“We know there are things we know we know. We also know there are known unknowns; that is to say that we know there are some things we do not know. But there are also unknown unknowns—the ones we don’t know we don’t know.”
– Donald Rumsfeld, February 12, 2002
The history of informed consent is one of continuous evolution in search of a best practice, from the mid-20th century, physician-oriented “paternalistic” approach to the “reasonable patient” standard established by Canterbury v Spence in 1972.1 The process of surgical informed consent still eludes a single, universal template. It is an inherently idiosyncratic interaction during which the experience, clinical judgment, and biases of the surgeon are distilled into a focused conversation between caregiver and patient, with the goal of reaching agreement and, ultimately, permission to proceed with a recommended intervention. Ideally, the surgeon weaves data and evidence (“facts and figures”) extracted from textbooks, published scientific literature, and other sources into a narrative tailored to fit the needs of the patient including the perceived appetite of that patient for information.2 An open-ended opportunity to ask questions and to express fears and concerns is essential, and surgeons should balance expressions of reassurance and empathy with appropriate expectation-setting around the more likely outcomes including the possibility of significant complications. The informed consent discussion is particularly challenging for riskier procedures with less certain outcomes. The advantages of a patient-oriented, shared decision-making model have been articulated by Schwarze et al, who propose using best-case, worst-case scenarios as an anchoring framework.3
The assumption underlying all informed consent discussions is that we as surgeons know the risks and know the benefits with a reasonable (but far from absolute) degree of certainty, and that we can accurately weigh those in comparison to the known alternatives, including the option of no intervention. How might the process of informed consent be adapted during a time of great medical uncertainty: the current COVID-19 pandemic?
Beginning in mid-March, once the scope and severity of COVID-19 on hospitals in the United States became clear, our institution instituted several response measures, among them cancellation of all non-time sensitive elective procedures, bi-weekly department-wide virtual conference discussions regarding ethical implications and challenges we were likely to face as an institution, and bi-weekly virtual town halls with the surgical housestaff and leadership to establish open communication as a group. The department also acted quickly to develop a quantitative, rational system for scoring medically necessary, time-sensitive procedures (MeNTS), based on current resource availability, patient risk factors, degree of resource utilization presented by a proposed procedure, and the medical and surgical feasibility of postponing an intervention.4
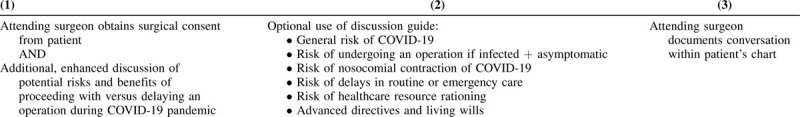
During one of the resident town halls explaining the MeNTS triage system, residents and advanced practice providers asked whether patients were specifically aware of the potential impact of the unprecedented circumstances on the recommendation to proceed with or postpone their operation. From this discussion, we instituted several policy changes regarding surgical informed consent during COVID-19: attending responsibility for obtaining consent, circulation of a conversation guide for use in discussions between attending surgeons and their patients, and standardized documentation regarding discussion of COVID-19 (Table 1).
TABLE 1.
Recommended Interventions and COVID-Enhanced Informed Consent
Like many academic medical centers, at our institution attending surgeons maintain full responsibility for the overall informed consent process but frequently delegate certain elements such as completion of paperwork to resident trainees (in the spirit of education) or to advanced practice providers (in the spirit of efficiency). However, during the COVID19 pandemic, we re-evaluated this approach, particularly for nonemergency, medically necessary, time-sensitive procedures.
The true impact of asymptomatic or presymptomatic COVID-19 disease on physiologic risks of surgery and/or anesthesia is not yet understood. We do not know the actual risk of nosocomial COVID-19 acquisition for a patient coming to the hospital during a time of otherwise mandatory social distancing, nor do we accurately know the risk of transmission of COVID-19 from unsuspectedly infected patients to members of the perioperative team. We also do not know the risks inherent in delaying otherwise medically indicated procedures (eg, cancer surgery), a problem amplified by uncertainty regarding future scheduling restrictions given the uncertain time frame of pandemic resolution and restoration of “business as usual.” It is important to recognize the significant scientific, ethical, and moral uncertainties that surround the care of patients and families during this pandemic and how they might be reflected in informed consent discussions. COVID-19 has added an additional imperative to the informed consent process: transparency about potential but unknown risks and an honest admission of how little we currently understand about the surgical outcomes of COVID-19 positive patients and patients with unknown COVID-19 status.
Given these uncertainties, we agreed that there is simply no substitute for the longitudinal relationship between an individual attending surgeon and an individual patient in coming to a shared decision to proceed with or to postpone a medically-necessary, time-sensitive procedure. We implemented a policy that an appropriately “enhanced” informed consent discussion regarding the risks of surgery during the pandemic must occur before patient arrival at the hospital on the date of surgery, and that this discussion must be conducted by the responsible surgeon (not a designee) and specifically documented in the patient's medical record.
We also developed a “script” to outline some of the unique considerations that might be included in informed consent conversations during the COVID-19 pandemic (Table 1). This script was distributed to all surgical faculty members and housestaff, and details 5 topics: the risk of operation for symptomatic and asymptomatic COVID-19 positive patients; the risk of contracting SARS-COV2 infection while in hospital; challenges in coordination of care and communication due to disruption of normal hospital operations in response to the pandemic; the possibility of future resource scarcity; and the heightened importance of living wills or advanced directives.
The first element of the COVID-19 enhanced informed consent discussion concerns the lack of information on the true risks of otherwise “routine” procedures during the pandemic. Although emerging evidence suggests increased cardiorespiratory and microembolic/thrombotic complications in symptomatic COVID-19 positive patients, there remains considerable uncertainty the extent to which the risks of undergoing an operation or general anesthesia are increased in asymptomatic or pre-symptomatic individuals.5,6 At the time of this writing, there are continued shortages of testing in the United States, and screening of preoperative patients is not practically feasible and possibly not reliable. Although there have been anecdotal reports of adverse outcomes in asymptomatic patients, we caution against extrapolation of these early reports as definitive evidence of increased risk.7 We believe patients should know this is an area of ongoing uncertainty and investigation.
Second, we advise surgeons to discuss the uncertain (but likely increased) risk of nosocomial infection with SARS-COV2. The possibility of contracting COVID-19 disease during any of the many logistical steps of undergoing an operation, from traveling to the hospital, riding in an elevator, to the actual perioperative process including postoperative care is undoubtedly increased compared to continued “sheltering in place.” Patients should understand that “social distancing” from caregivers and hospital staff is inherently imperfect despite best efforts and meticulous attention to infection control.
Third, we believe that it is important to inform patients that the COVID-19 pandemic has changed day-to-day hospital operations (dramatically so in the hardest hit centers) in ways that have the potential to significantly impact their perioperative care and experience. For example, many hospitals, including ours, have instituted visitor restriction policies that may potentially alter their ability (or their caregivers’ ability) to communicate with families and loved ones. Because of the need to cohort COVID-19-affected patients and patients under investigation for COVID-19, it is possible that postoperative care may be delivered in nursing units with personnel who are less familiar with routine surgical management.
We also suggest that surgeons discuss the possible impact of pandemic-associated healthcare resource shortages on the care of the postoperative patient. This shortage could affect the surgical patient who develops COVID-19 disease in the postoperative period (e.g., ICU bed capacity or ventilator availability). Moreover, treatment of postoperative complications may be impacted by limitations in diagnostic or interventional services including imaging, interventional radiology, or endoscopy due to COVID-19 disruptions in services. A patient who requires emergency room evaluation or readmission due to complications that develop after hospital discharge may be impacted by bed availability or other shortages of future resources later in the course of the pandemic.
Finally, we encourage surgeons to emphasize the particular importance of advanced directives and living wills for patients considering operative procedures during the pandemic. We frame the increased importance of documentation in the context not only of concerns over increased perioperative risk but also the impact of visitor restrictions that may limit the ability of surrogate medical decision-makers to interact with caregivers at the bedside. Given the uncertain perioperative risks and anecdotal reports of unexpectedly sudden (though, we hope, rare) decompensation and cardiorespiratory arrest in postoperative patients subsequently found to carry previously unsuspected COVID-19 disease, we believe that prior documentation of patient preferences is particularly important during this pandemic to allow care teams to make critical, time-sensitive medical decisions that respect the wishes and dignity of the patient.
Although the operating room environment—clean, quiet, and controlled—can feel a world away from the overwhelmed emergency rooms on the true front lines of this pandemic, we believe the implications for the informed consent process are profound.
Footnotes
The authors report no conflicts of interest.
REFERENCES
- 1.Jones JW, McCollough LB, Richman BW. A comprehensive primer of surgical informed consent. Surg Clin N Am 2007; 87:903–1918. [DOI] [PubMed] [Google Scholar]
- 2.Schwarze ML, Kehler JM, Campbell TC. Navigating high-risk procedures with more than just a street map. J Palliat Med 2013; 16:1160–1171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kruser JM, Nabozny MJ, Steffens NM, et al. Best case/worst case”: evaluation of a novel communication tool for difficult in-the-moment surgical decisions. J Am Geriatr Soc 2015; 63:1805–1811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Prachand VN, Milner R, Angelos, P, et al. Medically-necessary, time-sensitive procedures: a scoring system to ethically and efficiently manage resource scarcity and provider risk during the COVID-19 pandemic. Accepted for publication in JACS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guo T, Fan Y, Chen M, et al. Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19) [published online ahead of print, 2020 Mar 27]. JAMA Cardiol 2020; e201017.doi:10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zhou F. Du R. Fan G, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. Published online March 9, 2020. DOI: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lei S, Jiang F, Su W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection [published online ahead of print, 2020 Apr 5]. EClinicalMedicine 2020; 21:100331.doi:10.1016/j.eclinm.2020.100331. [DOI] [PMC free article] [PubMed] [Google Scholar]


