Dear Editor,
We read with great interest the article of Yang et al. about the effect of corticosteroid treatment on patients with coronavirus infection.1 In their systematic review and meta-analysis, the authors included 15 studies that reported glucocorticoid therapy in patients infected with the severe acute respiratory syndrome coronavirus (SARS-CoV; n = 11), the Middle East respiratory syndrome coronavirus (MERS-CoV; n = 2), or the severe acute respiratory syndrome caused by the novel 2019 coronavirus (SARS-CoV-2; n = 2). They conclude that patients with severe conditions were more likely to require corticosteroids and that mortality rate was higher in patients who received glucocorticoid treatment. This study, however, has several limitations that prevent any conclusion about treatment recommendations. First, there is a lack in the literature of randomized trials on this topic. Thus, most of the included studies in the meta-analysis were retrospective cohort studies with biases and weaknesses. Second, there is a great heterogeneity between included studies with differences among design, therapeutic strategies and case-mix population, and this was also confirmed by the sensitivity analysis. And third, there are only 2 cohort studies focusing on SARS-CoV-2. Finally, this meta-analysis is unable to deliver strong evidence and powered information about beneficial or harmful effect of glucocorticoids in COVID-19 patients.
To date, corticosteroids are still on debate, especially for critically ill patients with ARDS related to COVID-19.2 , 3 Several questions regarding targets such as type of pulmonary lesion and severity of disease, and the best timing for corticosteroid use remain unanswered. Based on recent interim WHO guidance,4 some authors did not support corticosteroid treatment for SARS-CoV-2 lung injury,5 and glucocorticoids are rarely used in descriptive studies of critically ill patients with COVID-19 pneumonia admitted in the intensive care unit (ICU).6 , 7 Interestingly, pathological findings in a deceased patient after acute respiratory distress syndrome (ARDS) due to SARS-CoV-2 infection have been recently described.8 The authors concluded that some histological lesions like pulmonary edema and hyaline membrane formation might be the target for corticosteroid use in severe patients. Another team have performed postmortem biopsies in 6 COVID-19 positive patients and reported the presence of acute fibrinous and organizing pneumonia (AFOP), which differ from the diffuse alveolar damage (DAD) usually associated with ARDS, and is a well-known target of corticosteroids.9 This is why, starting from these findings of a specific histological pattern sensitive to glucocorticoids to go to a clinical point of view, and in order to improve knowledge about the potential impact of corticosteroid therapy in ARDS COVID-19 patients, we report an impressive response to corticosteroids in 2 critically ill patients without comorbidities hospitalized in April 2020 in a French ICU for confirmed SARS-CoV-2 pneumonia by reverse transcription-polymerase chain reaction (RT-PCR).
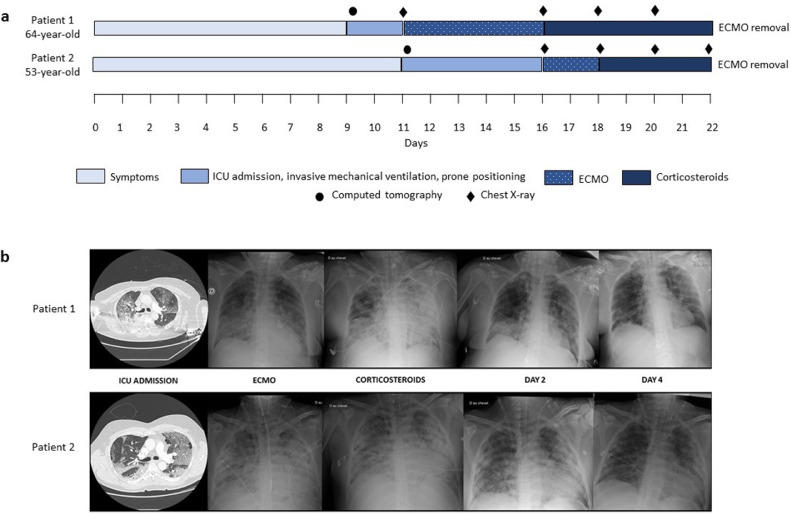
Schematic representation of time-course of major events for both cases is presented in Fig. 1 a. After immediate intensive care unit admission and intubation, clinical condition impaired rapidly with severe ARDS despite protective mechanical ventilation strategy with high level of positive end-expiratory pressure, neuromuscular blockers use and prone positioning. Initial computed tomography examination showed bilateral ground glass opacities and reticulation (crazy paving pattern) for both patients, with small posterior consolidations in patient 1. Because of refractory hypoxemia, veno-venous extracorporeal membrane oxygenation (ECMO) was implemented few days after intubation. Unfortunately, we noted radiological worsening with diffuse alveolar opacities and persistent worrisome level of hypoxemia without cardiac involvement and co-infection. A low-dose methylprednisolone treatment (1 mg/Kg/day) was initiated as rescue therapy. The next day and subsequently, we observed a significant clinical and radiological improvement allowing ECMO removal, and then weaning from mechanical ventilation (Fig. 1b).
Fig. 1.
(a) Schematic time course of two critically ill COVID-19 patients. Dots and lozenges represent computed tomography and chest X-rays, respectively, corresponding to Fig. 1b. (b) Radiological evolution of two patients with severe acute respiratory distress syndrome related to COVID-19 who were treated with low-dose corticosteroids. ICU: intensive care unit, ECMO: extracorporeal membrane oxygenation.
Pathological findings of SARS-CoV-2-induced ARDS are still poorly understood and currently being explored. Some severe COVID-19 patients seem to present a specific pattern characterized by a rapid adverse course leading to refractory ARDS associated with predominant diffuse radiological alveolar opacities. Overwhelming inflammation and cytokine-related lung injury could maybe explain this type of aggressive pneumonia. Consequently, if glucocorticoids may not be helpful in all severe SARS-CoV-2 pneumonia associated with predominant ground glass opacity in chest imaging, our experience highlights that some selected critically ill patients with Covid-19 would benefit from wise and timely use of corticosteroids. Further studies are warranted to test this hypothesis.
Declaration of Competing Interest
The authors declare that they have no competing interest.
Footnotes
Correspondence regarding the article published by Yang et al., April 10, 2020.
References
- 1.Yang Z., Liu J., Zhou Y., Zhao X., Zhao Q., Liu J. The effect of corticosteroid treatment on patients with coronavirus infection: a systematic review and meta-analysis. J Infect. 2020 Apr 10 doi: 10.1016/j.jinf.2020.03.062. pii: S0163-4453(20)30191-2[Epub ahead of print] Review. PubMed PMID 32283144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Phua J., Weng L., Ling L., Egi M., Lim C.M., Divatia J.V. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30161-2. PMID: 32272080Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 Feb 15;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. Epub 2020 Jan 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected—Interim guidance. Published January 28, 2020. Accessed February 11, 2020. https://www.who.int/publications-detail/clinicalmanagement-of-severe-acute-respiratoryinfection-when-novel-coronavirus-(ncov)-infection-is-suspected
- 5.Russel C.D., Millar J.E., Baillie J.K. Clinical evidence does not support corticosteroid treatment for 2019-nCoV lung injury. Lancet. 2020;395:473–475. doi: 10.1016/S0140-6736(20)30317-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grasselli G., Zangrillo A., Zanella A., Antonelli M., Cabrini L., Castelliet A. COVID-19 Lombardy ICU network. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the lombardy region, Italy. JAMA. 2020 Apr 6 doi: 10.1001/jama.2020.5394. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhatraju P.K., Ghassemieh B.J., Nichols M., Kim R., Jerome K.R., Nalla A.K. Covid-19 in critically Ill patients in the seattle region - case series. N Engl J Med. 2020 Mar 30 doi: 10.1056/NEJMoa2004500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. Apr 2020;8(4):420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Copin M.C., Parmentie E., Duburcq T., Poissy J., Mathieu D., Lille COVID-19 ICU and Anatomopathology Group Time to consider histologic pattern of lung injury to treat critically ill patients with COVID-19 infection. Intensive Care Med. 2020 Apr 23 doi: 10.1007/s00134-020-06057-8. doi.org/[Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]