Abstract
The present study was designed to determine the association between the genetic polymorphisms/expression variations of RB1 and CCND1 genes and brain tumor risk. For this purpose, 250 blood samples of brain tumor patients along with 250 controls (cohort I) and 96 brain tumor tissues (cohort II) with adjacent control section were collected. Mutation analysis of RB1 (rs137853294, rs121913300) and CCND1 (rs614367, rs498136) genes was performed using ARMS-PCR followed by sequencing, and expression analysis was performed using real-time PCR and immunohistochemistry. The results showed homozygous mutant genotype of RB1 gene polymorphism, rs121913300 (P=0.003) and CCND1 gene polymorphism rs614367 (P=0.01) were associated significantly with brain tumor risk. Moreover, significant down-regulation of RB1 (P=0.005) and up-regulation of CCND1 (P=0.0001) gene was observed in brain tumor sections vs controls. Spearman correlation showed significant negative correlation between RB1 vs proliferation marker, Ki-67 (r = −0.291*, P<0.05) in brain tumors. Expression levels of selected genes were also assessed at protein level using immunohistochemical analysis (IHC) and signification down-regulation of RB1 (P=0.0001) and up-regulation of CCND1 (P=0.0001) was observed in brain tumor compared with control sections. In conclusion, it is suggested that polymorphisms/expression variations of RB1 and CCND1 genes may be associated with increased risk of brain tumor.
Keywords: Brain tumor, CCND1, Expression analysis, Polymorphism, RB1
Introduction
Brain cancer develops in brain or in spinal cord and is categorized into different types on the basis of their location and origin such as glioma, meningioma, pituitary adenomas, medulloblastoma and schwannoma [1]. Among these types, glioma also referred to as tumors of glial cells, are the most common type of primary brain tumors [2]. Gliomas are further classified into various categories as per their morphological appearance which includes astrocytomas, oligodendrogliomas, ependymomas and glioblastomas. According to World Health Organization (WHO) 2007 classification, gliomas are classified into four categories namely grades I, II, III and IV which are decided on the basis of severity [3,4]. Regardless of advancements in therapeutical procedures like radiotherapy, chemotherapy and surgical removal, the prognosis and survival of patients (especially glioblastoma) is still lacking [5,6]. Therefore, it is significant to illuminate the exact molecular cause of glioma/brain tumor, which may possibly support in the diagnosis and prognosis of brain tumor patients. Radiation exposure to head and inherited syndromes (which are rare) are among the established risk factors of brain tumorigenesis [7]. The exact molecular mechanism of these risk factors to increase the risk of tumor development in brain is still unknown. Nevertheless, it has been observed that radiation disturbs the G1/S and S phases of the cell cycle pathway and ultimately resulted in increased proliferation and tumorigenesis.
G1/S transition phase defines the fate of the cell based on the proliferation or apoptotic signals. Genes which are involved in the transition of G1/S phase transition are cyclin-dependent kinases, cyclins and retinoblastoma 1 gene [8–10]. RB1 gene confines the cell in gap phase in absence of proliferation signals. Activated pRB protein binds with E2F transcription factor and halt transcription mechanism. RB1/E2F complex suppresses the transcription in quiescent cells [11]. Any polymorphism or expression variation in RB1 gene may disrupt the transition of cell cycle phases. RB1 gene is found to be mutated in many cancers including brain tumor [12]. Selected polymorphisms of RB1 gene rs137853294 and rs121913300 are exonic single nucleotide nucleotides (SNPs). These SNPs result in aberrant mRNA structure and protein of RB1 gene in breast cancer patients [13].
Another important cell cycle pathway gene is CCND1, which forms a complex with CDK4 and initiates the transition of gap phase into synthesis phase. CCND/CDK complex inactivates pRb protein through phosphorylation resulting E2F transcription factor starts progression of cell from G-phase to S-phase [14]. Any mutation in proto-oncogene CCND1 may lead to carcinogenesis through abnormal cell proliferation of cell. Its expression also varies most of the cancers including brain tumor [15]. CCND1 polymorphisms rs614367 and rs498136 are intergenic SNPs which affects the regulation and expression of CCND1 gene in breast cancer and malignant melanoma, respectively [16,17].
A number of studies have been published for expression analysis of RB1 and CCND1 in different cancers including brain cancer. However, till now, no study has been reported to screen out the hotspot polymorphisms of RB1 and CCND1 genes along with expression variations of respective genes in brain tumor and different subtypes of brain tumor. Present study was designed to find out whether the polymorphisms or expressional variation in the RB1 and CCND1 genes can modify the risk for brain tumor, and if the effects of these polymorphisms differ in different pathological parameters of brain tumor patients.
Materials and methods
Specimen collection
Ethical board of both COMSATS Institute of Information Technology and collaborating hospital approved the proposal of present study. Two study cohorts of brain tumors were patients enrolled in present study. Study cohort I consisted of 250 blood samples of brain tumor patients and 250 age and sex matched controls. Selection criteria for patients included in cohort 1 comprised confirmed histological diagnosis of brain tumor, no preoperative therapy and availability of complete follow-up data. However, no restrictions related to histological subtypes of primary brain tumors were applied. Different subtypes such as anaplastic astrocytoma, anaplastic oligodendroglioma, anaplastic meningioma, meningioma, diffuse astrocytoma, choroid glioma, oligodendroglioma, eppendoma, atypical meningioma, GBM, diffuse medine glioma and pituitary adenomas were included in the present study. Inclusion criterion for controls included absence of prior history of cancer or precancerous lesions. Patients and controls suffering from any other familial disease (diabetes, blood pressure and cardiovascular impairment) were excluded from the present study. Cohort I was used for screening of hotspot polymorphisms of RB1 and CCND1 genes in brain tumor patients. Study cohort II consisted of 96 brain tumor tissues along with adjacent uninvolved healthy area used as controls. Samples of tumor core, the invasive edge of tumor and microscopically healthy mucosa (control) were obtained from each surgical section and stored in RNA at −80°C. Presence of tumor cells in the collected tissues was rectified by examination of frozen sections following Hematoxylin and Eosin stain (HE stain) by a consultant pathologist. Whereas, samples of control were obtained from macroscopically confirmed (by a pathologist) uninvolved healthy area more than 2 cm away from the tumor. Cohort II was used for the expression analysis of RB1 and CCND1 gene using the quantitative real-time PCR technique. Both brain tumor cohorts were collected after taking the consent from patients from Department of Neurosurgery, Pakistan Institute of Medical and Health Sciences (PIMS) Hospital in during 2015–2017. After obtaining informed consent, all individuals were personally interviewed using the specifically designed questionnaire. Information on age, gender, ethnic group and detailed exposure data on smoking was recorded.
RNA and DNA extraction
Blood samples of cohort I were collected in ETDA vacutainers. DNA was extracted from blood samples through phenol-chloroform method [18]. DNA samples were stored in TE buffer at 4°C for further mutation analysis. In case of cohort II, tumor samples were collected in 15-ml Eppendorf tube containing RNA later solution. RNA was extracted from fresh tissue samples of both tumor and control through TRIzol method [19]. Extracted RNA was stored in DEPC at −20°C for expression analysis of selected genes. Extracted RNA and DNA were visualized and confirmed by performing 1% agarose gel electrophoresis.
Polymorphism screening and sequencing
Polymorphisms for RB1 and CCND1 gene were selected from dbSNP database. The SNP selection criteria were based on minor allele frequency (MAF) > 0.05. The selected SNPs included rs137853294, rs121913300 for RB1, rs614367 and rs498136 for CCND1.
Genotyping was performed by the amplification-refractory mutation system polymerase chain reaction (ARMS-PCR). Primers for PCR amplification were designed using WASP (web-based allele specific primer designing tool) and purchased from Macrogen (Korea). Primers specific for each polymorphism are given in Table 1. PCR was performed in a reaction volume of 10 μl containing 50–100 ng genomic DNA, 100 μM of each primers and Solis BioDyne Master Mix. The thermal cycling protocol used was: 94°C for 5 min and 35 cycles at 94°C for 30 s, optimized annealing temperature for 45 s, 72°C for 1 min and final extension for 10 min. The PCR products were visualized on a 2% agarose gel electrophoresis (100 V, 300 A for 45 min). Presence or absence of expected product size bands, specific for wild or mutant primers, were evaluated using UV transilluminator (Gel Doc Bio-Rad, U.S.A.). β-Actin was used as internal control in each reaction. PCR products with homozygous wild, homozygous mutant and heterozygous mutant genotypes were further confirmed by DNA sequence analysis
Table 1. Primer sequence of RB1 and CCND1 genes.
| Primer name | Primer sequence | Product size |
|---|---|---|
| Primers specific for real-time PCR | ||
| CCND1 F | CCTCGGTGTCCTACTTCAAATG (sense) | 100 bp |
| CCND1 R | CACTTCTGTTCCTCGCAGAC (antisense) | |
| RB1 F | GCAGTATGCTTCCACCAG (sense) | 108 bp |
| RB1 R | TAGATGTTCCCTCCAGGAAT (antisense) | |
| Primers specific for ARMS-PCR | ||
| RB1 first SNP | ||
| RB1 rs137853294 FI (T allele) | CAGTGTATCGGCTAGCCTATCGCT | 188 bp |
| RB1 rs137853294 RI (C allele) | AAGCGTTCACAAAGTGTATTTAGACG | 257 bp |
| RB1 rs137853294 FO (5′–3′) | TGCATTTCTTCATCTGTATCCCTTGT | 394 bp |
| RB1 rs137853294 RO (5′–3′) | GTAGGGAGGAGAGAAGGTGAAGTGC | |
| RB1 second SNP | ||
| RB1 rs121913300 FI (T allele) | AAGGTTGAAAATCTTTCTACAT | 150 bp |
| RB1 rs121913300 RI (C allele) | AGATAAATTTCTTCGTAGCG | 214 bp |
| RB1 rs121913300 FO (5′–3′) | CAATTTTCTGTACCTCACTTT | 322 bp |
| RB1 rs121913300 RO (5′–3′) | CTAAAGCAAATCAATCAAATAT | |
| CCND1 first SNP | ||
| CCND1 rs614367 FI (T allele) | TTGGCTTCTCTGCAACGCT | 214 bp |
| CCND1 rs614367 RI (C allele) | GGGGCCTAAAGAGATGTAATTCG | 293 bp |
| CCND1 rs614367 FO (5′–3′) | TTACATAGAAGGGGGTGAGCCA | 465 bp |
| CCND1 rs614367 RO (5′–3′) | TGTTCTGTCCATTGTCCAGCAT | |
| CCND1 second SNP | ||
| CCND1 rs498136 FI (T allele): | CATTATTGTGCTTCTCAACGGT | 153 bp |
| CCND1 rs498136 RI (G allele) | AAACTCTTAAGTTTCACTGTTTGGTC | 103 bp |
| CCND1 rs498136 FO (5′–3′) | CTGCCAGAGGACTTAGAAAGTG | 208 bp |
| CCND1 rs498136 RO (5′–3′) | TAGACATGGAAAATATTCACGACA | |
Expression analysis
Expression variation of RB1, CCND1 and Ki-67 genes was analyzed by performing quantitative real-time PCR technique. cDNA was synthesized and confirmed by amplification of β-actin which was taken as endogenous control. Primers were designed for β-actin, RB1, CCND1 and Ki-67 genes by IDT software for real-time PCR to estimate the relative expression of these genes in control and tumor samples.
Each qPCR was performed in a 20-μl reaction mixture containing ∼1 μl of product from RT reaction, 10 μl of 2× SYBR Green, 1 μl of each primer and 7 μl of RNase-free water. qPCR was performed using Real-Time PCR system (Applied Biosystems Step One Plus) under standard conditions. The relative mRNA levels of RB1, CCND1, Ki-67 and β-actin were computed using the 2−ΔΔCt analysis method [19]. Melt curve analysis of selected genes was also performed to detect the heterogeneity in brain tumor cohort and specificity or qPCR [20].
Immunohistochemistry
Immunohistochemical analysis (IHC) was performed using the DAB kit (Sigma). Paraffin-embedded sections of brain tumor sections and adjacent uninvolved control sections were used for the present study after deparaffinization and rehydration steps using xylene and ethanol respectively, as described previously [21]. Sections were incubated for 1 h with mouse anti-RB1 (Novus Biologicals, at a dilution of 1:1000), mouse anti-CCND1 (Novus Biologicals, at a dilution of 1:1000) and mouse anti-Ki-67 (Novus Biologicals, at a dilution of 1:1000). Species-specific secondary antibody (Novus Biologicals) was also used for each selected gene. Additionally, negative controls were prepared using the same procedure except that the primary antibodies were replaced with PBS. Negative controls were used for assessment of specificity of this current assay [21].
The relative intensities of the completed immunohistochemical reactions were also evaluated using light microscopy by three independently trained observers, unaware of the clinical data. Tumor cells were counted randomly in ten high power fields for measurement of immunoreactivity. The following formula was used for the evaluation of immunoreactivity:
Structure prediction
Centroid secondary structure of mRNA of wild-type RB1 transcript and its selected exonic SNPS were designed by dot block model using Veinna RNA Web Services software. Furthermore, protein structure of normal pRB and mutated pRB were predicted using SWISS-MODEL software.
Statistical analysis
Statistical analysis was performed using MedCalc statistical software and GraphPad Prism (5.03) software. Comparison between the expected and actual genotypes was done using Hardy–Weinberg equilibrium test. Chi-square tests was applied to estimate the difference in genotypes and allele frequencies between patients and control individuals. Odds ratio (ORs) and 95% confidence intervals (CIs) were assessed through logistic regression. This predictive analysis was performed with respect to demographic features, smoking status, family history, tumor types and grading. SNPs analysis and their multiplicative interactions were also calculated by three genetic models (additive, dominant and recessive) and logistic regression model, respectively. P-value <0.05 represents the statistically significant difference between patients and controls. Genotyped data of SNPs were used to design their haplotypes using Haploview 4.2 software. Linkage disequilibrium (LD) between all selected SNPs was determined through expectation maximization (EM) algorithm.
For cohort II, Chi-square tests and one-way analysis of variance was used to assess the association of RB1 and CCND1 gene expression with clinical and histopathological parameters. Spearman correlation coefficient was used to assess correlations among the gene expression and clinical and histopathological parameters.
Results
Retrospective cohort study
In study cohort I, 250 brain tumor patients and 250 control individuals were examined for four selected SNPs including rs137853294, rs121913300 (RB1), rs614367 and rs498136 (CCND1). In study cohort II, 96 brain tumor tissues and 96 healthy tissues were analyzed for the expression variation of RB1 and CCND1 genes. Demographic features of the study cohort are given in Table 2.
Table 2. Demographic parameters of brain tumor cases and controls.
| Variables | Cases (n=250) | Controls (n=250) | Tumor tissues (n=96) |
|---|---|---|---|
| Age (years) | |||
| Median (range) | 42 (8–88) | 47 (9–88) | 45 (21–71) |
| Age | |||
| ≤30 | 62 (24.8%) | 49 (19.6%) | 12 (12.5%) |
| >30 | 188 (75.2%) | 201 (80.4%) | 84 (87.5%) |
| Gender | |||
| Males | 165 (66%) | 172 (68.8%) | 59 (61.5%) |
| Females | 85 (34%) | 78 (31.2%) | 37 (38.5%) |
| Smoking | |||
| Smokers | 83 (33.2%) | 120 (48%) | 44 (46%) |
| Non-smokers | 167 (66.8%) | 130 (52%) | 52 (54%) |
| Family history | |||
| Positive | 26 (10.4%) | - | 13 (14%) |
| Negative | 224 (89.6%) | - | 83 (86%) |
| Brain tumor types | |||
|
Glioma Diffuse astrocytoma (II) Anaplastic astrocytoma (III) Choroid glioma (II) Oligodandroglioma (II) Anaplastic oligodandroglioma (III) GBM (IV) Diffuse medine glioma (IV) Eppendoma (II) |
170 (68%) 35 64 25 06 04 27 06 03 |
- | 68 (70.8%) 07 19 12 05 03 11 04 07 |
|
Meningioma Meningioma (I) Atypical meningioma (II) Anaplastic meningioma (III) |
64 (25.6%) 21 30 13 |
- | 21 (21.9%) 09 08 04 |
|
Pituitary adenoma Grade II Grade III |
16 (6.4%) 09 07 |
- | 07 (7.3%) 04 03 |
| Tumor grade | |||
| Grade I | 21 | 09 | |
| Grade II | 108 | 43 | |
| Grade III | 88 | 29 | |
| Grade IV | 33 | 15 | |
| Ionizing radiation | |||
| Exposed | 24 (9.6%) | - | 16 (16.7%) |
| Unexposed | 226 (90.4%) | - | 80 (83.3%) |
Genotype and allele frequencies of RB1 and CCND1 SNPs
Genotype and allele frequencies of RB1 polymorphisms are mentioned in Table 3. RB1 polymorphism rs137853294 showed significantly higher frequency of heterozygous mutant genotype (OR, 1.49; 95% CI, 1.02–2.16; P=0.04) in patients as compared with controls. Mutant allele (T) frequency of rs137853294 was significantly higher (OR, 1.50; 95% CI, 1.11–2.01; P=0.007) in tumor patients as compared with control individuals. In case of rs121913300 RB1 polymorphism, ∼20.48-fold increased risk of brain tumor was associated with homozygous mutant genotype (OR, 20.48; 95% CI, 2.72–154.21; P=0.003) in tumor patients. Moreover, significantly higher frequency of heterozygous mutant genotype (OR, 1.68; 95% CI, 1.05–2.66; P=0.03) and mutant T allele (OR, 1.56; 95% CI, 1.22–2.01; P=0.0005) was observed in sampled tumor patients as compared with controls.
Table 3. Genotypes and allele frequency of selected SNPs of RB1 and CCND1 in brain tumor patients.
| Genotype/Allele | Cases, n (%) | Controls, n (%) | OR (95% CI) | P-value |
|---|---|---|---|---|
| RB1 gene | ||||
| rs137853294 | ||||
| CC | 135 (54%) | 164 (65.6%) | 1 | 1 |
| CT | 95 (38%) | 73 (29.2%) | 1.49 (1.02–2.16) | 0.04* |
| TT | 20 (8%) | 13 (5.2%) | 1.60 (0.77–3.26) | 0.21 |
| C allele frequency | 365 (73%) | 401 (80.2%) | 1 | 1 |
| T allele frequency | 135 (27%) | 99 (19.8%) | 1.50 (1.11–2.01) | 0.007† |
| rs121913300 | ||||
| CC | 17 (6.8%) | 54 (21.6%) | 1 | 1 |
| CT | 214 (85.6%) | 195 (78%) | 1.68 (1.05–2.66) | 0.03* |
| TT | 19 (7.6%) | 1 (0.4%) | 20.48 (2.72–154.21) | 0.003† |
| C allele frequency | 248 (49.6%) | 303 (60.6%) | 1 | 1 |
| T allele frequency | 252 (50.4%) | 197 (39.4%) | 1.56 (1.22–2.01) | 0.0005‡ |
| CCND1 gene | ||||
| rs614367 | ||||
| CC | 119 (47.6%) | 154 (61.6%) | 1 | 1 |
| CT | 117 (46.8%) | 93 (37.2%) | 1.48 (1.04–2.12) | 0.03* |
| TT | 14 (5.6%) | 3 (1.2%) | 4.88 (1.39–17.21) | 0.01* |
| C allele frequency | 355 (71%) | 401 (80.2%) | 1 | 1 |
| T allele frequency | 145 (29%) | 99 (19.8%) | 1.65 (1.23–2.22) | 0.0007‡ |
| rs498136 | ||||
| GG | 85 (34%) | 104 (41.6%) | 1 | 1 |
| GT | 157 (62.8%) | 145 (58%) | 1.22 (0.85–1.75) | 0.27 |
| TT | 8 (3.2%) | 1 (0.4%) | 8.23 (1.02–66.31) | 0.047* |
| G allele frequency | 327 (65.4%) | 353 (70.6%) | 1 | 1 |
| T allele frequency | 173 (34.6%) | 147 (29.4%) | 1.27 (0.97–1.66) | 0.078 |
Abbreviation: n, number of samples.
Level of significance: P-value <0.05*, <0.01†, <0.001‡.
CCND1 polymorphism’s genotype and allele frequencies are given in Table 3. Genotype frequency of CCND1 polymorphism rs614367 showed ∼4.88-fold increased risk of brain tumor with homozygous mutant genotype (OR, 4.88; 95% CI, 1.39–17.21; P=0.01) in sampled tumor patients. Furthermore, higher frequency of heterozygous mutant genotype (OR, 1.48; 95% CI, 1.04–2.12, P=0.03) and mutant T allele (OR, 1.65; 95% CI, 1.23–2.22; P=0.0007) was observed in tumor patients as compared with control individuals. In case of rs498136 polymorphism of CCND1, ∼8.23-fold increased risk of brain tumor was observed associated with homozygous mutant genotype (OR, 8.23; 95% CI, 1.02–66.31; P=0.047) in brain tumor patients compared with controls.
Logistic regression models analysis
Three logistic regression models (dominant, recessive, additives) were used for further analyses of genotype frequencies of all SNPs as shown in Table 4. For RB1 SNP rs137853294, dominant (OR, 1.62; 95% CI, 1.13–2.33; P=0.008) and additive genetic model (OR, 1.50; 95% CI, 1.11–2.01; P=0.007) showed significant association with increased risk of brain tumor. Similarly, rs121913300 SNP showed the significant association of brain tumor risk with all three genetic models, i.e. dominant (P<0.0001), recessive (P=0.003) and additives (P=0.0005). Moreover, CCND1 polymorphism rs614367 showed significant association of all three genetic models, i.e. dominant (P=0.002), recessive (P=0.01) and additive (P=0.0007) with increased risk of brain tumor. rs498136 polymorphism also showed significant association of recessive genetic model (OR, 8.23; 95% CI, 1.02–66.31; P=0.047) with increased risk of brain tumor.
Table 4. Association of SNPs of RB1 and CCND1 gene with brain tumor risk based on genetic models.
| Genotype/Allele | Model | OR (95% CI) | P-value |
|---|---|---|---|
| RB1 gene | |||
| rs137853294 | |||
| CC vs CT + TT | Dominant | 1.62 (1.13–2.33) | 0.008† |
| TT vs CC + CT | Recessive | 1.58 (0.77–3.26) | 0.21 |
| T vs C | Additive | 1.50 (1.11–2.01) | 0.007† |
| rs121913300 | |||
| CC vs CT + TT | Dominant | 3.78 (2.12–6.73) | <0.0001**** |
| TT vs CC + CT | Recessive | 20.48 (2.72–154.21) | 0.003† |
| T vs C | Additive | 1.56 (1.22–2.01) | 0.0005‡ |
| CCND1 gene | |||
| rs614367 | |||
| CC vs CT + TT | Dominant | 1.77 (1.24–2.52) | 0.002† |
| TT vs CC + CT | Recessive | 4.88 (1.39–17.21) | 0.01* |
| T vs C | Additive | 1.65 (1.23–2.22) | 0.0007‡ |
| rs498136 | |||
| GG vs GT + TT | Dominant | 1.38 (0.96–1.99) | 0.08 |
| TT vs GG +GT | Recessive | 8.23 (1.02–66.31) | 0.047* |
| T vs G | Additive | 1.27 (0.97–1.66) | 0.08 |
Association of RB1 and CCND1 SNPs with different parameters
Genotypes of all four selected SNPs of cell cycle genes were associated with demographic features, risk factors and histopathological subtypes by applying logistic regression model as shown in Table 5. Results showed that rs137853294 polymorphism (OR, 2.272; 95% CI, 0.088–0.084; P=0.024) and rs121913300 polymorphism of RB1 (OR, 0.264; 95% CI, 0.082–0.0851; P=0.026) showed positive association with tumor grades. For CCND1 gene, rs614367 and rs498136 also showed positive association with tumor grades (OR, 4.197; 95% CI, 0.054–0.771; P=0.014 and OR, 2.137; 95% CI, 0.258–5.007; P=0.03), as shown in Table 5.
Table 5. Association of selected SNPs of RB1 and CCND1 genes with different parameters.
| SNPs vs parameters | B | Std. error | Wald | Sig. | OR | 95% CI |
|---|---|---|---|---|---|---|
| rs137853294 vs | ||||||
| Gender | −0.636 | 0.533 | 1.428 | 0.232 | 0.529 | 0.186–1.503 |
| Age | 0.399 | 0.558 | 0.512 | 0.474 | 1.491 | 0.499–4.451 |
| Smoking | 0.33 | 0.614 | 0.289 | 0.591 | 0.719 | 0.216–2.394 |
| Family history | −0.877 | 0.783 | 1.255 | 0.263 | 0.416 | 0.090–1.929 |
| IR | −0.07 | 1.281 | 0.003 | 0.956 | 0.932 | 0.076–11.490 |
| Grade | 3.3 | 0.577 | 5.077 | 0.024 | 2.272 | 0.088–0.844 |
| Types | −0.536 | 0.603 | 0.790 | 0.374 | 0.585 | 0.180–1.907 |
| rs121913300 vs | ||||||
| Gender | −0.127 | 0.524 | 0.059 | 0.809 | 0.881 | 0.316–2.459 |
| Age | 0.332 | 0.617 | 0.289 | 0.591 | 1.393 | 0.416–4.668 |
| Smoking | 1.958 | 0.518 | 3.418 | 0.064 | 1.384 | 0.139–1.059 |
| Family history | 0.247 | 0.509 | 0.235 | 0.628 | 1.28 | 0.472–3.470 |
| IR | 0.061 | 0.823 | 0.005 | 0.941 | 1.062 | 0.212–5.327 |
| Grade | 4.333 | 0.598 | 4.976 | 0.026 | 3.264 | 0.082–0.851 |
| Types | -0.405 | 0.596 | 0.462 | 0.497 | 0.667 | 0.208–2.144 |
| rs614367 vs | ||||||
| Gender | −0.017 | 0.616 | 0.001 | 0.978 | 0.983 | 0.294–3.285 |
| Age | 0.168 | 0.659 | 0.065 | 0.798 | 1.183 | 0.325–4.304 |
| Smoking | 1.589 | 0.678 | 5.496 | 0.019 | 0.204 | 0.054–0.771 |
| Family History | 0.572 | 1.139 | 0.253 | 0.615 | 1.772 | 0.190–16.512 |
| IR | 0.334 | 1.159 | 0.083 | 0.773 | 1.397 | 0.144–13.537 |
| Grade | 5.625 | 0.659 | 6.084 | 0.014 | 4.197 | 0.054–0.716 |
| Types | −0.249 | 0.685 | 0.133 | 0.716 | 0.779 | 0.204–2.983 |
| rs498136 vs | ||||||
| Gender | 0.56 | 0.864 | 0.42 | 0.517 | 1.75 | 0.322–9.517 |
| Age | −1.052 | 0.777 | 1.834 | 0.176 | 0.349 | 0.076–1.601 |
| Smoking | −0.586 | 0.759 | 0.597 | 0.44 | 0.556 | 0.126–2.462 |
| Family history | 0.124 | 1.162 | 0.011 | 0.915 | 1.132 | 0.116–11.049 |
| IR | −0.822 | 1.201 | 0.468 | 0.494 | 0.44 | 0.042–4.625 |
| Grade | 2.128 | 0.756 | 0.029 | 0.035 | 2.137 | 0.258–5.007 |
| Types | 0.788 | 1.117 | 0.498 | 0.480 | 2.200 | 0.247–19.633 |
Bold values are statistically significant.
Level of significance: P-value <0.05.
Haplotype analysis of RB1 and CCND1 SNPs
LD was estimated between all selected SNPs of RB1 and CCND1 genes. Haplotypes of these SNPs were also examined to determine their association with tumor risk. Thirteen common haplotypes were generated from these selected SNP, among brain tumor patients and controls as shown in Table 6. Haplotypes which significantly increased the risk of brain tumor included CCTG (P=0.002), CCTT (P=3.57e-006), CTCG (P=5.41e-010), TCCT (P=0.008), TCTG (P=0.006), TCTT (P=0.0006), TTTT (P=0.01) and CTCT (P=2.16e-006). Whereas, haplotypes which significantly reduced the risk of brain tumor included CCCG (P=6.21e-012), CCCT (P=1.09e-009), CTTG (P=0.0005) and TTTG (P=0.003).
Table 6. Haplotypes of cell cycle genes (RB1 and CCND1) in brain tumor patients.
| RB1 haplotypes (SNPs) | CCND1 haplotypes (SNPs) | Frequency | χ² | P-value | OR | 95% CI | |||
|---|---|---|---|---|---|---|---|---|---|
| rs137853294 | rs121913300 | rs614367 | rs498136 | Cases | Controls | ||||
| C | C | C | G* | 0.107 | 0.279 | 47.336 | 6.21e-012 | 0.31 | 0.219–0.437 |
| C | C | C | T* | 0.091 | 0.234 | 37.222 | 1.09e-009 | 0.329 | 0.228–0.476 |
| C | C | T | G* | 0.054 | 0.018 | 9.456 | 0.002113 | 3.127 | 1.458–6.707 |
| C | C | T | T* | 0.074 | 0.014 | 21.51 | 3.57e-006 | 5.717 | 2.506–13.040 |
| C | T | C | G* | 0.295 | 0.134 | 38.583 | 5.41e-010 | 2.711 | 1.966–3.739 |
| C | T | T | G* | 0.06 | 0.124 | 12.078 | 0.000513 | 0.453 | 0.288–0.715 |
| T | C | C | G* | 0.035 | 0.018 | 2.709 | 0.099806 | 1.962 | 0.867–4.440 |
| T | C | C | T* | 0.058 | 0.025 | 6.845 | 0.008905 | 2.403 | 1.223–4.721 |
| T | C | T | G* | 0.021 | 0.003 | 7.507 | 0.006161 | 8.424 | 1.361–52.138 |
| T | C | T | T* | 0.056 | 0.016 | 11.582 | 0.00067 | 3.642 | 1.648–8.044 |
| T | T | C | G* | 0.081 | 0.109 | 2.213 | 0.136876 | 0.724 | 0.473–1.110 |
| T | T | T | G* | 0.001 | 0.022 | 8.746 | 0.003113 | 0.053 | 0.007–0.376 |
| T | T | T | T* | 0.017 | 0.001 | 6.109 | 0.013468 | 11.843 | 1.815–77.292 |
Abbreviation: χ², chi-square. P-value <0.05 was statistically significant.
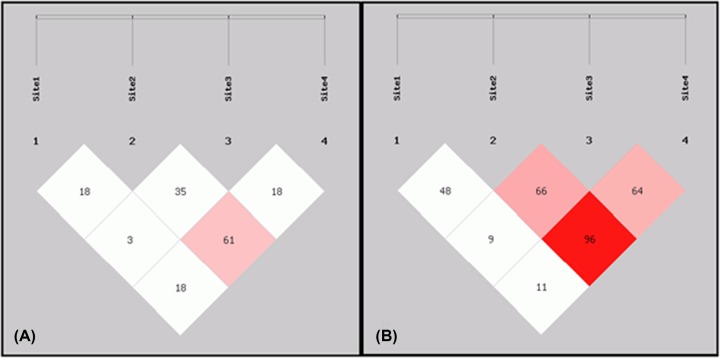
Moreover, LD plot showed strong LD between exonic RB1 SNP (rs121913300) and intergenic CCND1 SNP (rs614367) in tumor patients. Highly strong LD was also observed between CCND1 intergenic SNPs (rs614367 and rs498136) in brain tumor patients compared with controls as illustrated in Figure 1. Logistic regression analysis for SNP–SNP interactions among all four SNPs of RB1 and CCND1 genes showed positive significant correlation between s137853294 vs rs498136 (OR, 3.372; 95% CI, 0.520–21.872; P=0.02) and rs614367 vsrs498136 (OR, 3.083; 95% CI, 0.559–17.00; P=0.029) with increased risk of brain tumor as shown in Table 7.
Figure 1. LD plot for RB1 and CCND1 polymorphism.
(A) Control sample; (B) tumor patient samples. Site1 for rs137853294; Site2 for rs121913300; Site3 for rs614367; Site4; rs498136; darker region shows higher r2-value.
Table 7. SNP–SNP interactions of all selected SNPs with brain tumor risk based on logistic regression model.
| SNP–SNP interactions | B | Std. error | Wald | Sig. | OR | 95% CI |
|---|---|---|---|---|---|---|
| rs137853294 vs rs121913300 | 0.852 | 0.756 | 1.269 | 0.26 | 2.343 | 0.532–10.315 |
| rs137853294 vs rs614367 | 1.509 | 1.153 | 1.715 | 0.19 | 0.221 | 0.023–2.116 |
| rs137853294 vs rs498136 | 3.329 | 0.954 | 1.624 | 0.0203 | 3.372 | 0.520–21.872 |
| rs121913300 vs rs614367 | 1.064 | 0.738 | 2.076 | 0.15 | 2.897 | 0.682–12.314 |
| rs121913300 vs rs498136 | 0.078 | 1.14 | 0.005 | 0.945 | 1.081 | 0.116–10.106 |
| rs614367 vs rs498136 | 3.126 | 0.871 | 1.67 | 0.0296 | 3.083 | 0.559–17.006 |
P-value<0.05 was statistically significant.
mRNA secondary structure and protein structure prediction of RB1 SNPs
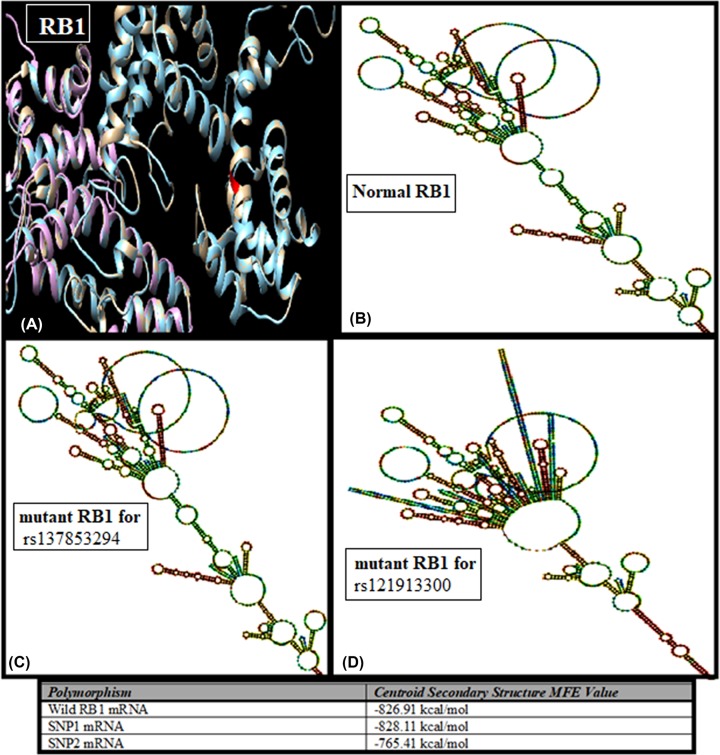
Sequence of wild RB1 gene and its two exonic SNPs were used to predict their secondary structure of mRNA using ViennaRNA Web Service. Prediction showed that there is no visual change in the structure of wild RB1 mRNA and first missense mutated mRNA. While second mutated mRNA changed and shortened its structure as demonstrated in Figure 5. According to centroid secondary structure, minimum free energy (MFE) of wild mRNA and mutated mRNA were −826.91 and −828.11 kcal/mol, respectively. Moreover, truncated mRNA had −765.41 kcal/mol minimum free energy. Protein structure of wild RB1 gene, SNP1 mutated RB1 and SNP2 truncated RB1 gene were predictive using SWISS-MODEL as illustrated in Figure 2.
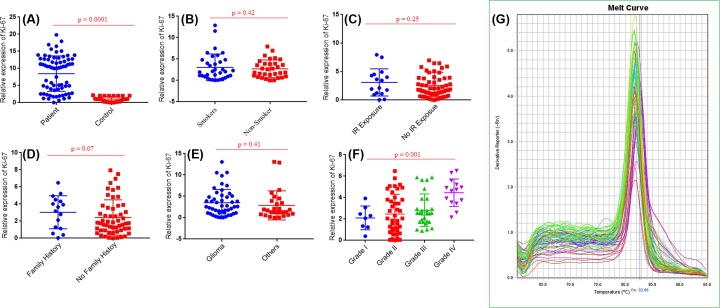
Figure 5. Expression profiling of Ki-67 gene in study cohort.
mRNA expression of (A) Ki-67 in brain tumor samples and normal control samples, (B) Ki-67 in brain tumor samples with smoking status (C) Ki-67 in brain tumor samples with IR. (D) Ki-67 in tumor samples with family history, (E) Ki-67 in different types of brain tumor, (F) Ki-67 in brain tumor samples with different grades. Among these grades, grade I included meningiomas (9), grade II included diffuse astrocytoma (7), choroid glioma (12), oligodandroglioma (5), eppendoma (7), atypical meningioma (8) and pituitary adenoma (4). Grade III inculded anaplastic astrocytoma (19), anaplastic oligodandroglioma (3), anaplastic meningioma (4) and pituitary adenoma (3). Grade IV included GBM (11) and diffuse medine glioma (4). (G) Melt curve analysis of Ki-67 gene.
Figure 2. Protein and mRNA secondary structure prediction of RB1 exonic SNPs.
(A) Super-imposed structure of normal and mutated RB1 proteins (blue, wild; white, SNP1 mutated); purple, SNP2 truncated). (B) mRNA secondary structure of normal RB1 gene. (C) mRNA secondary structure of SNP1 rs137853294 polymorphism. (D) mRNA secondary structure of SNP2 rs121913300 polymorphism.
Expression analysis of RB1 and CCND1 gene at mRNA
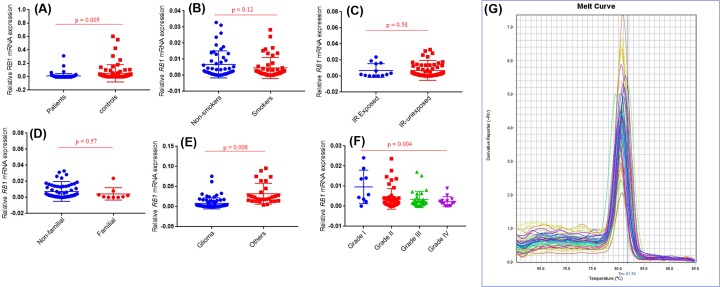
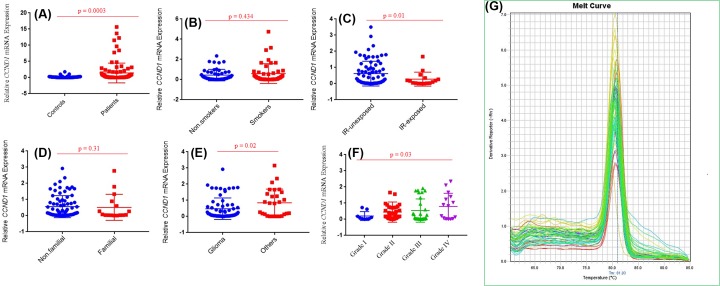
RB1 and CCND1 mRNA levels were observed in study cohort II including 96 brain tumor tissues and adjacent uninvolved healthy section used as control. RB1 expression has observed significantly lower in brain tumour (P=0.005) than in normal tissue samples. Statistical significant decrease in RB1 mRNA level was observed in brain tumors with anatomical site of glioma (P=0.008) compared with other anatomical sites. Significant decreased mRNA level of RB1 gene was also observed in grade IV (P=0.004) brain tumor as compared with other grades (Figure 3). In case of second selected gene CCND1, significantly higher mRNA level was observed in brain tumors section compared with adjacent control section (P=0.0003). Further analysis showed significantly increased CCND1 mRNA level in grade IV (P=0.03) brain tumor patients compared with other grades (Figure 4).
Figure 3. Expression profiling of RB1 gene in study cohort.
mRNA expression of (A) RB1 in brain tumor samples and normal control samples. (B) RB1 in brain tumor samples with smoking status. (C) RB1 in brain tumor samples with IR. (D) RB1 in tumor samples with family history. (E) RB1 in different types of brain tumor. (F) RB1 in brain tumor samples with different grades. Among these grades, grade I included meningiomas (9), grade II included diffuse astrocytoma (7), choroid glioma (12), oligodandroglioma (5), eppendoma (7), atypical meningioma (8) and pituitary adenoma (4). Grade III inculded anaplastic astrocytoma (19), anaplastic oligodandroglioma (3), anaplastic meningioma (4) and pituitary adenoma (3). Grade IV included GBM (11) and diffuse medine glioma (4). (G) Melt curve analysis of RB1 gene.
Figure 4. Expression profiling of CCND1 gene in study cohort.
mRNA expression of (A) CCND1 in brain tumor samples and normal control samples, (B) CCND1 in brain tumor samples with smoking status, (C) CCND1 in brain tumor samples with IR, (D) CCND1 in tumor samples with family history, (E) CCND1 in different types of brain tumor, (F) CCND1 in brain tumor samples with different grades. Among these grades, grade I included meningiomas (9), grade II included diffuse astrocytoma (7), choroid glioma (12), oligodandroglioma (5), eppendoma (7), atypical meningioma (8) and pituitary adenoma (4). Grade III inculded anaplastic astrocytoma (19), anaplastic oligodandroglioma (3), anaplastic meningioma (4) and pituitary adenoma (3). Grade IV included GBM (11) and diffuse medine glioma (4). (G) melt curve analysis of CCND1 gene.
Expression level of proliferation marker Ki-67 was also observed to find out whether the change in expression level of cell cycle gene affected the proliferation process in brain tumorigenesis. Significantly higher level of Ki-67 was observed in brain tumor (P=0.0001) compared with adjacent control section and this up-regulation was more pronounced in grade IV brain tumor tissue (P=0.001) compared with other grades (Figure 5).
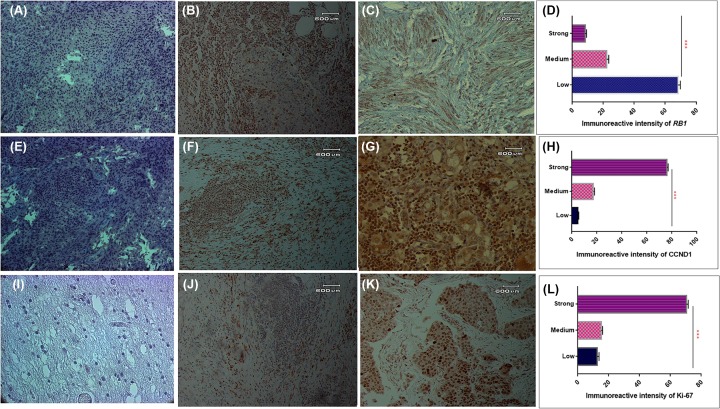
Expression analysis of RB1 and CCND1 gene at protein level
Expression level of RB1, CCND1 and Ki-67 was also observed in 96 brain tumor section and adjacent control section using IHC. Expression of RB1 was observed lower in brain tumors compared with adjacent control sections as shown in Figure 6A,B,C. Measurement of immunoreactive intensity showed that weak immunoreactivity of RB1 was observed significantly higher (P=0.001) in brain tumor sections as compared with moderate and strong immunoreactive intensity as shown in Figure 6D. Expression analysis of CCND1 at protein level showed the increased expression of CCND1 in brain tumor section compared with control section as shown in Figure 6E,F. Measurement of immunoreactive intensity also showed that strong immunoreactive intensity of CCND1 was observed significantly higher (P=0.001) in brain tumor sections as compared with weak and moderate immunoreactive intensity as shown in Figure 6G.
Figure 6. Immunohistochemical analysis of cell cycle pathway genes in study cohort.
Protein expression of RB1 gene (A), negative control (B), adjacent control section (C) brain tumor. Immunoreactive intesity of RB1 gene in brain tumor sections (D). Protein expression of CCND1 gene (E), negative control (F), adjacent control section (G) brain tumor. Immunoreactive intesity of CCND1 gene in brain tumor sections (H). Protein expression of Ki-67 gene (I), negative control (J), adjacent control section (K) brain tumor. Immunoreactive intesity of Ki-67 gene in brain tumor sections (L).
Expression level of Ki-67 was also observed at protein level using the IHC and expression level of Ki-67 was observed to be higher in brain tumors section compared with adjacent control section as shown in Figure 6H,I. Measurement of immunoreactive intensity also showed that strong immunoreactive intensity of Ki-67 was observed significantly higher (P=0.001) in brain tumor sections as compared with weak and moderate immunoreactive intensity as shown in Figure 6J.
Correlation between RB1, CCND1 and Ki-67 expression and clinicopathological characteristics
Correlations were tested between RB1, CCND1 and Ki-67, clinical and pathological features of brain tumor patients group II. The RB1 mRNA level was negatively correlated with grades (r = −0.252**, P<0.01), however positive correlation was observed for CCND1 mRNA level and grades (r = 0.222*, P<0.05) of brain tumor patients. In case of gene to gene correlation, a significant negative correlation was observed between CCND1 vs RB1 (r = −0.337**, P<0.001) and RB1 vs Ki-67 (r = −0.291*, P<0.05) in brain tumor patients as shown in Table 8.
Table 8. Spearman correlations among clinical features and cell cycle pathway genes expression of brain tumors*.
| mRNA | Gender | Type | Survival | Family | Grade | I.R | Area | RB1 | CCND1 | Ki-67 |
|---|---|---|---|---|---|---|---|---|---|---|
| Age | 0.039 | −0.037 | 0.074 | 0.111 | 0.06 | −0.247‡ | −0.22 | −0.33 | 0.126 | 0.124 |
| Gender | 0.02 | 0.416 | 0.067 | −0.04 | 0.016 | 0.195† | 0.009 | 0.104 | 0.33‡ | |
| Type | 0.056 | −0.058 | 0.146 | −0.027 | −0.016 | −0.067 | −0.132 | 0.07 | ||
| Survival | −0.057 | 0.01 | 0.108 | 0.049 | −0.150 | −0.05 | 0.171 | |||
| Family | −0.182† | −0.081 | 0.005 | 0.137 | −0.016 | −0.169 | ||||
| Grade | 0.045 | −0.117 | −0.252† | 0.222† | 0.103 | |||||
| I.R | −0.051 | −0.098 | 0.072 | 0.091 | ||||||
| Area | 0.045 | 0.047 | −0.264† | |||||||
| RB1 | −0.337‡ | −0.291† | ||||||||
| CCND1 | 0.135 |
| Protein level | Gender | Type | Survival | Family | Grade | I.R | Area | RB1 | CCND1 | Ki-67 |
|---|---|---|---|---|---|---|---|---|---|---|
| Age | 0.039 | −0.037 | 0.074 | 0.111 | 0.06 | −0.247§ | −0.22 | −0.29 | 0.12 | 0.07 |
| Gender | 0.02 | 0.416 | 0.067 | −0.04 | 0.016 | 0.195† | 0.32 | 0.09 | 0.05 | |
| Type | 0.056 | −0.058 | 0.146 | −0.027 | −0.016 | −0.12 | −0.11 | 0.13 | ||
| Survival | −0.057 | 0.01 | 0.108 | 0.049 | −0.08 | −0.07 | 0.08 | |||
| Family | −0.182† | −0.081 | 0.005 | 0.06 | 0.02 | 0.14 | ||||
| Grade | 0.045 | −0.117 | −0.394‡ | 0.19 | 0.54§ | |||||
| I.R | −0.051 | −0.16 | 0.06 | 0.16 | ||||||
| Area | 0.08 | 0.12 | 0.21† | |||||||
| RB1 | −0.54§ | −0.29† | ||||||||
| CCND1 | 0.43‡ |
*Spearman correlation coefficients. The expression levels of RB1, CCND1 and Ki-67 for the patient cohort were based on the relative mRNA level and protein level. The P-values were computed using one-way ANOVA and χ2-test.
P<0.05.
P<0.01.
P<0.001.
Correlations was also tested at protein level between selected genes and clinicopathological parameters of gastric cancer patients as shown in Table 8. A significant negative correlation was observed between CCND1 vs RB1 (r = −0.54***, P<0.0001) and RB1 vs Ki-67 (r = −0.29*, P<0.05) in brain tumor patients. However, a significant positive correlation was observed between CCND1 vs Ki-67 (r = 0.43**, P<0.001) in brain tumor patients as shown in Table 8.
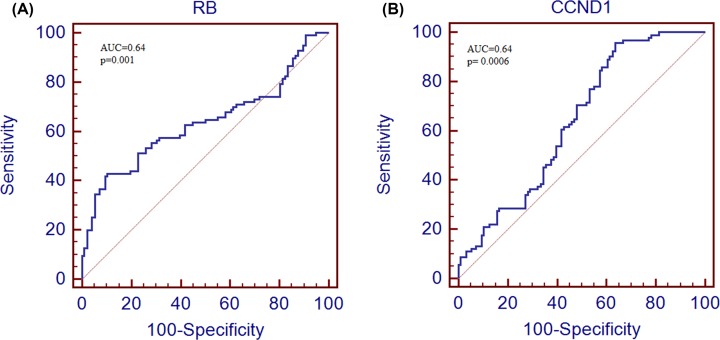
ROC curve analysis
To assess the diagnostic value of both selected genes ROC curve analysis was performed. After the generation of ROC curve, area under the curve (AUC) and 95% CI was also calculated. The area under the curve for RB1 gene was 63.5 (95% CI, 0.562–0.703; P<0.001) and for CCND1 gene was 64.0 (95% CI, 0.567–0.709; P<0.0006) as shown in Figure 7.
Figure 7. ROC curve analysis of cell cycle pathway genes in study cohort.
ROC curve anlysis of RB1 gene (A) and CCND1 (B) in brain tumor patients.
Discussion
The present study was designed to explore the correlation between the genetic polymorphism of RB1 and CCND1 genes to brain tumor risk in Pakistani population. The present study encompasses the genetic analysis of RB1 exonic and CCND1 intergenic polymorphisms in brain tumor patients to find their association with brain carcinogenesis. This has followed by structure prediction of exonic variants performed to assess the effect of these polymorphism on transcription level. Expression levels of RB1 and CCND1 were also analyzed in brain tumor patients. Furthermore, expression levels of cell cycle pathway genes were also correlated with proliferation marker, Ki-67 to illuminate correlation between cell cycle pathway gene variation and proliferation process in brain tumorigenesis.
In present study we used two study cohorts, cohort I consisted of 250 blood samples of brain tumor patients and cohort II consisted of 96 brain tumors. Both cohorts of brain cancer contained higher number of glioma patients compared with other type of brain tumors such as meningioma and pituitary adenomas. Previous studies have also reported the increased incidence of glioma (77–81% of all primary malignant tumors of CNS) in the southeast, northwest, and midwest of U.S.A. [22], Asian population and Hispanic population [23] compared with meningioma and pituitary adenomas. Reasons binding these incidence differences can be variations in geographic regions, environmental factors, diet, occupational and personal exposures and lifestyle [22,24]. In addition, ethnic/race variations are likely to contribute to observed differences [25,26].
Retinoblastoma 1 gene has been found mutated or deregulated in many human cancers [27–35] and one subtype of brain tumor, glioma [36]. Present study examined the two exonic SNPs of RB1 gene (rs137853294 and rs121913300) in brain tumor patients. Exonic or coding region SNPs mainly influence the transcription of the gene by altering the structure and function of transcribed protein [37]. Among SNPs, rs137853294 showed the significant association in heterozygous mutant genotype to brain tumor risk in current study. This SNP alters the protein structure of RB1 by replacing amino acid Arginine to Tryptophan. As a result of this missense mutation, altered pRB protein is formed which disrupts the cell cycle checkpoints and contributes to tumorigenesis [13]. Furthermore, second exonic variant, rs121913300 was also observed significantly associated with brain tumor risk, indicated by genotypic frequency of both homozygous and heterozygous mutants in current study. This SNP stops the transcription of RB1 gene by inducing the stop codon. Resulting truncated pRB protein is formed which causes the abnormality in cell cycle control [13]. These findings of both SNPs agree with many earlier studies which state that genetic mutations in RB1 gene vary its expression and can contribute in retinoblastoma [13,27].
Cyclin D1 gene, second important molecule of cell cycle pathway has also been found mutated in almost every human cancer by altering the normal cell cycle pathway. CCND1 gene polymorphisms have been found in several cancers [38–47] including gliomas also [48]. However, till now no study has been published with respect to brain tumor and different subtypes of brain tumor such as glioma, meningioma and pituitary adenoma. In this study, two intergenic SNPs (rs614367 and rs498136) of CCND1 were analyzed which can potentially influence the regulation and expression of CCND1 gene. Any polymorphism in intergenic regions may disrupt the transcription of CCND1 gene by altering its expression and may increase the susceptibility of diseases [49].
SNP rs613467 is present in the regulatory region of CCND1 which regulates the transcription of CCND1 gene. Alterations in that region can cause the abnormality in interpretation of regulating signals resultantly producing transcription abnormalities [50]. rs614367, was found significantly associated with increased risk of brain tumor in both homozygous and heterozygous mutant genotypes. Similar trend of rs614367 association has earlier been found in breast cancer patients in earlier studies [51,52]. SNP rs498136 is located in 5′ promotor region of CCND1 at transcription binding site and resultantly alters the binding site of transcription factors for CCND1 gene and aberrant regulation of the gene [53]. Second selected SNP of CCND1 polymorphism rs498136, was also showed significant association in brain tumor patients in homozygous mutant genotype in present study. Findings of the present study are in line with the previous study suggested the strong association of rs498136 with malignant melanoma [16].
To test the hypothesis that SNPs in coding region/intragenic region result in variations at transcription level and change expression level of respective genes. Expression levels of RB1 and CCND1 gene was also measured in cohort II of brain tumor patients and controls using qPCR and immunohistochemistry. Significant down-regulation of RB1 expression was observed in brain tumor patients when compared with adjacent controls, after qPCR and IHC. This down-regulation was observed as more pronounced in grade IV tumors compared with lower grade tumors. Expression pattern variations between the controls and patients may be due to genetic heterogeneity in RB1 gene by different environmental factors and genetic and epigenetic changes [54,55].
Expression level of RB1 gene was also correlated with different type of brain tumors and significant down-regulation of RB1 gene was observed in glioma compared with meningioma and pituitary adenomas. Deregulation of RB1 gene has been reported in different types of brain tumor such as glioma [56] and meningioma [57]. It has also been reported in previous study that down-regulation of RB1 gene in glioma was associated with increased cell proliferation and decrease survival in more than one-third of patients [58]. One of basic reason of down-regulated expression of RB1 gene in glioma compared with meningioma and pituitary adenoma, can be that number of gliomas are significantly higher in our study cohort compared with other type of brain tumors. Other reasons of this down-regulation are genetic variations [30,59], RB1 promoter hypermethylation [31,60–63], variations in microRNA binding affinity [64,57] and this down-regulated/loss of expression ultimately resulted in increased invasion of tumor cells and more aggressive type of brain tumor in CNS carcinogenesis process [62].
In case of second selected molecule, CCND1 gene, significant up-regulation was observed in brain tumor patients compared with controls using qPCR and immunohistochemistry. Additionally, this up-regulation was observed higher in aggressive brain tumors in present study. CCND1 overexpressed and gene amplification is reported in many cancers including the meningioma and pituitary adenomas [65–68]. Mechanisms which are involved in over expression of CCND1 gene by upstream factors, remain unknown. Genetic variations in exonic region [42] and intragenic/UTR region resulted in abnormal binding of transcription factors. [67] has found the relation between abnormal binding of octamer-binding transcription factor 4 (OCT4) due to polymorphism in UTR region of CCND1 with the octamer motif (ATTTTGCAT) and promoted proliferation of cell cycle [66] and tumorigenesis. Additionally, expression levels of RB1 and CCND1 gene was also correlated with expression level of proliferation marker, Ki-67. Significant correlation was observed which is according to earlier findings that genetic aberrations and expression deregulation of cell cycle pathway genes results in uncontrolled cell cycle process and enhanced proliferation.
In conclusion, our study demonstrates a significant association between cell cycle pathway genes, polymorphisms and brain tumors in Pakistani population. Our study also confirms that the deregulated cell cycle pathway gene is linked with increased brain tumorigenesis, at least in Pakistani population. As the matter of fact, tumorigenesis and deregulated cell cycle genes are the major challenging items in neoplastic initiation and progression. Additional studies such as, a large-scale studies adjusting for a wide range of factors, [7,10] functional alteration studies as single cell level will be recommended to validate these findings and to fully explore the molecular mechanisms that contribute to the deregulation of cell cycle pathway genes in brain tumorigenesis.
Acknowledgements
Authors acknowledge infrastructural help from Higher Education Commission of Pakistan (HEC) and COMSATS University, Islamabad. Authors are thankful to patients and staff of Pathology Department, PIMS, Islamabad, and for contribution to this research.
Abbreviations
- CI
confidence interval
- DEPC
diethyl pyrocarbonate
- GBM
glioblastoma multiforme
- IDT
integrated DNA technologies
- IHC
immunohistochemical analysis
- LD
linkage disequilibrium
- OR
odds ratio
- PIMS
Pakistan Institute of Medical Sciences
- SNP
single nucleotide polymorphism
Competing Interests
The authors declare that there are no competing interests associated with the manuscript.
Funding
The authors declare that there are no sources of funding to be acknowledged.
Author Contribution
All the authors read and approved the final version of manuscript. A.Z.N., S.A., M.W.A. and A.U.K. collected and isolated the DNA/RNA samples. A.Z.N., M.W.A. and Z.A. performed the genotyping and drafted the manuscript. S.A., A.U.K. and I.M. performed the relative expression analysis studies and drafted the manuscript. I.M. performed the genotyping/expression studies, statistical analyses of the data and draft of the manuscript. M.A.K. supervised the project, helped to analyze the statistical data and provided critical revisions. All the authors discussed the results and commented on the manuscript.
References
- 1.Louis D.N., Perry A., Reifenberger G., Von Deimling A., Figarella-Branger D., Cavenee W.K. et al. (2016) The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. (Berl.) 131, 803–820 10.1007/s00401-016-1545-1 [DOI] [PubMed] [Google Scholar]
- 2.Gladson C.L., Prayson R.A. and Liu W.M. (2010) The pathobiology of glioma tumors. Annu. Rev. Pathol. Mech. Dis. 5, 33–50 10.1146/annurev-pathol-121808-102109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Louis D.N., Ohgaki H., Wiestler O.D., Cavenee W.K., Burger P.C., Jouvet A. et al. (2007) The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 114, 97–109 10.1007/s00401-007-0243-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ohgaki H., Dessen P., Jourde B., Horstmann S., Nishikawa T., Di Patre P.L. et al. (2004) Genetic pathways to glioblastoma: a population-based study. Cancer Res. 64, 6892–6899 10.1158/0008-5472.CAN-04-1337 [DOI] [PubMed] [Google Scholar]
- 5.Ohgaki H. and Kleihues P. (2005) Epidemiology and etiology of gliomas. Acta Neuropathol. (Berl) 109, 93–108 10.1007/s00401-005-0991-y [DOI] [PubMed] [Google Scholar]
- 6.Stewart L.A. (2002) Chemotherapy in adult high-grade glioma: a systematic review and meta-analysis of individual patient data from 12 randomised trials. Lancet 359, 1011–1018 [DOI] [PubMed] [Google Scholar]
- 7.Yosunkaya E., Kucukyuruk B., Onaran I., Gurel C.B., Uzan M. and Kanigur-Sultuybek G. (2010) Glioma risk associates with polymorphisms of DNA repair genes, XRCC1 and PARP1. Br. J. Neurosurg. 24, 561–565 10.3109/02688697.2010.489655 [DOI] [PubMed] [Google Scholar]
- 8.Belanger H., Beaulieu P., Moreau C., Labuda D., Hudson T.J. and Sinnett D. (2005) Functional promoter SNPs in cell cycle checkpoint genes. Hum. Mol. Genet. 14, 2641–2648 10.1093/hmg/ddi298 [DOI] [PubMed] [Google Scholar]
- 9.Dalton S. (2015) Linking the cell cycle to cell fate decisions. Trends Cell Biol. 25, 592–600 10.1016/j.tcb.2015.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dickson M.A. (2014) Molecular pathways: CDK4 inhibitors for cancer therapy. Clin. Cancer Res. 20, 3379–3383 10.1158/1078-0432.CCR-13-1551 [DOI] [PubMed] [Google Scholar]
- 11.Bertoli C., Skotheim J.M. and De Bruin R.A. (2013) Control of cell cycle transcription during G1 and S phases. Nat. Rev. Mol. Cell Biol. 14, 518 10.1038/nrm3629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.VanArsdale T., Boshoff C., Arndt K.T. and Abraham R.T. (2015) Molecular pathways: targeting the cyclin D–CDK4/6 axis for cancer treatment. Clin. Cancer Res. 21, 2905–2910 10.1158/1078-0432.CCR-14-0816 [DOI] [PubMed] [Google Scholar]
- 13.Uddin S.N., Majumder A., Islam K.K., Hossain S.A. and Sarker P.K. (2015) Minimum free energy based evaluation of mRNAs secondary structures constructed by 18 clinically significant exonic single nucleotide polymorphisms (SNPs) and haplotypes of 5 missense SNPs of RB1 gene. Am. J. Biochem. Biotechnol. 11, 191 [Google Scholar]
- 14.Petre-Draviam C.E., Williams E.B., Burd C.J., Gladden A., Moghadam H., Meller J. et al. (2005) A central domain of cyclin D1 mediates nuclear receptor corepressor activity. Oncogene 24, 431 10.1038/sj.onc.1208200 [DOI] [PubMed] [Google Scholar]
- 15.Musgrove E.A., Caldon C.E., Barraclough J., Stone A. and Sutherland R.L. (2011) Cyclin D as a therapeutic target in cancer. Nat. Rev. Cancer 11, 558 10.1038/nrc3090 [DOI] [PubMed] [Google Scholar]
- 16.Law M.H., Bishop D.T., Lee J.E., Brossard M., Martin N.G., Moses E.K. et al. (2015) Genome-wide meta-analysis identifies five new susceptibility loci for cutaneous malignant melanoma. Nat. Genet. 47, 987 10.1038/ng.3373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Turnbull C., Ahmed S., Morrison J., Pernet D., Renwick A., Maranian M. et al. (2010) Genome-wide association study identifies five new breast cancer susceptibility loci. Nat. Genet. 42, 504 10.1038/ng.586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mahjabeen I., Baig R.M., Masood N., Sabir M., Malik F.A. and Kayani M.A. (2011) OGG1 gene sequence variation in head and neck cancer patients in Pakistan. Asian Pac. J. Cancer Prev. 12, 2779–2783 [PubMed] [Google Scholar]
- 19.Mahjabeen I., Chen Z., Zhou X. and Kayani M.A. (2012) Decreased mRNA expression levels of base excision repair (BER) pathway genes is associated with enhanced Ki-67 expression in HNSCC. Med. Oncol. 29, 3620–3625 10.1007/s12032-012-0300-2 [DOI] [PubMed] [Google Scholar]
- 20.Mahjabeen I. and Kayani M.A. (2016) Loss of mitochondrial tumor suppressor genes expression is associated with unfavorable clinical outcome in head and neck squamous cell carcinoma: data from retrospective study. PLoS ONE 11, e0146948 10.1371/journal.pone.0146948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mahjabeen I., Ali K., Zhou X. and Kayani M.A. (2014) Deregulation of base excision repair gene expression and enhanced proliferation in head and neck squamous cell carcinoma. Tumour Biol. 35, 5971–5983 10.1007/s13277-014-1792-5 [DOI] [PubMed] [Google Scholar]
- 22.Xu H., Chen J., Xu H. and Qin Z. (2017) Geographic variations in the incidence of glioblastoma and prognostic factors predictive of overall survival in US adults from 2004–2013. Front. Aging Neurosci. 9, 352 10.3389/fnagi.2017.00352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dubrow R. and Darefsky A.S. (2011) Demographic variation in incidence of adult glioma by subtype, United States, 1992-2007. BMC Cancer 11, 325 10.1186/1471-2407-11-325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Miranda-Filho A., Piñeros M., Soerjomataram I., Deltour I. and Bray F. (2016) Cancers of the brain and CNS: global patterns and trends in incidence. Neuro Oncol. 19, 270–280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barnholtz-Sloan J.S., Maldonado J.L., Williams V.L., Curry W.T., Rodkey E.A., Barker F.G. et al. (2007) Racial/ethnic differences in survival among elderly patients with a primary glioblastoma. J. Neuro Oncol. 85, 171 10.1007/s11060-007-9405-4 [DOI] [PubMed] [Google Scholar]
- 26.Barnholtz‐Sloan J.S., Sloan A.E. and Schwartz A.G. (2003) Racial differences in survival after diagnosis with primary malignant brain tumor. Cancer 98, 603–609 10.1002/cncr.11534 [DOI] [PubMed] [Google Scholar]
- 27.Barbosa R.H., Aguiar F.C., Silva M.F., Costa R.A., Vargas F.R., Lucena E. et al. (2013) Screening of RB1 alterations in Brazilian patients with retinoblastoma and relatives with retinoma: phenotypic and genotypic associations. Invest. Ophthalmol. Vis. Sci. 54, 3184–3194 [DOI] [PubMed] [Google Scholar]
- 28.Berge E.O., Knappskog S., Geisler S., Staalesen V., Pacal M., Børresen-Dale A.-L. et al. (2010) Identification and characterization of retinoblastoma gene mutations disturbing apoptosis in human breast cancers. Mol. Cancer 9, 173 10.1186/1476-4598-9-173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.del Río N.R., Gómez J.A., de la Rosa F. A.G., Calvo J.P. and de las Heras Martín A. (2014) Trilateral retinoblastoma. Correlation between the genetic anomalies of the RB1 gene and the presence of pineal gland cysts. Arch. Soc. Esp. Oftalmol. 89, 4–9 [DOI] [PubMed] [Google Scholar]
- 30.Sabir M., Baig R.M., Mahjabeen I., Saeed M., Malik F.A. and Kayani M.A. (2012) Rb1/105 gene alterations and head and neck carcinogenesis. Mol. Biol. Rep. 39, 9573–9581 10.1007/s11033-012-1822-6 [DOI] [PubMed] [Google Scholar]
- 31.Sabir M., Baig R.M., Ali K., Mahjabeen I., Saeed M. and Kayani M.A. (2014) Retinoblastoma (RB1) pocket domain mutations and promoter hyper-methylation in head and neck cancer. Cell. Oncol. 37, 203–213 10.1007/s13402-014-0173-9 [DOI] [PubMed] [Google Scholar]
- 32.Thakur N., Hussain S., Nasare V., Das B.C., Basir S.F. and Bharadwaj M. (2012) Association analysis of p16 (CDKN2A) and RB1 polymorphisms with susceptibility to cervical cancer in Indian population. Mol. Biol. Rep. 39, 407–414 10.1007/s11033-011-0752-z [DOI] [PubMed] [Google Scholar]
- 33.Song H., Ramus S.J., Shadforth D., Quaye L., Kjaer S.K., DiCioccio R.A. et al. (2006) Common variants in RB1 gene and risk of invasive ovarian cancer. Cancer Res. 66, 10220–10226 10.1158/0008-5472.CAN-06-2222 [DOI] [PubMed] [Google Scholar]
- 34.Krecicki T., Smigiel R., Fraczek M., Kowalczyk M. and Sasiadek M.M. (2004) Studies of the cell cycle regulatory proteins P16, cyclin D1 and retinoblastoma protein in laryngeal carcinoma tissue. J. Laryngol. Otol. 118, 676–680 [DOI] [PubMed] [Google Scholar]
- 35.Li A.F.-Y., Li A.C.-H., Tsay S.-H., Li W.-Y., Liang W.-Y. and Chen J.-Y. (2008) Alterations in the p16 INK4a/cyclin D1/RB pathway in gastrointestinal tract endocrine tumors. Am. J. Clin. Pathol. 130, 535–542 10.1309/TLLVXK9HVA89CHPE [DOI] [PubMed] [Google Scholar]
- 36.Goldhoff P., Clarke J., Smirnov I., Berger M.S., Prados M.D., James C.D. et al. (2012) Clinical stratification of glioblastoma based on alterations in retinoblastoma tumor suppressor protein (RB1) and association with the proneural subtype. J. Neuropathol. Exp. Neurol. 71, 83–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sinnett D., Beaulieu P., Bélanger H., Lefebvre J.-F., Langlois S., Théberge M.-C. et al. (2006) Detection and characterization of DNA variants in the promoter regions of hundreds of human disease candidate genes. Genomics 87, 704–710 10.1016/j.ygeno.2006.01.001 [DOI] [PubMed] [Google Scholar]
- 38.Bachmann K., Neumann A., Hinsch A., Nentwich M.F., El Gammal A.T., Vashist Y. et al. (2015) Cyclin D1 is a strong prognostic factor for survival in pancreatic cancer: analysis of CD G870A polymorphism, FISH and immunohistochemistry. J. Surg. Oncol. 111, 316–323 10.1002/jso.23826 [DOI] [PubMed] [Google Scholar]
- 39.Ishigaki T., Sasaki K., Watanabe K., Nakamura N., Toyota S., Kobayashi H. et al. (2010) Amplification of IGH/CCND1 fusion gene in a primary plasma cell leukemia case. Cancer Genet. Cytogenet. 201, 62–65 10.1016/j.cancergencyto.2010.05.006 [DOI] [PubMed] [Google Scholar]
- 40.Li Z., Li X., Li C., Su Y., Fang W., Zhong C. et al. (2014) Transcription factor OCT4 promotes cell cycle progression by regulating CCND1 expression in esophageal carcinoma. Cancer Lett. 354, 77–86 10.1016/j.canlet.2014.07.049 [DOI] [PubMed] [Google Scholar]
- 41.Liao D., Wu Y., Pu X., Chen H., Luo S., Li B. et al. (2014) Cyclin D1 G870A polymorphism and risk of nasopharyngeal carcinoma: a case-control study and meta-analysis. PLoS ONE 9, e113299 10.1371/journal.pone.0113299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sabir M., Baig R.M., Mahjabeen I. and Kayani M.A. (2013) Significance of cyclin D1 polymorphisms in patients with head and neck cancer. Int. J. Biol. Markers 28, 49–55 10.5301/JBM.2012.9768 [DOI] [PubMed] [Google Scholar]
- 43.Wang N., Qian X., Wang S., Gao H., Wang L., Huo Y. et al. (2012) CCND1 rs9344 polymorphisms are associated with the genetic susceptibility to cervical cancer in Chinese population. Mol. Carcinog. 51, 196–205 10.1002/mc.20801 [DOI] [PubMed] [Google Scholar]
- 44.Wang X., Cao L., Zhang F., Wang X., Zhang J., Pei J. et al. (2016) Association study of CCND1 G870A polymorphism with gastric cancer risk: evidence from a meta-analysis. Int. J. Clin. Exp. Pathol. 9, 1644–1651 [Google Scholar]
- 45.Wen L., Hu Y.Y., Yang G.L. and Liu D.X. (2014) CCND1 G870A polymorphism contributes to the risk of esophageal cancer: An updated systematic review and cumulative meta? analysis Biomed. Rep. 2, 549–554 10.3892/br.2014.286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Xu X.M., Ni X.B., Yang G.L., Luo Z.G., Niu Y.M. and Shen M. (2016) CCND1 G870A polymorphism and colorectal cancer risk: An updated meta-analysis. Mol. Clin. Oncol. 4, 1078–1084 10.3892/mco.2016.844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Xue J., Qin Z., Li X., Zhang J., Zheng Y., Xu W. et al. (2017) Genetic polymorphisms in cyclin D1 are associated with risk of renal cell cancer in the Chinese population. Oncotarget 8, 80889 10.18632/oncotarget.20720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Xu Z., Zeng X., Tian D., Xu H., Cai Q., Wang J. et al. (2014) MicroRNA-383 inhibits anchorage-independent growth and induces cell cycle arrest of glioma cells by targeting CCND1. Biochem. Biophys. Res. Commun. 453, 833–838 10.1016/j.bbrc.2014.10.047 [DOI] [PubMed] [Google Scholar]
- 49.Chen J. and Tian W. (2016) Explaining the disease phenotype of intergenic SNP through predicted long range regulation. Nucleic Acids Res. 44, 8641–8654 10.1093/nar/gkw519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Buckland P.R. (2006) The importance and identification of regulatory polymorphisms and their mechanisms of action. Biochim. Biophys. Acta Mol. Basis Dis. 1762, 17–28 10.1016/j.bbadis.2005.10.004 [DOI] [PubMed] [Google Scholar]
- 51.Lambrechts D., Truong T., Justenhoven C., Humphreys M.K., Wang J., Hopper J.L. et al. (2012) 11q13 is a susceptibility locus for hormone receptor positive breast cancer. Hum. Mutat. 33, 1123–1132 10.1002/humu.22089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Silvestri V., Rizzolo P., Scarnò M., Chillemi G., Navazio A.S., Valentini V. et al. (2015) Novel and known genetic variants for male breast cancer risk at 8q24. 21, 9p21. 3, 11q13. 3 and 14q24. 1: Results from a multicenter study in Italy. Eur. J. Cancer 51, 2289–2295 10.1016/j.ejca.2015.07.020 [DOI] [PubMed] [Google Scholar]
- 53.Guo Y. and Jamison D.C. (2005) The distribution of SNPs in human gene regulatory regions. BMC Genomics 6, 140 10.1186/1471-2164-6-140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tateno T., Zhu X., Asa S.L. and Ezzat S. (2010) Chromatin remodeling and histone modifications in pituitary tumors. Mol. Cell. Endocrinol. 326, 66–70 10.1016/j.mce.2009.12.028 [DOI] [PubMed] [Google Scholar]
- 55.Zhou Y., Zhang X. and Klibanski A. (2014) Genetic and epigenetic mutations of tumor suppressive genes in sporadic pituitary adenoma. Mol. Cell. Endocrinol. 386, 16–33 10.1016/j.mce.2013.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ferreira W.A.S., Araújo M.D., Anselmo N.P., de Oliveira E.H.C., Brito J.R.N., Burbano R.R. et al. (2015) Expression analysis of genes involved in the RB/E2F pathway in astrocytic tumors. PLoS ONE 10, e0137259 10.1371/journal.pone.0137259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Torres-Martín M., Martinez-Glez V., Peña-Granero C., Isla A., Lassaletta L., De Campos J.M. et al. (2013) Gene expression analysis of aberrant signaling pathways in meningiomas. Oncol. Lett. 6, 275–279 10.3892/ol.2013.1363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kim Y.H., Lachuer J., Mittelbronn M., Paulus W., Brokinkel B., Keyvani K. et al. (2011) Alterations in the RB1 pathway in low‐grade diffuse gliomas lacking common genetic alterations. Brain Pathol. 21, 645–651 10.1111/j.1750-3639.2011.00492.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Llinas-Arias P. and Esteller M. (2017) Epigenetic inactivation of tumour suppressor coding and non-coding genes in human cancer: an update. Open Biol. 7, 170152 10.1098/rsob.170152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ku S.Y., Rosario S., Wang Y., Mu P., Seshadri M., Goodrich Z.W. et al. (2017) Rb1 and Trp53 cooperate to suppress prostate cancer lineage plasticity, metastasis, and antiandrogen resistance. Science 355, 78–83 10.1126/science.aah4199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Liu L., Ling X., Wu M., Chen J., Chen S., Tan Q. et al. (2017) Rb silencing mediated by the down‐regulation of MeCP2 is involved in cell transformation induced by long‐term exposure to hydroquinone. Mol. Carcinog. 56, 651–663 10.1002/mc.22523 [DOI] [PubMed] [Google Scholar]
- 62.Nakamura M., Watanabe T., Yonekawa Y., Kleihues P. and Ohgaki H. (2001) Promoter methylation of the DNA repair gene MGMT in astrocytomas is frequently associated with G: C→ A: T mutations of the TP53 tumor suppressor gene. Carcinogenesis 22, 1715–1719 10.1093/carcin/22.10.1715 [DOI] [PubMed] [Google Scholar]
- 63.Zacksenhaus E., Liu J., Jiang Z., Yao Y., Xia L., Shrestha M. et al. (2017) Transcription factors in breast cancer—lessons from recent genomic analyses and therapeutic implications. Adv. Prot. Chem. Struct. Biol. 107, 223–273 [DOI] [PubMed] [Google Scholar]
- 64.Chen P., Guo X., Zhang L., Zhang W., Zhou Q., Tian Z. et al. (2017) MiR-200c is a cMyc-activated miRNA that promotes nasopharyngeal carcinoma by downregulating PTEN. Oncotarget 8, 5206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Angadi P.V. and Krishnapillai R. (2007) Cyclin D1 expression in oral squamous cell carcinoma and verrucous carcinoma: correlation with histological differentiation. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 103, e30–e35 10.1016/j.tripleo.2006.09.011 [DOI] [PubMed] [Google Scholar]
- 66.Gautschi O., Ratschiller D., Gugger M., Betticher D.C. and Heighway J. (2007) Cyclin D1 in non-small cell lung cancer: a key driver of malignant transformation. Lung Cancer 55, 1–14 10.1016/j.lungcan.2006.09.024 [DOI] [PubMed] [Google Scholar]
- 67.Li J., Luo F., Zhang H., Li L. and Xu Y. (2014) The CCND1 G870A polymorphism and susceptibility to bladder cancer. Tumour Biol. 35, 171–177 10.1007/s13277-013-1021-7 [DOI] [PubMed] [Google Scholar]
- 68.Maia L., Breginski F., Cavalcanti T., de Souza R., Roxo V. and Ribeiro E. (2016) No difference in CCND1 gene expression between breast cancer patients with and without lymph node metastasis in a Southern Brazilian sample. Clin. Exp. Med. 16, 593–598 10.1007/s10238-015-0392-z [DOI] [PubMed] [Google Scholar]