Abstract
Purpose
The adult population is under-represented in existing ice hockey injury studies, despite the number of United States (US) adult ice hockey players increasing from 103,533 in 2007 to 180,400 in 2016 (74%). This study establishes trends in demographics, injury location, and injury type for adult ice hockey players (≥19 years old) in the United States.
Methods
The National Electronic Injury Surveillance System (NEISS) was queried for all ice hockey injuries from January 1, 2007 to December 31, 2016. Cases under age 19 were excluded. Each injury's narrative text field was reviewed to determine mechanism of injury.
Results
A total of 1,653 patients, representing an estimated 68,786 ice-hockey related injuries, presented to NEISS-participating US EDs. The most commonly injured body parts were the face (n = 12,432, 18.1%), head (n = 10,201, 14.8%), shoulder (n = 9,654, 14.0%) and ankle (n = 5,389, 7.8%). The most common diagnoses made were laceration (n = 18,153, 26.4%), strain/sprain (n = 12,202, 17.7%), fracture (n = 10,079, 14.7%), contusion (n = 9,283, 13.5%) and concussion (n = 4,794, 7.0%). The most common mechanisms of injury were falling (n = 11,786, 18.7%), puck contact (n = 10,544, 15.3%) and player contact (n = 9,449, 13.7%). Concussions increased from 46 in 2007 to 928 in 2016 (R2 = 0.8, β = 0.9, p < 0.001). Females (n = 1,852, 32%) had a higher proportion of head injuries than males (n = 8,349, 13.3%) (IPR = 2.4, p < 0.0001). The 50+ year old cohort showed a significant increase in injuries during the study period (n = 146 vs. 982, R2 = 0.75, β = 0.87, p = 0.001).
Conclusions
Despite changing trends in age and sex-related demographics, the majority of injuries in this population may be preventable with adequate enforcement of protective gear use. Increased education amongst players, coaches, trainers, orthopaedic surgeons and primary care physicians should be encouraged to minimize injuries.
Keywords: Adult athletes, Ice hockey, Injury epidemiology, Injury trends, Concussion, National electronic injury surveillance system, Level of evidence, Level III, Retrospective study
1. Introduction
The number of adult ice hockey players in the United States of America has increased over the last decade. USA Hockey, the governing body for the sport, saw a 74% increase in adult membership from 103,533 in 2007 to 180,400 in 2016. This rise is likely due to the increase of club hockey teams at the collegiate level as well as continued engagement by post-collegiate players. For most of the 20th century, college hockey was confined to leagues operating under the National Collegiate Athletic Association (NCAA) regulatory framework. While the number of NCAA teams and players has been stagnant since the 1990's, collegiate club hockey has experienced significant growth over that same time period. The American College Hockey Association (ACHA), the largest recognized conglomerate of collegiate club hockey, has grown from roughly 150 teams in the 1990s to more than 500 teams at present.1,2 The relatively new development of competitive club ice hockey has almost certainly exposed more players to the perils of full-contact ice hockey.
Additionally, the game of ice hockey has seen overall growth since the early 2000s, which is likely attributable to an increase in exposure of the game and improved access. The National Hockey League has established contracts with several major television broadcasting networks, which has introduced many more Americans to a once esoteric and cultish sport. Increased access to equipment, rinks, and ice time allowed more participants at the youth and adult levels to join the game, contributing to ice hockey's national growth in recent times.
With ice hockey being a perilous sport played at high speeds on thin blades of steel, the variety of injuries ranges from minor complaints (e.g. superficial lacerations, dehydration) to higher severity problems (e.g. long bone fractures, traumatic brain injuries). Junior hockey is played with a cadre of body armor. At the adult level, however, there are few leagues that mandate use of full equipment. Many post-collegiate players forgo face, shoulder, and mouth protection, making these areas more susceptible to injury. Exposed areas are subject to lacerations, contusions and abrasions. Joints may succumb to either traumatic dislocation or overuse injuries. Perhaps most importantly, hockey helmets are notoriously flimsy rendering the players’ heads less protected and at risk for concussions and coup/contrecoup-type injuries.3,4
The mechanism of injury has been shown to be directly related to the rules of competition. For example, in body-checking leagues, studies have shown a greater number of injuries, as well as an increase in the severity of those injuries, regardless of age or level of play (youth vs. adult, novice vs. elite).5, 6, 7, 8 Even in non-checking leagues, however, the game is not without risk. Incidental collisions and inadvertent falls contribute to the majority of injuries in leagues designed without contact.9 Overall, falls account for roughly 15–30% of all hockey injuries, with variation dependent on the level of competition.10,11
Despite the enormous growth in the adult ice hockey population, this demographic is underrepresented in existing hockey injury studies. The majority of research focuses primarily on elements at the youth level.12,13 Several studies examine injury-rates and types at the NCAA level but very few if any consider the entire college-age and post-graduate hockey population. Our study seeks to fill a void in the literature surrounding adult hockey injury epidemiology, by including populations that have been previously overlooked to provide more clarity on the burden and characteristics of injuries affecting adult ice hockey players. The goal of this study is to identify risk factors for injury in the adult hockey population and to provide data to guide education in primary injury prevention for players, coaches, trainers, orthopedic surgeons, and primary care physicians.
2. Materials and methods
2.1. Data sources
The National Electronic Injury Surveillance System (NEISS) provides a nationwide probability sample of injuries based on emergency department (ED) visits collected from a cohort of about 100 hospitals across the United States. The NEISS employs trained coders to review all ED records daily and log injury-related information in real time. Each NEISS hospital is assigned a sample weight to accurately represent the total number of representative cases across the country. Each hospital collects patient age, sex, race, date of visit, diagnosis category, injured body part, injury location, disposition, and a narrative text field for injury description.14
2.2. Subject selection
We evaluated all NEISS cases from January 1, 2007 to December 31, 2016 that included the product code for ice hockey (code 1279). Cases under the age of 19 are considered to be youth players by USA hockey rules and were excluded from the study.
2.3. Study variables
The demographic variables that we investigated included patient age, sex, and injured body part, as well as descriptive details included in the narrative text field. NEISS narratives were used to categorize the mechanism of injury into the following: (1) contact with boards, (2) falls, (3) player contact, (4) hit by puck, (5) skate, (6) hit by stick, and (7) other. In cases where player-to-player contact led to a fall or contact with boards, the mechanism of injury was categorized as player-to-player mechanism.
2.4. Statistical analysis
Descriptive statistics and statistical analyses were performed using SPSS version 24.0 (IBM® Corp., Armonk, New York). Injury proportion ratios (IPR) and 95% confidence intervals (95% CI) were achieved using one sample t-tests. Injury proportion ratios were calculated using the following formula: (e.g. number of female concussions - total number of female injuries)/(number of male concussions - total number of male injuries). Previously described by Knowles et al.,15 the IPR is useful in comparing injury proportion by cohort, thus providing more context for reported incidence rates. Comparisons of injury proportion by age group or sex were made with student's two sample t-tests with 95% CI. Temportal trend analyses were performed using linear regression models. Student's t-tests were two-tailed and the threshold for significance was set at a p-value of 0.05.
2.5. Ethical considerations
This study was deemed exempt by the institutional review board of the corresponding author, due to the de-identified and publicly available nature of NEISS data.
3. Results
3.1. National estimate of cases
From 2007 through 2016, 1,653 patients presented to NEISS-participating emergency departments with ice hockey related injuries. These patients represented an estimated 68,786 total ice hockey related injuries. The majority of injuries occurred in males (n = 62,990, 92% vs. n = 5,796, 8%). The most commonly injured age group was the youngest cohort studied, aged 19–25 years old (n = 31,385, 46%), with the proportion of injuries decreasing as age increased: 26–35 years old (n = 17,196, 25%), 36–49 years old (n = 13,960, 20%), and 50+ years old (n = 5,280, 8%) (Table 1).
Table 1.
Patients with ice hockey injuries presenting to US Emergency Departments by age and sex, 2007–2016, per the National Electronic Injury Surveillance System (NEISS).
| Characteristics | Unweighted Case Count, n (%) | National Estimates, n (%) | 95% Confidence Interval |
|---|---|---|---|
| Age Group (years) | |||
| 19–25 | 714 (43.2) | 31,385 (45.6) | 30,402–33,558 |
| 26–35 | 433 (26.2) | 17,196 (25.0) | 15,965–18,403 |
| 36–49 | 385 (23.3) | 13,960 (20.3) | 13,798–16,043 |
| 50+ | 121 (7.3) | 5,280 (7.7) | 4,605–5,953 |
| Sex | |||
| Male | 1,485 (90.0) | 62,990 (91.6) | 60,707–65,263 |
| Female | 164 (10.0) | 5,795 (8.4) | 5,105–6,485 |
| Total | 1,653 (100.0) | 68,786 (100.0) | 66,401–71,162 |
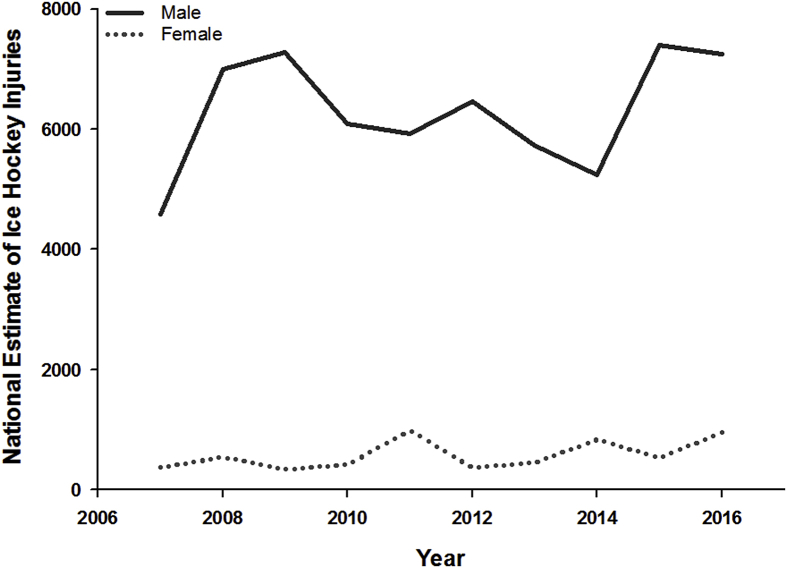
The estimated national incidence of patients with ice hockey injuries presenting to the emergency department increased 65% from 4,956 in 2007 to 8,201 in 2016, although this change was not significant (p = 0.21). The 26–35 year old cohort experienced a 94% increase in annual visits over that same 10-year period, though also not statistically significant (1,337 vs. 2,603, R2 = 0.19, β = 0 .43, p = 0.20). The 50+ year old cohort did show a significant increase in injuries during the study period (n = 146 vs. 982, R2 = 0.75, β = 0.87, p = 0.001). Female hockey injuries also showed an upward trend, increasing from 369 in 2007 to 955 in 2016, though not significant (R2 = 0.32, β = 0.57, p = 0.085) (Fig. 1).
Fig. 1.
National estimates of ice hockey injuries among adult players from 2007 to 2016 by sex.
3.2. Injury characteristics
Nearly all patients were treated and discharged from the emergency department (>99%), with 350 (0.005%) patients admitted to the hospital. The most commonly injured body parts were the face (n = 12,432, 18.1%), head (n = 10,201, 14.8%), shoulder (n = 9,654, 14.0%) and ankle (n = 5,389, 7.8%). The most common diagnoses made were laceration (n = 18,153, 26.4%), strain/sprain (n = 12,202, 17.7%), fracture (n = 10,079, 14.7%), contusion (n = 9,283, 13.5%) and concussion (n = 4,794, 7.0%). The most common mechanisms of injury overall were falling (n = 11,786, 18.7%), puck contact (n = 10,544, 15.3%) and player contact (n = 9,449, 13.7%) (Table 2). The most common injury was facial laceration (n = 10,614) accounting for 58.4% of lacerations and 85% of facial injuries. The most common sprain/strain injuries were of the shoulder (n = 3,750) and ankle (n = 2,027). Fractured body parts varied widely: ankle (n = 2,107; mean age = 40yo), hand/finger n = 1,275; mean age 31yo), face (n = 1,271; mean age = 30yo) and wrist (n = 1,010, mean age = 51yo).
Table 2.
Patients with ice hockey injuries presenting to US Emergency Departments, 2007–2016: mechanism of injury by body site and diagnosis (n = 68,786), per the National Electronic Injury Surveillance System (NEISS).
| Characteristics | Mechanism of Injury, % |
|||||||
|---|---|---|---|---|---|---|---|---|
| Falls | Contact with Boards | Contact with Stick | Player-Player Contact | Contact with Puck | Contact with Skate | Other/Unknown | Total | |
| Body Site | ||||||||
| Head | 21.0 | 32.0 | 9.3 | 18.2 | 0.8 | 3.2 | 15.5 | 100.0 |
| Neck | 14.5 | 31.4 | 9.5 | 8.4 | 0.0 | 12.2 | 24.0 | 100.0 |
| Face/Mouth | 6.4 | 11.9 | 2.8 | 33.5 | 3.1 | 20.9 | 21.4 | 100.0 |
| Shoulder | 32.9 | 27.0 | 15.1 | 0.8 | 0.0 | 0.0 | 24.1 | 100.0 |
| Elbow | 63.9 | 4.0 | 5.5 | 0.0 | 0.6 | 2.2 | 23.8 | 100.0 |
| Wrist | 38.8 | 4.0 | 7.6 | 6.6 | 3.4 | 1.1 | 38.4 | 100.0 |
| Hand/Fingers | 16.5 | 8.5 | 7.1 | 16.6 | 10.7 | 11.5 | 29.1 | 100.0 |
| Trunk | 14.3 | 26.5 | 13.8 | 5.6 | 1.0 | 0.9 | 37.8 | 100.0 |
| Knee | 21.5 | 11.7 | 1.7 | 2.2 | 5.7 | 0.0 | 57.2 | 100.0 |
| Ankle | 17.0 | 3.9 | 4.3 | 17.0 | 2.6 | 1.2 | 54.0 | 100.0 |
| Foot | 6.3 | 11.3 | 5.9 | 46.4 | 6.8 | 4.9 | 18.4 | 100.0 |
| Diagnosis | ||||||||
| Concussion | 22.0 | 39.7 | 9.4 | 11.5 | 1.6 | 2.5 | 13.4 | 100.0 |
| Contusion, Abrasion | 15.9 | 22.6 | 9.6 | 20.9 | 0.2 | 8.0 | 22.8 | 100.0 |
| Dislocation | 44.9 | 12.2 | 12.1 | 1.4 | 0.0 | 0.0 | 29.4 | 100.0 |
| Fracture | 32.7 | 12.6 | 9.5 | 15.1 | 1.0 | 1.4 | 27.6 | 100.0 |
| Laceration | 7.8 | 10.6 | 2.0 | 26.6 | 10.9 | 18.4 | 23.6 | 100.0 |
| Internal Organ Injury | 22.3 | 26.7 | 12.8 | 16.6 | 0.0 | 2.9 | 18.6 | 100.0 |
| Strain or Sprain | 23.1 | 16.7 | 8.8 | 1.7 | 1.1 | 1.0 | 47.6 | 100.0 |
3.3. Age-specific characteristics
Injury location and diagnosis differed with age (Table 3). Lacerations were the most common diagnosis in the 19–25 year old (n = 8,750, 27.9%), 26–35 year old (n = 5,409, 31.5%) and 36–49 year old (n = 3,291, 22.1%) cohorts. Comparatively, lacerations accounted for a lesser proportion of injuries amongst 50+ players (n = 703, 13.3%) (19–35 vs 50+; IPR = 2.1; 95%CI, 1.4–3.42, p < 0.001), and more specifically, the proportion of lacerations was significantly higher in the 26–35 year old cohort as compared to the 36–49 year old cohort (IPR = 1.42; 95%CI, 1.1–1.8, p < 0.01). The proportion of fracture injuries was higher in players 36+ (n = 4,229, 21.4%) than 19–35 (5,850, 12%) (19–35 vs 36+: IPR = 1.8, 95%CI, 1.3–2.3, p < 0.001).
Table 3.
Patients with ice hockey injuries presenting to US emergency departments by age, 2007–2016: body site, diagnosis and mechanism of injury, per the National Electronic Injury Surveillance System (NEISS).
| Characteristics | Age Group (n), % |
||||
|---|---|---|---|---|---|
| Overall (n = 68,786), % | 19 to 25y (n = 31,385), % | 26 to 35y (n = 17,196), % | 36 to 50y (n = 14,924), % | >50y (n = 5,280), % | |
| Body Site | |||||
| Head | 14.8 | 19.1 | 10.3 | 9.2 | 19.8 |
| Neck | 1.9 | 1.8 | 1.7 | 2.1 | 2.3 |
| Face/Mouth | 22.4 | 23.1 | 26.4 | 19.1 | 14.2 |
| Shoulder | 14.0 | 13.2 | 14.7 | 14.6 | 15.4 |
| Elbow | 4.0 | 3.8 | 4.6 | 3.7 | 4.1 |
| Wrist | 4.0 | 4.4 | 3.4 | 4.5 | 2.5 |
| Hand/Finger | 4.3 | 3.2 | 2.4 | 2.1 | 1.1 |
| Trunk | 9.4 | 6.8 | 10.4 | 11.3 | 15.3 |
| Knee | 5.1 | 4.2 | 6.2 | 6.9 | 1.3 |
| Ankle | 7.8 | 6.8 | 6.9 | 9.0 | 13.6 |
| Foot | 1.8 | 1.4 | 1.3 | 4.0 | 0.0 |
| Diagnosis | |||||
| Concussion | 7.0 | 10.1 | 5.1 | 4.9 | 0.3 |
| Contusion, Abrasion | 13.5 | 14.2 | 16.6 | 10.5 | 7.6 |
| Dislocation | 4.9 | 4.0 | 4.1 | 5.9 | 10.2 |
| Fracture | 14.7 | 11.2 | 13.5 | 20.4 | 22.4 |
| Laceration | 26.4 | 27.9 | 31.5 | 22.1 | 13.3 |
| Internal Organ Injury | 6.6 | 6.8 | 4.6 | 3.9 | 18.7 |
| Strain or Sprain | 17.7 | 19.0 | 14.1 | 20.8 | 13.2 |
| Mechanism of Injury | |||||
| Fall | 20.2 | 18.2 | 19.1 | 25.3 | 21.5 |
| Contact with Boards | 7.7 | 7.5 | 8.3 | 7.5 | 7.9 |
| Contact with Stick | 7.0 | 7.0 | 7.9 | 6.4 | 5.6 |
| Player-Player Contact | 16.8 | 18.8 | 16.7 | 15.6 | 9.3 |
| Contact with Puck | 15.5 | 12.8 | 15.7 | 15.6 | 31.0 |
| Contact with Skate | 3.4 | 4.1 | 4.2 | 1.9 | 0.6 |
| Other/Unknown | 29.3 | 31.5 | 28.1 | 27.7 | 24.4 |
The face was the most commonly injured body location in the 19–25 year old (n = 5,911, 18.8%), 26–35 year old (n = 3,750, 21.8%), and 36–49 year old (n = 2,222, 14.9%) cohorts, whereas the 50+ year old cohort experienced a significantly lower proportion of facial injuries (n = 550, 10.4%) (19–49 vs 50+; IPR = 1.8; 95%CI, 1.1–3.8, p = 0.02).
The proportion of shoulder injuries was essentially equal across all age groups (19–25: 13.2%, 26–35: 14.7%, 36–50: 14.6%, 50+: 15.4%). Similarly, head injuries were a top three injury site in all age groups, with a slight predominance to the youngest and oldest players: 19–25 (n = 6,007, 19.1%), 26–35 (n = 1,771, 10.3%), 36–49 (n = 1,378, 9.2%), 50+ (n = 1,045, 19.8%). The 19–25 age group did have a significantly higher proportion of head injuries than the 26–35 (IPR = 1.9; 95%CI, 1.3–2.75, p < 0.001) and 36–49 groups but not the 50+ cohort.
The mechanism of injury was generally consistent across age cohorts, with falls (μ = 20.2%, range: 18.2–25.3%), board contact (μ = 7.7%, range: 7.5–8.3%), and stick-related (μ = 7.0%, range: 5.6–7.9%) injuries being equally common. However, the 50+ year old cohort (n = 493, 9.3%) had a significantly lower proportion of injuries caused by player contact than did all the younger cohorts combined (19–49 years old, n = 11,077, 16.1%)(IPR = 1.7; 95% CI, 1.17–3.65, p < 0.05), and the 50+ group (n = 1,637, 31%) had a higher proportion of puck mechanism injuries than the 19–49 group (n = 9,034, 14.7%) (50+ vs. 19–49: IPR = 2.1; 95%CI, 1.1–3.8, p < 0.001).
3.4. Sex-specific characteristics
The data showed that females (n = 1,852, 32%) had a higher proportion of head injuries than males (n = 8,349, 13.3%) (IPR = 2.4; 95%CI, 1.7–3.3, p < 0.001); and conversely, males (n = 12,129, 19.3%) experienced a greater proportion of facial injuries than females (n = 303, 5.2%) (IPR = 3.7; 95%CI, 2.0–13.3, p < 0.01).
Males (n = 17,681, 28.1%) were found to have suffered more than three times the proportion of laceration injuries as females (n = 472, 8.1%) (IPR = 3.5; 95%CI, 2.3–6.2, p < 0.001); whereas females (n = 829, 14.3%) had more than double the proportion of concussion diagnoses as males (n = 3,965, 6.3%) (IPR = 2.3, 95%CI = 1.3–3.5, p < 0.001).
Further, mechanism of injury varied by sex. The top three injury mechanisms for females were falls (29.5%), puck contact (24.3%) and player contact (11.1%). For males, the top three mechanisms were falls (19.3%), player contact (17.3%) and puck contact (14.7%). Although not a top injury mechanism, males experienced more than three times the proportion of stick injuries (n = 4,712, 7.5%) than females (n = 110, 1.9%) (IPR = 3.9, 95%CI = 1–169, p = 0.07).
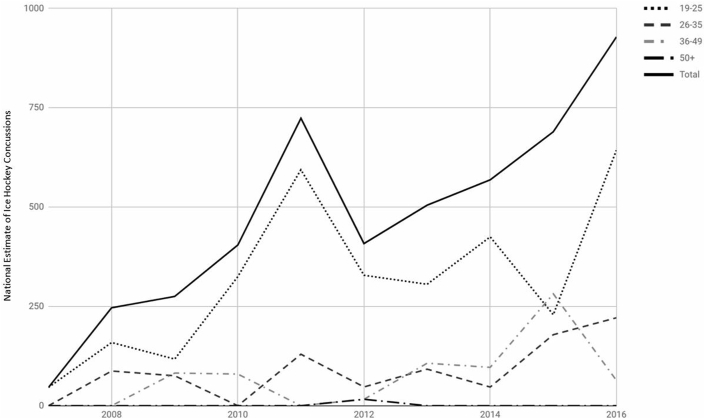
3.5. Head injuries
The incidence of concussions increased from 46 in 2007 to 928 in 2016 (p < 0.001, R2 = 0.8, β = 0.9) (Fig. 2). This increase was driven mostly by the younger age cohorts (19–25, 26–35; both p < 0.05); however, the proportion of concussions was significantly higher in the 19–25 year old group than the 26–35 year old group (IPR = 2.0; 95% CI = 1.2–3.6, p < 0.001). There were only 16 reported concussions in the 50+ year old cohort during the study period.
Fig. 2.
National estimates of concussions among adult ice hockey players from 2007 to 2016 by age group.
4. Discussion
This study examined the burden and nature of injuries affecting an often-overlooked population – US adult hockey players. The game of ice hockey has evolved significantly over the past fifteen years to adapt to safer play. For example, rule changes, specifically USA Hockey Rule 620 – ‘head contact is the action of a player contacting an opponent in the head, face or neck with any part of the player's body, equipment or stick, penalized with a minor/major plus a game misconduct’ – have sought to make the game safer by outlawing illegal head contact.6,16,17 Additionally, hockey equipment has evolved over the past decade, with more substantial body padding and advances in helmet technology (the focus of much media attention) to safeguard against concussions.3,18,19 However, it is difficult to determine whether these attempts towards a safer game have extended beyond the NHL, NCAA, and USA Hockey, to include men's or women's adult league or club hockey competition. Most injuries captured by this study occurred in recreational leagues outside the well-studied spheres of organized hockey mentioned above, which suggests that the information gleaned in this study may be used to improve the safety in these leagues.
Despite a significant increase in age 50+ cohort injuries during the study period, the total number of injuries decreased progressively with age. These findings may be due to the fact that the game becomes less intense as players age. Other authors have shown that for athletes in all sports and the general population, age-related muscle atrophy begins at approximately 50 years of age and performance decreases are observed before the onset of muscle fiber loss.21 A slower pace of play may mitigate the mechanisms of injury seen throughout the sport as older players skate at slower velocities, which reduces the impact of collisions and falls. The decrease in the proportion of injuries seen as player age increased may also be explained by the fact that there are less active players with increasing age, or perhaps by a lower level of competition. Participation by older players may be driven less by competition than an interest in cardiovascular exercise or the sense of community offered by a hockey team. We suggest a survey-based approach to determine what, if any, biopsychosocial differences between younger and older players may be contributing to differences in injury rates.
Conversely, this study noted an overall uptrend in adult female hockey injuries. This trend is most likely related to the increasing popularity of ice hockey in the United States, with a particular increase in female hockey participation over the study period. The growing population of female hockey players has been well documented. USA Hockey reported a 34% increase in female adult membership from 13,690 in 2007 to 18,335 in 2016.21 As membership and participation continue to expand, this study will help guide players, coaches, and physicians on the increasing importance of recognizing risks and continuing preventative education.
Clinicians should encourage the use of protective equipment for the face and mouth as our findings show that the face is the most commonly injured body part. Although NEISS does not collect data on the use of protective equipment, full face shield and mouth guards have been shown to be effective at preventing the majority of ice hockey injuries to the face when worn appropriately.22 Our results suggest that protective equipment may either be worn improperly or may be not worn at all, particularly in the younger age cohorts. The rate of mouthguard use among the adult hockey population is not known but survey-based studies of high school and college players estimate that mouthguard utilization varies between 20% and 80% depending on practice or game environments and league or team-wide rule enforcement. Hootman et al. reported that 20% of recreational hockey players were not using facial protection at the time of injury.23 A study of 8,741 NHL players over 10 seasons found there was a significantly increased risk of eye or orbital injury when a visor was not worn (OR 4.23, 95% CI 2.84–6.30).24 Data collected in this study showed that facial lacerations accounted for the most common injury type across all the younger cohorts. This may be attributable to the decreasing intensity of play as age increases, or perhaps a more brazen attitude with regard to equipment amongst younger players. USA Hockey may consider raising awareness by introducing educational material around hockey rinks or mandating the use of protective gear – especially face masks - at sanctioned facilities.
There was a stunning rise in head injuries over the study period. This increase follows a general trend of increased incidence of head injuries in the United States since at least 2001. Coronado et al. observed a 120% increase in adult (>19 year old) sport- and recreational-related concussions presenting to US emergency departments between 2001 and 2012.25 Likewise, Taylor et al.26 observed greater than a 47% increase concussions presenting to US emergency departments across all adult cohorts from 2007 to 2013. The increased incidence of head injuries can likely be explained by heightened public awareness of signs and symptoms of concussions, with greater oversight and surveillance of head injuries by players, families, coaches, and team trainers.27,28 There is no current data on helmet use rates among US adult hockey players but our study suggests that rates may be substantially lower than 100%. Our study bolsters players, coaches and clinicians advocating for greater utilization of existing helmets and further advancements in helmet technology.
The proportion of concussion diagnoses was two times greater in females than in males. These findings are consistent with those of previous studies, which have consistently showed that women have a 1.2–2.0-fold increase in concussions per athletic exposure.27,28 Studies differ, however, on the reason for the greater incidence of concussions in females. In NCAA players wearing instrumented helmets – specially designed and equipped with impact sensors – head impacts between females were less common and were shown to have less magnitude and peak linear acceleration compared males.27,28 This data implies a lower threshold of force in the development of concussion amongst women as compared to men. Our work supports the pursuit of neurobiological factors as potential contributors to perceived lower concussive thresholds in women as compared to men.
The findings in this study are subject to several limitations. First, this study does not include data on patients who did not seek care related to an ice hockey injury formally at an emergency department. Therefore, visits to primary care physicians, urgent care centers, or other outpatient facilities were missed in this analysis. Thus, the case volume of ice hockey injuries as represented by the NEISS-participating emergency department registry would grossly underestimate the true incidence of annual cases nationally. Additionally, this analysis is unable to qualify the clinical severity of included ice hockey injuries, as the NEISS national database includes exclusively demographic and minimally descriptive data on each case. Furthermore, with any national database registry study that includes a large volume of cases, overpowering analyses threaten the meaningfulness of statistically significant differences. Despite these limitations, the use of a national database yields the most comprehensive representation of injuries in the adult ice hockey population across the country.
There is a paucity of current literature available on the epidemiology and trends of adult ice hockey injuries in the United States. This study utilized a national database registry of emergency room visits to show that ice hockey injuries vary by age and sex, and the overall incidence of adult ice hockey injuries has increased on an annual basis on average, with a significant increase in the incidence of head injuries, disproportionately affecting the female population more significantly. Adult ice hockey safety may be improved by utilizing this data to increase player education, heighten awareness of injuries, and amend regulations regarding protective equipment. Further research should be pursued to understand specific trends and differences in an effort to make the game safer, with specific focus on the increasing frequency of head injuries.
Source of funding
No sources of internal or external funding were sought after or utilized for completion of any aspect of this study. No conflicts of interest influenced any aspect of this study.
Declaration of competing interest
All of the co-authors report no financial conflicts of interest to disclosure.
References
- 1.Smith J. ACHA celebrating nearly 30 Years of competitive college hockey. https://www.usahockey.com/news_article/show/940942 Rediline Editorial Inc.
- 2.Decker D. The rise of the American college hoceky association. http://achahockey.org/view/achahockey/acha-hockey-news/news_467345 Letsplayhockey.org.
- 3.Rowson B., Rowson S., Duma S.M., Hockey S.T.A.R. A methodology for assessing the biomechanical performance of hockey helmets. Ann Biomed Eng. 2015;43(10):2429–2443. doi: 10.1007/s10439-015-1278-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clark J.M., Post A., Hoshizaki T.B., Gilchrist M.D. Protective capacity of ice hockey helmets against different impact events. Ann Biomed Eng. 2016;44(12):3693–3704. doi: 10.1007/s10439-016-1686-3. [DOI] [PubMed] [Google Scholar]
- 5.Cusimano M.D., Taback N.A., McFaull S.R., Hodgins R., Bekele T.M., Elfeki N. Effect of bodychecking on rate of injuries among minor hockey players. Open Med. 2011;5(1):57–64. [PMC free article] [PubMed] [Google Scholar]
- 6.Donaldson L., Asbridge M., Cusimano M.D. Bodychecking rules and concussion in elite hockey. PLoS One. 2013;8(7):3–8. doi: 10.1371/journal.pone.0069122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Macpherson A. Body-checking rules and childhood injuries in ice hockey. Pediatrics. 2006;117(2):e143–e147. doi: 10.1542/peds.2005-1163. [DOI] [PubMed] [Google Scholar]
- 8.Trofa D.P., Park C.N., Noticewala M.S., Lynch T.S., Ahmad C.S., Popkin C.A. The impact of body checking on youth ice hockey injuries. Orthop J Sport Med. 2017;5(12):4–7. doi: 10.1177/2325967117741647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Darling S.R., Schaubel D.E., Baker J.G., Leddy J.J., Bisson L.J., Willer B. Intentional versus unintentional contact as a mechanism of injury in Youth ice hockey. Br J Sports Med. 2011;45(6):492–497. doi: 10.1136/bjsm.2009.063693. [DOI] [PubMed] [Google Scholar]
- 10.Deits J., Yard E.E., Collins C.L., Fields S.K., Comstock R.D. Patients with ice hockey injuries presenting to US emergency departments, 1990-2006. J Athl Train. 2010;45(5):467–474. doi: 10.4085/1062-6050-45.5.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flik K., Lyman S., Marx R.G. American collegiate men's ice hockey: an analysis of injuries. Am J Sports Med. 2005;33(2):183–187. doi: 10.1177/0363546504267349. [DOI] [PubMed] [Google Scholar]
- 12.Emery C.A., Hagel B., Decloe M., Carly M. Risk factors for injury and severe injury in youth ice hockey: a systematic review of the literature. Inj Prev. 2010;16(2):113–118. doi: 10.1136/ip.2009.022764. [DOI] [PubMed] [Google Scholar]
- 13.MacCormick L., Best T.M., Flanigan D.C. Are there differences in ice hockey injuries between sexes? A systematic review. Orthop J Sport Med. 2014;2(1):1–7. doi: 10.1177/2325967113518181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schroeder T., Ault K. DC US Consum Prod Saf Comm; Washington: 2001. The NEISS Sample (Design and Implementation) 1997-present. (June) [Google Scholar]
- 15.Knowles S.B., Kucera K.L., Marshall S.W. The injury proportion ratio: What’s It All About? 2010;45(5):475–477. doi: 10.4085/1062-6050-45.5.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith A.M., Stuart M.J., Dodick D.W., Sorenson M.C., Finnoff J.T., Krause D. 2010. Zero Tolerance for Concussions and Other Neurotrauma in Ice Hockey: Rationale for Collaborative Action. Ice Hockey Summit Action Concussion; pp. 1–43. internal-pdf://rationale_collaborative_action-1242275905/Rationale_Collaborative_Action.pdf. [Google Scholar]
- 17.Smith A.M., Stuart M.J., Greenwald R.M. Proceedings from the ice hockey summit on concussion: a call to action. Curr Sports Med Rep. 2011;10(4):241–247. doi: 10.1249/JSR.0b013e318224624a. [DOI] [PubMed] [Google Scholar]
- 18.Emery C.A., Black A.M., Kolstad A. What strategies can be used to effectively reduce the risk of concussion in sport? A systematic review. Br J Sports Med. 2017;51(12):978–984. doi: 10.1136/bjsports-2016-097452. [DOI] [PubMed] [Google Scholar]
- 19.Virani S., Russell C.N., Bruschetta M.L. The effect of shoulder pad design on head impact severity during checking. Med Sci Sports Exerc. 2017;49(3):573–580. doi: 10.1249/MSS.0000000000001136. [DOI] [PubMed] [Google Scholar]
- 21.No Title USA Hockey National Registration Reports. https://www.usahockey.com/membershipstats
- 22.Covassin T., Moran R., Elbin R.J. Sex differences in reported concussion injury rates and time loss from participation: an update of the national collegiate athletic association injury surveillance program from 2004-2005 through 2008-2009. J Athl Train. 2016;51(3):189–194. doi: 10.4085/1062-6050-51.3.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hootman J.M., Dick R., Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42(2):311–319. doi: 10.1111/j.1600-0838.2006.00528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Micieli J.A., Zurakowski D., Ahmed I.I.K. Impact of visors on eye and orbital injuries in the National Hockey League. Can J Ophthalmol. 2014;49(3):243–248. doi: 10.1016/j.jcjo.2014.03.008. [DOI] [PubMed] [Google Scholar]
- 25.Chen J.E., Glover G.H. HHS public access. 2016;25(3):289–313. doi: 10.1007/s11065-015-9294-9. (Functional) [DOI] [Google Scholar]
- 26.Taylor C.A., Bell J.M., Breiding M.J., Xu L. Traumatic brain injury-related emergency department visits, hospitalizations, and deaths - United States, 2007 and 2013. MMWR Surveill Summ. 2017;66(9):1–16. doi: 10.15585/mmwr.ss6609a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stead T.S., Rastogi V., Hedna V.S., Ganti L. Awareness of the CDC “heads up!” to youth sports campaign among pediatric sports coaches: a pilot survey study. Cureus. 2016;8(8) doi: 10.7759/cureus.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smith A.M., Stuart M.J., Roberts W.O. Concussion in ice hockey. Clin J Sport Med. 2017;27(5):1. doi: 10.1097/JSM.0000000000000412. [DOI] [PubMed] [Google Scholar]