Throughout our nation, and in many Asian and European hospitals, there has been a profound decrease in patients without coronavirus disease 2019 (COVID-19) seeking emergent care. This reduction has been observed across all major specialties and has affected patients treated for cardiac, oncologic, and neurologic diagnoses alike. The reasons behind this decline are multifactorial and include factors affecting the hospitals' and patients' decisions to offer/seek care, respectively. On the patients' side, the reluctance to seek emergency department care for life-threatening diagnoses is primarily driven by their fear of becoming infected with COVID-19 while in the hospital. For many, the perceived risk of COVID-19 infection outweighs the benefits of urgent medical evaluation. This, in turn, has led to delays in care, often with profound repercussions. At the Medical University of South Carolina, for example, the Washington Post reported late presentations of appendicitis in 70% of patients on the service.1 Late presentation of appendicitis can result in abscess formation, requiring prolonged antibiotics therapy and surgical drainage, all before definitive appendectomy treatment. Similarly, in a recent New England Journal of Medicine commentary, Rosenbaum2 discusses several cases of delayed care, as well as the workflow changes in various subspecialties.
At our institution, similarly, we have seen both a huge decline in patients seeking care for neurologic and neurosurgical diagnoses, as well as late presentation of life-threatening conditions. For example, a 62-year-old white female patient was brought to our emergency department with somnolence. By her husband's report, she developed severe headache 6 days before presentation, with associated nausea and vomiting. She refused to seek care at the hospital due specifically to fear of contracting COVID-19.
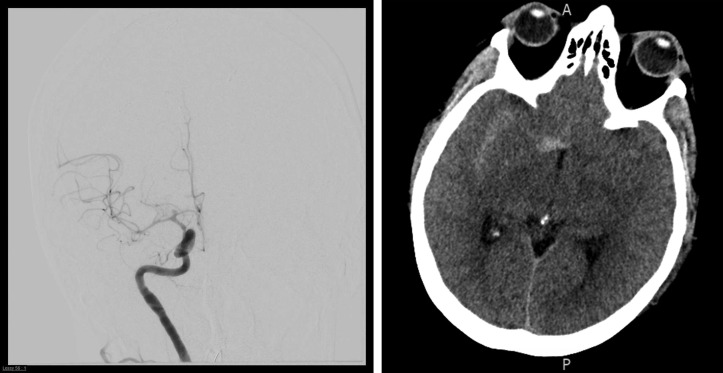
At presentation, she was obtunded, not following commands, and not protecting her airway. She was emergently intubated, and computed tomography/computed tomography angiogram demonstrated subacute subarachnoid hemorrhage most pronounced in the right sylvian fissure, a right carotid terminus aneurysm, and moderate multifocal vasospasm (Figure 1 ). Her sodium at presentation was 114 mmol/L. Despite endovascular embolization of the aneurysm and aggressive medical care, her examination remains poor. What remains unknown is how many patients with known or unknown pathologies are having progression of a deficit (i.e., worsening vision secondary to a supersellar mass or worsening cervical myelopathy) that would otherwise have brought them to seek urgent medical care.
Figure 1.
Right internal carotid artery (ICA) injection demonstrates a carotid terminus aneurysm, and moderate multifocal vasospasm (left panel). Axial non-contrast CT demonstrates subacute subarachnoid hemorrhage most pronounced in the right sylvian fissure (right panel).
Fortunately, we are seeing a significant decrease in admissions as the rate of new COVID-19 cases has leveled out. In our own institution, resources and staff are finally being able to assist with non-COVID patient duties. Rather than being able to only perform emergent surgeries, we are starting to schedule urgent and semi-elective cases. Faculty, house-staff, and physician extenders, who had been redeployed to help with the COVID-19 pandemic, are slowly returning to their previous roles. In the next few weeks, we will need to create an algorithm to identify patients whose surgeries must be prioritized. Who should be scheduled first: A 68-year-old patient with cervical spondylotic myelopathy, a 47-year-old patient with a glioblastoma, or a 36-year-old patient with a middle cerebral artery aneurysm? These decisions will be difficult to make, but, yet, must be made in the near future.
Quite likely, the greater challenge will be finding the people who are afraid to seek care to begin with. Social distancing has led to isolation and fewer visits by friends and family members. The support network that is often the catalyst to seek medical care, and also the system that provides for them in times of convalescence, must be reestablished. As the pandemic subsides, we will need to ask our leaders, public health officials, and the media to send a message to patients at risk: please seek help if you're not well or having worsening symptoms.
Footnotes
Conflict of interest statement: The authors declare that the article content was composed in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Patients with heart attacks, strokes and even appendicitis vanish from hospitals. Washington Post. April 19. 2020. [Google Scholar]
- 2.Rosenbaum L. The untold toll—The pandemic’s effects on patients without COVID-19. https://doi.org/10.1056/NEJMms2009984 [e-pub ahead of print]. N Engl J Med. accessed May 3, 2020. [DOI] [PubMed]