The novel COVID-19 pandemic will alter the educational experience for surgical residents across the country. It has already led to significant changes within most hospitals, including limiting the number of residents who are in-house, cancellation of elective procedures, decreased volume of acute care surgery following surgical society guidelines, and cancellation of lectures and educational conferences to adhere to social distancing recommendations. In response to these necessary changes, the American Board of Surgery has modified the training requirements of graduating chief residents to include 44 weeks of clinical time with a 10% reduction in required total cases.1 However, these changes and recommendations do not remedy the hours of surgical education content lost when residents are unable to participate in didactics, simulation, and operative cases.
Historically, surgical resident education has been overseen at an institutional level, with individual programs determining the best resources and delivery format for instruction. National curriculum and resources exist, including the Surgical Council on Resident Education (SCORE) curriculum, the ACS/APDS Surgery Resident Skills Curriculum, and various question banks. However, given the new work environment and demands placed on surgery residents during the COVID-19 pandemic, many standard instructional modalities must be altered. Daodu et al provide an insightful overview of the general implications that COVID-19 has on surgical education.2 Herein, we describe several practical strategies for resident education focused on operative preparation, educational didactics, and skills development and simulation, that transcend the geographical and temporal restrictions brought about by the COVID-19 pandemic (Fig. 1).
FIGURE 1.
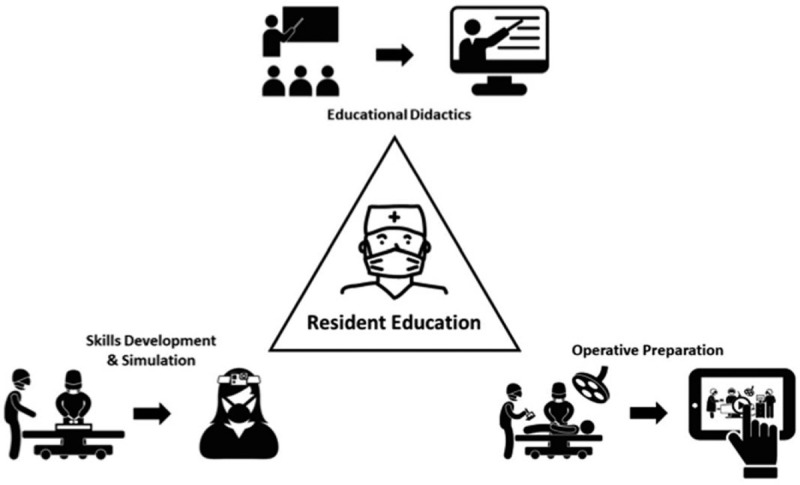
Adapting the 3 pillars of surgical resident education to the COVID-19 era. Traditional in-person lectures and didactic sessions can be transitioned to video-based and recorded teaching sessions. Simulation and skills development can adapt appropriate social distancing recommendations by utilization of home-based skills recording and remote assessment. Operative education and preparation can employ peer-reviewed video-based education modules.
OPERATIVE VIDEO-BASED EDUCATION
Before the COVID-19 pandemic, video-based education (VBE) has become an increasingly utilized, effective technique for both knowledge acquisition and operating room preparation.3 VBE is the delivery of educational content through video platforms, which stimulates dual use of a learners auditory and visual processing pathways. Previous studies in dual-coding learning theory have demonstrated when educational content is presented to both pathways concurrently, as in VBE, learners have a higher likelihood of recall.4 This platform is particularly useful for operative case preparation, especially in the setting of a pandemic where limited surgical cases are proceeding.
Although individual residency programs may choose to create their own VBE modules, this is often labor intensive, cost prohibitive, and can feel daunting. Instead, preexisting operative video libraries could be utilized to supplement resident education. Two examples of peer-reviewed libraries with VBE operative content include the Journal of Medical Insight (JOMI) and the American College of Surgeons (ACS) Online Video Library. Our institution is further answering this call, by creating an open-access, peer-reviewed video library available to all learners world-wide. This free resource, MGH SurgEdOnline, will be available in the next couple of months. These resources instruct residents on proper surgical indications, preoperative workup, and operative anatomy and techniques. With COVID-19 limitations on elective cases and acute care surgical management, the videos offer an educational alternative that can be safely watched from a learner's home or call room. Multi-institutional collaborations can alleviate the administrative burdens and costs associated with video production and increase residents’ access to educational material that transcends traditional institution silos.
VIRTUAL DIDACTICS
Virtual Lectures
Amidst the uncertainty of a pandemic, some residency programs may prefer to maintain an institution-specific educational program structure. There also may be a desire to cultivate camaraderie and connection during the changing clinical atmosphere. By offering virtual lectures through a video-based conferencing platform, such as ZOOM (Zoom Video Communications, Inc, San Jose, CA), trainees can continue to “meet” regularly and learn from local lecturers. Video-based conferencing platforms offer lecturers the ability to screen share their slides in real time, as well as a recording option for viewing outside of the scheduled didactic hours. This permits flexible learning and allows didactic lectures to transcend traditional residency schedules and clinical rotation site limitations. This technique also provides an opportunity for multi-institutional surgical education collaborations. Programs can share live or recorded virtual lecture content across multiple institutions to distribute their teaching and content expertise nationally. Surgical residencies have varying sizes and resources, and this virtual platform can facilitate the distribution of educational content to under resourced residency programs and those programs most disrupted by the COVID-19 pandemic. This software may also offer a solution to the problem of educational conference continuity when trainees are on off-site rotations beyond the COVID-19 era.
Independent Learning
A key tenet within surgical education is the theory of self-directed learning.5 In preparing for the COVID-19 crisis, many programs are currently in a waiting period between cancelling elective cases and climbing the upslope of the epidemiologic COVID-19 curve. This waiting period contains a surgeon's most valuable resource: time. Trainees can use this time to reflect on their personal learning methodologies, establish a goal, such as improved in-service examination performance or developing a deeper understanding of a certain topic, and then utilize multiple resources and principles of adult learning theory, such as spaced repetition, to achieve that goal.6 Tangible, measurable goals will allow for improved self-regulated learning. Trainees can use in-service review materials such as SCORE, TrueLearn, or ABSITE Quest (free 1-year subscription for e-learning during the COVID pandemic), textbooks, online review articles, and previously described virtual educational modules.
Additional Virtual Learning Methods
A number of additional modalities exist that provide virtual surgical educational content, including society curated content, podcasts, and social media. National societies, including American Society of Transplant Surgeons, Society of Critical Care Medicine, Society of Surgical Oncology, Society of American Gastrointestinal and Endoscopic Surgeons, and others, have created online repositories of relevant resources related to their areas of expertise that include surgical topics and COVID-19-specific resources. Podcasts, such as Behind The Knife and Audible Bleeding, provide another avenue to engage millennial learners with educational content. Although podcasts are an easy-to-access supplemental resource for this remote learning era, there is little formal evidence to support their use as a standalone teaching method.7 Thus, we also recommend offering VBE resources, which can review operative content and high-yield didactic material. One open-access resource, following the weekly SCORE curriculum, is SurgEdVidz, which is available via Twitter(R) or YouTube(R).
VIRTUAL SIMULATION
To adhere to recommendations for social distancing, many group simulation sessions have been cancelled. Along with decreased operative volumes, this could lead to skill decay during remote learning. To prevent this, Phase I of the ACS/APDS Surgery Resident Skills Curriculum can be modified to be completed independently at home. Models and instruments, such as suturing kits with felt or silicone “tissue” or fundamentals of laparoscopic surgery (FLS) box trainers, can be borrowed for technical practice. Written or verbal feedback can be provided remotely, either through faculty review of uploaded recordings or hosted ZOOM sessions in which residents focus their camera on their technical performance for faculty feedback in real-time.8
For residents on the wards, case-cancellations and virtual clinics might mean more free time in the hospital. This downtime is an opportunity for technical skill practice and residents can capitalize on near-peer learning by receiving feedback from their fellow residents—standing 6 feet away—on their technical skill performance. In-hospital residents could also schedule times to individually practice on simulation laboratorys’ fundamentals of endoscopic surgery, FLS, and robotic surgery trainers. By signing up for times in advance, residents would be able to maintain social distancing recommendations and allow for the appropriate disinfection of equipment between use to minimize COVID-19 transmission.
DESIGNING EDUCATIONAL MATERIALS
When developing educational content based on the aforementioned recommendations, it is important to utilize best practices in alignment with adult learning principles.9 Adult learners traditionally have poor retention rates following didactic lectures as attention spans wane after 15 to 20 minutes. For lectures delivered through an online platform, it is important to select clearly defined learning objectives for each session as opposed to covering vast amounts of material during the designated session. Additionally, PowerPoint slides should be created based on proven principles of multimedia design to enhance understanding and promote knowledge retention. Slides should be formatted to reduce extraneous processing, manage essential processing, and foster generative processing, aligning with Mayer's principles of multimedia design.10 One of the challenges educators face with virtual education is promoting active participation from a remote site, which is known to improve performance. Utilization of online audience response systems and small group-based learning, such as through ZOOM breakout rooms, provides a means for not only engaging learners remotely, but also providing instructors an opportunity to assess content understanding and knowledge deficits.
CONCLUSIONS
In conclusion, a multi-faceted approach to virtual surgical education during the COVID-19 pandemic is feasible and can meet the educational needs of surgical residents amidst the current constraints. The unique hospital setting brought about by this pandemic provides an opportunity to develop novel education strategies and utilize existing platforms in a way that transcends geospatial and temporal limitations. These flexible recommendations allow surgical residency programs the opportunity to maintain a rigorous educational experience despite the limitations imposed by COVID-19. As our surgical field unites to face this crisis, we are presented with a golden opportunity to embrace systemic change by developing and delivering collaborative educational content, forever leaving behind the limitations imposed by institutional silos.
Footnotes
TMC, KMJ, NMS, and DJC, contributed equally to this study.
REFERENCES
- 1. Modifications to Training Requirements—COVID-19 Update. American Board of Surgery. March 26 2020. Accessed March 31, 2020. [Google Scholar]
- 2.Daodu O, Panda N, Lopushinsky S, et al. COVID-19—considerations and implications for surgical learners. Ann Surg 2020. [DOI] [PubMed] [Google Scholar]
- 3.Ahmet A, Gamze K, Rustem M, et al. Is video-based education an effective method in surgical education? A systematic review. J Surg Educ 2018; 75:1150–1158. [DOI] [PubMed] [Google Scholar]
- 4.Ruiz GJ, Mintzer JM, Leipzig MR. The impact of E-learning in medical education. Acad Med 2006; 81:207–212. [DOI] [PubMed] [Google Scholar]
- 5.Artino AR, Jr, Brydges R, Gruppen LD. Cleland J, Durning SJ. Self-regulated learning in healthcare profession education: theoretical perspectives and research methods. Researching Medical Education. West Sussex, UK: The Association for the Study of Medical Education; 2015. 155–166. [Google Scholar]
- 6. Knowles MS. The modern practice of adult education: from pedagogy to andragogy. Rev. and updated. ed. New York: Cambridge, The Adult Education Company, 1980. [Google Scholar]
- 7.Cho D, Cosimini M, Espinoza J. Podcasting in medical education: a review of the literature. Korean J Med Educ 2017; 29:229–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McKinley SK, Hashimoto DA, Mansur A, et al. Feasibility and perceived usefulness of using head-mounted cameras for resident video portfolios. J Surg Res 2019; 239:233–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hopkins L, Hampton BS, Abbott JF, et al. To the point: medical education, technology, and the millennial learner. Am J Obstet Gynecol 2018; 218:188–192. [DOI] [PubMed] [Google Scholar]
- 10.Mayer R. Applying the science of learning: evidence-based principles for the design of multimedia instruction. Am Psychol 2008; 63:760–769. [DOI] [PubMed] [Google Scholar]


