (34.7%), and nearly one-third (30.7%) of our population were smokers. Approximately 70% of our population was admitted with a non-respiratory diagnosis, only 7.8% with a non-infectious respiratory disease and 22.1% with a respiratory infection. The mean (± SD) ventilation duration was 12 (± 13) days with the majority of patients (73.7%) having only one episode of ventilation.
Table 1.
Characteristics of the total study population (n = 2003)
| Characteristic | Mean ± SD or n (%) |
|---|---|
| Age, y | 62 ± 15 |
| BMI, kg/m2 | 26.6 ± .7.6 |
| Sex | |
| Male | 1308 (65.3) |
| Female | 695 (34.7) |
| Smoking status | |
| Non-smoker | 1389 (69.3) |
| Smoker | 614 (30.7) |
| Season of admission | |
| Winter (Dec–Mar) | 558 (27.9) |
| Spring (Mar–Jun) | 456 (22.8) |
| Summer (Jun–Sep) | 485 (24.1) |
| Autumn (Sep–Dec) | 504 (25.2) |
| SAPS3 | 61.0 ± 15.8 |
| APACHE IV | 40.6 ± 26.2 |
| Diagnosis | |
| Non-respiratory | 1405 (70.1) |
| Respiratory non-infectiousa | 156 (7.8) |
| Respiratory infectiousb | 442 (22.1) |
| Comorbidities | |
| COPD | 283 (14.1) |
| Asthma | 59 (2.9) |
| Other respiratoryc | 152 (7.6) |
| Neuromusculard | 73 (3.6) |
| Mortality | |
| ICU mortality | 635 (31.7) |
| Hospital mortality | 810 (40.4) |
| 28-day mortality | 622 (31) |
| Admission origin | |
| Emergency department | 592 (29.5) |
| Operating room | 518 (25.9) |
| Other hospital ICU | 240 (12) |
| Conventional ward | 424 (21.2) |
| Medium care unit | 169 (8.4) |
| Othere | 60 (3) |
| Ventilation (days) | 12.4 ± 13.4 |
| Episodes of ventilation | 1.4 ± 0.9 |
aFor example, acute lung injury not related to an infectious disease, non-infectious COPD exacerbation, CO intoxication, lobectomy, lung emboli, pneumonectomy, thoracic trauma, upper airway obstruction
bFor example, acute lung injury in conjunction with a respiratory infection, bronchiolitis, infectious COPD exacerbation, empyema, mediastinitis, pneumonia
cFor example, asbestoses, cystic fibrosis, lung fibrosis, obstructive sleep apnea syndrome, pneumonectomy, etc. (n = 2000)
dFor example, amyotrophic lateral sclerosis, Duchenne muscular dystrophy, Guillain–Barré syndrome, multiple sclerosis, myotonic dystrophy, etc. (n = 1999)
eOther origin includes maternity ward, coronary catheterization unit, interventional radiology and the recovery room after major surgery
Ambient exposure levels
Median (5th–95th percentiles) daily air pollution exposures up to 10 days before admission were 1.2 (0.4–3.6) μg/m3 for BC, 11.4 (4.5–37.3) μg/m3 for PM2.5, 18.9 (9.4–47.0) μg/m3 for PM10 and 23.5 (8.2–49.5) μg/m3 for NO2 (Table 2). The majority of participants lived in the province of Antwerp, relatively close to the Antwerp University Hospital, where we observed the highest levels of PM2.5 exposure in Belgium (Figure Electronic supplement)
Table 2.
Distribution of daily air pollution concentrations and temperature up to 10 days before admission
| Pollutant | P5 | P25 | P50 | P75 | P95 | IQR |
|---|---|---|---|---|---|---|
| BC (µg/m3) | 0.4 | 0.8 | 1.2 | 1.9 | 3.6 | 1.2 |
| PM2.5 (µg/m3) | 4.5 | 7.4 | 11.4 | 18.8 | 37.3 | 11.4 |
| PM10 (µg/m3) | 9.4 | 14 | 18.9 | 26.8 | 47 | 12.8 |
| NO2 (µg/m3) | 8.2 | 15.6 | 23.5 | 33.1 | 49.5 | 17.5 |
| Temp. (°C) | 0.3 | 5.9 | 10.5 | 15.5 | 20.6 | 9.6 |
IQR interquartile range
PM2.5, PM10 = particulate matter with an aerodynamic diameter ≤ 2.5 and 10 μm, respectively, BC black carbon, NO2 = nitrogen dioxide
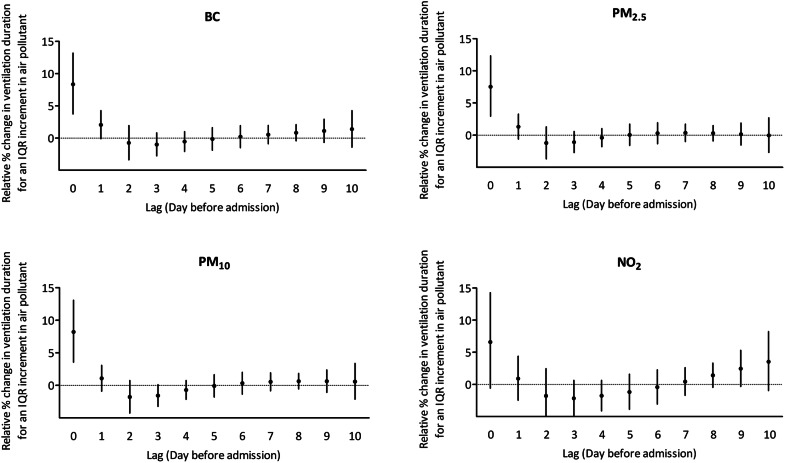
Main analysis
The lag-specific DLM estimates of the association between ventilation duration and air pollutant exposures up to 10 days before the ICU admission are shown in Fig. 2. The effect of all examined components of air pollution on ventilation duration was found to be acute, with significant effect estimates at lag0 (except for NO2) and estimates close to zero after lag1. An IQR (1.2 µg/m3) increment in BC exposure up to 10 days before ICU admission was associated with a 12.4% (95% CI 4.7 to 20.7) longer mechanical ventilation duration (Table 3). The corresponding estimates for PM2.5, PM10 and NO2 were 7.9% (95% CI 0.5–15.9), 7.8% (95% CI 0.4–15.8), and 8.0% (95% CI 0.02–16.4), respectively.
Fig. 2.
Lag-specific DLM estimates of the association between mechanical ventilation duration and exposure to air pollutants up to 10 days before ICU admission (lag0 to lag10). Estimates are presented for an IQR increment in BC (1.2 µg/m3), PM2.5 (11.4 µg/m3), PM10 (12.8 µg/m3) and NO2 (17.5 µg/m3). Models were adjusted for ambient temperature up to 10 days before admission, long-term trends and seasonality, age, sex, BMI, smoking status, SAPS3, day of the week, ICU origin and admission diagnosis. PM2.5, PM10 = particulate matter with an aerodynamic diameter ≤ 2.5 and 10 μm, respectively; BC black carbon, NO2 = nitrogen dioxide
Table 3.
Effect estimates of the association between ventilation duration (percentage change) and air pollutant exposure up to 10 days before ICU admission
| Model | No. | Air pollutant | |||
|---|---|---|---|---|---|
| BC (+ 1.2 µg/m3) | PM2.5 (+ 11.4 µg/m3) | PM10 (+ 12.8 µg/m3) | NO2 (+ 17.5 µg/m3) | ||
| Main model | 2003 | 12.4 (4.7, 20.7) | 7.9 (0.5, 15.9) | 7.8 (0.4, 15.8) | 8 (0.2, 16.4) |
| Corrected for APACHE IV instead of SAPS3 | 2003 | 12.4 (4.7, 20.6) | 7.3 (− 0.8, 16) | 7.8 (0.2, 16.2) | 8 (0.2, 16.4) |
| Accounting for exposure misclassification | 2003 | 11 (2.6, 20) | 7.1 (− 1.0, 15.8) | 7.9 (0.1, 16.4) | 8.1 (− 0.9, 17.9) |
| Excl. patients coming from another ICU | 1755 | 12.2 (4, 21) | 7.3 (− 1.3, 16.7) | 8.5 (0.1, 17.6) | 9.1 (0.7, 18.2) |
| Excl. COPD, asthma | 1672 | 16.9 (8.1, 26.5) | 11.5 (2.4, 21.5) | 11.4 (2.5, 21) | 10.5 (1.8, 19.8) |
| Excl. respiratorya, neuromuscular comorbidities | 1463 | 16.6 (7, 27) | 10 (0.2, 20.8) | 10.2 (0.7, 20.7) | 10.6 (1.4, 20.6) |
| Excl. respiratorya, neuromuscular comorbidities & deaths | 1027 | 17.9 (6.5, 30.4) | 8.4 (− 2.9, 21) | 9.1 (− 1.9, 21.3) | 12.2 (1.2, 24.4) |
The estimates represent the cumulative percentage change in ventilation duration for an IQR (μg/m3) increment in the air pollutant up to 10 days before the ICU admission
All models were adjusted for long-term trends and seasonality, age, sex, BMI, smoking habit, SAPS3, day of the week, ICU origin and admission diagnosis
aIncluding preexisting COPD, asthma and all other respiratory comorbidities
PM2.5, PM10 = particulate matter with an aerodynamic diameter ≤ 2.5 and 10 μm, respectively, BC black carbon, NO2 = nitrogen dioxide
Secondary analysis
Correcting our models for APACHE IV or using data where we took into account possible exposure misclassification had a little effect on our estimates for all pollutants except that the estimates of PM2.5 did not reach significance anymore (Table 3). Excluding patients who had been hospitalized in another hospital ICU, days prior to admission to our ICU, also did not change our effect estimates substantially (Table 3). Restricting our analysis to patients without preexisting COPD and asthma resulted in stronger associations for all pollutants: 16.9% (95% CI 8.1–26.5) for BC, 11.5% (95% CI 2.4–21.5) for PM2.5, 11.4% (95% CI 2.5–21.0) for PM10, and 10.5% (95% CI 1.8–19.8) for NO2 even after excluding all patients with respiratory and neuromuscular comorbidities. Further restricting the study population to patients without preexisting comorbidities, leaving the ICU alive, resulted in a further increase in cumulative effect estimates for BC and NO2 and similar (although no longer significant) estimates for PM2.5 and PM10. To differentiate between short- and long-term effects, we added annual average air pollution levels (as a proxy for long-term exposure) to our main model but found it not to be associated with the duration of ventilation.
Discussion
In our study of ICU patients, requiring mechanical ventilatory support for a diversity of reasons, ventilation duration was significantly associated with pre-admission exposure to BC, PM2.5, PM10 and NO2. For an IQR higher air pollution exposure up to 10 days before admission, the duration of ventilation was estimated to be 7.8–12.4% longer. Our data were obtained in a large and diverse ICU population, and the relationship between air pollution exposure and duration of ventilation was shown irrespective of preexisting lung disease or ICU admission diagnosis.
It has been shown that medical and sociodemographic characteristics [8, 10, 17] already present prior to ICU admission contribute to the occurrence and severity of organ failure including respiratory failure as well as the outcome in the critically ill. However, pre-admission environmental factors have hardly been studied in this context, or studies have found no effect (i.e., sunlight exposure prior to ICU admission has been found not to influence the incidence of ICU-acquired delirium) [18]. We are the first to report on the effect of pre-admission air pollution exposure on the duration of mechanical ventilation.
The findings of this study are of critical public health importance because of the ubiquity of ambient air pollution. Short-term ambient particulate air pollution is independently associated with daily all-cause, cardiovascular and respiratory mortality [19, 20]. As such, air pollution has important molecular and physiological effects on the lung, an organ frequently failing in the critically ill. A few recent studies have demonstrated some effects of air pollution on the occurrence of (only) the acute respiratory distress syndrome (ARDS) and associated mortality. Long-term ozone and PM2.5 exposure are associated with an increased risk for ARDS among older adults in the USA [21] and in patients at risk for ARDS (e.g., trauma patient, active smoker) [22]. Rush et al. [23] described how chronic exposure to high levels of ozone and PM results in higher mortality rates in ARDS patients, and most recently, Reilly et al. [24] added long-term exposure to low to moderate levels of sulfur dioxide, NO2 and carbon monoxide to the risk factors for ARDS in trauma patients.
Our results indicate the acute effects of air pollution on ventilation duration. Significant associations were observed for lag0, representing the day of ICU admission, but positive estimates (close to significance for BC and PM2.5) were also observed for lag1. A similar lagged pattern (lag0 and lag1) has been shown in a recent study investigating the association between the short-term effect of ambient air pollution (PM1 and PM2.5) and hospital admission for respiratory diseases [25]. The mechanism of this lagged pattern is not completely understood, but (pulmonary and/or systemic) oxidative stress and inflammation might be plausible biological mechanisms. For example, in a prospective panel study, increased blood levels of C-reactive protein and ICAM-1 were observed for an increase in PM10 and ultrafine particles with a delay of 1–2 days [26]. In 3996 individuals of the Framingham Heart Study, elevated exposure to relatively low levels of ambient air pollution for a few days was associated with higher levels of biomarkers of systemic inflammation (including C-reactive protein, interleukin-6 and tumor necrosis factor receptor 2) [27]. Therefore, it is reasonable to assume that acute air pollution-induced inflammation processes occur, at least in the lung, since this is the primary site of inflammation. The effects of air pollutants on the lung originate from extracellular activation of the inflammatory response and/or oxidative stress-mediated inflammation in airway epithelial cells [28].
Known detrimental effects of airway inflammation comprise a reduction in pulmonary function, increased airway reactivity with hypersecretion of mucus and alterations in mucociliary activity [29]. The latter will of course contribute to a protracted exposure of the airway epithelium to toxic particles, thus generating a prolonged inflammatory response. We hypothesize that inflammatory reactions on the alveolar, airway and/or pulmonary capillary level result in gas exchange impairment, thus contributing to the lengthening of ventilation duration.
Modern critical care does not only focus on the prevention of primary ventilation-associated morbidities such as ventilator-associated pneumonia or barotrauma [30, 31] but also tries to prevent long-term sequela related to prolonged mechanical ventilation by the use of short-acting sedatives and daily appraisal of the need for mechanical ventilation. Indeed, duration of ventilation-related conditions such as cognitive impairment, depression, neuro-myopathy and pulmonary function alterations (e.g., reduced diffusion capacity) can persist in the ICU survivor, resulting in a long-term need of medical, psychological and/or physiotherapeutic care, causing considerable economic burden [32, 33]. Our data thus represent a novel and potentially modifiable environmental risk factor, which, if improved, will not only ameliorate the post-ICU quality of life but might also reduce health care costs. The incentive to “clear the air” will gain even more importance in the future, considering the projected increase in an aging [34] population who are even more at risk for air pollution-related respiratory diseases due to an age-related defective mucociliary function in combination with decreased muscle strength, compromising the ability to clear inhaled particles [35, 36].
Our study was conducted in the northern part of Flanders (Belgium), where levels of air pollutants continued to decrease between 2010 and 2017. In 2017, the annual levels of air pollutants in our study population nearly reached the WHO standards for PM2.5 (12.8 vs. 10 µg/m3) and for PM10 (20.2 vs. 20 µg/m3) and even dived under the limit for NO2 (23.4 vs. 40 µg/m3) (Table Electronic supplement) [1]. The European Union (EU) air quality directives are less stringent (annual limits 25 μg/m3 for PM2.5, 40 µg/m3 for PM10 and NO2) than the WHO guidelines. In light of the fact that we found significant effects on duration of ventilation at air pollution levels well below the EU limits, our findings support a further down-revision of the current EU air pollution directives in the direction of the WHO guidelines.
Our findings need to be interpreted within the context of its strengths and limitations. Although we used validated exposure models, there might be some exposure misclassification. For example, we interpolated daily exposure levels at the residence without taking the amount of exposure at the address of employment or the time spent indoors into account. However, considering the higher age and expected preexisting health problems in our study population, we may assume that a considerable portion of time before admission was spent at the home address. Furthermore, a number of patients had been admitted to our hospital some days before ICU admission, thus generating some exposure misclassification. However, it is reasonable to assume that the exposure misclassification is random, resulting in an underestimation of effect estimates [37, 38]. Moreover, our findings stayed robust after accounting for possible exposure misclassification and excluding patients coming from another hospital ICU. In terms of validity of the exposure model, we showed that the estimated long-term residential exposure correlates with the internal nano-sized carbon load in urine [39].
Secondly, we recognize the multifactorial character of ventilation duration, but we wish to emphasize that the use of short-acting sedatives, lung-protective ventilation and spontaneous breathing trials has been the mainstay of ICU ventilation care in the Antwerp University Hospital before, during and after the study period. Any differences in duration of ventilation are therefore not attributable to physician-specific particularities, but a priori to (preexistent) patient characteristics. Additionally, our findings were robust after adjusting for APACHE IV, excluding all patients with preexisting lung disease (COPD and asthma) or other comorbidities and even after excluding the patients that died in the ICU to account for the competing risk of early mortality. Thirdly, due to patient heterogeneity in the intensive care and random exposure misclassification—which cannot be ruled out in epidemiology—we observed relatively wide confidence intervals around our estimates. Finally, we could not retrieve information on socioeconomic status (SES). Although SES is important in long-term exposure outcomes, it is less likely to be an important confounder in acute exposure studies as no relation between short-term temporal differences in air pollution exposure and SES is expected.
Conclusion
Our results add to the growing body of evidence that links air pollution exposure to respiratory health. Our study is the first to examine the effect of pre-admission ambient air pollution on duration of artificial ventilation in the ICU. Our results suggest that a further optimization of air quality could influence ICU-related morbidity and—although not directly studied—ICU-related health costs. Our study also demonstrates that exposure to “low-level” air pollution prior to mechanical ventilation is clinically relevant.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
This study received no external funding. No entity other than the authors listed played any role in the design of the study; the collection, analysis or interpretation of data; the writing of the report; or in the decision to submit this paper for publication. All authors have full access to the data. Tim Nawrot is a beneficiary of the European Research Council. Bram Janssen and Bianca Cox are postdoctoral fellows of the Research Foundation—Flanders (FWO 12W3218N and 12Q0517N, respectively, and supported by FWO project G082317N). We would like to thank Hilde Fleurackers for the administrative support and assistance she provided.
Authors’ contribution
Annick De Weerdt, Bram G. Janssen, Tim S. Nawrot and Philippe G. Jorens designed the study and acquired data. Walter Verbrugghe extracted data from the ICU Patient Data Management System, Bram G. Janssen developed the air pollution exposure matrixes (with input from Charlotte Vanpoucke and Wouter Lefebvre), Esmée M. Bijnens contributed to the geocoding of the residential addresses, and Omar El Salawi and Margot Jans retrieved additional data from the patient records under the supervision of Annick De Weerdt. Annick De Weerdt, Bram G. Janssen and Bianca Cox analyzed and interpreted the data. Annick De Weerdt, Bram G. Janssen, Philippe G. Jorens wrote the initial version of the manuscript. All authors were involved in constructive criticism of the manuscript and approved the final version.
Compliance with ethical standards
Conflicts of interest
We declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Annick De Weerdt and Bram G. Janssen have contributed equally to this work.
Tim S. Nawrot, Philippe G. Jorens: share senior authorship.
References
- 1.World Health Organisation . WHO Air quality guidelines for particulate matter, ozone, nitrogen dioxide and sulfur dioxide. Geneva: WHO; 2006. [PubMed] [Google Scholar]
- 2.Traboulsi H, Guerrina N, Iu M, Maysinger D, Ariya P, Baglole CJ. Inhaled pollutants: the molecular scene behind respiratory and systemic diseases associated with ultrafine particulate matter. Int J Mol Sci. 2017;18:243–262. doi: 10.3390/ijms18020243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xing YF, Xu YH, Shi MH, Lian YX. The impact of PM2.5 on the human respiratory system. J Thorac Dis. 2016;8:E69–E74. doi: 10.21037/jtd.2016.06.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Collaborators GBDCRD. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir Med. 2017;5:691–706. doi: 10.1016/S2213-2600(17)30293-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dauchet L, Hulo S, Cherot-Kornobis N, Matran R, Amouyel P, Edme JL, Giovannelli J. Short-term exposure to air pollution: associations with lung function and inflammatory markers in non-smoking, healthy adults. Environ Int. 2018;121:610–619. doi: 10.1016/j.envint.2018.09.036. [DOI] [PubMed] [Google Scholar]
- 6.Goeminne PC, Kicinski M, Vermeulen F, Fierens F, De Boeck K, Nemery B, Nawrot TS, Dupont LJ. Impact of air pollution on cystic fibrosis pulmonary exacerbations: a case-crossover analysis. Chest. 2013;143:946–954. doi: 10.1378/chest.12-1005. [DOI] [PubMed] [Google Scholar]
- 7.Ruttens D, Verleden SE, Bijnens EM, Winckelmans E, Gottlieb J, Warnecke G, Meloni F, Morosini M, Van Der Bij W, Verschuuren EA, Sommerwerck U, Weinreich G, Kamler M, Roman A, Gomez-Olles S, Berastegui C, Benden C, Holm AM, Iversen M, Schultz HH, Luijk B, Oudijk EJ, Kwakkel-van Erp JM, Jaksch P, Klepetko W, Kneidinger N, Neurohr C, Corris P, Fisher AJ, Lordan J, Meachery G, Piloni D, Vandermeulen E, Bellon H, Hoffmann B, Vienneau D, Hoek G, de Hoogh K, Nemery B, Verleden GM, Vos R, Nawrot TS, Vanaudenaerde BM. An association of particulate air pollution and traffic exposure with mortality after lung transplantation in Europe. Eur Respir J. 2017;49:1600484. doi: 10.1183/13993003.00484-2016. [DOI] [PubMed] [Google Scholar]
- 8.Chen W, Janz DR, Bastarache JA, May AK, O’Neal HR, Jr, Bernard GR, Ware LB. Prehospital aspirin use is associated with reduced risk of acute respiratory distress syndrome in critically ill patients: a propensity-adjusted analysis. Crit Care Med. 2015;43:801–807. doi: 10.1097/CCM.0000000000000789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McKown AC, McGuinn EM, Ware LB, Wang L, Janz DR, Rice TW, Semler MW. Preadmission oral corticosteroids are associated with reduced risk of acute respiratory distress syndrome in critically ill adults with sepsis. Crit Care Med. 2017;45:774–780. doi: 10.1097/CCM.0000000000002286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Muscedere J, Waters B, Varambally A, Bagshaw SM, Boyd JG, Maslove D, Sibley S, Rockwood K. The impact of frailty on intensive care unit outcomes: a systematic review and meta-analysis. Intensive Care Med. 2017;43:1105–1122. doi: 10.1007/s00134-017-4867-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moreno RP, Metnitz PG, Almeida E, Jordan B, Bauer P, Campos RA, Iapichino G, Edbrooke D, Capuzzo M, Le Gall JR, Investigators S. SAPS 3—from evaluation of the patient to evaluation of the intensive care unit. Part 2: development of a prognostic model for hospital mortality at ICU admission. Intensive Care Med. 2005;31:1345–1355. doi: 10.1007/s00134-005-2763-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zimmerman JE, Kramer AA, McNair DS, Malila FM. Acute Physiology and Chronic Health Evaluation (APACHE) IV: hospital mortality assessment for today’s critically ill patients. Crit Care Med. 2006;34:1297–1310. doi: 10.1097/01.CCM.0000215112.84523.F0. [DOI] [PubMed] [Google Scholar]
- 13.Janssen S, Dumont G, Fierens F, Mensink C. Spatial interpolation of air pollution measurements using CORINE land cover data. Atmos Environ. 2008;42:4884–4903. doi: 10.1016/j.atmosenv.2008.02.043. [DOI] [Google Scholar]
- 14.Lefebvre W, Vercauteren J, Schrooten L, Janssen S, Degraeuwe B, Maenhaut W, de Vlieger I, Vankerkom J, Cosemans G, Mensink C, Veldeman N, Deutsch F, Van Looy S, Peelaerts W, Lefebre F. Validation of the MIMOSA-AURORA-IFDM model chain for policy support: modeling concentrations of elemental carbon in Flanders. Atmos Environ. 2011;45:6705–6713. doi: 10.1016/j.atmosenv.2011.08.033. [DOI] [Google Scholar]
- 15.Gasparrini A, Armstrong B, Kenward MG. Distributed lag non-linear models. Stat Med. 2010;29:2224–2234. doi: 10.1002/sim.3940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gasparrini A. Distributed lag linear and non-linear models in R: the package dlnm. J Stat Softw. 2011;43:1–20. doi: 10.18637/jss.v043.i08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hofhuis JG, Spronk PE, van Stel HF, Schrijvers AJ, Bakker J. Quality of life before intensive care unit admission is a predictor of survival. Crit Care. 2007;11:R78. doi: 10.1186/cc5970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Simons KS, Workum JD, Slooter AJ, van den Boogaard M, van der Hoeven JG, Pickkers P. Effect of preadmission sunlight exposure on intensive care unit-acquired delirium: a multicenter study. J Crit Care. 2014;29:283–286. doi: 10.1016/j.jcrc.2013.10.027. [DOI] [PubMed] [Google Scholar]
- 19.Liu C, Chen R, Sera F, Vicedo-Cabrera AM, Guo Y, Tong S, Coelho M, Saldiva PHN, Lavigne E, Matus P, Valdes Ortega N, Osorio Garcia S, Pascal M, Stafoggia M, Scortichini M, Hashizume M, Honda Y, Hurtado-Diaz M, Cruz J, Nunes B, Teixeira JP, Kim H, Tobias A, Iniguez C, Forsberg B, Astrom C, Ragettli MS, Guo YL, Chen BY, Bell ML, Wright CY, Scovronick N, Garland RM, Milojevic A, Kysely J, Urban A, Orru H, Indermitte E, Jaakkola JJK, Ryti NRI, Katsouyanni K, Analitis A, Zanobetti A, Schwartz J, Chen J, Wu T, Cohen A, Gasparrini A, Kan H. Ambient particulate air pollution and daily mortality in 652 cities. N Engl J Med. 2019;381:705–715. doi: 10.1056/NEJMoa1817364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bein T, Karagiannidis C, Quintel M. Climate change, global warming, and intensive care. Intensive Care Med. 2019 doi: 10.1007/s00134-019-05888-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rhee J, Dominici F, Zanobetti A, Schwartz J, Wang Y, Di Q, Balmes J, Christiani DC. Impact of long-term exposures to ambient PM2.5 and ozone on ARDS risk for older adults in the United States. Chest. 2019;156:71–79. doi: 10.1016/j.chest.2019.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ware LB, Zhao Z, Koyama T, May AK, Matthay MA, Lurmann FW, Balmes JR, Calfee CS. Long-term ozone exposure increases the risk of developing the acute respiratory distress syndrome. Am J Respir Crit Care Med. 2016;193:1143–1150. doi: 10.1164/rccm.201507-1418OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rush B, McDermid RC, Celi LA, Walley KR, Russell JA, Boyd JH. Association between chronic exposure to air pollution and mortality in the acute respiratory distress syndrome. Environ Pollut. 2017;224:352–356. doi: 10.1016/j.envpol.2017.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reilly JP, Zhao Z, Shashaty MGS, Koyama T, Christie JD, Lanken PN, Wang C, Balmes JR, Matthay MA, Calfee CS, Ware LB. Low to moderate air pollutant exposure and acute respiratory distress syndrome after severe trauma. Am J Respir Crit Care Med. 2019;199:62–70. doi: 10.1164/rccm.201803-0435OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang Y, Ding Z, Xiang Q, Wang W, Huang L, Mao F. Short-term effects of ambient PM1 and PM2.5 air pollution on hospital admission for respiratory diseases: case-crossover evidence from Shenzhen, China. Int J Hyg Environ Health. 2020;224:113418. doi: 10.1016/j.ijheh.2019.11.001. [DOI] [PubMed] [Google Scholar]
- 26.Ruckerl R, Ibald-Mulli A, Koenig W, Schneider A, Woelke G, Cyrys J, Heinrich J, Marder V, Frampton M, Wichmann HE, Peters A. Air pollution and markers of inflammation and coagulation in patients with coronary heart disease. Am J Respir Crit Care Med. 2006;173:432–441. doi: 10.1164/rccm.200507-1123OC. [DOI] [PubMed] [Google Scholar]
- 27.Li W, Dorans KS, Wilker EH, Rice MB, Ljungman PL, Schwartz JD, Coull BA, Koutrakis P, Gold DR, Keaney JF, Jr, Vasan RS, Benjamin EJ, Mittleman MA. Short-term exposure to ambient air pollution and biomarkers of systemic inflammation: the framingham heart study. Arterioscler Thromb Vasc Biol. 2017;37:1793–1800. doi: 10.1161/ATVBAHA.117.309799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Michael S, Montag M, Dott W. Pro-inflammatory effects and oxidative stress in lung macrophages and epithelial cells induced by ambient particulate matter. Environ Pollut. 2013;183:19–29. doi: 10.1016/j.envpol.2013.01.026. [DOI] [PubMed] [Google Scholar]
- 29.Wright DT, Cohn LA, Li H, Fischer B, Li CM, Adler KB. Interactions of oxygen radicals with airway epithelium. Environ Health Perspect. 1994;102(Suppl 10):85–90. doi: 10.1289/ehp.94102s1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ioannidis G, Lazaridis G, Baka S, Mpoukovinas I, Karavasilis V, Lampaki S, Kioumis I, Pitsiou G, Papaiwannou A, Karavergou A, Katsikogiannis N, Sarika E, Tsakiridis K, Korantzis I, Zarogoulidis K, Zarogoulidis P. Barotrauma and pneumothorax. J Thorac Dis. 2015;7:S38–S43. doi: 10.3978/j.issn.2072-1439.2015.01.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nair GB, Niederman MS. Ventilator-associated pneumonia: present understanding and ongoing debates. Intensive Care Med. 2015;41:34–48. doi: 10.1007/s00134-014-3564-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Desai SV, Law TJ, Needham DM. Long-term complications of critical care. Crit Care Med. 2011;39:371–379. doi: 10.1097/CCM.0b013e3181fd66e5. [DOI] [PubMed] [Google Scholar]
- 33.Sakusic A, Gajic O, Singh TD, O’Horo JC, Jenkins G, Wilson GA, Petersen R, Fryer JD, Kashyap R, Rabinstein AA. Risk factors for persistent cognitive impairment after critical illness, nested case-control study. Crit Care Med. 2018;46:1977–1984. doi: 10.1097/CCM.0000000000003395. [DOI] [PubMed] [Google Scholar]
- 34.Eurostat (2019) Ageing Europe—looking at the lives of older people in the EU. Luxembourg
- 35.Lowery EM, Brubaker AL, Kuhlmann E, Kovacs EJ. The aging lung. Clin Interv Aging. 2013;8:1489–1496. doi: 10.2147/CIA.S51152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mordukhovich I, Lepeule J, Coull BA, Sparrow D, Vokonas P, Schwartz J. The effect of oxidative stress polymorphisms on the association between long-term black carbon exposure and lung function among elderly men. Thorax. 2015;70:133–137. doi: 10.1136/thoraxjnl-2014-206179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hennekens CH, Buring JE, Mayrent SL. Epidemiology in medicine. Boston: Little Brown; 1987. [Google Scholar]
- 38.Lokken RP, Wellenius GA, Coull BA, Burger MR, Schlaug G, Suh HH, Mittleman MA. Air pollution and risk of stroke: underestimation of effect due to misclassification of time of event onset. Epidemiology. 2009;20:137–142. doi: 10.1097/EDE.0b013e31818ef34a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Saenen ND, Bove H, Steuwe C, Roeffaers MBJ, Provost EB, Lefebvre W, Vanpoucke C, Ameloot M, Nawrot TS. Children’s urinary environmental carbon load. A novel marker reflecting residential ambient air pollution exposure? Am J Respir Crit Care Med. 2017;196:873–881. doi: 10.1164/rccm.201704-0797OC. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.