Abstract
Purpose
Periprosthetic femoral fractures are difficult to treat, but few reports have included many periprosthetic femoral fractures. The purpose of this study was to investigate the trends and characteristics of a large number of periprosthetic femoral fractures and to determine the best treatment strategy for such fractures.
Methods
The fracture type according to the Vancouver classification, the stem fixation style of previous surgery, the elapsed time from previous surgery, and the treatment method for periprosthetic fractures of 51 patients with periprosthetic femoral fractures who were seen between 2006 and 2018 were investigated.
Results
The types of fractures according to the Vancouver classification were: type A 5.9%, type B1 47%, type B2 20%, type B3 2.0%, and type C 25%. Of the previous surgeries, 76% were cementless fixation, and 24% were cemented fixation. The mean duration from previous surgery to periprosthetic femoral fracture was 8 years and 7 months (1–358 months), and injury within 1 year from previous surgery was most commonly observed (24%). As treatment for periprosthetic femoral fractures, conservative treatment was performed in 8%, and surgery was performed in 92%. Of the surgery cases, 53% underwent osteosynthesis, and 39% underwent revision surgery. Of type B1 surgery cases, 58% were treated with osteosynthesis, and 33% underwent revision surgery, although type B1 had no stem loosening.
Conclusion
Many periprosthetic femoral fractures occurred within 1 year after the previous surgery. Therefore, preventive measures for periprosthetic femoral fractures should be started immediately after total hip replacement. In addition, revision surgery was performed even if the stem was not loosened in cases where it was judged that sufficient osteosynthesis could not be performed.
Keywords: Periprosthetic femoral fracture, Total hip replacement, Femoral neck replacement, Revision arthroplasty, Vancouver classification
1. Introduction
With the recent growth in the number of older people, the number of patients undergoing total hip replacement (THR) and femoral head replacement (FHR) has been increasing. Furthermore, the aging of patients who have undergone these operations has resulted in an increase in periprosthetic fractures.1
Periprosthetic fractures, especially periprosthetic femoral fractures after THR or FHR, make it difficult to install osteosynthesis implants because of the implants already in the bone. In addition, bone healing is difficult to obtain because the contact area between bones is very small. Thus, periprosthetic femoral fractures are often difficult to treat.
Despite that, because there are few comprehensive reports of periprosthetic femoral fractures, it is not yet clear what kind of patient is prone to periprosthetic femoral fracture and what type of treatment is being used for what type of periprosthetic femoral fracture.
Because periprosthetic femoral fracture is a disease that significantly reduces patients’ quality of life, its prevention is very important. To investigate what kind of patient is at risk of a periprosthetic femoral fracture is important in considering the target group for prevention.
It is also difficult to know how to treat patients who have suffered such fractures around the femoral stem. The first step in considering an ideal treatment for the periprosthetic femoral fracture is to investigate what type of treatment is actually applied to which type of periprosthetic femoral fracture.
Therefore, the purpose of this study was to investigate which patients are more likely to develop periprosthetic femoral fractures and what types of treatments are applied to which types of periprosthetic femoral fractures.
2. Materials and methods
The subjects were 51 patients with periprosthetic femoral fractures who were taken to 8 general hospitals from March 2006 to March 2018. There were 12 men and 39 women, with a mean age of 78 years (range: 43–91 years). The assessment criteria were: the fracture type on the Vancouver classification,2 the type of previous surgery, the type of stem fixation procedure at previous surgery, the duration from previous surgery to periprosthetic femoral fracture, and the treatment method for periprosthetic femoral fractures.
3. Results
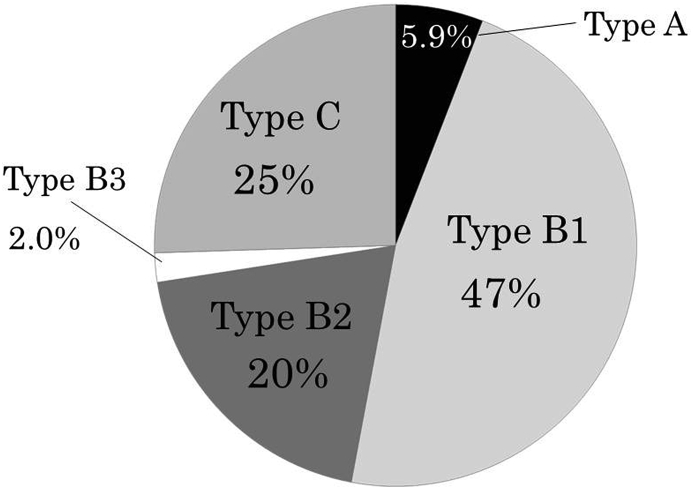
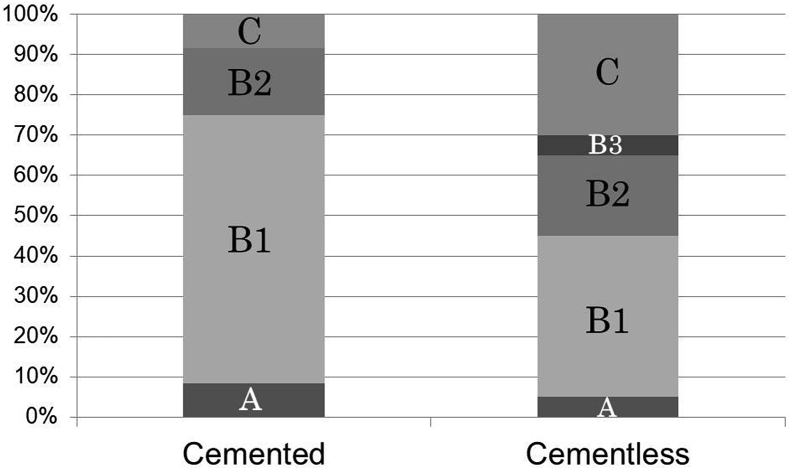
The types of fractures according to the Vancouver classification were: type A (n = 3, 5.9%), type B1 (n = 24, 47%), type B2 (n = 10, 20%), type B3 (n = 1, 2.0%), and type C (n = 13, 25%); approximately half of the fractures were type B1 (Fig. 1).
Fig. 1.
The types of fractures according to the Vancouver classification.
Approximately half of the fractures are Type B1.
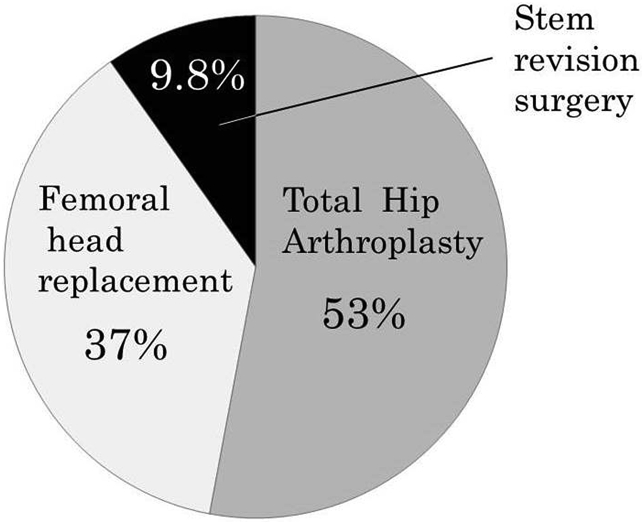
Previous surgeries were THR (n = 27, 53%), FHR (n = 19, 37%), and stem revision surgery (n = 5, 9.8%) (Fig. 2).
Fig. 2.
The kind of previous surgeries before the periprosthetic femoral fractures.
Periprosthetic fractures after stem revision surgeries are close to 10% and are relatively frequent.
Of the previous surgeries, 76% were cementless fixation, and 24% were cemented fixation (Fig. 3).
Fig. 3.
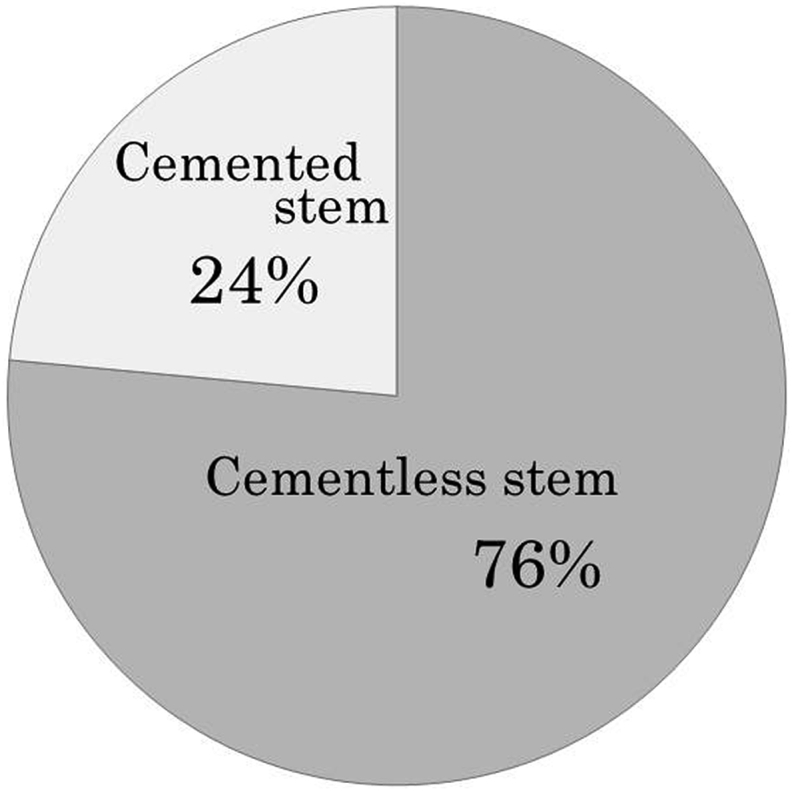
The fixation methods of the stem in previous surgeries.
Of the previous surgeries, three-quarters used cementless fixation, while one-quarter used cemented fixation.
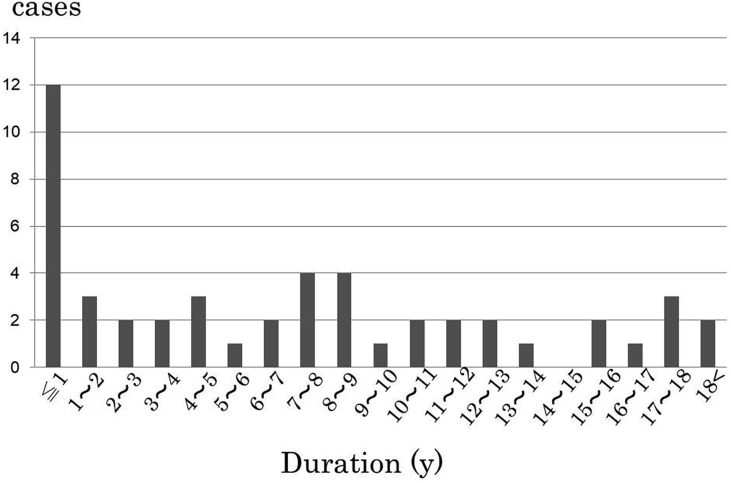
The mean duration from previous surgery to periprosthetic femoral fracture was 8 years and 7 months (range: 1–358 months), and injury within 1 year from previous surgery was most commonly observed (24%) (Fig. 4).
Fig. 4.
The duration from previous surgery to periprosthetic femoral fractures.
The mean duration from previous surgery to periprosthetic femoral fractures is 8 years and 7 months (range: 1–358 months), and injury within 1 year from previous surgery is most commonly observed (24%).
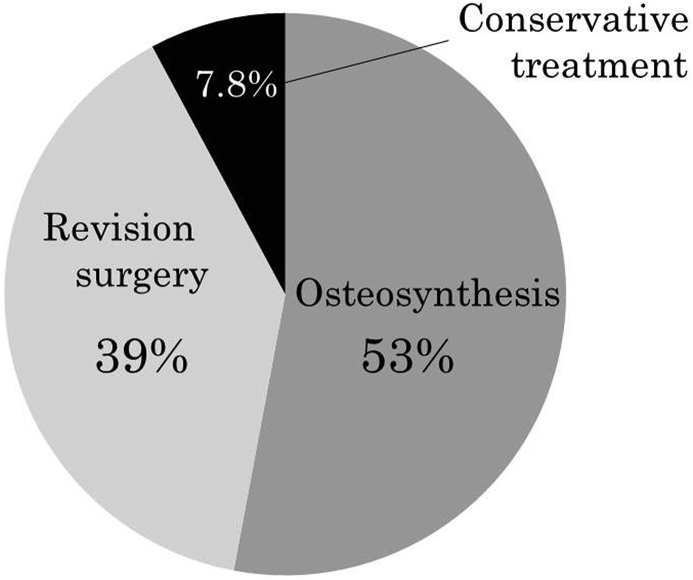
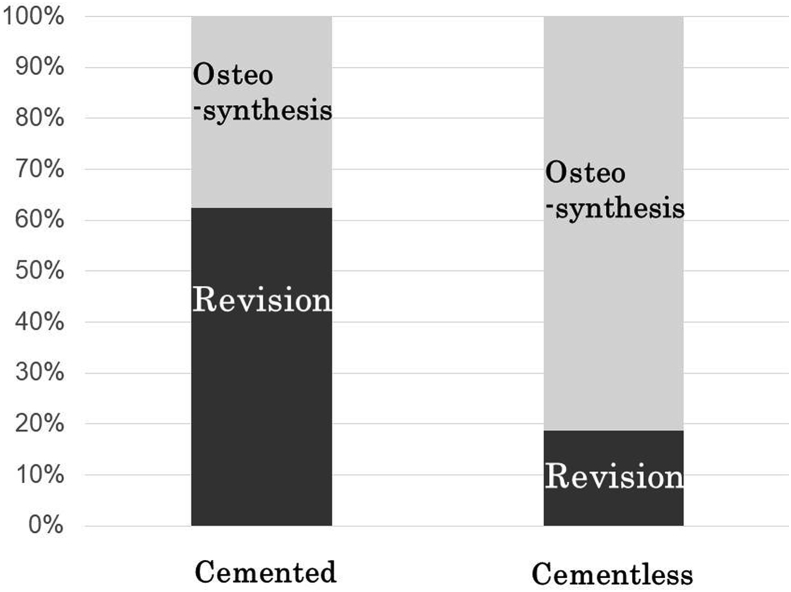
As treatment for periprosthetic femoral fractures, conservative treatment was performed in 8%, and surgery was performed in 92%. Of the surgery cases, 53% underwent osteosynthesis, and 39% underwent revision surgery (Fig. 5).
Fig. 5.
Treatment for periprosthetic femoral fractures.
Conservative treatment was performed in 8% and surgery was performed in 92%. Of the surgery cases, 53% underwent osteosynthesis and 39% underwent revision surgery.
Only 3 cases were classified as Vancouver type A, of which 1 case underwent osteosynthesis, and 2 underwent conservative treatment.
For Vancouver type B1, 9% underwent conservative treatment, and 91% underwent surgery. Among type B1 surgery cases, 58% were treated with osteosynthesis, and 33% underwent revision surgery, although type B1 had no stem loosening. Type B1 cases tended to have many cemented stem cases (Fig. 6), and revision surgery was selected in significantly more cases for type B1 cases with a cemented stem than for type B1 cases with a cementless stem (P = 0.0321) (Fig. 7).
Fig. 6.
Percentages of Vancouver classifications in cemented and cementless stems.
Vancouver type B1 is the most common in peri-cemented stem femoral fractures.
Fig. 7.
Treatment type in Type B1 fractures.
Revision surgery was selected in significantly more cases for Type B1 cases with a cemented stem than for Type B1 cases with a cementless stem (P = 0.0321).
Revision surgery was selected for all type B2 and type B3 cases where the stems were determined to be loose.
For Vancouver type C, 92% underwent osteosynthesis, and 8% underwent revision surgery. All cases that underwent revision surgery were cemented stem cases.
4. Discussion
The periprosthetic femoral fracture is definitely a major problem for both patients and the healthcare system, and it is one of the biggest complications after THR and FHR.3 On the one hand, it is also difficult to treat these fractures. Thus, the prevention of periprosthetic femoral fractures is also important.
Age over 60 years, osteoporosis, and prior revision surgery have been reported as the risk factors for periprosthetic femoral fractures.4, 5, 6 In addition to these, the present study also showed that periprosthetic femoral fractures are likely to occur within 1 year of prior THR or FHR. Thus, strict fall prevention is important for the prevention of periprosthetic femoral fractures, in addition to osteoporosis treatment, especially for cases within 1 year of prior surgery.
With regard to treatment methods for periprosthetic femoral fractures, revision surgery was mainly selected for types B2 and B3, because these cases had loosened stems, and osteosynthesis was mainly selected for types A, B1, and C, because these cases did not have loosened stems. However, for types B1 and C, there were relatively many cases where revision surgery was selected even though the stems were not loose. In the case of cemented stems where removal of the stem was relatively easy, and in cases where it was not possible to obtain sufficient fixation even if osteosynthesis were performed and walking could not be permitted over a long time, the stems without loosening were removed and replaced.
In this study, type A included only 3 of 51 cases, and all 3 cases were fractures of the greater trochanter. Of the type A fractures, osteosynthesis with wiring was selected in 1 case, and conservative treatment was selected in the remaining 2 cases. One case that underwent osteosynthesis was the Pseudo type A that Huang et al.7 described, and the 2 cases that underwent conservative treatment were the Pure type A described by Huang et al. For Pure type A, in which there is a fracture line purely in the greater trochanter, conservative treatment is selected because there is little loss of function even if the bone fragment displaces because only the tip fracture. When there is a fracture line that contacts the stem, even if the fracture exists in the trochanteric area, it is Pseudo type A, and osteosynthesis is chosen because it causes abduction muscle power loss if the bone fragment displaces.
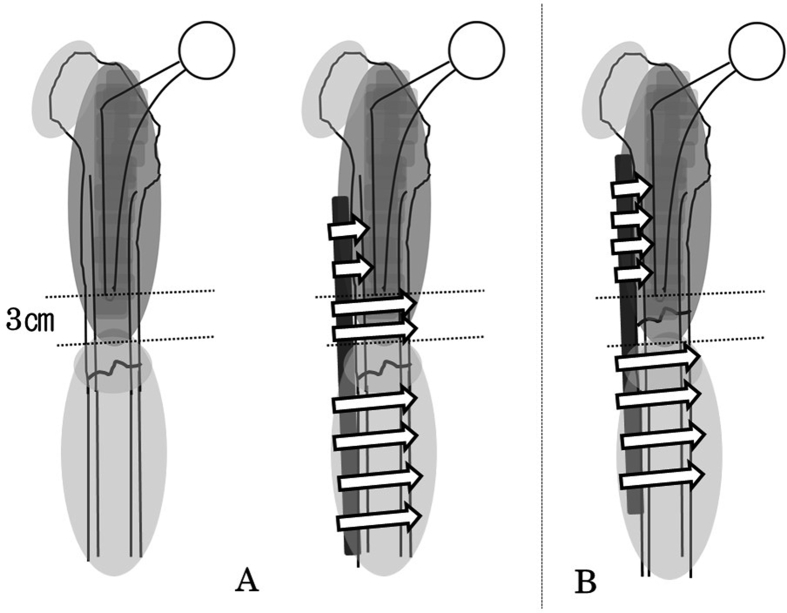
In type C fracture, the stem does not loosen due to the fracture because the fracture is distal to the implant. Therefore, osteosynthesis is usually selected for type C. However, it is reported that stress concentration occurs between the stem and the implants for osteosynthesis, and the fracture occurs further, unless the implant for osteosynthesis and the stem are separated by 6 cm or more or overlap by 6 cm or more.8 In addition, it is reported that 6–8 cortical fixations are required on both sides of the fracture line as a necessary condition to achieve successful osteosynthesis.9 In other words, in the case of type C fractures directly under the stem, it is necessary to sufficiently overlap the plate with the stem and then insert a sufficient amount of screws into the overlapping plate. If this was not possible, revision surgery with a long stem was selected even in cases where it was judged that the stem was not loose. However, all cases that were replaced by removing the unloosened stem were cemented stems. Thus, all type C fractures that occurred in cementless stems underwent osteosynthesis, because there is a high possibility that a new fracture will occur when removing the cementless stem that is not loose.
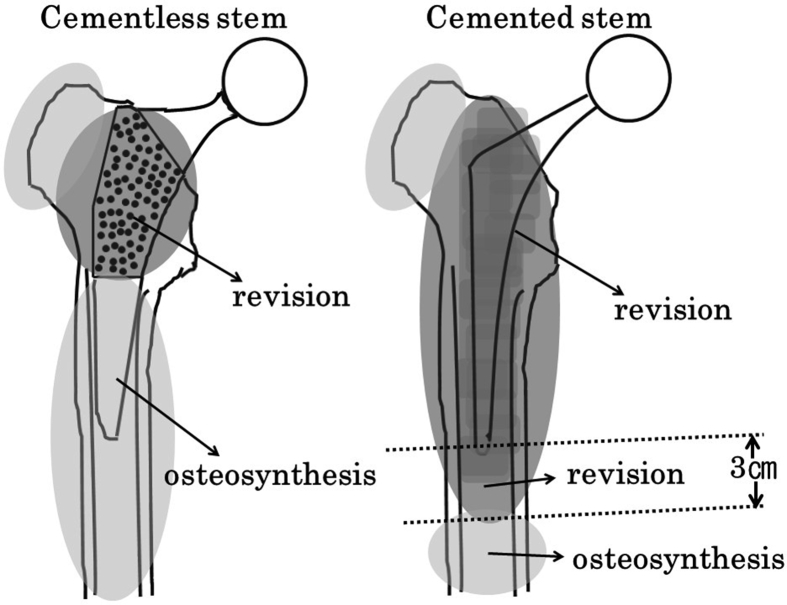
Cases without stem loosening in type B fractures (i.e. type B1 fractures) were treated in exactly the same way as type C fractures. That is, osteosynthesis is the first choice in type B1 fractures because the stem is not loosened. However, if 6–8 cortical fixations on both sides of the fracture line, a prerequisite for successful osteosynthesis, cannot be obtained, there is a high risk of failure, and long postoperative rehabilitation is required. In such type B1 cases, revision surgery using a long cementless stem with distal locking screws was selected even if the stem was not loose. For this reason, 33% of patients with type B1 (no stem loosening) underwent revision surgery. However, similar to type C cases, almost all cases that were replaced by removing the unloosened stem were cemented stem cases. Thus, almost all type B1 fractures that occurred in cementless stems underwent osteosynthesis, because there is a high possibility that a new fracture will occur when removing the cementless stem that is not loose.
Therefore, as Baba et al. showed, the treatment strategies should be considered separately for peri-cementless stem fractures and peri-cemented stem fractures.10 It is considered that the cementless stem is not loose unless there are fracture lines in the porous coating sites.10 There is a report that cementless stems will re-adhere even if they are slightly loose.11 That is, if the fracture line does not exist in the porous coating part, osteosynthesis should be selected, and if does exist in the porous coating site, revision surgery should be selected.
A cemented stem is relatively easy to remove even if it is not loose. If osteosynthesis is performed for peri-cemented stem fractures, the screws may break the cement and may loosen the stem. Therefore, revision surgery has been performed for periprosthetic fractures where the fracture line is on the cemented stem or cement around the stem.
In addition, in the case of type C fractures directly under the cemented stem, if the distance between the stem and the fracture line is about 3 cm or more, about 2 bicortical screws can be inserted proximal to the fracture line (Fig. 8). In the case of fractures less than 3 cm from the end of the stem, it is difficult to obtain fixing force equivalent to 6–8 cortical bone fixations. Therefore, removing the cemented stem and replacing it with a long stem can facilitate early rehabilitation for the patients.
Fig. 8.
Fractures more than 3 cm away from below the cemented stem (A) and less than 3 cm away from the cemented stem (B).
In fractures directly under the cemented stem, if the distance between the stem and the fracture line is about 3 cm or more, about 2 bicortical screws can be inserted proximal to the fracture line (A). In the case of fractures less than 3 cm near the end of the stem, it is difficult to obtain the fixing force equivalent to 6–8 cortical bone fixations (B).
From the above, we devised a method for classifying periprosthetic femoral fractures based on the area where the fracture line exists (Fig. 9). If this method is used, the treatment strategy can be determined based only on the position of the fracture lines with respect to the stem, without considering the looseness of the stem.
Fig. 9.
Classification and treatment based on the area where the fracture line exists.
For peri-cementless stem fractures, osteosynthesis is desirable except for fractures apparently in the porous coating. Revision surgery is selected even if there is no looseness of the stem, when the fracture line exist within 3 cm from the cemented stem.
5. Conclusions
This study investigated periprosthetic femoral fractures after THR or FHR. It became clear that there were many periprosthetic femoral fractures within 1 year after the previous surgery. Therefore, preventive measures for periprosthetic femoral fractures should be started immediately after THR or FHR.
The present study also investigated the treatment strategy for periprosthetic femoral fractures. It was found that the cementless stem is difficult to remove, and even if it is slightly loosened, there is a possibility of it re-adhering. Therefore, osteosynthesis was performed except for cases with fracture lines that were apparently in the porous coating part in peri-cementless stem fractures. On the other hand, cemented stems are relatively easy to remove, and the presence of cement is disadvantageous for bone healing and osteosynthesis. Therefore, in cases where it was judged that sufficient osteosynthesis could not be performed, revision surgery was performed even if the stem was not loosened. Thus, the treatment strategy for periprosthetic femoral fractures may be determined by the fixation mode of the stem and the position of the fracture lines.
Credit author statement
Yoshihiko Okudera: Investigation, Data Curation, Writing - Original Draft.
Hiroaki Kijima: Conceptualization, Methodology, Writing - Review & Editing.
Shin Yamada: Resources, Data Curation, Supervision.
Natsuo Konishi: Resources, Data Curation, Supervision.
Hitoshi Kubota: Conceptualization, Supervision.
Hiroshi Tazawa: Resources, Data Curation.
Takayuki Tani: Investigation, Resources.
Norio Suzuki: Investigation, Resources.
Keiji Kamo: Resources, Data Curation.
Masashi Fujii: Resources, Data Curation.
Ken Sasaki: Visualization, Investigation.
Tetsuya Kawano: Visualization, Investigation.
Yosuke Iwamoto: Software, Validation.
Itsuki Nagahata: Software, Validation.
Takanori Miura: Methodology, Formal analysis.
Naohisa Miyakoshi: Supervision, Project administration.
Yoichi Shimada: Supervision, Project administration.
Data availability
All data generated or analyzed during this study are included in this published article.
Funding statement
This research was not supported by any external funding.
Declaration of competing interest
None of the authors has any conflicts of interest to declare in relation to this manuscript.
References
- 1.Lindahl H., Oden A., Garellick G. The excess mortality due to periprosthetic femur fracture. A study from the Swedish national hip arthroplasty register. Bone. 2007;40(5):1294–1298. doi: 10.1016/j.bone.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 2.Duncan C.P., Masri B.A. Fractures of the femur after hip replacement. Instr Course Lect. 1995;44:293–304. [PubMed] [Google Scholar]
- 3.Zhang Z., Zhuo Q., Chai W. Clinical characteristics and risk factors of periprosthetic femoral fractures associated with hip arthroplasty: a retrospective study. Medicine (Baltim) 2016;95(35) doi: 10.1097/MD.0000000000004751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Watts C.D., Abdel M.P., Lewallen D.G. Increased risk of periprosthetic femur fractures associated with a unique cementless stem design. Clin Orthop Relat Res. 2015;473(6):2045–2053. doi: 10.1007/s11999-014-4077-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hagel A., Siekmann H., Delank K.S. Periprosthetic femoral fracture - an interdisciplinary challenge. Dtsch Arztebl Int. 2014 Sep 26;111(39):658–664. doi: 10.3238/arztebl.2014.0658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meek R.M., Norwood T., Smith R. The risk of peri-prosthetic fracture after primary and revision total hip and knee replacement. J Bone Joint Surg Br. 2011;93(1):96–101. doi: 10.1302/0301-620X.93B1.25087. [DOI] [PubMed] [Google Scholar]
- 7.Huang J.F., Jiang X.J., Shen J.J. Modification of the Unified Classification System for periprosthetic femoral fractures after hip arthroplasty. J Orthop Sci. 2018;23(6):982–986. doi: 10.1016/j.jos.2018.07.014. [DOI] [PubMed] [Google Scholar]
- 8.Walcher M.G., Giesinger K., du Sart R. Plate positioning in periprosthetic or interprosthetic femur fractures with stable implants-a biomechanical study. J Arthroplasty. 2016;31(12):2894–2899. doi: 10.1016/j.arth.2016.05.060. [DOI] [PubMed] [Google Scholar]
- 9.Karabila M.A., Bardouni A. Periprosthetic hip fracture type C Vancouver, what not to do. Pan Afr Med J. 2016;17 doi: 10.11604/pamj.2016.23.5.8611. 23:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baba T., Homma Y., Momomura R. New classification focusing on implant designs useful for setting therapeutic strategy for periprosthetic femoral fractures. Int Orthop. 2015;39(1):1–5. doi: 10.1007/s00264-014-2476-x. [DOI] [PubMed] [Google Scholar]
- 11.Joestl J., Hofbauer M., Lang N. Locking compression plate versus revision-prosthesis for Vancouver type B2 periprosthetic femoral fractures after total hip arthroplasty. Injury. 2016;47(4):939–943. doi: 10.1016/j.injury.2016.01.036. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.