Abstract
There is no consensus for the treatment of a tandem occlusion (TO) in a patient presenting with an acute ischemic stroke. In this review article, we will focus on the controversial treatment strategies for TOs. First, we will discuss treatment options including retrograde, antegrade, and delayed approaches. Second, the role of carotid stent placement versus balloon angioplasty for the extracranial occlusion will be presented. Third, anticoagulation and antiplatelet regimens for the treatment TOs published in the literature will be reviewed. Finally, we will discuss whether there is a role for coil occlusion of the cervical carotid artery or whether staged carotid revascularization days after mechanical thrombectomy of the intracranial occlusion maybe appropriate. The optimal treatment strategy of TO has not been established and further larger trials need to be performed to answer the question.
Keywords: stroke, embolization, stent, angioplasty, occlusion, stenosis, interventional radiology
Tandem occlusions (TOs) involving the ipsilateral internal carotid artery (ICA) and a central large intracranial vessel occur in up to 20% of patients with an acute ischemic stroke (AIS). 1 Intravenous tissue plasminogen activator (IV-tPA) has a limited role in TOs due to its diminished ability to penetrate and lyse the thrombus. 2 3 4 5 This is related to poor antegrade blood flow and a large thrombus burden. Clinical improvement is seen only in 25% of cases with this presentation after the administration of IV t-PA. 6 Over the past 5 years, endovascular thrombectomy has become the standard of care for the treatment of an AIS presenting up to 24 hours from ictus; however, these trials did not specifically aim to evaluate patients with TOs. 7 8 9 10 11 12 13 14 In the ESCAPE trial, 17% of the total patient population presented with acute TOs. 9 MR CLEAN and REVASCAT investigators reported an incidence of 32.3 and 18.6% TOs, respectively. 8 12 SWIFT PRIME and EXTEND IA trials excluded subjects with cervical carotid dissection or complete occlusion. 10 11 In a meta-analysis of 33 studies with acute TOs published in 2018, about half of the patients treated with mechanical thrombectomy had a good outcome. 15
In this review article, we will focus on the treatment strategies for TOs. First, we will discuss whether intracranial or extracranial lesions should be treated first. Second, we will shed some light on whether the carotid lesion is best treated with balloon angioplasty or stent placement. Third, we will briefly discuss different antithrombotic and platelet regimens in the treatment of a carotid stenosis in the acute stroke setting. Finally, we will discuss whether there is a role for coil occlusion of the cervical carotid artery in the acute setting or whether staged carotid revascularization days after mechanical thrombectomy of the intracranial occlusion maybe appropriate.
Which Occlusion Should Be Treated First?
It remains unclear if the extracranial or intracranial lesions should be treated first. In a meta-analysis published in 2018, eight studies provided data on 90-day modified Rankin's scale (mRS) scores of less than or equal to 2 in extracranial-first mechanical thrombectomy (MT) treatments of TO patients with a rate of 53%, while seven studies in intracranial-first treatment showed a rate of 49%. The 90-day mortality was 8% in the extracranial-first and 15% in the intracranial-first patients, respectively. No difference was seen between both groups for procedure-related complications, symptomatic intracranial hemorrhage (sICH), thrombolysis in cerebral infarction (TICI) IIB/III, carotid revascularization rates, or procedural times. 15 Since this publication, more articles have evaluated whether carotid revascularization should be performed antegrade versus retrograde. Antegrade revascularization is when the extracranial lesion is treated first, whereas in retrograde the intracranial lesion is treated first. Yang et al evaluated 60 TOs and found more favorable outcomes in patients undergoing retrograde therapy than in patients who received the antegrade approach. Patients undergoing the retrograde approach spent less time in distal occlusion recanalization (125 [86–167] vs. 95 [74–122] minutes; p = 0.04) and achieved better functional outcomes at 90 days (69.0% [20/29] vs. 32.3% [10/31]; p = 0.004) than in patients who received antegrade therapy. 16 Eker et al in a series of 121 patients with TOs found no difference between the antegrade and retrograde approach with a trend toward less distal emboli using the retrograde approach (4.0 vs. 13.0%, p = 0.082). 17 Furthermore, Wallocha et al in a series of 163 patients showed no difference in clinical outcome when comparing the antegrade with the retrograde approach. The regression analysis of the cohort showed that only younger age ( p = 0.002) and shorter recanalization times ( p = 0.017) were associated with good outcome. 18 The authors' initial hypothesis was that a better outcome should be obtained in the retrograde approach since patients would mostly benefit from the earliest possible intracranial recanalization. Furthermore, in the hypothesis they assumed the acute symptoms were related to the middle cerebral artery occlusion rather than to the extracranial ICA occlusion in this population with a chronic high-grade ICA stenosis. Among the patients from the TITAN cohort, the order of treatment of intracranial occlusion or cervical occlusion led to a similar rate of successful reperfusion. 19 As expected, treating the intracranial occlusion first was associated with faster time from puncture to reperfusion; however, the order of treatment was not associated with clinical outcomes.
The main advantage of the antegrade approach ( Fig. 1 ) is the theoretical increased likelihood of successful distal recanalization following improvement in proximal flow due to the increase in distal perfusion from collaterals. Another advantage is the theoretical decrease risk of vessel dissection or perforation because of nonblind navigation of the ICA with the microwire and microcatheter after restoring flow in the cervical ICA. Furthermore, another advantage of the antegrade technique is the improved accessibility of intracranial lesions for effective treatment with thrombectomy device.
Fig. 1.
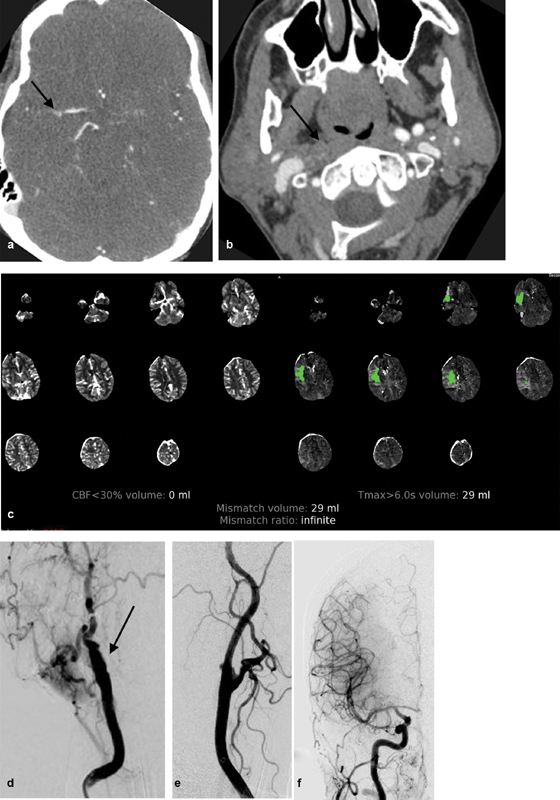
A 56-year-old woman with a history of a recent right carotid endarterectomy presents to the hospital 22 hours from last seen normal with stroke-like symptoms and National Institute of Health Stroke Score (NIHSS) of 11. Computed tomographic angiography (CTA) shows occlusion of the right internal carotid artery and an embolus at the right middle cerebral artery (RMCA) bifurcation ( a and b ; black arrows). CT perfusion with the RAPID software shows a 29-mL volume penumbra with no evidence of infarcted tissue ( c ). Initial right anterior oblique (RAO) right common carotid artery (RCCA) angiography shows an occlusion of the right internal carotid artery (RICA) at its origin ( d ; black arrow). The patient subsequently underwent antegrade revascularization with placement of a carotid stent and mechanical thrombectomy of the RMCA embolus. Final lateral RCCA angiography over the neck shows a widely patent RICA ( e ). Final RCCA angiography in the anteroposterior (AP) projection centered over the head shows a widely patent RMCA and right anterior cerebral artery consistent with a thrombolysis in cerebral infarction scale (TICI) score of III ( f ). The patient was discharged 7 days after the stroke with NIHSS of 4.
Disadvantages of the antegrade technique include the risk of distal embolization from stent placement and the mechanical thrombectomy device getting entrapped within the carotid stent. Distal embolization during treatment of the carotid lesion can be prevented by use of a distal or proximal protective device. Entrapment of the thrombectomy device within the carotid stent can also be avoided by advancing the occlusion balloon or sheath distal to the carotid stent. Furthermore, with the antegrade technique, there is a theoretical concern of migration or occlusion of the carotid stent by placing the large guide sheath through the stent during performance of the intracranial thrombectomy. Another potential disadvantage of the antegrade approach compared with the retrograde strategy is that the procedural time used for carotid stent placement increases the time from symptom onset to intracranial reperfusion, which might lead to an increased final infarct volume. 20 21 Moreover, restoration of blood flow after primary carotid artery stenting (CAS) may led to an increased pressure on the intracranial thrombus, which may result in clot fragmentation distally into the territory and this is known to be associated with a worse outcome. 22
Proponents of the retrograde approach ( Fig. 2 ) claim the intracranial occlusion is the most urgent step in revascularization of TOs since obtaining TICI III flow will limit the size of the cerebral infarction. Moreover, successful intracranial thrombectomy allows for the administration of antiplatelet agents for carotid stent placement which may be questionable in case of failure to open the intracranial LVO. Disadvantages include blindly navigating through the ICA and intracranial circulation possibly causing an arterial dissection/perforation or distal embolization. With both techniques, balloon angioplasty and carotid stent placement can be performed utilizing distal or proximal protection. Based on this analysis, a preferred approach cannot be determined.
Fig. 2.
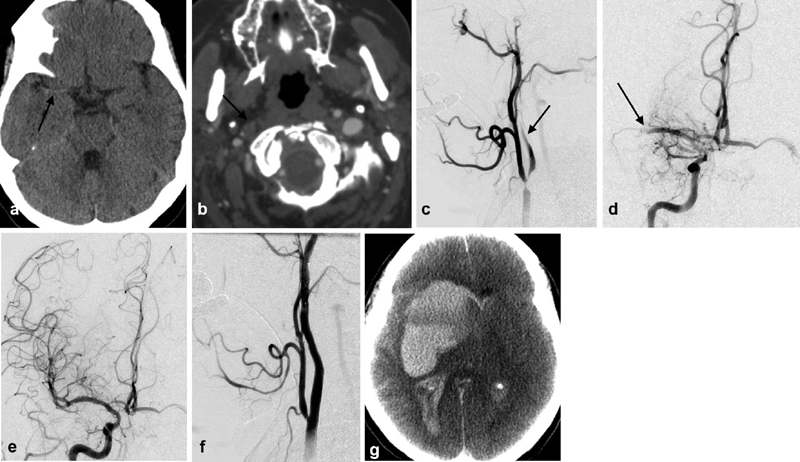
A 65-year-old woman who was last seen normal at 10 p.m. on August 20, 2018. She went to an outside hospital, where she initially presented with NIH stroke scale of 10 and was administered intravenous (IV) tPA. She was subsequently transferred to our hospital. Upon presentation to the emergency room, her NIH stroke scale was 15. CT shows a hyperdense RMCA ( a , black arrow). CTA ( b ) shows occlusion of the RICA at its origin black arrow. Initial RCCA angiography ( c ) shows very poor antegrade flow within the cervical segment of the RICA (black arrow). Initial RICA angiography ( d ) shows an embolus within the mid M1 segment thrombolysis in cerebral infarction (TICI) 0 flow (black arrow). The patient was loaded with dual-antiplatelet agents and treated using the retrograde approach. Final RCCA angiography shows a widely patent RMCA with TICI III flow ( e ). The RICA is also widely patent after balloon angioplasty/stent placement ( f ). Approximately 3 hours later, patient had acute deterioration of her neurological exam. CT showed acute intracerebral hemorrhage with midline shift ( g ). The patient was declared brain dead and died.
Should the Carotid Occlusion Be Treated with Balloon Angioplasty or Stent Placement?
Studies directly comparing balloon angioplasty to carotid stent placement for the treatment of the extracranial component of a TO are sparse. A meta-analysis in 2018 showed no difference between outcomes with and without acute stent placement. Since this publication, a few additional studies have been published in the literature. Li et al in a cohort of 37 patients with a TO performed angioplasty alone in 18 patients and 19 underwent carotid stent placement. Successful recanalization rate was statistically significantly higher in the stenting group than in the angioplasty-alone group (74 vs. 39%) and although not statistically significant, more patients in the stent group than in the angioplasty-alone group had favorable outcomes (63 vs. 50%). 23 The STRATIS Registry included 147 patients with tandem lesions. Eighty patients underwent carotid stent placement, 43 patients underwent balloon angioplasty, and 24 patients did not undergo angioplasty or stent placement. Good outcomes (mRS, 0–2 at 90 days) were higher in the stenting group (68.5 vs. 42.2%; p = 0.003) with no difference in mortality or symptomatic hemorrhage. After adjustment for covariates, stenting continued to be associated with superior outcomes. 24 Most studies of TOs report stent placement within the proximal ICA prior to recanalization of the intracranial occlusion.
Advantages of acute stenting are most likely related to augmentation of perfusion with a widely patent carotid artery in addition to a lower likelihood of recurrent events and reocclusion that may occur in the hyperacute setting of untreated carotid artery. 25 Data from randomized controlled trials are limited. In the recently completed endovascular trials, acute stenting was performed in only a small portion of patients (REVASCAT trial: 9 patients, ESCAPE trial: 17 patients; MR CLEAN trial: 30 patients). 8 9 12 In the ESCAPE trial, although the number of tandem patients was small and not statistically significant, numerically there were higher rates of successful reperfusion (71 vs. 46%) and good outcomes (65 vs. 54%) with lower rates of death (6 vs. 15%) and sICH (0 vs. 8%) in the acute carotid intervention group compared with the no acute carotid intervention group. 26 Mpotsaris et al similarly observed a nonsignificant trend in their small sample size toward better outcomes in the acute stenting group versus nonstenting group (54 vs. 42%), as well as higher rates of independent ambulation (85 vs. 63%). 27 Based on the current evidence, patients suffering from acute TOs should not be deprived of an acute CAS. Reasons for this might be that (1) the vulnerable carotid lesion is stabilized, which prevents further cerebral thromboembolism within the postinterventional period and (2) the occurrence of sICH in acute TO seems justifiable with a rate between 4 and 9%, as demonstrated in large studies. 28 29 30 31 32 33 34 In a study of 62 patients with TOs, cervical balloon angioplasty alone was attempted followed by intracranial recanalization; however, 40 of 62 (65%) patients required stent placement in the acute setting due to elastic recoil or to maintain distal access. 35 A nationwide comparison study of stenting versus angioplasty in patients with carotid stenosis and acute stroke found the risk of mortality to be elevated in patients who underwent angioplasty. 36 Based on these retrospective case series, we can suggest that acute carotid stent placement at the time of intracranial thrombectomy may be appropriate.
Which Antithrombotic and Platelet Regimens in the Treatment of a Carotid Stenosis in the Acute Stroke Setting Are Preferred?
The data on the safety and efficacy of periprocedural antithrombotic medications during concomitant CAS and intracranial mechanical thrombectomy are scarce. 37 In the TITAN Registry, periprocedural heparin use during EVT of anterior circulation TOs was not associated with better functional, angiographic, or safety outcomes. 38 The dose of IV unfractionated heparin ranged from 1,500 to 2,500 IU. Post hoc analysis of the TREVO 2 trial showed that the use of heparin was independently associated with good functional outcome (90-day mRS: 0–2) (odds ratio [OR], 5.30; 95% confidence interval [CI], 1.70–16.48). 39 A post hoc analysis of the MERCI trial reported similar results. 40 41 Theoretically, the use of antithrombotic medication in the acute setting may increase the risk of sICH, given there is breakdown of the blood–brain barrier in an AIS. However, an international multicenter registry showed that antithrombotic therapy plus intracranial thrombectomy and carotid stent placement was associated with the highest recanalization rates without an increased incidence of sICH. 42 Many of the reports in the literature do not give unfractionated heparin in the acute setting of revascularization of a TO given the risk of sICH. The potential risk of sICH in patients with a TO treated with mechanical thrombectomy and CAS may depend on the size of the penumbra and infarct volume and further studies are warranted related to the use of heparin in this scenario.
The need of antiplatelet loading doses for carotid stent placement after the administration of IV thrombolytic medication for an AIS is a challenging situation and needs to be analyzed on a specific case-to-case basis. Many European series report utilizing an IV loading dose of acetylsalicylic acid (250–1,000 mg) and then an enteric loading dose of clopidogrel (300 mg) after a postprocedural follow-up CT scan shows no evidence of hemorrhage. 43 44 45 46 Other series have given a loading doses of clopidogrel (300–600 mg) and aspirin (300 mg) prior to stent placement without prior treatment with IV alteplase. 16 47 In other studies, patients treated with IV t-PA received aspirin (100 mg) and clopidogrel (75 mg) 24 hours after carotid stent placement. 16 23 A single study preferred the use of ticagrelor (TIC; 180 mg PO via a nasogastric tube) prior to emergent stent placement given the faster inhibition in platelet aggregation with an implemented bridging concept with the glycoprotein IIb/IIIa inhibitor eptifibatide (given as a single body weight adapted IV bolus) with strict blood pressure control (systolic blood pressure <130 mm Hg) for a minimum of 3 days. 48 Overlapping medication of full-dose glycoprotein IIb/IIIa inhibitor and dual-antiplatelet agents has been reported to be associated with an increased rate of sICH. 49 50 However, recently two studies showed that overlapping use of intraprocedural low-dose glycoprotein IIb/IIIa inhibitor and postprocedural dual-antiplatelet therapy showed a more durable patency of rescue intracranial stent placement without an increase rate of sICH in patients with AIS. 32 33
Based on the currently available literature, there is no clear antiplatelet regimen which appears to be superior for patients undergoing emergent stent placement for an AIS presenting with a TO with or without prior IV t-PA administration. The only antiplatelet agent which should not be used in an AIS is prasugrel which has a black box warning for patients with a history of transient ischemic attack or stroke. Eptifibatide may be the optional glycoprotein IIb/IIIa receptor for emergent carotid stent placement versus abciximab or tirofiban, given it reversibly binds only to activated platelets, has a shorter half-life, and can provide 80% platelet inhibition within less than 15 minutes (https://www.pbm.va.gov/PBM/clinicalguidance/drugclassreviews/GlycoproteinGPIIbIIIaReceptorInhibitorsDrugClassReview).
Does Coil Occlusion or Staged Revascularization of the Carotid Artery Have a Role?
In a staged approach, carotid revascularization with a CAS or endarterectomy is performed a few days after intracranial MT and represents an additional treatment option. The first reported case series for this approach was recently published with CAS days after MT and exclusion of postinterventional ICH. 51 In the acute setting, the proximal lesion was treated with balloon angioplasty to maintain access to the intracranial vessels. In this study, promising results were reported with a successful reperfusion rate of 80% and a favorable outcome of 67%. However, the study sample was small ( n = 15). The rationale for such a staged approach is that first the patient's overall favorable outcome can be ensured before the second intervention is performed and that futile stenting can be prevented in cases of an ICH after MT. In a second study of 35 patients treated with a conservative strategy, acute percutaneous transluminal angioplasty (PTA) and/or stenting was necessary in 8 (22.9%) and 3 patients (8.6%), respectively. Of 27 surviving patients, 7 (25.9%) underwent delayed treatment of the ICA lesion. No new embolic events occurred between MT and delayed treatment. A favorable clinical outcome (mRS ≤ 2) was achieved in 15/35 patients (45.7%) and was associated with higher baseline ASPECTS (OR: 1.62, 95% CI: 1.08–2.45, p = 0.002) and successful recanalization (OR: 9.39, 95% CI: 1.92–45.80, p = 0.0005). 46
Labeyrie et al reported 6 approaches to manage the cervical occlusion in 49 patients with TO (14% of MT): medical treatment alone in 16/64 (25%), stenting/angioplasty in 16/64 (25%), occlusion with coils in 12/64 (19%), angioplasty alone in 9/64 (14%), stent retriever in 8/64 (12%), and/or thromboaspiration in 3/64 (5%). Early ipsilateral embolic recurrence occurred in 9/64 (14%). It was strongly associated with the presence of a cervical intraluminal thrombus ( p = 0.001) and was then lower after occlusion with coils and stent retriever compared with medical treatment alone and thromboaspiration ( p = 0.002). Occlusion with coils had a lower rate of radiological intracranial hemorrhage at 48 hours compared with other approaches ( p = 0.009). The 3-month rates of favorable outcome ( p = 0.806) and mortality ( p = 0.878) were similar. One delayed stroke was imputable to an occlusion with coils, for a median (Q1–Q3) follow-up of 10 (3–20) months. 52 Data on staged revascularization or coil occlusion of the cervical ICA after intracranial thrombectomy of a TO is limited, and further studies need to be performed; therefore, no recommendations can be made.
Conclusion
In summary, the optimal treatment strategy of TO is not established and further larger trials need to be performed to answer the question. The authors believe that there is an equipoise for antegrade versus retrograde revascularization. There is reasonable evidence in favor of acute revascularization of the cervical carotid artery occlusion with stent placement. The optimal anticoagulation and antiplatelet regimen has not been established and many options exist. There is no evidence to support coil occlusion of the cervical carotid artery stenosis in the acute setting or data to suggest a staged approach may be appropriate.
Footnotes
Conflict of Interest None declared.
References
- 1.Rubiera M, Ribo M, Delgado-Mederos R et al. Tandem internal carotid artery/middle cerebral artery occlusion: an independent predictor of poor outcome after systemic thrombolysis. Stroke. 2006;37(09):2301–2305. doi: 10.1161/01.STR.0000237070.80133.1d. [DOI] [PubMed] [Google Scholar]
- 2.Kim Y S, Garami Z, Mikulik R, Molina C A, Alexandrov A V; CLOTBUST Collaborators.Early recanalization rates and clinical outcomes in patients with tandem internal carotid artery/middle cerebral artery occlusion and isolated middle cerebral artery occlusion Stroke 20053604869–871. [DOI] [PubMed] [Google Scholar]
- 3.National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group.Tissue plasminogen activator for acute ischemic stroke N Engl J Med 1995333241581–1587. [DOI] [PubMed] [Google Scholar]
- 4.Christou I, Felberg R A, Demchuk A M et al. Intravenous tissue plasminogen activator and flow improvement in acute ischemic stroke patients with internal carotid artery occlusion. J Neuroimaging. 2002;12(02):119–123. doi: 10.1111/j.1552-6569.2002.tb00107.x. [DOI] [PubMed] [Google Scholar]
- 5.Rubiera M, Alvarez-Sabín J, Ribo M et al. Predictors of early arterial reocclusion after tissue plasminogen activator-induced recanalization in acute ischemic stroke. Stroke. 2005;36(07):1452–1456. doi: 10.1161/01.STR.0000170711.43405.81. [DOI] [PubMed] [Google Scholar]
- 6.Linfante I, Llinas R H, Selim M et al. Clinical and vascular outcome in internal carotid artery versus middle cerebral artery occlusions after intravenous tissue plasminogen activator. Stroke. 2002;33(08):2066–2071. doi: 10.1161/01.str.0000021001.18101.a5. [DOI] [PubMed] [Google Scholar]
- 7.Goyal M, Menon B K, van Zwam W Het al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials Lancet 2016387(10029):1723–1731. [DOI] [PubMed] [Google Scholar]
- 8.Berkhemer O A, Fransen P S, Beumer D et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(01):11–20. doi: 10.1056/NEJMoa1411587. [DOI] [PubMed] [Google Scholar]
- 9.Goyal M, Demchuk A M, Menon B K et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019–1030. doi: 10.1056/NEJMoa1414905. [DOI] [PubMed] [Google Scholar]
- 10.Saver J L, Goyal M, Bonafe A et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015;372(24):2285–2295. doi: 10.1056/NEJMoa1415061. [DOI] [PubMed] [Google Scholar]
- 11.Campbell B C, Mitchell P J, Kleinig T J et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372(11):1009–1018. doi: 10.1056/NEJMoa1414792. [DOI] [PubMed] [Google Scholar]
- 12.Jovin T G, Chamorro A, Cobo E et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372(24):2296–2306. doi: 10.1056/NEJMoa1503780. [DOI] [PubMed] [Google Scholar]
- 13.Nogueira R G, Jadhav A P, Haussen D C et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018;378(01):11–21. doi: 10.1056/NEJMoa1706442. [DOI] [PubMed] [Google Scholar]
- 14.Albers G W, Marks M P, Kemp S et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378(08):708–718. doi: 10.1056/NEJMoa1713973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilson M P, Murad M H, Krings T et al. Management of tandem occlusions in acute ischemic stroke - intracranial versus extracranial first and extracranial stenting versus angioplasty alone: a systematic review and meta-analysis. J Neurointerv Surg. 2018;10(08):721–728. doi: 10.1136/neurintsurg-2017-013707. [DOI] [PubMed] [Google Scholar]
- 16.Yang D, Shi Z, Lin M et al. Endovascular retrograde approach may be a better option for acute tandem occlusions stroke. Interv Neuroradiol. 2019;25(02):194–201. doi: 10.1177/1591019918805140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eker O F, Bühlmann M, Dargazanli C et al. Endovascular treatment of atherosclerotic tandem occlusions in anterior circulation stroke: technical aspects and complications compared to isolated intracranial occlusions. Front Neurol. 2018;9:1046. doi: 10.3389/fneur.2018.01046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wallocha M, Chapot R, Nordmeyer H, Fiehler J, Weber R, Stracke C P. Treatment methods and early neurologic improvement after endovascular treatment of tandem occlusions in acute ischemic stroke. Front Neurol. 2019;10:127. doi: 10.3389/fneur.2019.00127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhu F, Bracard S, Anxionnat R et al. Impact of emergent cervical carotid stenting in tandem occlusion strokes treated by thrombectomy: a review of the TITAN collaboration. Front Neurol. 2019;10:206. doi: 10.3389/fneur.2019.00206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lockau H, Liebig T, Henning T et al. Mechanical thrombectomy in tandem occlusion: procedural considerations and clinical results. Neuroradiology. 2015;57(06):589–598. doi: 10.1007/s00234-014-1465-5. [DOI] [PubMed] [Google Scholar]
- 21.Marnat G, Mourand I, Eker O et al. Endovascular management of tandem occlusion stroke related to internal carotid artery dissection using a distal to proximal approach: insight from the RECOST study. AJNR Am J Neuroradiol. 2016;37(07):1281–1288. doi: 10.3174/ajnr.A4752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gratz P P, Schroth G, Gralla J et al. Whole-brain susceptibility-weighted thrombus imaging in stroke: fragmented thrombi predict worse outcome. AJNR Am J Neuroradiol. 2015;36(07):1277–1282. doi: 10.3174/ajnr.A4275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li W, Chen Z, Dai Z et al. Management of acute tandem occlusions: stent-retriever thrombectomy with emergency stenting or angioplasty. J Int Med Res. 2018;46(07):2578–2586. doi: 10.1177/0300060518765310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jadhav A P, Zaidat O O, Liebeskind D S et al. Emergent management of tandem lesions in acute ischemic stroke. Stroke. 2019;50(02):428–433. doi: 10.1161/STROKEAHA.118.021893. [DOI] [PubMed] [Google Scholar]
- 25.Johansson E, Cuadrado-Godia E, Hayden D et al. Recurrent stroke in symptomatic carotid stenosis awaiting revascularization: a pooled analysis. Neurology. 2016;86(06):498–504. doi: 10.1212/WNL.0000000000002354. [DOI] [PubMed] [Google Scholar]
- 26.Assis Z, Menon B K, Goyal M et al. Acute ischemic stroke with tandem lesions: technical endovascular management and clinical outcomes from the ESCAPE trial. J Neurointerv Surg. 2018;10(05):429–433. doi: 10.1136/neurintsurg-2017-013316. [DOI] [PubMed] [Google Scholar]
- 27.Mpotsaris A, Bussmeyer M, Buchner H, Weber W. Clinical outcome of neurointerventional emergency treatment of extra- or intracranial tandem occlusions in acute major stroke: antegrade approach with Wallstent and solitaire stent retriever. Clin Neuroradiol. 2013;23(03):207–215. doi: 10.1007/s00062-013-0197-y. [DOI] [PubMed] [Google Scholar]
- 28.Sivan-Hoffmann R, Gory B, Armoiry X et al. Stent-retriever thrombectomy for acute anterior ischemic stroke with tandem occlusion: a systematic review and meta-analysis. Eur Radiol. 2017;27(01):247–254. doi: 10.1007/s00330-016-4338-y. [DOI] [PubMed] [Google Scholar]
- 29.Behme D, Mpotsaris A, Zeyen P et al. Emergency stenting of the extracranial internal carotid artery in combination with anterior circulation thrombectomy in acute ischemic stroke: a retrospective multicenter study. AJNR Am J Neuroradiol. 2015;36(12):2340–2345. doi: 10.3174/ajnr.A4459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rangel-Castilla L, Rajah G B, Shakir H J et al. Management of acute ischemic stroke due to tandem occlusion: should endovascular recanalization of the extracranial or intracranial occlusive lesion be done first? Neurosurg Focus. 2017;42(04):E16. doi: 10.3171/2017.1.FOCUS16500. [DOI] [PubMed] [Google Scholar]
- 31.Steglich-Arnholm H, Holtmannspötter M, Kondziella D et al. Thrombectomy assisted by carotid stenting in acute ischemic stroke management: benefits and harms. J Neurol. 2015;262(12):2668–2675. doi: 10.1007/s00415-015-7895-0. [DOI] [PubMed] [Google Scholar]
- 32.Chang Y, Kim B M, Bang O Y et al. Rescue stenting for failed mechanical thrombectomy in acute ischemic stroke: a multicenter experience. Stroke. 2018;49(04):958–964. doi: 10.1161/STROKEAHA.117.020072. [DOI] [PubMed] [Google Scholar]
- 33.Baek J H, Kim B M, Kim D J, Heo J H, Nam H S, Yoo J. Stenting as a rescue treatment after failure of mechanical thrombectomy for anterior circulation large artery occlusion. Stroke. 2016;47(09):2360–2363. doi: 10.1161/STROKEAHA.116.014073. [DOI] [PubMed] [Google Scholar]
- 34.Jeong H G, Kim B J, Yang M H, Han M K, Bae H J, Lee S H. Stroke outcomes with use of antithrombotics within 24 hours after recanalization treatment. Neurology. 2016;87(10):996–1002. doi: 10.1212/WNL.0000000000003083. [DOI] [PubMed] [Google Scholar]
- 35.Kang D H, Kim Y W, Hwang Y H, Kim Y S. Endovascular recanalization of acute tandem cervical carotid and intracranial occlusions: efficacy of cervical balloon angioplasty alone then intracranial target recanalization strategy. World Neurosurg. 2019;126:e1268–e1275. doi: 10.1016/j.wneu.2019.02.240. [DOI] [PubMed] [Google Scholar]
- 36.Villwock M R, Padalino D J, Deshaies E M. Carotid artery stenosis with acute ischemic stroke: stenting versus angioplasty. J Vasc Interv Neurol. 2015;8(04):11–16. [PMC free article] [PubMed] [Google Scholar]
- 37.van de Graaf R A, Chalos V, Del Zoppo G J, van der Lugt A, Dippel D WJ, Roozenbeek B. Periprocedural antithrombotic treatment during acute mechanical thrombectomy for ischemic stroke: a systematic review. Front Neurol. 2018;9:238. doi: 10.3389/fneur.2018.00238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhu F, Piotin M, Steglich-Arnholm H et al. Periprocedural heparin during endovascular treatment of tandem lesions in patients with acute ischemic stroke: a propensity score analysis from TITAN Registry. Cardiovasc Intervent Radiol. 2019;42(08):1160–1167. doi: 10.1007/s00270-019-02251-4. [DOI] [PubMed] [Google Scholar]
- 39.Winningham M J, Haussen D C, Nogueira R G et al. Periprocedural heparin use in acute ischemic stroke endovascular therapy: the TREVO 2 trial. J Neurointerv Surg. 2018;10(07):611–614. doi: 10.1136/neurintsurg-2017-013441. [DOI] [PubMed] [Google Scholar]
- 40.Nahab F, Walker G A, Dion J E, Smith W S. Safety of periprocedural heparin in acute ischemic stroke endovascular therapy: the multi MERCI trial. J Stroke Cerebrovasc Dis. 2012;21(08):790–793. doi: 10.1016/j.jstrokecerebrovasdis.2011.04.009. [DOI] [PubMed] [Google Scholar]
- 41.Nahab F, Kass-Hout T, Shaltoni H M. Periprocedural antithrombotic strategies in acute ischemic stroke interventional therapy. Neurology. 2012;79(13) 01:S174–S181. doi: 10.1212/WNL.0b013e31826959af. [DOI] [PubMed] [Google Scholar]
- 42.Papanagiotou P, Haussen D C, Turjman F et al. Carotid stenting with antithrombotic agents and intracranial thrombectomy leads to the highest recanalization rate in patients with acute stroke with tandem lesions. JACC Cardiovasc Interv. 2018;11(13):1290–1299. doi: 10.1016/j.jcin.2018.05.036. [DOI] [PubMed] [Google Scholar]
- 43.Rodrigues M, Cunha A, Figueiredo S et al. Emergent carotid artery stenting in atherosclerotic disease of the internal carotid artery with tandem intracranial occlusion. J Neurol Sci. 2018;387:196–198. doi: 10.1016/j.jns.2018.02.034. [DOI] [PubMed] [Google Scholar]
- 44.Marnat G, Bühlmann M, Eker O F et al. Multicentric experience in distal-to-proximal revascularization of tandem occlusion stroke related to internal carotid artery dissection. AJNR Am J Neuroradiol. 2018;39(06):1093–1099. doi: 10.3174/ajnr.A5640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Díaz-Pérez J, Parrilla G, Espinosa de Rueda Met al. Mechanical thrombectomy in acute stroke due to carotid occlusion: a series of 153 consecutive patients Cerebrovasc Dis 201846(3-4):132–141. [DOI] [PubMed] [Google Scholar]
- 46.Blassiau A, Gawlitza M, Manceau P F et al. Mechanical thrombectomy for tandem occlusions of the internal carotid artery-results of a conservative approach for the extracranial lesion. Front Neurol. 2018;9:928. doi: 10.3389/fneur.2018.00928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Park S E, Choi D S, Baek H Jet al. Endovascular therapy of acute ischemic stroke related to tandem occlusion: comparison of occlusion and severe stenosis of the proximal cervical internal carotid artery Br J Radiol 2018 10.1259/bjr.20180051[Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shimada Y J, Bansilal S, Wiviott S D et al. Impact of glycoprotein IIb/IIIa inhibitors on the efficacy and safety of ticagrelor compared with clopidogrel in patients with acute coronary syndromes: analysis from the Platelet Inhibition and Patient Outcomes (PLATO) trial. Am Heart J. 2016;177:1–8. doi: 10.1016/j.ahj.2016.03.015. [DOI] [PubMed] [Google Scholar]
- 49.Heck D V, Brown M D. Carotid stenting and intracranial thrombectomy for treatment of acute stroke due to tandem occlusions with aggressive antiplatelet therapy may be associated with a high incidence of intracranial hemorrhage. J Neurointerv Surg. 2015;7(03):170–175. doi: 10.1136/neurintsurg-2014-011224. [DOI] [PubMed] [Google Scholar]
- 50.Stampfl S, Ringleb P A, Möhlenbruch M et al. Emergency cervical internal carotid artery stenting in combination with intracranial thrombectomy in acute stroke. AJNR Am J Neuroradiol. 2014;35(04):741–746. doi: 10.3174/ajnr.A3763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Akpinar C K, Gürkaş E, Aytac E. Carotid angioplasty-assisted mechanical thrombectomy without urgent stenting may be a better option in acute tandem occlusions. Interv Neuroradiol. 2017;23(04):405–411. doi: 10.1177/1591019917701113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Labeyrie M A, Ducroux C, Civelli V et al. Endovascular management of extracranial occlusions at the hyperacute phase of stroke with tandem occlusions. J Neuroradiol. 2018;45(03):196–201. doi: 10.1016/j.neurad.2017.10.003. [DOI] [PubMed] [Google Scholar]


