Clinical challenge
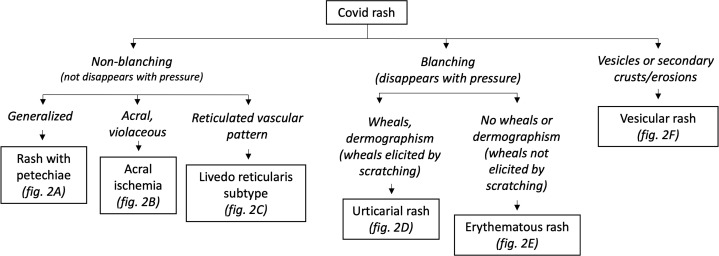
Up to 20% of patients with coronavirus disease 2019 develop cutaneous manifestations such as erythematous rash, rash with petechiae, vesicular rash, acral ischemia, livedo reticularis, and widespread urticaria.1 , 2 The appropriate classification of these manifestations, crucial for accurate scientific research, depends on physical examination and cannot be correctly assessed with teledermatology. To make classification easier, our suggestion is a simple algorithm that can be easily performed by patients, general practitioners, and intensive care unit professionals on the front lines who are confronting coronavirus disease 2019 and not used to dermatologic examination (Fig 1 ).
Fig 1.
Proposed algorithm. COVID, Coronavirus disease 2019.
Solution
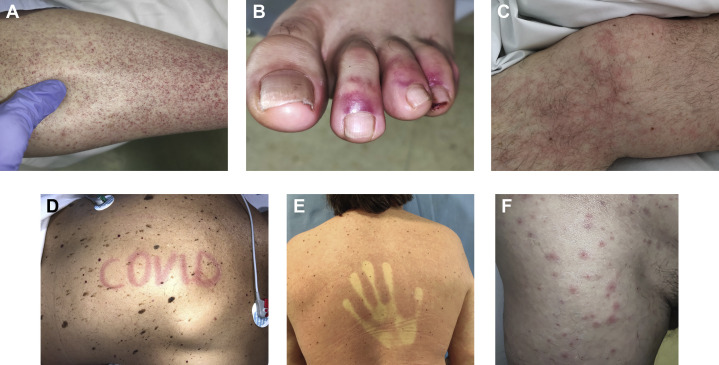
When patients with generalized exanthem from coronavirus disease 2019 are examined, the first step is to look for the presence of vesicles or secondary erosions with crusts (Fig 2 , F). If these are absent, a blanching component can be easily assessed by firmly pressing the affected area for several seconds. Nonblanching generalized rashes composed of small red macules are indicative of a rash with petechiae (Fig 2, A). An acral distribution of nonblanching violaceus lesions is indicative of acral ischemia (Fig 2, B). A reticulated vascular pattern indicates livedo reticularis subtype (Fig 2, C). For blanching rashes, the next step in our algorithm is to scratch the skin. Dermographism would manifest as linear wheals at sites of scratching and indicate a diagnosis of urticarial rash (Fig 2, D), whereas its absence indicates erythematous rash (Fig 2, E). A flashlight photograph after each step may be taken immediately afterward by the patient or medical staff so that lesions can be easily assessed by teledermatology.
Fig 2.
Examples of coronavirus disease 2019–associated rash with petechiae (A), acral ischemia (B), livedo reticularis subtype located on the lower extremities (C), urticarial rash (D), erythematous rash (E), and vesicular rash (F). Erythematous rash blanches on pressure, whereas rash with petechiae, livedo reticularis subtype, and acral ischemia does not. Urticarial rash may be associated with dermographism. Severe acute respiratory syndrome coronavirus 2 infection was confirmed in all the patients by reverse-transcriptase polymerase chain reaction assay.
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
Reprints not available from the authors.
References
- 1.Joob B., Wiwanitkit V. COVID-19 can present with a rash and be mistaken for dengue. J Am Acad Dermatol. 2020;82(5):e177. doi: 10.1016/j.jaad.2020.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatol Venereol. 2020;34(5):e212–e213. doi: 10.1111/jdv.16387. [DOI] [PubMed] [Google Scholar]