Abstract
Background
Medial patellofemoral ligament reconstruction and tibial tuberosity anteromedialization are common treatment options for recurrent lateral patellar instability, although ligament reconstruction is not commonly applied to knees with lateral malalignment.
Methods
Multibody dynamic simulation was used to assess knee function following tibial tuberosity anteromedialization and medial patellofemoral ligament reconstruction for knees with lateral malalignment. Dual limb squatting was simulated with six models representing knees being treated for patellar instability with an elevated tibial tuberosity to trochlear groove distance. The patellar tendon attachment on the tibia was shifted medially (10 mm) and anteriorly (5 mm) to represent tibial tuberosity anteromedialization. A hamstrings tendon graft was represented for medial patellofemoral ligament reconstruction. Patellar tracking was quantified based on bisect offset index. The patellofemoral contact pressure distribution was quantified using discrete element analysis. Data were analyzed with repeated measures comparisons with post-hoc tests.
Findings
Both procedures significantly reduced bisect offset index, primarily at low flexion angles. The decrease was larger for tibial tuberosity anteromedialization, peaking at 0.18. Tibial tuberosity anteromedialization shifted contact pressures medially, significantly increasing the maximum medial contact pressure at multiple flexion angles, with the maximum pressure increasing up to 1 MPa.
Interpretation
The results indicate tibial tuberosity anteromedialization decreases lateral patellar maltracking more effectively than medial patellofemoral ligament reconstruction, but shifts contact pressure medially. Tibial tuberosity anteromedialization is likely to reduce the risk of post-operative instability compared to medial patellofemoral ligament reconstruction. The medial shift in the pressure distribution should be considered for knees with medial cartilage lesions, however.
Keywords: patellar instability, tibial tuberosity anteromedialization, medial patellofemoral ligament reconstruction, patellar tracking, cartilage pressure
1. Introduction
Medial patellofemoral ligament (MPFL) reconstruction is currently the most popular surgical option to treat recurrent lateral patellar instability [22, 27], but other options are recommended to address specific types of pathology. Tibial tuberosity osteotomy and medialization is typically recommended for patients with a laterally malaligned tibial tuberosity, typically expressed as a tibial tuberosity to trochlear groove (TT-TG) distance greater than 15 to 20 mm based on diagnostic imaging [11, 34, 48]. Medializing the tibial tuberosity reduces the TT-TG distance and the lateral force acting on the patella during function. Medialization is commonly combined with anteriorization (anteromedialization) to decrease patellofemoral compression. Compared to MPFL reconstruction, tuberosity medialization is associated with increased operative morbidity and post-operative pain, longer rehabilitation, and the risk of fracture or non-union at the osteotomy site, so MPFL reconstruction has also been advocated as a viable surgical option regardless of the TT-TG distance [20].
Numerous biomechanical studies have been performed to evaluate the influence of tibial tuberosity anteromedialization and MPFL reconstruction on post-operative function, but direct comparisons of the approaches have been limited. In vitro simulation studies have generally shown that both tibial tuberosity medialization and MPFL reconstruction decrease lateral maltracking [31, 32, 39, 43–45]. Tuberosity medialization also shifts contact pressures medially on the patella [35, 39], which is a concern for patients with medial cartilage lesions [33]. MPFL reconstruction has also been shown to shift contact pressures medially, with the primary effect an increase in pressure applied to the medial facet of the patella, but only when a short resting length or non-anatomic femoral fixation increase graft tension [3, 32, 44]. In vitro studies performed with cadaveric specimens do not include the anatomic pathology associated with patellar instability, so computational models have been developed to simulate dynamic function for pathologic knees. Dynamic simulation studies have shown that both tibial tuberosity medialization and MPFL reconstruction decrease lateral patellar maltracking [1, 14, 15, 17]. Tibial tuberosity medialization and anteromedialization have been shown to increase the pressure applied to medial cartilage, with the effect smaller for anteromedialization [14]. MPFL reconstruction allowing some lateral patellar glide in the trochlear groove when setting the graft length has been shown to have minimal influence on the patellofemoral contact pressure distribution [16].
The current study focuses on application of MPFL reconstruction to treat patellar instability for knees with an elevated TT-TG distance by comparing the approach to tibial tuberosity anteromedialization. The study utilizes dynamic simulation of function applied to knees being treated for recurrent patellar instability to characterize pre-operative and post-operative patellar tracking and pressure applied to patellofemoral cartilage. The hypothesis of the study is that tibial tuberosity anteromedialization will decrease lateral patellar maltracking more than MPFL reconstruction, but also elevate contact pressures applied to medial patellofemoral cartilage.
2. Methods
2.1. Dynamic Simulation of Knee Function
Dynamic simulation of knee function was performed with six multibody dynamic simulation models (RecurDyn, FunctionBay, Seongnam, Korea) representing the symptomatic knees of subjects treated for recurrent lateral patellar instability [14–17]. The study was approved by the institutional review board. The models were reconstructed (3D Doctor, Able Software Corp, Lexington, MA, United States and Mimics, Materialise, Leuven, Belgium) from MRI scans (five 3.0 T and one 1.5 T, proton density weighted, slice thickness ranging from 0.5 mm to 3.0 mm). The models included tension-only springs representing the cruciate ligaments (2 each), collateral ligaments (3 each), patellar tendon (5), posterior joint capsule (4), lateral retinaculum (2), and the residual medial retinaculum following injury to the MPFL (1) (Fig. 1A). Stiffness, damping, and pre-strain at full extension were assigned to the springs based on previous studies [5, 7, 10, 42]. Quadriceps forces representing the vastus medialis obliquus, vastus lateralis, and combination of the vastus intermedius, rectus femoris, and vastus medialis longus were applied in physiological directions through springs representing the quadriceps tendon based on previous studies [29, 50]. The vastus medialis obliquus was represented in a weakened state, based on subjects with lateral patellar malalignment [29], by carrying 5% of the total quadriceps force [18]. Medial and lateral hamstrings forces were also applied, with a total magnitude equal to one-third of the quadriceps force during knee squatting [13]. The bones and cartilage of the femur, tibia and patella were extracted from the MRI scans, with cartilage thickness quantified as the distance from elements on the articular surface to the underlying bone. Contact at the articulating surfaces was represented by simplified Hertzian contact [24]. Anatomical coordinate systems were fixed to the femur and tibia to characterize tibiofemoral kinematics based on the floating axis convention [23].
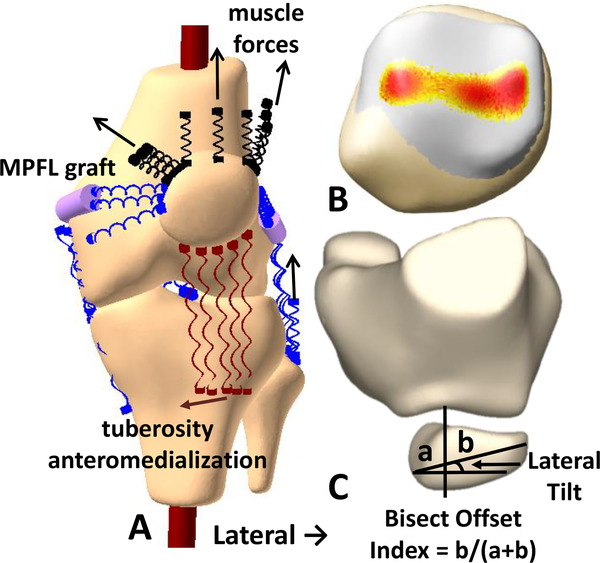
Fig. 1:
(A) A multibody dynamic simulation model of a knee showing an MPFL graft wrapping around the femur and the direction of tibial tuberosity anteromedialization. (B) Representation of the patellofemoral pressure distribution. (C) The measures used to characterize patellar tracking.
The patellofemoral contact pressure distribution was characterized using discrete element analysis [19] (Fig. 1B). When the patella was within the trochlear groove, overlap of femoral and patellar cartilage surfaces determined articular reaction forces and moments based on linear elastic theory (discrete element analysis). These forces and moments were balanced against patellofemoral reaction forces and moments output from multibody dynamic simulation. Starting with the patellofemoral alignment determined from dynamic simulation, the position of the patella was iteratively adjusted to balance the total articular compression force, medial/lateral force and lateral tilt moment applied to the patella between discrete element analysis and multibody dynamic simulation.
The modeling approach was previously validated by comparing knee function within a diagnostic scanner for subjects being treated for patellar instability to simulated knee function for models representing each subject. The functional activity was either dynamic knee extension against gravity within a dynamic CT scanner (Aquilion ONE, Canon Medical Systems, Ōtawara, Japan) [12] or isometric knee extension against resistance at multiple positions of knee flexion within an MRI scanner (Magnetom Skyra, Siemens Healthcare GmbH, Erlangen, Germany) [6], with simulations developed to represent each activity [14, 16]. The activities were reconstructed from the diagnostic imaging and characterized with respect to the same anatomical coordinate systems applied to the computational models [6, 12]. The simulations reproduced the patellar tracking patterns of the subjects, with lateral tracking peaking near full extension [17] and a decrease in lateral tracking following surgical stabilization [16]. For nine models, root mean square errors for the simulated pre-operative lateral patellar shift and tilt were 2.7 mm and 3.7°, respectively [16]. The simulations also produced contact pressure patterns similar to those based on overlap of cartilage surfaces from the diagnostic imaging and linear elastic theory. The simulations showed pressure primarily applied to the lateral facet of the patella, similar to the reconstructions from diagnostic imaging, with a root mean square error for maximum pressure of 1.4 MPa for ten models [14]. The discrete element analysis approach for characterizing the pressure distribution was also previously validated against in vitro experimental measurements characterizing the influence of altering forces applied to the patella on the pressure distribution [19]. Additional models generated for the current study were similarly validated against function of the subjects represented by the models, maintaining the previously reported trends and levels for root mean square errors.
Knee function was assessed for simulation of a dual limb knee squat [14]. A simulated hip joint allowed flexion/extension, varus/valgus rotation, and proximal/distal translation. A simulated ankle joint allowed 3 rotational degrees of freedom. Body weight of 200 N was applied at the hip. The total quadriceps force increased from 42 N at full extension to 300 N at 90° of flexion. To initiate motion, a flexion moment was applied at the hip over the first few degrees of flexion.
The six models with the largest recorded TT-TG distance values were chosen for analysis from a cohort of fifteen models representing knees with patellar instability. The models were aligned at full extension and validated with representation of knee function. Therefore, the TT-TG distance was quantified during simulated function rather than for representation of a supine, unloaded knee within an MRI or CT scanner. The TT-TG distance was characterized as the medial-lateral distance from the center of the tibial tuberosity to the deepest point of the trochlear groove [6]. The tibial tuberosity point was fixed to the moving tibia, while the deepest point of the groove was automatically identified (Matlab, Mathworks, Natick, MA, United States) at each flexion angle within a plane perpendicular to the long axis of the patella. Automated algorithms were used to identify anatomical landmarks that varied with the flexion angle to limit the variability associated with repeated manual identification of landmarks [21]. The medial-lateral direction was determined by the posterior condylar axis of the femur. The maximum TT-TG distance during squatting had to exceed 15 mm to be considered suitable for tibial tuberosity medialization, taking into account that measuring TT-TG distance while representing weight-bearing decreased the value compared to a diagnostic scan, likely by approximately 5 mm [26]. The peak TT-TG distance exceeded 15 mm for three knee models. The next three largest maximum TT-TG distance values were 15 mm, 13 mm, and 13 mm. For these three models, the patellar tendon attachment points on the tibia were lateralized to make the maximum TT-TG distance exceed 15 mm. The models were reconstructed from 5 females and 1 male. The average age was 26 years (range: 16 to 43 years).
Trochlear dysplasia and patella alta were also characterized for the knee models. The lateral trochlear inclination was measured with the knee at 0° of flexion, based on the maximum slope of the lateral ridge of the trochlear groove [15]. The Caton-Deschamps index was measured with the knee at 30° of flexion, based on the ratio of the distance from the distal point of the patellar articular surface to the anterior-superior point of the tibia to the length of the articular surface of the patella [15].
2.2. Tibial Tuberosity Anteromedialization and MPFL Reconstruction
Tibial tuberosity anteromedialization and MPFL reconstruction were simulated as the two patellar stabilization options. Tibial tuberosity anteromedialization was represented by shifting the patellar tendon attachment on the tibia medially by 10 mm and anteriorly by 5 mm with the knee extended, representing a tibial osteotomy with low obliquity common for patellar stabilization [11, 27]. The anteriorization component was applied to minimize pressure elevation related to tuberosity medialization [14]. For the MPFL graft, the femoral attachment was set at the Schöttle point [40], and the patellar attachment was positioned between the medial edge of the vastus medialis obliquus attachment and the medial edge of the patella. A dual strand gracilis tendon graft was represented by two springs with a total stiffness of 20 N/mm [38]. The grafts wrapped around the femoral condyle, with the portion from the femoral attachment to the wrapping surface represented by a rigid cylinder. To represent the patellar glide allowed intraoperatively [8, 37], the graft resting length was set at 30° of flexion while allowing 0.5 quadrants of patellar lateral translation. A quadrant represents one-quarter of the medial-lateral width of the patella. The graft tensioning approach has previously been shown to limit lateral maltracking without over constraining the patella during simulated knee function [16]. The combination of the two stabilization approaches was also simulated as a surgical option for each knee.
Patellar tracking was characterized based on bisect offset index (measure of lateral shift) and lateral patellar tilt. Bisect offset index and lateral patellar tilt were quantified at 5° intervals of knee flexion within a plane normal to the long axis of the patella with the posterior condylar axis of the femur oriented horizontally (Fig. 1C). The contact pressure distribution was characterized based on the lateral force percentage (contact force applied to the lateral facet of the patella divided by the total contact force) and the maximum pressure applied to cartilage on the medial and lateral facets of the patella. The pressure output was quantified from 15° to 90° of flexion, when the patella was constrained by the trochlear groove for all knees.
2.3. Statistical Analysis
Parameters of patellar tracking and contact pressure were compared between the pre-operative and three post-operative conditions with repeated measures analyses. The primary approach was repeated measures analysis of variance, with Student-Newman-Keuls post-hoc comparisons between each condition. A Greenhouse-Geisser correction was applied if the analysis failed a Mauchly test for sphericity (SPSS Statistics 24, IBM, Armonk, New York, United States). If a Shapiro-Wilk test indicated the residuals of the comparisons were not normally distributed, a Friedman test with a nonparametric version of Student-Newman-Keuls post-hoc tests was used. Statistical significance was set at P < 0.05.
3. Results
The average of the largest pre-operative TT-TG distance values during squatting was 18 mm (SD 2 mm). The mean Caton-Deschamps index at 30° was 1.2 (SD 0.2). The mean lateral trochlear inclination at 0° was 14° (SD 8°).
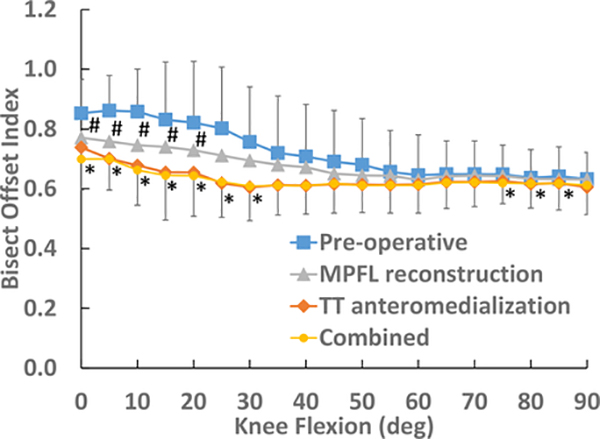
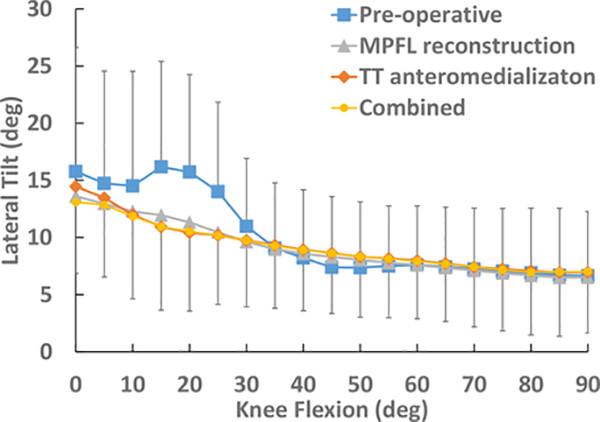
Tibial tuberosity anteromedialization and MPFL reconstruction both decreased lateral patellar maltracking, although tuberosity anteromedialization produced a larger decrease. The average pre-operative bisect offset index peaked at approximately 0.85 near full extension and decreased to approximately 0.65 by 60° of knee flexion (Fig. 2). The stabilization procedures decreased the average bisect offset to approximately 0.75 at full extension. The average bisect offset index decreased to approximately 0.60 by 30° of flexion for tuberosity anteromedialization compared to 60° for MPFL reconstruction. Multiple statistically significant differences between the conditions were identified near full extension and near 90° of flexion. Average pre-operative patellar tilt peaked at approximately 16° near full extension and decreased to approximately 8° by 45° of flexion (Fig. 3). The stabilization procedures did not significantly influence patellar tilt. Bisect offset index and patellar tilt for the combination of the two procedures were similar to the results for tibial tuberosity anteromedialization.
Fig. 2:
Average (SD) bisect offset index for the pre-operative and post-operative conditions. Data points for MPFL reconstruction (#) or tibial tuberosity (TT) anteromedialization and the combination of procedures (*) that are significantly lower than pre-operative data are marked. Data points for TT anteromedialization and the combination of procedures are also significantly lower than for MPFL reconstruction at 30° and 80° – 85°, with the combination of procedures also significantly lower than MPFL reconstruction at 75°.
Fig. 3:
Average (SD) lateral patellar tilt for the pre-operative and post-operative conditions. No significant differences were identified.
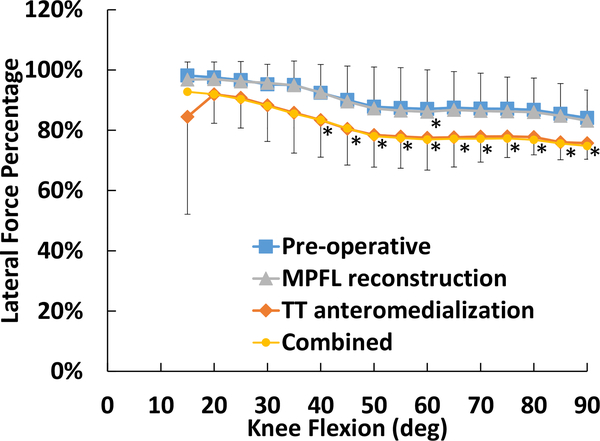
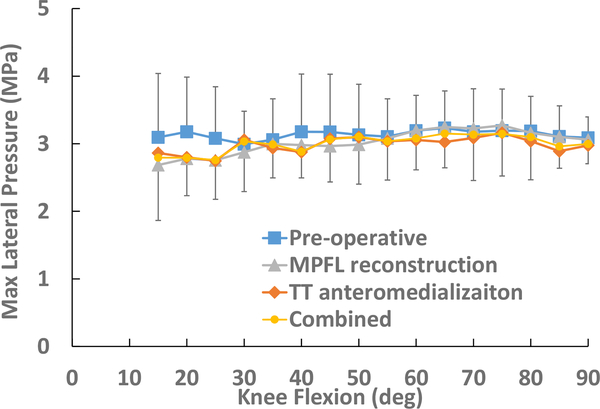
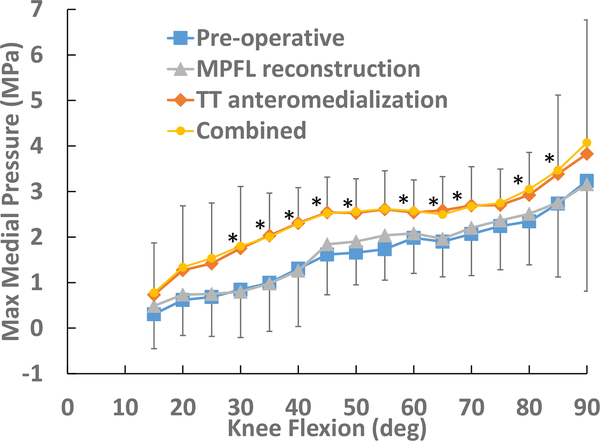
The primary change in the contact pressure distribution was tibial tuberosity anteromedialization shifting contact pressure from the lateral to the medial facet of the patella. The lateral force percentage was significantly lower for tibial tuberosity anteromedialization than the pre-operative and MPFL reconstruction conditions from 40°–90° of flexion (Fig. 4). The average maximum lateral pressure was on the order of 3 MPa throughout the full range of flexion for the pre-operative and post-operative conditions (Fig. 5). The average maximum medial pressure increased with knee flexion, peaking at approximately 3 MPa at 90° of flexion for the pre-operative condition (Fig. 6). Tibial tuberosity anteromedialization significantly increased the maximum medial pressure by 0.6 to 1.0 MPa from 30° to 85° of flexion, with the exception of 75°. Lateral force percentage and the maximum medial and lateral pressures for the combination of the two procedures were similar to tibial tuberosity anteromedialization.
Fig. 4:
Average (SD) lateral force percentage for the pre-operative and post-operative conditions. Data points for tibial tuberosity anteromedialization and the combination of procedures that are significantly lower than the other two conditions are marked (*). The combination of procedures was also significantly lower than tuberosity anteromedialization at 55°, and MPFL reconstruction was significantly lower than the pre-operative condition at 60°.
Fig. 5:
Average (SD) maximum lateral pressure for the pre-operative and post-operative conditions. No significant differences were identified.
Fig. 6:
Average (SD) maximum medial pressure for the pre-operative and post-operative conditions. Data points for tibial tuberosity anteromedialization and the combination of procedures that are significantly larger than the other two conditions are marked (*).
4. Discussion
The current results indicate that both tibial tuberosity anteromedialization and MPFL reconstruction decrease lateral patellar maltraking, while supporting the hypothesis that tuberosity anteromedialization decreases lateral patellar maltracking more than MPFL reconstruction. The simulated patellar stabilization procedures did not significantly influence lateral patellar tilt. The decrease in bisect offset index was greatest at low flexion angles. The average bisect offset index of 0.85 at full extension for the pre-operative condition is considered lateral maltracking, compared to approximately 0.75 for the post-operative conditions that is the cut-off between lateral maltracking and normal patellar tracking [46]. MPFL reconstruction only significantly decreased bisect offset index from 0° to 20° of flexion, while tuberosity anteromedialization significantly decreased bisect offset index over the majority of the flexion range. The lower bisect offset index for tuberosity anteromedialization than MPFL reconstruction over the flexion range that the patella becomes engaged with the trochlear groove likely indicates a lower risk of post-operative recurrent instability related to a malaligned tibial tuberosity.
The current results also support the hypothesis that tibial tuberosity anteromedialization elevates contact pressures applied to medial patellofemoral cartilage, while MPFL reconstruction has less influence on contact pressures. The medial shift in the contact pressure is a concern for knees with medial cartilage lesions related to patellar dislocation, which is common [30, 36]. The results are supported by clinical outcomes showing that tuberosity anteromedialization is less effective at improving outcomes for patients with medial cartilage lesions on the patella, in comparison to lateral lesions [33]. Therefore, the condition of the cartilage should be factored into treatment decisions when considering tuberosity anteromedialization. The medial shift in the contact force produced by tibial tuberosity anteromedialization could potentially be a benefit in the presence of lateral cartilage lesions, although these are less common than medial lesions [30, 36]. The medial shift did not significantly decrease the maximum lateral contact pressure, likely due in part to the vast majority of the contact force still being applied to the lateral facet after tibial tuberosity anteromedialization.
Previous studies utilizing in vitro simulation of function with cadaveric knees have shown that both MPFL reconstruction and tibial tuberosity anteromedialization decrease patellar lateral tracking [32, 39, 43–45]. Contrary to the current study, one previous study directly compared MPFL reconstruction to tibial tuberosity medialization, and indicated that MPFL reconstruction was more effective at stabilizing the patella than tuberosity medialization [31]. Another indicated that MPFL reconstruction could not restore normal patellar tracking for TT-TG distance values greater than 15 mm [43]. Contrary to the current study, previous in vitro studies have indicated that tuberosity medialization and anteromedialization decrease peak lateral contact pressures [35, 39, 45]. Similar to the current study, previous in vitro studies have indicated that tuberosity medialization and anteromedialization shift contact pressure medially and increase peak medial contact pressures [4, 39, 45]. Studies focused on MPFL reconstruction have primarily shown an increase in the maximum medial pressure only when the graft is over tensioned or the attachment site on the femur is poorly positioned [3, 32, 44]. The in vitro studies did not include pathologic anatomy associated with patellar instability, with lower lateral force percentage values in the pre-operative condition [39], likely contributing to some different trends for the current study than noted previously.
Previous computational simulation studies using models representing knees with patellar instability showed that both MPFL reconstruction and tibial tuberosity anteromedialization decrease lateral patellar maltracking [1, 14, 16, 17]. Previous studies also showed an increase in medial contact pressures for tuberosity anteromedialization [14], while MPFL reconstruction only increased medial contact pressures when the graft force was elevated due to an error in femoral attachment or setting the graft length [16, 17]. The previous computational studies did not directly compare MPFL reconstruction to tuberosity anteromedialization while representing a laterally malaligned tibial tuberosity for all knees, as done for the current study.
The current study utilized computational models with pathologic anatomy representative of knees with recurrent instability. Further, each knee model represented moderate lateral malalignment of the tibial tuberosity that would elevate the lateral force acting on the patella and make the knee a candidate for tibial tuberosity anteromedialization. A weak vastus medialis obliquus was also represented to elevate the resultant lateral force acting on the patella [18]. Due to development and validation of the models to represent knees during function, the TT-TG distance values were also measured during simulated knee function. In a clinical setting, the noted TT-TG distance would be larger in an unloaded condition, by approximately 5 mm [26], which is why the TT-TG distance was required to exceed 15 mm instead of the 20 mm cut-off more commonly noted for consideration of tuberosity anteromedialization [48]. Assessment of tibial tuberosity position based on the tibial tuberosity to posterior cruciate ligament attachment (TT-PCL) distance would have eliminated the influence of loading on the measurement [41]. Current surgical guidelines for tibial tuberosity medialization are primarily based on TT-TG distance, however [27, 34, 48]. Effectiveness of TT-PCL distance for identifying knees with initial and recurrent patellar instability has generally been inferior to TT-TG distance [9, 25, 47]. The models also included a mix of representation of trochlear dysplasia and patella alta. The average Caton-Deschamps index of 1.2 (SD 0.2) is on the borderline of values typically considered an indication of patella alta [28, 49]. The average lateral trochlear inclination measurement of 14° (8°) shows some knees would be considered to display trochlear dysplasia based on a cut-off value of 11° [2]. Representing pathologic anatomy produces a higher demand on the MPFL grafts and tibial tuberosity anteromedialization to correct patellar maltracking and preferentially alter the contact pressure distribution.
The current study focused on specific parameters of tuberosity realignment and MPFL reconstruction. Tuberosity medialization of 10 mm reduced the TT-TG distance into a recommended post-operative range, considering the difference between the unloaded and loaded TT-TG distance [11]. Anteriorization of 5 mm was added based on a previous simulation study showing lower elevation in medial contact pressures than for tuberosity medialization alone [14], but was conservative due to guidelines for knees with patella alta [11, 27]. MPFL reconstruction with 5 mm of allowed patellar glide was chosen based on a previous simulation study showing it to be the most restrictive MPFL graft tensioning protocol that did not elevate medial contact pressures [16]. The combination of MPFL reconstruction with tibial tuberosity anteromedialization resulted in minimal changes compared to tuberosity anteromedialization alone, due to anteromedialization decreasing lateral maltracking more than MPFL reconstruction so that the grafts were under relatively little tension. Release of the lateral retinaculum is also an option for combination with either procedure [11, 48], but was not performed to directly compare the two approaches. Regardless of the surgical parameters, the bone osteotomy needed for tuberosity anteromedialization complicates the surgical procedure and post-operative management compared to MPFL reconstruction. Further studies focused on identifying the optimal approach to maintain stability without overloading cartilage for patient-specific anatomy are warranted.
Limitations of the study should be noted. Several properties assigned to the models, such as the quadriceps force distribution and elastic properties and initial tension values for springs representing ligaments, tendons, and retinacular structures were assigned based on previously published data, emphasizing the importance of the validation against in vivo motion performed for each model. To achieve malalignment with the TT-TG distance exceeding 15 mm for six knees, the tibial tuberosity attachment position was modified for three knees. The original maximum TT-TG distance values were 13 mm, 13 mm, and 15 mm for these knees, so the applied changes were relatively small. The noted trends for patellar tracking and contact pressures did not vary between the three models that were manipulated and the other three models. The TT-TG distance was also characterized based on a loaded condition, instead of from unloaded imaging typically used for clinical assessment, due to setting the initial alignment at full extension and validating the models with application of muscle forces. Similar to previous studies [4, 39], tibial tuberosity anteromedialization was represented without changing the quadriceps force to account for an increased moment arm of the patellar tendon about the center of rotation of the knee. The study represented a simple squatting activity without representing external forces or more complex loading patterns likely to induce instability to allow for characterization of patellar tracking and patellofemoral contact pressures throughout the full range of flexion.
5. Conclusions
The simulations performed with knees being treated for recurrent instability with an elevated TT-TG distance indicate that both tibial tuberosity anteromedialization and MPFL reconstruction decrease lateral maltracking. The tuberosity anteromedialization procedure evaluated for the study provides the benefit of a larger decrease in maltracking at low flexion angles, which could facilitate the trochlear groove capturing the patella and preventing post-operative recurrent instability. The MPFL reconstruction procedure evaluated provides the advantage of a more favorable surgical technique and no elevation in pressure for cartilage on the medial facet of the patella. All of these factors should be considered when selecting a patellar stabilization approach for knees with malalignment of the tibial tuberosity.
Highlights.
Medial patellofemoral ligament reconstruction reduces lateral patellar maltracking
The decrease in lateral maltracking occurs in the presence of lateral malalignment
Tibial tuberosity anteromedialization produces a larger decrease in lateral tracking
Tibial tuberosity anteromedialization produces a medial shift in contact pressures
Acknowledgement
Research reported in this publication was supported by the National Institute Of Arthritis And Musculoskeletal And Skin Diseases of the National Institutes of Health under Award Number R21AR069150.
Dr. Elias received a research grant from NIH/NIAMS to conduct the study. Dr. Cosgarea reports textbook royalties from Elsevier and membership on the board of directors of the Patellofemoral Foundation. Dr. Tanaka is a committee member for the American Academy of Orthopedic Surgeons and the International Society of Arthroscopy Knee Surgery and Orthopaedic Sports Medicine, on the electronic media editorial board for the American Journal of Sports Medicine, and on the editorial board for the Arthroscopy Journal. Dr. Jones has no potential conflicts of interest to declare.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Alvarez O, Steensen RN, Rullkoetter PJ, Fitzpatrick CK. Computational approach to correcting joint instability in patients with recurrent patellar dislocation. J Orthop Res. 2019. [Epub ahead of print] 10.1002/jor.24526. [DOI] [PubMed] [Google Scholar]
- 2.Batailler C, Neyret P. Trochlear dysplasia: imaging and treatment options. EFORT Open Rev. 2018;3(5):240–247. 10.1302/2058-5241.3.170058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beck P, Brown NA, Greis PE, Burks RT. Patellofemoral contact pressures and lateral patellar translation after medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(9):1557–63. 10.1177/0363546507300872. [DOI] [PubMed] [Google Scholar]
- 4.Beck PR, Thomas AL, Farr J, Lewis PB, Cole BJ. Trochlear contact pressures after anteromedialization of the tibial tubercle. Am J Sports Med. 2005;33(11):1710–5. 10.1177/0363546505278300. [DOI] [PubMed] [Google Scholar]
- 5.Besier TF, Gold GE, Delp SL, Fredericson M, Beaupré GS. The influence of femoral internal and external rotation on cartilage stresses within the patellofemoral joint. J Orthop Res. 2008;26(12):1627–35. 10.1002/jor.20663. [DOI] [PubMed] [Google Scholar]
- 6.Biyani R, Elias JJ, Saranathan A, Feng H, Guseila LM, Morscher MA, Jones KC. Anatomical factors influencing patellar tracking in the unstable patellofemoral joint. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2334–41. 10.1007/s00167-014-3195-y. [DOI] [PubMed] [Google Scholar]
- 7.Blankevoort L, Kuiper JH, Huiskes R, Grootenboer HJ. Articular contact in a three-dimensional model of the knee. J Biomech. 1991;24(11):1019–1031. 10.1016/0021-9290(91)90019-j. [DOI] [PubMed] [Google Scholar]
- 8.Camp CL, Krych AJ, Dahm DL, Levy BA, Stuart MJ. Medial patellofemoral ligament repair for recurrent patellar dislocation. Am J Sports Med. 2010;38(11):2248–54. doi: 10.1177/0363546510376230. [DOI] [PubMed] [Google Scholar]
- 9.Clifton B, Richter DL, Tandberg D, Ferguson M, Treme G. Evaluation of the Tibial Tubercle to Posterior Cruciate Ligament Distance in a Pediatric Patient Population. J Pediatr Orthop. 2017;37(6):e388–e393. 10.1097/BPO.0000000000001035. [DOI] [PubMed] [Google Scholar]
- 10.Conlan T, Garth WP Jr, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75(5):682–693. 10.2106/00004623-199305000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Duchman K, Bollier M. Distal realignment: indications, technique, and results. Clin Sports Med. 2014;33(3):517–30. 10.1016/j.csm.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 12.Elias JJ, Carrino JA, Saranathan A, Guseila LM, Tanaka MJ, Cosgarea AJ. Variations in kinematics and function following patellar stabilization including tibial tuberosity realignment. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2350–6. 10.1007/s00167-014-2905-9. [DOI] [PubMed] [Google Scholar]
- 13.Elias JJ, Faust AF, Chu YH, Chao EY, Cosgarea AJ. The soleus muscle acts as an agonist for the anterior cruciate ligament. An in vitro experimental study. Am J Sports Med 2003;31(2):241–6. 10.1177/03635465030310021401. [DOI] [PubMed] [Google Scholar]
- 14.Elias JJ, Jones KC, Copa AJ, Cosgarea AJ. Computational simulation of medial versus anteromedial tibial tuberosity transfer for patellar instability. J Orthop Res. 2018;36(12):3231–3238. 10.1002/jor.24108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Elias JJ, Jones KC, Cyrus Rezvanifar S, Gabra JN, Morscher MA, Cosgarea AJ. Dynamic tracking influenced by anatomy following medial patellofemoral ligament reconstruction: Computational simulation. Knee. 2018;25(2):262–270. 10.1016/j.knee.2018.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Elias JJ, Jones KC, Lalonde MK, Gabra JN, Rezvanifar SC, Cosgarea AJ. Allowing one quadrant of patellar lateral translation during medial patellofemoral ligament reconstruction successfully limits maltracking without overconstraining the patella. Knee Surg Sports Traumatol Arthrosc. 2018;26(10):2883–2890. 10.1007/s00167-017-4799-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Elias JJ, Kelly MJ, Smith KE, Gall KA, Farr J. Dynamic Simulation of the Effects of Graft Fixation Errors During Medial Patellofemoral Ligament Reconstruction. Orthop J Sports Med. 2016;4(9):2325967116665080 10.1177/2325967116665080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Elias JJ, Kilambi S, Goerke DR, Cosgarea AJ. Improving vastus medialis obliquus function reduces pressure applied to lateral patellofemoral cartilage. J Orthop Res. 2009;27(5):578–83. 10.1002/jor.20791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elias JJ, Saranathan A. Discrete element analysis for characterizing the patellofemoral pressure distribution: model evaluation. J Biomech Eng. 2013;135(8):81011. doi: 10.1115/1.4024287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Erickson BJ, Nguyen J, Gasik K, Gruber S, Brady J, Shubin Stein BE. Isolated Medial Patellofemoral Ligament Reconstruction for Patellar Instability Regardless of Tibial Tubercle-Trochlear Groove Distance and Patellar Height: Outcomes at 1 and 2 Years. Am J Sports Med. 2019;47(6):1331–1337. 10.1177/0363546519835800. [DOI] [PubMed] [Google Scholar]
- 21.Fürmetz J, Sass J, Ferreira T, Jalali J, Kovacs L, Mück F, Degen N, Thaller PH. Three-dimensional assessment of lower limb alignment: Accuracy and reliability. Knee. 2019;26(1):185–193. 10.1016/j.knee.2018.10.011. [DOI] [PubMed] [Google Scholar]
- 22.Gao B, Dwivedi S, Fabricant PD, Cruz AI Jr. Patterns in Outcomes Reporting of Operatively Managed Pediatric Patellofemoral Instability: A Systematic Review and Meta-analysis. Am J Sports Med. 2019;47(6):1516–1524. 10.1177/0363546518765152. [DOI] [PubMed] [Google Scholar]
- 23.Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng 1983;105(2):136–144. 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- 24.Guess TM, Liu H, Bhashyam S, Thiagarajan G. A multibody knee model with discrete cartilage prediction of tibio-femoral contact mechanics. Comput Methods Biomech Biomed Engin 2013;16(3):256–70. 10.1080/10255842.2011.617004. [DOI] [PubMed] [Google Scholar]
- 25.Heidenreich MJ, Camp CL, Dahm DL, Stuart MJ, Levy BA, Krych AJ. The contribution of the tibial tubercle to patellar instability: analysis of tibial tubercle-trochlear groove (TT-TG) and tibial tubercle-posterior cruciate ligament (TT-PCL) distances. Knee Surg Sports Traumatol Arthrosc. 2017;25(8):2347–2351. 10.1007/s00167-015-3715-4. [DOI] [PubMed] [Google Scholar]
- 26.Izadpanah K, Weitzel E, Vicari M, Hennig J, Weigel M, Südkamp NP, Niemeyer P. Influence of knee flexion angle and weight bearing on the Tibial Tuberosity-Trochlear Groove (TT-TG) distance for evaluation of patellofemoral alignment. Knee Surg Sports Traumatol Arthrosc. 2014;22(11):2655–61. 10.1007/s00167-013-2537-5. [DOI] [PubMed] [Google Scholar]
- 27.Liu JN, Steinhaus ME, Kalbian IL, Post WR, Green DW, Strickland SM, Shubin Stein BE. Patellar Instability Management: A Survey of the International Patellofemoral Study Group. Am J Sports Med. 2018;46(13):3299–3306. 10.1177/0363546517732045. [DOI] [PubMed] [Google Scholar]
- 28.Magnussen RA, De Simone V, Lustig S, Neyret P, Flanigan DC. Treatment of patella alta in patients with episodic patellar dislocation: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2014;22(10):2545–50. 10.1007/s00167-013-2445-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Makhsous M, Lin F, Koh JL, Nuber GW, Zhang LQ. In vivo and noninvasive load sharing among the vasti in patellar malalignment. Med Sci Sports Exerc. 2004;36(10):1768–75. 10.1249/01.MSS.0000142302.54730.7F. [DOI] [PubMed] [Google Scholar]
- 30.Nomura E, Inoue M. Cartilage lesions of the patella in recurrent patellar dislocation. Am J Sports Med. 2004;32(2):498–502. 10.1177/0095399703258677. [DOI] [PubMed] [Google Scholar]
- 31.Ostermeier S, Stukenborg-Colsman C, Hurschler C, Wirth CJ. In vitro investigation of the effect of medial patellofemoral ligament reconstruction and medial tibial tuberosity transfer on lateral patellar stability. Arthroscopy. 2006;22(3):308–19. 10.1016/j.arthro.2005.09.024. [DOI] [PubMed] [Google Scholar]
- 32.Philippot R, Boyer B, Testa R, Farizon F, Moyen B. Study of patellar kinematics after reconstruction of the medial patellofemoral ligament. Clin Biomech. 2012;27(1):22–6. 10.1016/j.clinbiomech.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 33.Pidoriano AJ, Weinstein RN, Buuck DA, Fulkerson JP. Correlation of patellar articular lesions with results from anteromedial tibial tubercle transfer. Am J Sports Med 1997;25(4):533–7. 10.1177/036354659702500417. [DOI] [PubMed] [Google Scholar]
- 34.Post WR, Fithian DC. Patellofemoral instability: A consensus statement from the AOSSM/PFF Patellofemoral Instability Workshop. Orthop J Sports Med. 2018;6(1):2325967117750352 10.1177/2325967117750352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ramappa AJ, Apreleva M, Harrold FR, Fitzgibbons PG, Wilson DR, Gill TJ. 2006. The effects of medialization and anteromedialization of the tibial tubercle on patellofemoral mechanics and kinematics. Am J Sports Med. 2006;34(5):749–56. 10.1177/0363546505283460. [DOI] [PubMed] [Google Scholar]
- 36.Salonen EE, Magga T, Sillanpää PJ, Kiekara T, Mäenpää H, Mattila VM. Traumatic Patellar Dislocation and Cartilage Injury: A Follow-up Study of Long-Term Cartilage Deterioration. Am J Sports Med. 2017;45(6):1376–1382. 10.1177/0363546516687549. [DOI] [PubMed] [Google Scholar]
- 37.Sampatacos NE, Getelman MH. Medial patellofemoral ligament reconstruction using a modified “reverse-loop” technique. Arthrosc Tech. 2013;2(2):e175–81. https://10.1016/j.eats.2013.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Saper MG, Meijer K, Winnier S, Popovich J Jr, Andrews JR, Roth C. Biomechanical Evaluation of Classic Solid and All-Soft Suture Anchors for Medial Patellofemoral Ligament Reconstruction. Am J Sports Med. 2017;45(7):1622–1626. 10.1177/0363546517691951. [DOI] [PubMed] [Google Scholar]
- 39.Saranathan A, Kirkpatrick MS, Mani S, Smith LG, Cosgarea AJ, Tan JS, Elias JJ. The effect of tibial tuberosity realignment procedures on the patellofemoral pressure distribution. Knee Surg Sports Traumatol Arthrosc. 2012;20(10):2054–61. 10.1007/s00167-011-1802-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schöttle PB, Schmeling A, Rosenstiel N, Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35(5):801–4. 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
- 41.Seitlinger G, Scheurecker G, Högler R, Labey L, Innocenti B, Hofmann S. Tibial tubercle-posterior cruciate ligament distance: a new measurement to define the position of the tibial tubercle in patients with patellar dislocation. Am J Sports Med. 2012;40(5):1119–25. 10.1177/0363546512438762. [DOI] [PubMed] [Google Scholar]
- 42.Shin CS, Chaudhari AM, Andriacchi TP. The influence of deceleration forces on ACL strain during single-leg landing: a simulation study. J Biomech. 2007;40(5):1145–52. 10.1016/j.jbiomech.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 43.Stephen JM, Dodds AL, Lumpaopong P, Kader D, Williams A, Amis AA. The ability of medial patellofemoral ligament reconstruction to correct patellar kinematics and contact mechanics in the presence of a lateralized tibial tubercle. Am J Sports Med. 2015;43(9):2198–2207. 10.1177/0363546515597906. [DOI] [PubMed] [Google Scholar]
- 44.Stephen JM, Kittl C, Williams A, Zaffagnini S, Marcheggiani Muccioli GM, Fink C, Amis AA. Effect of Medial Patellofemoral Ligament Reconstruction Method on Patellofemoral Contact Pressures and Kinematics. Am J Sports Med. 2016;44(5):1186–94. 10.1177/0363546516631736. [DOI] [PubMed] [Google Scholar]
- 45.Stephen JM, Lumpaopong P, Dodds AL, Williams A, Amis AA. The effect of tibial tuberosity medialization and lateralization on patellofemoral joint kinematics, contact mechanics, and stability. Am J Sports Med. 2015;43(1):186–94. 10.1177/0363546514554553. [DOI] [PubMed] [Google Scholar]
- 46.Tanaka MJ, Elias JJ, Williams AA, Demehri S, Cosgarea AJ. Characterization of patellar maltracking using dynamic kinematic CT imaging in patients with patellar instability. Knee Surg Sports Traumatol Arthrosc. 2016;24(11):3634–3641. 10.1007/s00167-016-4216-9. [DOI] [PubMed] [Google Scholar]
- 47.Tensho K, Shimodaira H, Akaoka Y, Koyama S, Hatanaka D, Ikegami S, Kato H, Saito N. Lateralization of the Tibial Tubercle in Recurrent Patellar Dislocation: Verification Using Multiple Methods to Evaluate the Tibial Tubercle. J Bone Joint Surg Am. 2018;100(9):e58 10.2106/JBJS.17.00863. [DOI] [PubMed] [Google Scholar]
- 48.Weber AE, Nathani A, Dines JS, Allen AA, Shubin-Stein BE, Arendt EA, Bedi A. An Algorithmic Approach to the Management of Recurrent Lateral Patellar Dislocation. J Bone Joint Surg Am. 2016;98(5):417–27. 10.2106/JBJS.O.00354. [DOI] [PubMed] [Google Scholar]
- 49.Woodmass JM, Johnson NR, Cates RA, Krych AJ, Stuart MJ, Dahm DL. Medial Patellofemoral Ligament Reconstruction Reduces Radiographic Measures of Patella Alta in Adults. Orthop J Sports Med. 2018;6(1):2325967117751659 10.1177/2325967117751659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhang LQ, Wang G, Nuber GW, Press JM, Koh JL. In vivo load sharing among the quadriceps components. J Orthop Res. 2003;21(3):565–71. 10.1016/S0736-0266(02)00196-1. [DOI] [PubMed] [Google Scholar]