Abstract:
With the onset of the COVID-19 pandemic, the shifting of clinical care to telemedicine visits has been hastened. Because of current limitations in resources, many elective surgeons have been forced to venture into utilizing telemedicine, in which the standards for orthopaedic examinations have not previously been fully developed. We report our experience with protocols and methods to standardize these visits to maximize the benefit and efficiency of the virtual orthopaedic examination. At the time of scheduling, patients are asked to prepare for their virtual visit and are given a checklist. In addition to confirming audiovisual capabilities prior to the visit, patients are given specific instructions on camera positioning, body positioning, setting, and attire to improve the efficiency of the visit. During the examination, digital tools can be utilized as needed. In the setting of outpatient injury evaluations, a systematic virtual examination can aid in triaging and managing common musculoskeletal conditions. With the rapid incorporation of telehealth visits, as well as the unknown future with regard to the pandemic, the utilization and capabilities of telemedicine will continue to expand. Future directions include the development of validated, modified examination techniques and new technology that will allow for improved interactive physical examinations, as we rapidly move forward into the realm of telemedicine due to unexpected necessity.
With the onset of the COVID-19 pandemic, the process of shifting clinical care to telemedicine visits has been hastened1. Orthopaedic care has been limited in many practice settings primarily to urgent or emergency visits and surgical procedures2. Many elective surgeons have been forced to venture into finding new applications for telemedicine visits that have not previously been fully developed.
Although a virtual orthopaedic examination may lack the vital elements of palpation and dynamic testing, the current situation necessitates that we utilize available resources to optimize the quality and outcome of a patient’s virtual visit. We report our observations based on our current implementation of telemedicine and discuss our experience with tools and protocols for an efficient and successful virtual visit, focusing primarily on ways to obtain the essential elements of an orthopaedic examination for conditions commonly seen in sports medicine practices.
Virtual Visit Protocols
Prior to the visit, scheduling includes consent for a virtual visit with an explanation of the visit and associated payments. New-patient paperwork is sent securely to the patient and is returned through our electronic medical records patient portal.
New patients in our practice undergo radiographic imaging based on predetermined protocols prior to their visit. If performed in a facility outside of our access network, the patients are asked to obtain and send copies of their radiographs or other images to be uploaded and reviewed at the time of the visit.
Setting up for an optimal visit includes preparation by the patient. When scheduling the virtual appointment, patients can be sent a virtual visit checklist and are encouraged to confirm a number of items prior to the virtual orthopaedic examination. Patients are instructed to connect to a testing website to confirm their camera and microphone settings prior to the virtual encounter. Guidelines on proper positioning of the camera, location and lighting, and clothing to allow for appropriate visibility and examination of the affected body part can help to prepare for the visit. The specific details of such a protocol are listed in Table I. Prepared photographs or videos demonstrating examination maneuvers can be sent to the patient before the visit. As many musculoskeletal conditions require surgeons to rely on examination findings to triage and manage injuries, preparing and standardizing the conditions of the virtual examination can help to optimize the quality and efficiency of the encounter.
TABLE I.
The Virtual Visit Checklist for Patients
| The visit will begin with a face-to-face discussion of your symptoms, but the physical examination requires repositioning the camera so that we can appropriately visualize your extremity to obtain an appropriate evaluation. Please ensure that you conduct your virtual visit in a location that allows for the following: |
| Steady viewing. Your camera should be still and not held by hand during the examination. If using a mobile device, please plan on securing the camera in a position that can allow for the views described below. |
| Space and positioning. For each body part being evaluated, please confirm the following: |
| Knee and hip: Place the camera at a height 2 to 3 feet (0.6 to 0.9 m) off the ground (e.g., on a chair), and stand 6 feet (1.8 m) away from the camera. This will allow visualization of your entire lower extremity in the following positions: |
| Standing |
| Sitting or lying on the floor or couch with your side to the camera, with legs fully extended |
| Sitting in a chair with your front or side facing the camera. (Please have a chair or couch available for this part of the examination.) |
| Shoulder and elbow: Place the camera at a height 4 to 5 feet (1.2 to 1.5 m) off the ground (e.g., on a table or counter), and stand 6 feet (1.8 m) away from the camera. Ensure that there are sufficient space and visibility to extend your arms in all directions. |
| Lighting. Because this is a virtual examination, being able to see the details of your extremity is important. Please ensure that there is appropriate lighting in the examination positions described above (e.g., add a lamp, close curtains). Avoid having the camera face a window, as it can cause excessive backlighting. |
| Clothing. Please wear clothing that allows for proper evaluation of the affected joint: |
| Knee and hip: Please wear shorts, and not long pants that are rolled up past the knee. Remove shoes and socks. |
| Shoulder: During the examination, men will be asked to remove their shirts. Women should wear a tank top that allows for visualization of the shoulders from the front, and shoulder blades from the back. |
| Elbow: Please wear short or no sleeves, not long sleeves that are rolled past the elbow. |
| Privacy. Find a quiet space where background noise is minimized and you can speak privately. |
| It can be helpful to have a trusted assistant available during your visit to help with camera positioning. |
Virtual Examination
Knee
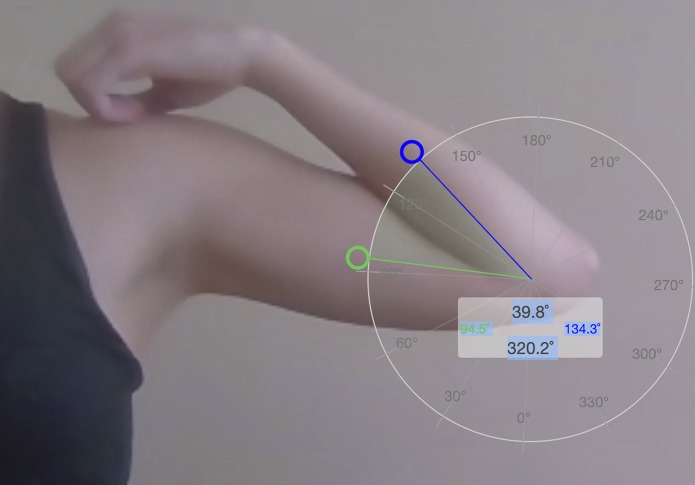
The examination begins with observation of the patient’s gait. The knee is observed for changes in overlying skin, presence of visible effusion, or erythema. The presence of muscle atrophy or symmetry is noted, and the quality of quadriceps contraction is observed. Deficiency in range of motion can be an important indication for further imaging or treatment. Range of motion is assessed in the standing or sitting position. Measurements can be obtained using a web-based goniometer, which, in our case, was used as a browser extension (Protractor; Ben Burlingham3) that is compatible with most applications (including Zoom, InTouch Health, and Doxy.me) when launched through the Chrome browser (Google). Hyperextension is best assessed by viewing the leg from the side with the patient in the standing position and having the patient push the knee posteriorly while maintaining the foot planted (Fig. 1). Flexion is assessed by having the patient pull the heel toward the body in the sitting position.
Fig. 1.
During the virtual examination, hyperextension of the knee is assessed by having the patient stand on the affected leg while pushing the knee posteriorly. A virtual goniometer can be utilized on most web-based platforms; in this case, it indicates hyperextension of 2.2°.
The patient can be asked to point to the maximum area of pain on the knee. Although reports on its utility are mixed, the Thessaly test, in which the patient stands on the affected leg bent at 20° while rotating the body internally and externally, can be performed to screen for meniscal pathology. A positive finding occurs with pain and mechanical sensations over the side of the affected meniscus4,5. The calves and the distal aspects of the extremities are assessed for swelling, varicosities, and color changes. Strength testing against gravity can be performed for all muscle groups. Inability to actively extend the knee or the presence of an extensor lag indicate the potential disruption of the extensor mechanism and may require further imaging. Limitations in the examination can be supplemented with advanced imaging as indicated on the basis of the history, presence of effusion, loss of motion, or other findings.
In atraumatic conditions, measurements of symmetry or alignment using on-screen assessment tools are used to identify contributing factors. Modifiable factors can be addressed with tailored rehabilitation protocols. Standing alignment and the quadriceps (Q) angle are measured using a web-based goniometer. Single-leg stance and squat are assessed from the frontal view as a measure of quadriceps, hip, and core function. Digital lines can be added to evaluate for pelvic obliquity, and side-to-side comparisons of pixel measurements can serve as a substitute for leg-length or circumference measurements. Observation of the J sign in a sitting position facing the camera can be helpful in the evaluation of patellar instability. Having the patient lie supine and perform a straight-leg raise or hip flexion can assess for hamstring tightness.
Hip
Many examination methods described above are applicable to the hip. The examination of the hip additionally includes the evaluation of the leg length, range of motion, and location of pain. For leg length, a virtual ruler can be used to make side-to-side comparisons of the measurements of the distance from the anterior superior iliac spine (ASIS) to the floor. Patients can be asked to place a finger on the ASIS to assist with finding this landmark for measurement.
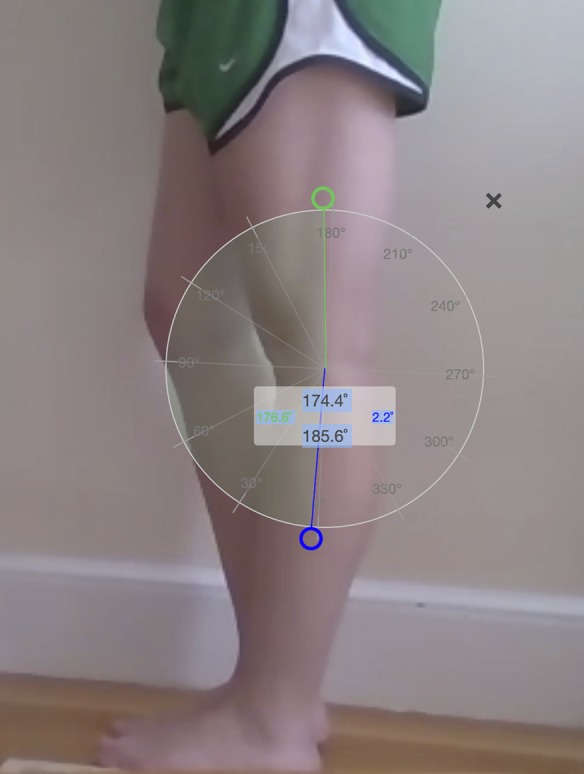
To measure hip flexion, the patient is asked to lie back with one side to the camera and to pull the knee to the chest. The measurements of internal and external rotation are obtained by having the patient sit in a chair facing the camera and rotating the hip with the knee bent at 90° (Fig. 2). External rotation can be assessed by asking the patient to initiate crossing the legs or placing them in a figure-of-4 position. Localization of pain and tenderness is assessed by asking the patient to point to this area and can include the C sign.
Fig. 2.
External rotation of the hip can be measured by having the patient sit in a chair facing the camera and rotating the hip with the knee bent at 90°.
In atraumatic cases, flexion, adduction, and internal rotation (FADIR) and flexion, abduction, and external rotation (FABER) tests may be performed by demonstrating (or providing a visual example of) the test and having the patient mimic this motion, to help differentiate between hip and spine-related pain. Strength testing can be important to rule out spine-related symptoms and to identify muscle groups that can be targeted for rehabilitation. A straight-leg raise to test for hip strength and pain is performed. The evaluation of abduction strength in the side-lying position (gluteus medius, L5) can be assessed. Having the patient perform toe-walking can demonstrate strength in L5/S1 and having the patient perform heel-walking can demonstrate strength in L4. Hip extension strength (gluteals, L5/S1) can be assessed by having the patient arise from a chair without using the arms to assist (Fig. 3).
Fig. 3.

Hip extension strength can be assessed by having the patient sit back in a chair and arise without using the arms to assist.
Shoulder
The evaluation begins with assessment of cervical range of motion. The shoulder is inspected anteriorly and posteriorly for overlying skin changes, scars, erythema or ecchymosis, and atrophy. The patient is asked to point with 1 finger to the area of maximal discomfort. For palpation, the patient can be directed to find the sternal notch and then walk the fingers to the sternoclavicular joint, across the clavicle, to the acromioclavicular joint. The bicipital groove faces forward with the arm in 10° of external rotation and can often be localized and palpated by a cooperative patient. Tenderness in each of these areas is noted.
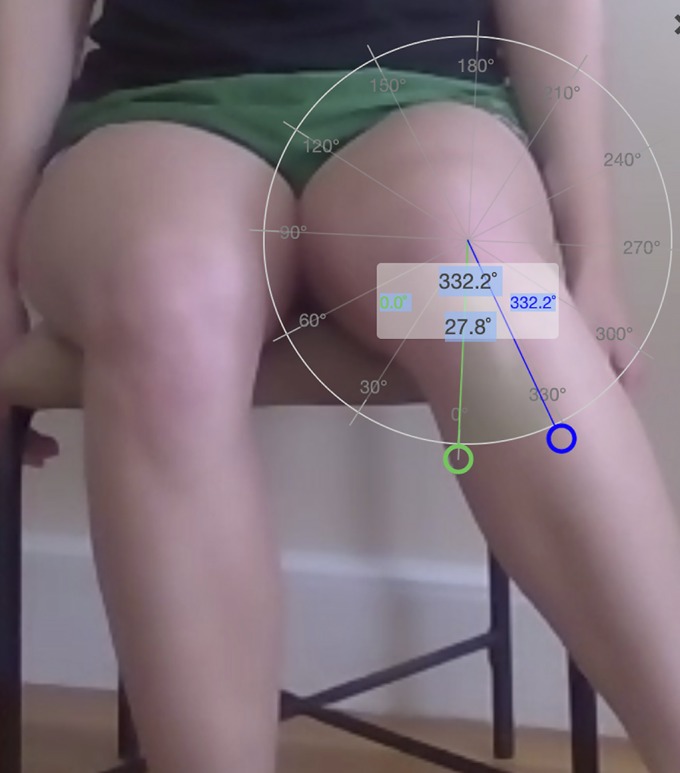
Range of motion is best assessed by evaluating for symmetry, and a virtual goniometer can be used throughout the examination as needed. Active abduction is performed with the patient facing the camera. With the arms at the waist, external rotation is assessed. Forward flexion is assessed by having the patient turn 90° to the side (Fig. 4). In the same position, the arms are abducted to 90°, and external and internal rotation are assessed in the limb closest to the camera. Internal rotation is additionally viewed with the patient facing away from the camera. Instruction using visual demonstration and mirroring can be helpful in this setting.
Fig. 4.
An internet-based goniometer can be used to assess forward flexion by measuring the angle between the midaxillary line and a line along the axis of the humeral shaft.
Strength testing in the upper extremity can be performed against gravity and with the addition of common household items of known weights (Table II). The lift-off test against gravity is viewed from the side. The inability to abduct the arm in pronation while grasping a 0.5-kg (1-lb) item may indicate a need for further imaging to assess for a large supraspinatus tear. A similar assessment can be performed in the side-lying position to test for weakness in external rotation. Evaluations of the distal aspect of the extremity, including anterior and posterior interosseous and ulnar nerve function and inspection for swelling or skin changes, are performed to complete the assessment for an acute injury.
TABLE II.
Approximate Weights of Household Items That Can Be Used During Strength or Provocative Testing of the Upper Extremity
| Item | Approximate Weight* |
| Handheld plastic stapler | 0.2 (0.5) |
| Bottle of water (450 mL or 16 oz); empty wine bottle (750 mL) | 0.5 (1) |
| Quart of milk (950 mL); 1-L bottle of soda | 1 (2) |
| Half-gallon of milk (1.9 L); 2-L soda bottle (full); unopened bottle of wine (750 mL) | 2 (4 to 5) |
| Gallon of milk (3.8 L) | 4 (8) |
The values are given in kilograms, with pounds in parentheses.
In atraumatic cases, scapular motion is assessed by having the patient face away from the camera during active abduction and forward flexion. A wall push-up can be performed while observing for scapular symmetry and strength along with an evaluation for scapular winging.
Although provocative testing can be limited in this setting, some tests requiring manual resistance can be simulated by having the patient grasp an object of a known size and weight for the empty can test, the Speed test, and the O’Brien test.
Elbow
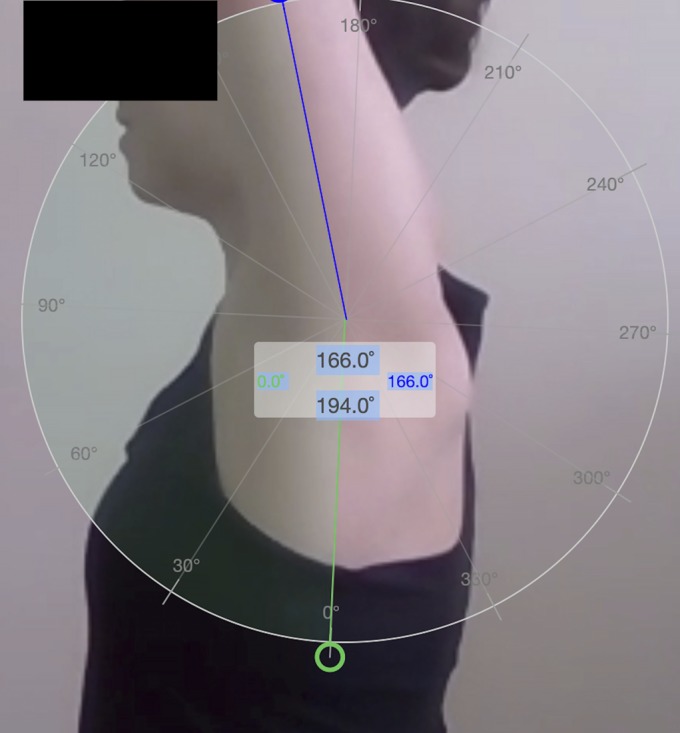
The virtual examination of the elbow begins with visual inspection. The presence of skin changes, effusion, erythema, or ecchymosis is noted. The patient is asked to point to the area of maximal pain. Flexion and extension of the elbow are observed with the patient facing the camera and abducting the arm to 90°, with the palms facing upward6 (Fig. 5). A virtual goniometer may be used to measure the range of motion. Active wrist flexion and extension can be viewed and quantified from this perspective.
Fig. 5.
Range of motion of the elbow is assessed from the front, with the arm abducted to 90°.
Supination and pronation are assessed by having the patient facing the camera, with the arms at the sides and the elbows bent to 90°. Abduction and extension of the fingers during assessment of supination and pronation can aid in visualization and in measurements if a goniometer is utilized (Fig. 6).
Fig. 6.

Pronation is assessed by having the patient facing the camera, with the arms at the sides and elbows bent to 90°.
Strength testing can be performed against gravity and while holding objects of known weight during wrist and elbow flexion and extension. In acute injuries with concerns for distal biceps injury, the muscle contour is assessed for asymmetry, both at rest and while the patient is flexing the biceps or holding weighted items with both arms at the waist. Similarly, the evaluation of triceps injuries involves inspection of the muscle contour for swelling or asymmetry posteriorly. Positive findings should be an indication for further imaging to confirm the diagnosis and to determine acuity of the need for treatment.
To assess for posterolateral stability, the chair push-up test can be performed by having the patient turn 90° with the injured elbow closest to the camera and push off from a chair, with the forearm in supination (Fig. 7)7. Pain or apprehension during this maneuver may suggest possible posterolateral rotatory instability and may be an indication for advanced imaging if in accordance with the patient’s described history and symptoms.
Fig. 7.

The chair push-up test can be used for the evaluation of posterolateral rotatory instability. The patient is asked to turn 90° with the injured elbow closest to the camera and to then push off from a chair with the fingers pointed away from the body. Pain or apprehension during this maneuver may indicate possible posterolateral rotatory instability.
In atraumatic cases, localization of the maximal point of pain during provocative testing can be performed with repeated wrist extension and supination while holding a weighted object to assess for lateral epicondylitis. Similarly, repeated wrist flexion and pronation while holding a weighted object can be helpful in assessing for medial epicondylitis.
Completing the Virtual Assessment
There are inherent limitations of the orthopaedic virtual visit. Provocative testing, discrete palpation, and strength or stability testing can be limited; increased utilization of magnetic resonance imaging (MRI) in this setting can be helpful in the diagnostic process. Despite this, we have found that obtaining a thorough history and a basic, standardized assessment of the joint can increase the diagnostic value and quality of a virtual visit.
After the assessment, the use of the screen-sharing function that is presumably available on all interactive telehealth platforms allows for shared visualization and explanation of imaging studies. Without the use of anatomic models, prepared pictures can be used as adjunct visual aids during the discussion with the patient.
Telemedicine in Orthopaedic Surgery
Prior to the ongoing pandemic, authors have explored the role of telemedicine in orthopaedic consultations, with good results8-10. A randomized controlled trial based in Norway compared video consultations with standard orthopaedic visits and included new referrals to the outpatient clinic, postoperative patients, and patients undergoing follow-up for traumatic or chronic orthopaedic disorders10. The authors reported that it was safe to offer video-assisted consultations for select orthopaedic patients, with no adverse events reported as a result of this and no difference in patient-reported satisfaction and health9. In that study, a trained nurse was present with the patient, and the physician had remote control of the camera. Furthermore, patients who were likely to need advanced physical examinations, such as those with athletic knee and shoulder injuries, were excluded from the study. This was in contrast to the patient population reported in our current experience.
Other authors have reported success in treating patients with orthopaedic trauma, particularly that related to fracture management11,12. A systematic review of telemedicine-based rehabilitation has shown strong evidence in favor of this method for postoperative hip and knee arthroplasty visits13. To our knowledge, the use of telemedicine in the care of patients with sports medicine diagnoses has not previously been addressed.
The utility of virtual goniometers during telemedicine visits have been validated in prior studies. Russell et al.14 reported on the use of an internet-based goniometer to assess knee range of motion and found, in a comparison of 540 knee positions, that face-to-face measurements and internet measurements showed high intrarater and interrater reliability. The authors measured the angle from a laterally based view, using a line along the axis of the femur and a line drawn from the fibular head to the lateral malleolus. They concluded that the internet-based goniometer was a valid tool for measuring knee extension and flexion angles. Dent et al.6 reported on 52 elbows that underwent range-of-motion measurements in person, through teleconference, and with still photography. The authors reported high agreement between teleconference-based goniometry and in-person measurements, based on the evaluation of healthy control patients. Other authors have shown equivalent accuracy and greater precision in joint measurements with digital goniometry when compared with visual estimation in shoulder abduction, shoulder internal rotation, elbow flexion, hip abduction, and knee extension15,16.
In addition to range-of-motion measurements, assessments of function have been found to be adequately performed during virtual evaluations of the shoulder. With regard to the assessment of shoulder function, Goldstein et al.17 compared Constant scores between conventional face-to-face examinations and video examinations. In their study, the video evaluations were performed on smartphones. The authors reported that the mean Constant score for the video assessment was 0.53 point lower than that for the in-person assessment and concluded that video evaluations resulted in a reliable estimate of shoulder function.
Challenges have been reported with telemedicine visits, particularly with implementation within the elderly population18; however, these patients may also benefit the most from televisit capabilities because of their limited mobility and higher risk of morbidity during the current pandemic. In this population, the use of mobile radiology services in Norway has been shown to increase access to imaging and may be a future area of consideration for such patients in the United States19. The use of telemedicine for orthopaedic visits in Norway has been shown to be cost-effective, particularly when considering travel time for patients. The authors reported that this conclusion held as long as >151 visits were performed per year8. Other reported benefits and roles for continued telehealth utilization past the COVID-19 pandemic include improved access12,20, improved communication with patients undergoing surgical treatment21, and improved reporting of functional outcomes in research settings22.
Future Directions
With the recent and rapid incorporation of telemedicine visits, as well as the unknown future with regard to the pandemic, the capability of telehealth will likely continue to expand. The standardization of virtual examinations and the validation of measurements are the next steps in improving the utility of telehealth in the field of orthopaedic surgery. Future directions include technological advancements to potentially incorporate motion-capture imaging and remote dynamic testing23,24. The development of validated, modified examination techniques that will allow for improved and interactive physical examinations is likely the next wave of progress as we move into this new realm. Research with regard to the reliability of the various testing maneuvers for each joint will be important in the future.
Summary
The advent and utilization of telemedicine have been hastened because of the COVID-19 pandemic, leading to a sudden shift toward the use of virtual orthopaedic assessments as a necessary measure. We provide guidelines, based on our experience, for orthopaedic surgeons and providers to optimize the quality and efficiency of the virtual visit, particularly as it relates to the role of the orthopaedic physical examination for common musculoskeletal conditions.
Footnotes
Investigation performed at Massachusetts General Hospital, Boston, Massachusetts
Disclosure: The authors indicated that no external funding was received for any aspect of this work. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJS/F868).
References
- 1.U.S. Centers for Medicare & Medicaid Services. Telehealth services. 2020. ,mbMarch Accessed 2020 Apr 14 https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/TelehealthSrvcsfctsht.pdf
- 2.U.S. Centers for Medicare & Medicaid Services. CMS adult elective surgery and procedures recommendations: limit all non-essential planned surgeries and procedures, including dental, until further notice. Accessed 2020. April 14 https://www.cms.gov/files/document/covid-elective-surgery-recommendations.pdf
- 3.Burlingham B. Protractor. 2020. January 23 Accessed 2020 Apr 14. https://chrome.google.com/webstore/detail/protractor/kpjldaeddnfokhmgdlmpdlecmobaonnj [Google Scholar]
- 4.Karachalios T, Hantes M, Zibis AH, Zachos V, Karantanas AH, Malizos KN. Diagnostic accuracy of a new clinical test (the Thessaly test) for early detection of meniscal tears. J Bone Joint Surg Am. 2005. May;87(5):955-62. [DOI] [PubMed] [Google Scholar]
- 5.Hegedus EJ. Thessaly test is no more accurate than standard clinical tests for meniscal tears. Evid Based Med. 2016. February;21(1):39 Epub 2015 Nov 4. [DOI] [PubMed] [Google Scholar]
- 6.Dent PA, Jr, Wilke B, Terkonda S, Luther I, Shi GG. Validation of teleconference-based goniometry for measuring elbow joint range of motion. Cureus. 2020. February 9;12(2):e6925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Regan W, Lapner PC. Prospective evaluation of two diagnostic apprehension signs for posterolateral instability of the elbow. J Shoulder Elbow Surg. 2006. May-Jun;15(3):344-6. [DOI] [PubMed] [Google Scholar]
- 8.Buvik A, Bergmo TS, Bugge E, Smaabrekke A, Wilsgaard T, Olsen JA. Cost-effectiveness of telemedicine in remote orthopedic consultations: randomized controlled trial. J Med Internet Res. 2019. February 19;21(2):e11330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buvik A, Bugge E, Knutsen G, Småbrekke A, Wilsgaard T. Patient reported outcomes with remote orthopaedic consultations by telemedicine: a randomised controlled trial. J Telemed Telecare. 2019. September;25(8):451-9. Epub 2018 Jul 4. [DOI] [PubMed] [Google Scholar]
- 10.Buvik A, Bugge E, Knutsen G, Småbrekke A, Wilsgaard T. Quality of care for remote orthopaedic consultations using telemedicine: a randomised controlled trial. BMC Health Serv Res. 2016. September 8;16(1):483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Prada C, Izquierdo N, Traipe R, Figueroa C. Results of a new telemedicine strategy in traumatology and orthopedics. Telemed J E Health. 2019. July 9 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 12.Blank E, Lappan C, Belmont PJ, Jr, Machen MS, Ficke J, Pope R, Owens BD. Early analysis of the United States Army’s telemedicine orthopaedic consultation program. J Surg Orthop Adv. 2011. Spring;20(1):50-5. [PubMed] [Google Scholar]
- 13.Pastora-Bernal JM, Martín-Valero R, Barón-López FJ, Estebanez-Pérez MJ. Evidence of benefit of telerehabitation after orthopedic surgery: a systematic review. J Med Internet Res. 2017. April 28;19(4):e142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Russell TG, Jull GA, Wootton R. Can the internet be used as a medium to evaluate knee angle? Man Ther. 2003. November;8(4):242-6. [DOI] [PubMed] [Google Scholar]
- 15.Russo RR, Burn MB, Ismaily SK, Gerrie BJ, Han S, Alexander J, Lenherr C, Noble PC, Harris JD, McCulloch PC. Is digital photography an accurate and precise method for measuring range of motion of the hip and knee? J Exp Orthop. 2017. September 7;4(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Russo RR, Burn MB, Ismaily SK, Gerrie BJ, Han S, Alexander J, Lenherr C, Noble PC, Harris JD, McCulloch PC. Is digital photography an accurate and precise method for measuring range of motion of the shoulder and elbow? J Orthop Sci. 2018. March;23(2):310-5. Epub 2017 Dec 20. [DOI] [PubMed] [Google Scholar]
- 17.Goldstein Y, Schermann H, Dolkart O, Kazum E, Rabin A, Maman E, Chechik O. Video examination via the smartphone: a reliable tool for shoulder function assessment using the Constant score. J Orthop Sci. 2019. September;24(5):812-6. Epub 2019 Jan 25. [DOI] [PubMed] [Google Scholar]
- 18.McLiesh P. Telehealth in contemporary orthopaedic nursing. Int J Orthop Trauma Nurs. 2019. May;33:1-3. Epub 2019 Mar 13. [DOI] [PubMed] [Google Scholar]
- 19.Kjelle E, Lysdahl KB, Olerud HM. Impact of mobile radiography services in nursing homes on the utilisation of diagnostic imaging procedures. BMC Health Serv Res. 2019. June 26;19(1):428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Seto E, Smith D, Jacques M, Morita PP. Opportunities and challenges of telehealth in remote communities: case study of the Yukon Telehealth System. JMIR Med Inform. 2019. November 1;7(4):e11353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.De La Cruz Monroy MFI, Mosahebi A. The use of smartphone applications (apps) for enhancing communication with surgical patients: a systematic review of the literature. Surg Innov. 2019. April;26(2):244-59. Epub 2019 Jan 2. [DOI] [PubMed] [Google Scholar]
- 22.Good DW, Lui DF, Leonard M, Morris S, McElwain JP. Skype: a tool for functional assessment in orthopaedic research. J Telemed Telecare. 2012. March;18(2):94-8. Epub 2012 Jan 13. [DOI] [PubMed] [Google Scholar]
- 23.Cai L, Ma Y, Xiong S, Zhang Y. Validity and reliability of upper limb functional assessment using the Microsoft Kinect V2 Sensor. Appl Bionics Biomech. 2019. February 11;2019:7175240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wochatz M, Tilgner N, Mueller S, Rabe S, Eichler S, John M, Völler H, Mayer F. Reliability and validity of the Kinect V2 for the assessment of lower extremity rehabilitation exercises. Gait Posture. 2019. May;70:330-5. Epub 2019 Mar 26. [DOI] [PubMed] [Google Scholar]