Summary
Background
India, one of the economic powerhouses of the world, is lacking in health development.Moreover, it is facing ‘Triple burden of disease’. Indians have one of highest proportion of out-of-pocket (OOP) health expenses. Salient reasons are poor quality public health care, costly private care and lack of health insurance. This has led to catastrophic health expenditure (CHE). Another contributor to this CHE is the chronic illness, which require long-term follow-up. It is estimated that catastrophic health expenditure impoverishes 3.3% of Indians every year. This study was undertaken with an aim to estimate the prevalence of catastrophic health expenditure and its associated factors.
Methods
A longitudinal study with one-year follow-up period was conducted among 350 households of an urban area in Bangalore city. Simple random sampling method was used to select the study sample. Data collection done using pre-tested, semi-structured questionnaire by interview method.
Results
Chronic illness mean health expenditure was 1155.67 INR (56.09% of the direct cost was spent on drugs). In acute illness, mean health expenditure was 567.45 INR (59.54% of the direct cost was spent on drugs). Fourty eight (14.86%) of the households experienced CHE in the one year Statistically significant association was found between socio-economic status and catastrophic health expenditure. Eighty-five 42% of the households who experienced CHE had a member with chronic illness in it.
Conclusion
Reducing the financial burden of high health care expenses is possible by improving the government health care system, free quality regular supply of medications to chronic disease patients and to improve the beneficiaries under insurance schemes.
Keywords: Government health care, Financial burden, Direct costs
Introduction
India, a country with impressive economic development, has failed to show similar results in field of health. Our country now suffers with ‘Triple burden of disease’. With growing communicable diseases, along with nutrition related health problems and rampantly increasing non-communicable diseases has added to the triple burden. In such a situation, equity in health-care distribution; a longstanding principle to serve all the under-privileged members of the society becomes important [1]. This is possible only with adequate public health expenditure. In developed countries, government health spending accounts to around 5 per cent of GDP or more. Even in Asian developing countries other than India, the average is around 3 per cent of GDP. But India, an economic powerhouse has government health expenditure amounting to less than 1 per cent of GDP [2]. Due to inadequate public spending for health development and also the high health care costs in private sector, the economic burden of health spending entirely lies on private spending which in India is majorly by out-of pocket expenses [3]. India has one of the highest proportions of household out-of-pocket health expenditures in the world, estimated at 71.1% in 2008-09 [1]. Household’s share in health spending is almost more than two-thirds in India which is around three times the amount of all government expenditure [4].
India has an estimation of more than 290 million people living below the poverty line [5]. Diseases can still further deteriorate an individual condition by affecting the quality of life, loss of savings and assets, indebtedness and an inability to cope with future illness [6]. Such a financial burden can be blamed on low-funded and low-quality health care of public health system which forces consumers to seek care from expensive private sector. Another contributor which causes the financial burden is the lack of protective mechanisms like health insurance [7]. Less than 10% of India’s population is covered by the protective mechanisms against health care expenses.1 The unpredictable character of illness requiring huge amounts of money are impoverishing an estimated 3.3% of India’s population every year [8].
World Health Organization proposes that health expenditure should be called catastrophic whenever it is greater than or equal to 40% of the capacity to pay [9]. Some studies, have defined Catastrophic Health Expenditure if the total health expenditure is more than 10% of annual income [10]. The precursors for catastrophic payments are the availability of expensive health services, low capability to pay, and the lack of health insurance [7]. Another contributor to catastrophic payments is Chronic diseases. It is a known fact that catastrophic payments are more in chronic illness. As people with chronic diseases require long-term follow-up, long-lasting medications and also have an increased risk of in-patient or Intensive care unit admissions, thus leading to more health expenses [11]. As there are fewer studies about catastrophic payments at household level, this study was conducted with an objective to assess the out-of pocket health expenses among the households, prevalence of CHE among the households and to determine the associated factors of CHE.
Materials and methods
STUDY DESIGN, AREA AND STUDY POPULATION
This was a longitudinal study with one-year follow-up conducted among the households of an urban area in Bangalore, Karnataka. The study was conducted from January 2016 to April 2017.
STUDY SAMPLE SIZE
Based on a previous study by Mani et al. [8], the preference of the households for health care at a government facility was found to be 65% and at 5% significance, sample size was calculated to be 350 households.
HOUSEHOLD SELECTION METHOD
There are 3 sectors in the urban field practice area with total 6237 households (1684 + 2182 + 2371). Sample size was achieved ensuring equal representation to all sectors in study area by Probability Proportional to Size sampling. Sample size 350 was proportionately divided obtaining 95,122 and 133 households in each sector. By simple random technique, households were chosen in each sector from the survey list available in the health center, irrespective of family composition and by using lottery method.
INCLUSION CRITERIA
Those who are the permanent residents in the area since 3 years.
Households who gave consent for a follow-up study.
EXCLUSION CRITERIA
Guests contributing to health expenditure at the time of study.
ETHICAL CONSIDERATION, STUDY TOOL AND DATA COLLECTION METHOD
Data collection was started after obtaining ethical clearance from the Institutional Ethical committee. A written informed consent was obtained from the households for study. Data was collected using a pre-tested and semi-structured questionnaire by interview method. Study tool was standardized by a Pilot study and those households who participated in pilot study were not included for analysis. The households who satisfied the eligibility criteria were recruited for the study. Data regarding socio-demographic profile, chronic illness in the family, health expenses incurred preferred health care system were obtained during recruitment of households into the study. Among the recruited households, the ones with chronic illness patients were noted down. Then those subjects and other households were followed up for a period of one year to assess the annual health expenditure and catastrophic health expenditure.
FOLLOW-UP DATA COLLECTION METHOD
A well informed contact person was identified in each household for follow-up. A log book was distributed to them which contained the components of health expenditure like type of visit to health center, illness, health center visited (private/ government), total health expenditure and also the split expenditure of direct and indirect cost. Direct cost contains consultation fees, drug expenses and investigation expenses. Whereas indirect costs contain transport expenses, food expenses and consecutive income loss. Each month the households were contacted and the data from the log book were retrieved.
STATISTICAL ANALYSIS
Data was entered in Microsoft Excel sheet and analyzed using SPSS software version 22. Descriptive statistics, Chi-Square test and logistic regression were used for analysis and results were presented in the form of tables and figures. The model for logistic regression used for this study was  .
.
The total health expenditure is divided into direct and indirect cost. Direct cost contains consultation fees, drug expenses and investigation expenses. Whereas indirect costs contain transport expenses, food expenses and consecutive income loss. Catastrophic health expenditure was calculated by considering total health expenditure spent by households annually for all type of services (curative, preventive, chronic illness) and the annual income of the household. The health expenditure was said to be catastrophic when the total health expenditure is more than 10% of the annual income [10].
Results
SOCIO-DEMOGRAPHIC PROFILE OF THE POPULATION
Study was conducted among 350 households of an urban area which included 1581 individuals. 991 (62.68%) adults, 162 (10.25%) under-5 children and 66 (4.17%) elderly population. It was seen that female population was slightly higher in our study (811, 51.3%) than the males (770, 48.7%). Most of the households belonged to upper lower class (54.29%) followed by lower middle (35.71%) class according to Modified Kuppuswamy scale 2016. Majority of households i.e. 263 (75.10%) were below poverty line.
SOCIO-DEMOGRAPHIC PROFILE OF SUBJECTS WITH CHRONIC ILLNESS
Among the 350 households the total number of individuals with chronic illness was 109 (6.90%): 72 (66.05%) were in the age-group of 30-60 years, and 37 (34%) above 60 years. Among them 64 (59%) were females. 84 (77.06%) were literates with majority of them completed primary education. Table I shows the various types of chronic illness among the households.
Tab. I.
Types of Chronic illness among individuals (n = 109).
| Chronic illness | Frequency | Percentage |
|---|---|---|
| Diabetes Mellitus | 32 | 29.36% |
| Hypertension | 25 | 22.94% |
| DM+HTN | 21 | 19.27% |
| Hypothyroidism | 7 | 6.42% |
| Respiratory illness | 7 | 6.42% |
| Cardiovascular diseases | 8 | 7.33% |
| Kidney disorder | 3 | 2.75% |
| Epilepsy | 2 | 1.83% |
| Others (mental disorders, bone disorders) | 4 | 3.66% |
HEALTH CARE SECTOR PREFERENCE IN INDIVIDUALS WITH AND WITHOUT CHRONIC ILLNESS
Table II depicts that the individuals with chronic illness prefer private clinics (68, 62.39%) over Government sector (30, 27.52%). Even in individuals with acute illness episodes (1204 episodes) majority of them were found to prefer private clinics over government sector (988, 82.06%). Over the counter medication history was higher among individuals with acute illness (86, 7.14%) compared to (3, 2.75%) those with chronic illness (109).
Tab. II.
Type of health sector visited for illness (both acute and chronic).
| Health sector | Acute illness (n = 1204) Frequency (%) |
Chronic illness (n = 109) Frequency (%) |
|---|---|---|
| Private clinic | 988 (82.06%) | 68 (62.39%) |
| Government | 98 (8.14%) | 30 (27.52%) |
| Nursing home | 30 (2.49%) | 5 (4.59%) |
| Over the counter medicine | 86 (7.14%) | 3 (2.75%) |
| Alternative system | 2 (0.10%) | 3 (2.75%) |
OUT-OF-POCKET HEALTH EXPENDITURE AMONG THE HOUSEHOLDS WITH AND WITHOUT CHRONIC ILLNESS IN FAMILY
In chronic illness mean health expenditure was 1155.67 INR. 56.09% of the direct cost was found to be spent on drugs and 26.16 % on investigations. Whereas lower proportion was for consultation fees. When interviewed about the health expenses spent for out-patient visits for acute illness, it was found that mean Total Health Expenditure was 567.45 INR during each visit. 59.54% of the direct cost was found to be spent on drugs and 23.70% on consultation fees. Whereas lower proportion was for investigation (16.69%). In indirect expenses major contributor was food expenses and income loss.
CATASTROPHIC HEALTH EXPENDITURE (CHE) AMONG HOUSEHOLDS
In our study 48 (14.86%) of the households experienced CHE in the one year. (Fig. 1) A large portion of health expenses was found to be out of pocket expenses i.e out of earning and savings. To cope up with the high health care expenses ten households were in debt.
Fig. 1.
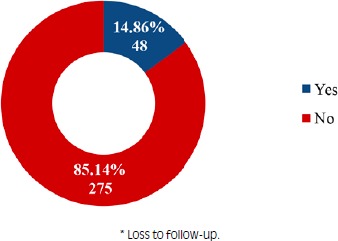
Proportion of households experienced CHE during follow-up of 1 year (n = 323)*.
Table III shows the association between various parameters of the households and catastrophic health expenditure. The association was found to be statistically significant (Chi-square value = 9.06 and P < 0.05) with socio-economic status. It depicts that as the socio-economic status lowers there is increase in Catastrophic Health Expenditure among the households. It emphasizes that the Lower middle and upper lower household population suffer CHE and are pushed more below poverty.
Tab. III.
Associated factors with catastrophic health expenditure (n = 323).
| Factors | CHE Yes |
CHE No |
Chi-square value | P value |
|---|---|---|---|---|
| Frequency | Frequency | |||
| Religion Hindu Muslim |
40 8 |
233 42 |
0.06 |
0.8 |
| Type of family Nuclear Joint 3-generation |
34 5 9 |
193 18 64 |
1.232 |
0.54 |
| Socio-economic status Upper middle Lower middle Upper lower |
5 8 35 |
28 106 141 |
9.06 | < 0.05 |
| Chronic illness Yes No |
41 7 |
58 217 |
79.55 |
< 0.001 |
|
*BPL card holders Yes No |
38 10 |
205 70 |
0.468 |
0.494 |
* below poverty line
The total number of households with one or the other member having chronic illness was 99. Table III shows that the association between households with chronic illness and CHE was statistically significant (X2 = 79.55, p value = < 0.001). It was seen that 41 out of 99 households with chronic illness experienced CHE (41.41%).
But we already have seen that total number of households who experienced CHE overall were only 48. Out of which 41 households have one or more member with chronic illness in it; i.e 85.42% of the households who experienced CHE had a member with chronic illness (Fig. 2). It was seen that the most common chronic illness among the households experiencing CHE was Diabetes Mellitus and Hypertension (70%).
Fig. 2.
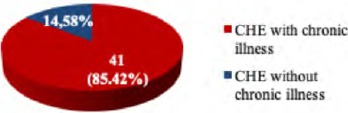
Comparison of CHE among households with and without chronic illness (n = 48).
Table IV depicts that the odds of CHE among joint family was 2.695 times more when compared to three-generation family (constant). Similarly, the odds of CHE was 1.29 times more among nuclear family compared to the odds among three-generation family. The odds of CHE was 1.5 times more among the households with chronic illness compared to the ones without chronic illness. Total number of family members and also socio-economic status of the household had odds ratio of 0.99 (approximately 1)
Tab. IV.
Logistic regression model for risk factors of catastrophic health expenditure
| SL No | Risk factors | Odds ratio | 95% CI for Odds ratio | |
|---|---|---|---|---|
| Lower | Upper | |||
| 1 |
Religion Hindu Muslim |
0.046 0.052 |
0.008 0.008 |
0.269 0.354 |
| 2 |
Type of family Nuclear Joint |
1.293 2.695 |
0.498 0.686 |
3.358 10.582 |
| 3 | Total family members | 0.996 | 0.682 | 1.179 |
| 4 |
Socio-economic status Lower middle Upper lower |
0.46 0.904 |
0.085. 0.396 |
2.49 2.063 |
| 5 | Chronic illness | 1.505 | 1.016 | 3.163 |
Discussion
Among the 350 households the total number of individuals with chronic illness was 109 (6.90%).
In a study by Bhojani et al. the prevalence of self-reported chronic conditions was 8.6% in the general population and 13.8% among adults (age ≥ 20 years). In this study majority of the visits were to private clinics, which is similar to a study conducted by Bhojani et al. where it found that overall, 80.6% of people with chronic conditions sought care from private healthcare providers, while 19.4% sought care from government health services [11]. But findings are in contradiction with another study by Kanungo et al. where 53.16% episodes were treated by non-qualified practitioners, 34.02% by qualified practitioner from private sector and only 12.82% by qualified practitioner from Government sector [12].
Diabetes Mellitus and hypertension were the most commonly reported conditions similar to study by Bhojani et al. where hypertension and diabetes had a self-reported prevalence of 10.0% and 6.4%, respectively [11].
When we look into the health expenses, similar results were also found by Bhojani e al. They found similar OOP payments for chronic illness treatment [11]. Another study which shows similar results is a study by Quintussi et al. where it was seen that the households’ average monthly costs related to non-communicable diseases (1573 INR) and bulk of expenditures on care for chronic diseases (74%) were related to additional medical services, mostly drugs [13].
In our study, the prevalence of catastrophic health expenditure was 14.86% (48 households) and major source of health expenses was from earnings and savings. Similarly, a study by Rehman et al. showed that a large majority (86%) of the study participants had to bear the expense out of pocket, either by borrowing money (42%); or by selling their household belongings (23%) [14]. Study by Balasubramanian et al. showed that the prevalence of catastrophic expenditure was 5.6% and almost 59% of the patients paid for the healthcare from their income or savings [15].
A statistically significant association was found between socio-economic status and catastrophic health expenditure in our study. Similar to the study by Bhojani et al. where the median share of household income spent on OOP payments was significantly higher among the lowest income quintile compared with the highest income quintile [11]. Our study also found that out of 48 households who experienced catastrophic health expenditure during one year, 41 (85.42%) were households with one or the other chronic illness.
LIMITATIONS OF THE STUDY
Catastrophic health expenditure can be better calculated by considering household‘s capacity to pay and proportion of health expenditure out of total expenditure which could not be computed in this study. Moreover, an element of recall bias could not be eliminated since it is a follow-up study.
Conclusions
We had conducted this study with an objective to study the health expenditure incurred by the households and to estimate the prevalence of catastrophic health expenditure. Nearly 7% of the population had chronic illness. Direct cost was more for the treatment of chronic illness when compared to acute illness episodes and majority of those expenses was for medications and investigations. Catastrophic health expenditure prevalence was found to be 14.85% which was significantly associated with lower socio-economic status and chronic illness. Only ways to reduce the financial burden of high health care expenses is to improve the government health care system by providing quality health care services, free quality regular supply of medications to chronic disease patients and also to improve the beneficiaries under insurance schemes.
Ethical approval
The study was approved by the Institutional Ethics Committee, Bangalore Medical College & Research Institute.
Figures and tables
Acknowledgements
Authors would like to thank the following for their invaluable support and guidance. Health staff at the urban health center, all the faculty and postgraduates of department of Community Medicine, BMCRI, Bangalore.
Funding sources: this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Conflict of interest statement
The authors declare no conflict of interest.
Authors’ contributions
NBS and SS planned, designed and conducted the study. NBS and SS did the data entry and analysis along with review of literature which was guided by SS.
References
- [1].Balarajan Y, Selvaraj S, Subramaniam SV. Health care and equity in India. Lancet 2011;377:505-15. https://doi.org/10.1016/S0140-6736(10)61894-6 10.1016/S0140-6736(10)61894-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Economic Research Foundation. Government Health Expenditure in India: a benchmark study. Undertaken for the MacArthur Foundation, India, New Delhi. 2006. August Available at: http://www.macroscan.org/anl/oct06/pdf/Health_Expenditure.pdf [Accessed on 11 Jan 2019].
- [3].Skordis-Worrall J, Pace N, Bapat U, Das S, More N S, Joshi W. Maternal and neonatal health expenditure in Mumbai slums (India): a cross-sectional study. BMC Public Health 2011; 11:1471-2458. https://doi.org/10.1186/1471-2458-11-150 10.1186/1471-2458-11-150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].World Health Organisation. Global Health Observatory [online] 2012; Available from URL: http://www.who.int/countries/ind/en/ [Accessed on 16 Jan 2019].
- [5].Barua N. How to develop a pro-poor private health sector in urban India? Mumbai. Presented at the Global Forum for Health Research: forum 9; 12–16 September; 2005. Available at: URL:https://www.researchgate.net/publication/241553007_How_to_develop_a_pro-poor_private_health_sector_in_urban_India. [Accessed on 16 Jan 2019].
- [6].Ranson MK. Reduction of catastrophic health care expenditures by a community-based health insurance scheme in Gujarat, India: current experiences and challenges. Bull World Health Organ 2002;80:613-21. [PMC free article] [PubMed] [Google Scholar]
- [7].Gupta I, Alam M, Ellis RP. Health insurance in India prognosis and prospects. Economic and Political weekly 2000;35(4) Available at: http://planetwealth.in/palash/pdf/301015013216health-insurance.pdf. [Accessed on 16 Jan 2019]. [Google Scholar]
- [8].Ministry of Health and Family Welfare, Government of India. Report of the National Commission on Macroeconomics and Health, New Delhi. 2005. August Available at: http://www.who.int/macrohealth/action/Report%20of%20the%20National%20Commission.pdf [Accessed on 18 Jan 2019].
- [9].Kawabata K, Xu K, Carrin G. Preventing impoverishment through protection against catastrophic health expenditure. Bull World Health Organ [serial online] 2002;8:612 Available at: https://apps.who.int/iris/handle/10665/71556 [Accessed on 18 Jan 2019]. [PMC free article] [PubMed] [Google Scholar]
- [10].Devadasan N, Criel B, Damme W, Ranson K, Van der Stuyft P. Indian community health insurance schemes provide partial protection against catastrophic health expenditure. BMC Health Services Research 2007;7:43 https://doi.org/10.1186/1472-6963-7-43 10.1186/1472-6963-7-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Bhojani U, Thriveni B., Devadasan R, Munegowda C, Devadasan N, Kolsteren P, Criel B. Out-of-pocket healthcare payments on chronic conditions impoverish urban poor in Bangalore, India. BMC Public Health 2012;12:990 https://doi.org/10.1186/1471-2458-12-990 10.1186/1471-2458-12-990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Kanungo S, Bhowmik K, Mahapatra T, Mahapatra S, Bhadra UK, Sarkar K. Perceived morbidity, healthcare-seeking behavior and their determinants in a poor-resource setting: observation from India. PLoS ONE 2015;10:e0125865 https://doi.org/10.1371/journal.pone.0125865 10.1371/journal.pone.0125865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Quintussi M, Poel EV, Panda P, Rutten F. Economic consequences of ill-health for households in northern rural India. BMC Health Services Research 2015;15:179 https://doi.org/10.1186/s12913-015-0833-0 10.1186/s12913-015-0833-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Rehman A, Shaikh BT, Ronis KA. Health care seeking patterns and out of pocket payments for children under five years of age living in Katchi Abadis (slums), in Islamabad, Pakistan. Int J Equity Health 2014;13:30 https://doi.org/10.1186/1475-9276-13-30 10.1186/1475-9276-13-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Balasubramanian D, Prinja S, Aggarwal AK. Effect of user charges on secondary level surgical care utilization and out-of-pocket expenditures in Haryana State, India. PLoS ONE. 2015;10(5):e0125202 https://doi.org/10.1371/journal.pone.0125202 10.1371/journal.pone.0125202 [DOI] [PMC free article] [PubMed] [Google Scholar]


