Coronavirus disease 2019 (COVID-19) due to infection with severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) remains a global pandemic. Although COVID-19 was initially thought to be a disease largely characterized by respiratory disease and a fever, subsequent data have highlighted this clinical scope was too narrow. Indeed, the majority of individuals infected with SARS-CoV-2 may be asymptomatic, although others present with a variety of symptoms including cardiac, neurologic, and hypercoagulable complications.1, 2, 3, 4 We recently have termed the broad spectrum of cardiovascular and thromboembolic complications the acute COVID-19 cardiovascular syndrome (ACovCS).3 These cardiac complications include acute coronary syndrome with obstructive coronary artery disease, acute myocardial injury with nonobstructive coronary artery disease, heart failure, cardiogenic shock, myocarditis, arrythmias, pericardial effusions, and cardiac tamponade, as well as thromboembolic complications such as stroke, pulmonary embolism, and deep vein thrombosis.3
Recently, cardiac presentations of COVID-19 in the absence of significant pulmonary involvement have been described in case reports or case series (Table 1 ). However, to our knowledge, a framework describing the variable presentations of cardiac involvement in COVID-19 within the broader spectrum of symptomatic SARS-CoV-2 infection has not been proposed previously. We attempt to fill this void by highlighting 2 patterns of cardiac presentations: the more common phenotype with cardiac involvement superimposed on the typical pulmonary predominate symptoms (“mixed pulmonary and cardiac”), or as an isolated or predominate cardiac presentation (“predominate cardiac”). Unquestionably, there are patients in whom the distinctions between these patterns is blurred (eg, a patient with an ST-elevation myocardial infarction who has mild pulmonary infiltrates); however, we believe this classification provides a useful framework for future research and therapeutic endeavors.
Table 1.
Cardiac Predominate Presentations in COVID-19
| Phenotype | Reference | Finding |
|---|---|---|
| Myocarditis | Inciardi et al, JAMA Cardiology, 202012 | Case report: 53-year-old with acute myopericarditis and normal chest radiograph. |
| Myocarditis | Fried et al, Circulation, 202013 | Case report: 64-year-old with fulminant myocarditis and normal chest radiograph. |
| Myocarditis | Paul et al, EHJ Cardiovascular Imaging, 202014 | Case report: 35-year-old with acute myocarditis and a normal chest CT scan. |
| STEMI | Bangalore et al, NEJM, 20206 | Case series: 17% of STEMI cases (n = 3) with normal chest radiograph. |
| STEMI | Stefanini et al, Circulation, 202015 | Case series: first clinical manifestation of COVID-19 was STEMI (n = 24/28, 86%). |
| Stress cardiomyopathy | Meyer et al, EHJ, 202016 | Case report: 83-year-old with Takotsubo cardiomyopathy and normal chest radiograph. |
| Tamponade | Dabbagh et al, JACC CR, 202017 | Case report: 67-year-old with tamponade and chest radiograph without infiltrate. |
| Tamponade | Hua et al, EHJ, 202018 | Case report: 47-year-old with tamponade and mild pulmonary congestion on chest radiograph. |
CT, computed tomography; COVID-19, coronavirus disease-2019; EHJ, European Heart Journal; JACC CR; Journal of the American College of Cardiology Case Reports; JAMA, Journal of the American Medical Association; NEJM, New England Journal of Medicine; STEMI, ST-elevation myocardial infarction.
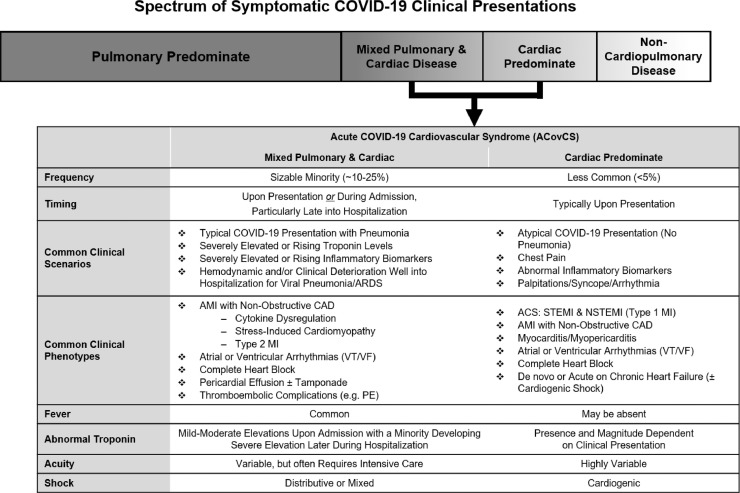
A contrast of the characteristics of the mixed pulmonary and cardiac versus predominate cardiac patterns is shown in Fig. 1 . First, the prevalence of mixed cardiopulmonary disease as assessed by elevated cardiac troponin levels, is variable, but occurs in 10%–25% of patients hospitalized with COVID-19.3 , 4 In contrast, the cardiac predominate phenotype appears to be much less common, likely well <5% of patients hospitalized with COVID-19.5 , 6 Fever is a common manifestation of COVID-19 when there is typical pulmonary involvement, but may be absent in the predominate cardiac phenotype. Both presentations can have elevated inflammatory and cardiac biomarkers (eg, cardiac troponin and natriuretic peptides); however, in the mixed presentations, the troponin is less likely to be severely elevated upon admission, although it can increase considerably during the hospitalization. In contrast, the troponin level with an isolated cardiac presentation can be absent or markedly increased, depending on the presentation (eg, when presenting with a ST-elevation myocardial infarction or myocarditis). ACovCS with cardiac-predominate disease may be more apparent at hospital presentation relative to mixed cardiopulmonary disease because the predominate cardiac manifestations (eg, chest pain owing to a myocardial infarction) often results in symptoms which lead patients to seek emergent care. In contrast, ACovCS superimposed on pulmonary disease is unpredictable and can occur at any time during hospital admission. Indeed, reports now suggest that this late complication can be seen in some critically ill patients even after apparent respiratory stabilization.7 Furthermore, in the minority of patients with COVID-19 who develop shock, patients with cardiac predominate disease would be anticipated to develop cardiogenic rather than distributive shock. In short, these 2 patterns of ACovCS presentation can be distinguished from each other by their associated clinical characteristics. We anticipate that future research will better characterize the differences in the disease course and outcomes between these 2 groups.
Fig. 1.
Spectrum of symptomatic coronavirus disease-2019 (COVID-19) clinical presentations. Spectrum of pulmonary, cardiac and noncardiopulmonary disease for hospitalized patients with the acute COVID-19 cardiovascular syndrome (ACovCS). Notably asymptomatic severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection may represent that greatest prevalence of infected patients; however, the majority of symptomatic patients have respiratory symptoms without cardiac involvement. Predominate cardiac syndromes in patients hospitalized with COVID-19 represent a less common clinical phenotype while patients with mixed pulmonary and cardiac disease represent a phenotypic overlap with multiorgan injury that occurs in a sizable minority of hospitalized patients. ACovCS encompasses cardiac manifestations and myocardial injury for both cardiac predominate and mixed disease. Noncardiopulmonary predominate disease represents a variety of other presentations such as altered mental status (neurologic), isolated deep vein thrombosis (hypercoagulable), diarrhea (gastrointestinal), and rash (dermatologic). ACS, acute coronary syndrome; AMI, acute myocardial injury; ARDS, acute respiratory distress syndrome; CAD, coronary artery disease; COVID-19, coronavirus disease-2019; MI, myocardial infarction; NSTEMI, non–ST-elevation myocardial infarction; PE, pulmonary embolism; STEMI, ST-elevation myocardial infarction; VF, ventricular fibrillation; VT, ventricular tachycardia.
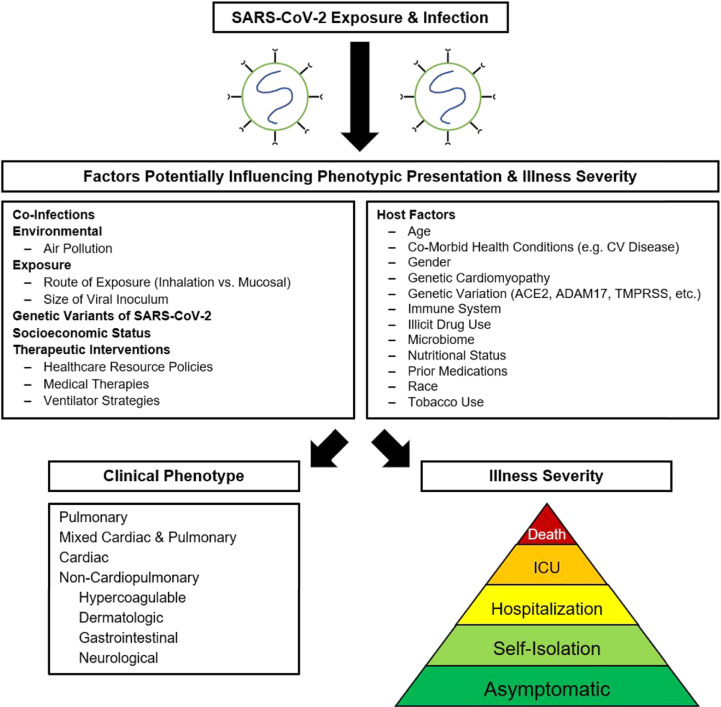
Just as there is variability in cardiac presentations of COVID-19, SARS-CoV-2 infection overall has a wide spectrum of disease penetrance with many patients displaying few to no symptoms, and an unfortunate minority developing severe life-limiting disease. The basis of such disease variability, including why the cardiac system is involved in only a minority of patients, is entirely unknown at this juncture but there are some putative risk factors to consider (Fig. 2 ). SARS-CoV-2 is the seventh coronavirus known to infect humans and strongly binds to the angiotensin-converting enzyme 2 (ACE2) receptor, which is expressed by pericytes and cardiomyocytes.8 Further analysis has determined that the receptor binding domain on the SARS-CoV-2 spike protein, the host ACE2 receptor, and host cell transmembrane serine protease 2 are all essential for host cell infection.3 , 8 In addition, the host cell ADAM metallopeptidase domain 17 participates in ACE2 receptor cleavage from the cell membrane leading to release into the circulation.9 Cleaved ACE2 has the potential to influence clotting cascades and feedback to the renin–angiotensin system, which may impact vascular, cardiac, and renal pathophysiology.4 As such, it is reasonable to speculate that genetic variations within the host—whether that be the ACE2 receptor, transmembrane serine protease, or ADAM metallopeptidase domain 17—may influence the variability of clinical presentations, the prevalence of ACovCS, and COVID-19 clinical outcomes. Whether such genetic differences contribute to the disparities in COVID-19 outcomes between populations is unknown. Finally, rare genetic mutations that lead to familial cardiomyopathy may predispose a subset of patients to developing fulminant myocarditis in the setting of a COVID-19 infection, a so-called 2-hit hypothesis. Support for this possibility comes from prior observations in children of an association of certain genetic mutations with an increased risk for developing acquired myocarditis in the setting of acute viral infections.10 Whether or not a 2-hit hypothesis contributes to the rarely described cases of biopsy-proven fulminant COVID-19 myocarditis is also unknown.
Fig. 2.
Potential factors influencing the variability of coronavirus disease-2019 (COVID-19). Factors influencing severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection penetrance and disease course remain unclear. Several factors are hypothesized to influence the clinical phenotype and illness severity of COVID-19 including the presence of a coinfection, environmental factors, host factors, host genetics, and viral factors, among others. ACE2, angiotensin-converting enzyme 2; ADAM17, ADAM metallopeptidase domain 17; CV, cardiovascular; ICU, intensive care unit; TMPRSS2, transmembrane serine protease 2.
Other factors that may influence the variable presentation of COVID-19 include mutations in the circulating SARS-CoV-2 virus, although it remains uncertain whether such observations explain the regional differences in the outcomes of COVID-19. Likewise, antecedent patient characteristics, including age, race, sex, and comorbid health conditions (particularly diabetes, chronic lung disease, and cardiovascular diseases such as hypertension, coronary artery disease, and heart failure) may impact disease severity and penetrance not only through baseline risk, but also potentially through differential ACE2 tissue expression. Additionally, the powerful influences of lower socioeconomic status and unfavorable environmental factors likely contribute to racial COVID-19 health disparities.11 Other factors that may influence disease variability in the overall population include a history of smoking, e-cigarette use, illicit drug use, the route of infection (inhaled vs direct mucosal contact), viral inoculation dose, health care delivery systems, and host immune status, among others. Urgent investigation is needed to understand the basis of this variability of disease progression, including those that predispose to cardiac involvement. We suspect that gaining such knowledge may also provide insights into the pathophysiology and progression of cardiomyopathy and heart failure that extends beyond COVID-19.
Declaration of Competing Interest
NH and MD report no relevant conflicts of interest or disclosures. JG reports consulting income from Pfizer, Inc, and Eidos Therapeutics.
Footnotes
See page 465 for disclosure information.
Dr. Mark Drazner is supported by the James M. Wooten Chair in Cardiology. Dr. Justin Grodin is supported by the Texas Health Resources Clinical Scholarship.
References
- 1.Poyiadji N., Shahin G., Noujaim D., Stone M., Patel S., Griffith B. COVID-19-associated acute hemorrhagic necrotizing encephalopathy: CT and MRI features. Radiology. 2020 doi: 10.1148/radiol.2020201187. Published online March 31, 2020. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bendavid E., Mulaney B., Sood N., Shah S., Ling E., Bromley-Dulfano R. COVID-19 antibody seroprevalence in Santa Clara County, California. medRxiv. 2020 doi: 10.1093/ije/dyab010. medRxiv. 2020:2020.04.14.20062463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hendren N.S., Drazner M.H., Bozkurt B., Cooper L.T., Jr Description and proposed management of the acute COVID-19 cardiovascular syndrome. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047349. Published online April 16, 2020. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tersalvi G., Vicenzi M., Calabretta D., Biasco L., Pedrazzini G. Elevated troponin in patients with coronavirus disease 2019: possible mechanisms. J Card Fail. 2020 doi: 10.1016/j.cardfail.2020.04.009. Published online April 18, 2020. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ruan Q., Yang K., Wang W., Jiang L., Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:846–848. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bangalore S., Sharma A., Slotwiner A., Yatskar L., Harari R., Shah B. ST-segment elevation in patients with COVID-19: a case series. N Engl J Med. 2020 doi: 10.1056/NEJMc2009020. Published online April 17, 2020. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhatraju P.K., Ghassemieh B.J., Nichols M., Kim R., Jerome K.R., Nalla A.K. Covid-19 in critically ill patients in the Seattle Region - case series. N Engl J Med. 2020 doi: 10.1056/NEJMoa2004500. Published online March 30, 2020. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Andersen K.G., Rambaut A., Lipkin W.I., Holmes E.C., Garry R.F. The proximal origin of SARS-CoV-2. Nat Med. 2020;26:450–452. doi: 10.1038/s41591-020-0820-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heurich A., Hofmann-Winkler H., Gierer S., Liepold T., Jahn O., Pohlmann S. TMPRSS2 and ADAM17 cleave ACE2 differentially and only proteolysis by TMPRSS2 augments entry driven by the severe acute respiratory syndrome coronavirus spike protein. J Virol. 2014;88:1293–1307. doi: 10.1128/JVI.02202-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Belkaya S., Kontorovich A.R., Byun M., Mulero-Navarro S., Bajolle F., Cobat A. Autosomal recessive cardiomyopathy presenting as acute myocarditis. J Am Coll Cardiol. 2017;69:1653–1665. doi: 10.1016/j.jacc.2017.01.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haynes N., Cooper L.A., Albert MA, Association of Black C At the heart of the matter: unmasking and addressing COVID-19′s toll on diverse populations. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.048126. Published online May 4, 2020. doi: [DOI] [PubMed] [Google Scholar]
- 12.Inciardi R.M., Lupi L., Zaccone G., Italia L., Raffo M., Tomasoni D. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1096. Published online March 27, 2020. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fried J.A., Ramasubbu K., Bhatt R., Topkara V.K., Clerkin K.J., Horn E. The variety of cardiovascular presentations of COVID-19. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047164. Published online April 3, 2020. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paul J.F., Charles P., Richaud C., Caussin C., Diakov C. Myocarditis revealing COVID-19 infection in a young patient. Eur Heart J Cardiovasc Imaging. 2020 doi: 10.1093/ehjci/jeaa107. Published online April 27, 2020. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stefanini G.G., Montorfano M., Trabattoni D., Andreini D., Ferrante G., Ancona M. ST-elevation myocardial infarction in patients with COVID-19: clinical and angiographic outcomes. Circulation. 2020 doi: 10.1161/CIRCULATIONAHA.120.047525. Published online April 30, 2020. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meyer P., Degrauwe S., Delden C.V., Ghadri J.R., Templin C. Typical takotsubo syndrome triggered by SARS-CoV-2 infection. Eur Heart J. 2020;41:1860. doi: 10.1093/eurheartj/ehaa306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dabbagh M.F., Aurora L., D'Souza P., Weinmann A.J., Bhargava P., Basir M.B. Cardiac tamponade secondary to COVID-19. JACC Case Rep. 2020 doi: 10.1016/j.jaccas.2020.04.009. Published online April 22, 2020. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hua A., O'Gallagher K., Sado D., Byrne J. Life-threatening cardiac tamponade complicating myo-pericarditis in COVID-19. Eur Heart J. 2020 doi: 10.1093/eurheartj/ehaa253. Published online March 30, 2020. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]