Abstract
Study objective
We aim to describe the variability and identify gaps in preparedness and response to the coronavirus disease 2019 pandemic in European emergency departments (EDs) caring for children.
Methods
A cross-sectional point-prevalence survey was developed and disseminated through the pediatric emergency medicine research networks for Europe (Research in European Pediatric Emergency Medicine) and the United Kingdom and Ireland (Paediatric Emergency Research in the United Kingdom and Ireland). We aimed to include 10 EDs for countries with greater than 20 million inhabitants and 5 EDs for less populated countries, unless the number of eligible EDs was less than 5. ED directors or their delegates completed the survey between March 20 and 21 to report practice at that time. We used descriptive statistics to analyze data.
Results
Overall, 102 centers from 18 countries (86% response rate) completed the survey: 34% did not have an ED contingency plan for pandemics and 36% had never had simulations for such events. Wide variation on personal protective equipment (PPE) items was shown for recommended PPE use at pretriage and for patient assessment, with 62% of centers experiencing shortage in one or more PPE items, most frequently FFP2 and N95 masks. Only 17% of EDs had negative-pressure isolation rooms. Coronavirus disease 2019–positive ED staff was reported in 25% of centers.
Conclusion
We found variation and identified gaps in preparedness and response to the coronavirus disease 2019 epidemic across European referral EDs for children. A lack in early availability of a documented contingency plan, provision of simulation training, appropriate use of PPE, and appropriate isolation facilities emerged as gaps that should be optimized to improve preparedness and inform responses to future pandemics.
Introduction
Background
Ever since the first human cases of the novel coronavirus were reported in Wuhan, Hubei Province, China, in December 2019, the coronavirus disease 2019 (COVID-19) pandemic has spread rapidly across the world.1 The epidemic in Europe initially centered around Northern Italy, where there was a steep increase in the number of cases and case fatalities from February 20, 2020, onward.2 While European countries were deciding on or were enacting containment measures of various degrees, the infection continued to spread across the continent, with devastating effect on health systems, the economy, and the society at large.
Editor’s Capsule Summary.
What is already known on this topic
Emergency departments’ (EDs’) preparedness for pandemics has an influence on care of patients and safety of health care workers.
What question this study addressed
How prepared were European referral pediatric EDs at the beginning of the COVID19 pandemic?
What this study adds to our knowledge
This cross-sectional survey demonstrated high variability regarding contingency plans, simulation training, appropriate use of PPE, and appropriate isolation facilities among 102 pediatric EDs.
How this is relevant to clinical practice
The pandemic has demonstrated the importance of planning and preparedness for such events.
Within health care, it is crucial that the emergency department (ED), as the entry point to hospital care, be prepared to manage high-risk COVID-19 patients in an efficient and safe way, from triage to final disposition. The ED should respond to the epidemic surge in agreement with hospital contingency plans and guidelines from local and national health authorities,3 also learning from the experience of other countries.4
Even though it has now become apparent that children are affected less frequently and with a much more benign disease spectrum than that of adults,5 , 6 appropriate management in the ED of patients with suspected and confirmed cases and of their families is essential.7 , 8 Children may present with conditions not linked to COVID-19, but some, when admitted for that condition, are found to have COVID-19–positive swab results as an incidental finding. This may be a feature related to the more widespread dissemination of COVID-19 throughout the population. In addition to the quality of care provided to patients with suspected or confirmed COVID-19, EDs should also maintain it for children presenting with serious illnesses or accidents not related to the pandemic.
Importance
Pathways and protocols need to be in place to ensure that rapid appropriate care is provided to children with suspected COVID-19 while avoiding delay in care of non–COVID-19 patients.9 In addition, it is paramount to ensure adequate protection and minimize exposure of patients and staff to the infection.10 However, the dialogue between European pediatric emergency physicians who liaised through their European society and their research networks (Research in European Pediatric Emergency Medicine [REPEM] and Paediatric Emergency Research in the United Kingdom and Ireland [PERUKI]) 11, 12, 13 highlighted differences and challenges in ED preparedness and response between countries as the COVID-19 pandemic unfolded throughout Europe.
Goals of This Investigation
Hence, we aimed to describe the preparedness and response to the COVID-19 pandemic in European referral EDs for children within the REPEM and PERUKI networks.
We hypothesized that European referral EDs for children would show variability and gaps in preparedness and response to the COVID-19 pandemic, from which lessons could be learned for the current and future pandemics.
Materials and Methods
Study Design and Setting
We conducted a cross-sectional point-prevalence survey. It was developed in English by the lead author (S.B.) and then underwent several rounds of review by the research team. The survey was distributed through the REPEM network,12 a research collaborative consisting of pediatric EDs and EDs of general hospitals with a separate pediatric section, serving as referral centers for children, and also the sites affiliated with the executive committee members of PERUKI. For each country, a country lead was identified on a volunteer basis, through the network, to disseminate the survey to centers meeting the criteria mentioned earlier. Country leads were pediatric emergency physicians or pediatricians working in the ED. We also included Israel as a European-associated country because it has been part of the REPEM network since the organization’s foundation.14
To ensure balanced representativeness of participating countries and feasibility of the study, the research team, using a quota sampling method,15 agreed to include a predetermined number of centers based on the population of participating countries. For countries with more than 20 million inhabitants (namely, Italy, France, Germany, Spain, and the United Kingdom), participation of 10 EDs was sought. For countries with less than 20 million inhabitants, 5 EDs were expected to participate, unless the number of eligible EDs was less than 5 (ie, Estonia: 4 EDs eligible; Iceland: 1 ED eligible; Latvia: 1 ED eligible; and Malta 2 EDs eligible). The denominator for our survey comprised 103 centers.
Country leads were to decide on the strategy to approach eligible EDs in their country. Some country leads approached more than the preestablished number of centers to ensure a 100% response rate, accounting for the possibility that some contacted centers might not respond. By adopting this approach, some countries actually exceeded the expected number of participating centers per country. For calculation of the survey response rate, the number of EDs exceeding the predetermined expected number of participating EDs per country was not considered.
ED directors or their delegates, staff members appointed by the ED director as most suitable to complete the survey, completed one survey for each participating center. The survey was open on March 20 and 21, 2020. Survey responses were collected in Research Electronic Data Capture (version 9.10.0; Vanderbilt University, Nashville, TN) a validated online data collection system.16 Respondents were asked to state their country of residency, but it was not mandatory to give the name of their hospital. Each country lead recorded the name of the invited and participating hospitals. Country leads communicated to the principal investigator the number of centers that completed the survey, without disclosing the hospitals’ identities, ensuring that the number of completed surveys per country matched the number of centers that actually completed the online survey.
Preparedness and response were defined according to consensus of the research team as organizational and operational actions taken by EDs to face the pandemic, including contingency plans, training, screening of patients with suspected cases, surge capacity, availability and use of personal protective equipment (PPE), ED infection control measures, care pathways and management of suspected cases, health professionals’ safety, and sustainability of care.
A first survey was completed by country leads to reflect the national situation of the COVID-19 pandemic as of March 20, 2020. The country lead survey included questions on range of COVID-19 cases (total and pediatric) per country, the date of identification of the first COVID-19 cases in the country, and the type of containment measures enforced in their country. Data on range of confirmed cases per country, as well as deaths, were cross-checked with the European Center for Disease Control and Worldometer Web sites on March 21 to ensure complete update of data up to March 20, 2020.17 , 18 There were no reported pediatric COVID-19 confirmed deaths in participating countries at the survey.
The ED survey completed by each participating center focused on organizational and operational aspects of preparedness and response, as reported in the above-mentioned definition.
We followed Strengthening the Reporting of Observational Studies in Epidemiology guidelines for reporting of observational studies.19
Primary Data Analysis
Descriptive statistics were used to analyze the data, with 95% confidence intervals around each point estimate. Data were analyzed with Stata (version 13; StataCorp, College Station, TX).
This survey accessed clinicians through a research collaborative to assess their departmental practice and therefore did not require formal ethics review, as determined by the ethics board of the University Hospital of Padova, Italy. Consent was implied by participation.
Results
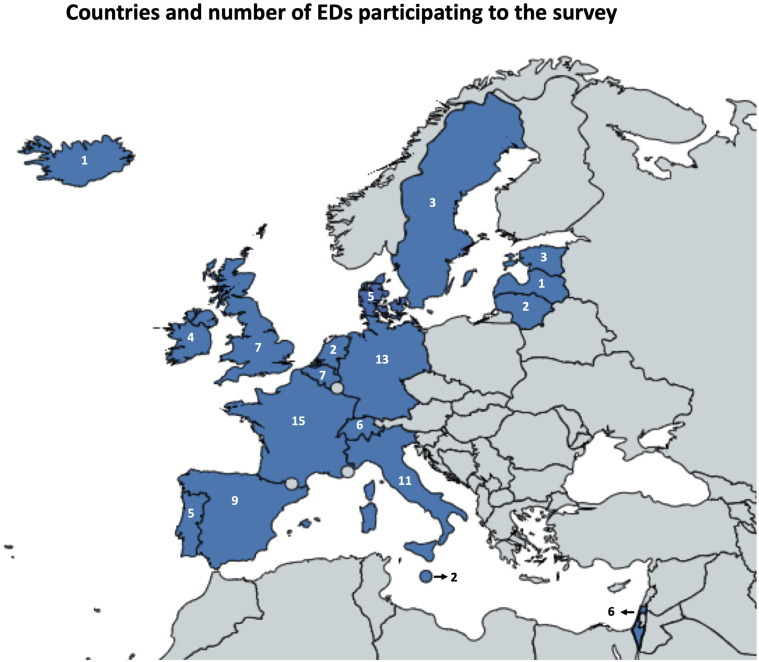
A total of 18 countries participated in the study. Eighty-nine of the expected 103 centers, in accordance with the preestablished number of participating centers per country, completed the survey (response rate 86%). However, some countries exceeded the number of expected participating EDs, leading to a total of 102 EDs participating to the survey (Table 1 and Figure 1 ). The survey was completed by the ED director in 48% of cases and by his or her delegate in 52%. The number and characteristics of participating centers and the range of COVID-19 confirmed cases per country are reported in Table 1. The majority of participating EDs were tertiary care pediatric ones (75%) and most centers had a pediatric yearly census greater than 10,000 visits per year (89%). Only a few pediatric patients with confirmed COVID-19, if any, were treated in participating EDs. Containment measures were variably enforced in participating countries as of March 20, 2020 (Table E1, available online at http://www.annemergmed.com). Measures less often taken were the most restrictive; namely, closure of nonessential commercial activities (67%), closure of borders (50%), and the prohibition of any travel not related to health or food shopping needs (50%). A summary of criteria for suspected COVID-19 cases in use at participating EDs is provided in Table E2 (available online at http://www.annemergmed.com). Definition criteria had changed over time in 90% of centers, reflecting the dynamic adjustments made to face a rapidly evolving crisis. At the survey, any child with flulike illness or fever was considered to have a suspected COVID-19 infection in 67% of centers.
Table 1.
Characteristics of participating countries and centers.
| Belgium | Denmark | Estonia | France | Germany | Iceland | Ireland | Israel | Italy | Latvia | Lithuania | Malta | Netherlands | Portugal | Spain | Sweden | Switzerland | UK | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predetermined No. of expected centers | 5 | 5 | 4∗ | 10 | 10 | 1∗ | 5 | 5 | 10 | 1∗ | 5 | 2∗ | 5 | 5 | 10 | 5 | 5 | 10 |
| No. centers actually participating | 7 | 5 | 3 | 15 | 13 | 1 | 4 | 6 | 11 | 1 | 2 | 2 | 2 | 5 | 9 | 3 | 6 | 7 |
| ED setting | ||||||||||||||||||
| Tertiary care PED of stand-alone hospital | 0 | 0 | 1 | 6 | 4 | 1 | 2 | 1 | 5 | 1 | 0 | 0 | 0 | 2 | 3 | 1 | 3 | 1 |
| Tertiary care PED in a hospital for adults and children | 2 | 3 | 1 | 7 | 8 | 0 | 0 | 5 | 6 | 0 | 1 | 0 | 1 | 1 | 5 | 1 | 1 | 3 |
| Referral general ED with pediatric section† | 5 | 2 | 1 | 2 | 1 | 0 | 2 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 0 | 2 | 3 |
| Other‡ | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 2 | 1 | 1 | 0 | 0 |
| Pediatric age limit, y | ||||||||||||||||||
| ≤14 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 0 | 0 |
| ≤15 | 2 | 0 | 0 | 3 | 0 | 0 | 1 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 1 |
| ≤16 | 3 | 0 | 0 | 3 | 0 | 0 | 3 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 5 | 6 |
| ≤18 | 2 | 5 | 3 | 9 | 13 | 1 | 0 | 6 | 4 | 1 | 2 | 1 | 2 | 5 | 2 | 3 | 1 | 0 |
| ED pediatric yearly census (visits/y) | ||||||||||||||||||
| <10,000 | 1 | 2 | 2 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2 | 0 | 0 | 1 | 0 | 0 |
| 10,000–15,000 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 1 |
| 15,000–25,000 | 2 | 3 | 0 | 0 | 9 | 1 | 1 | 1 | 4 | 0 | 0 | 1 | 0 | 1 | 2 | 1 | 2 | 0 |
| 25,000–50,000 | 0 | 0 | 0 | 11 | 1 | 0 | 2 | 5 | 5 | 0 | 1 | 0 | 0 | 2 | 1 | 0 | 4 | 4 |
| >50,000 | 0 | 0 | 1 | 4 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 2 | 6 | 0 | 0 | 2 |
| No. of pediatric positive COVID-19 cases treated in ED (total for all centers per country) | 7§ | 16 | 0 | 34 | 13§ | 2 | 11 | 4 | 48 | 2 | 0 | 1 | 0 | 12 | 26 | 0 | 14§ | 2§ |
| Time from first COVID case, wk | 3–4 | 3–4 | 3–4 | ≥ 4 | 3–4 | 3–4 | 2–3 | 3–4 | ≥ 4 | 2–3 | 3–4 | 1–2 | 3–4 | 2–3 | ≥ 4 | ≥ 4 | 3–4 | ≥ 4 |
| No. of total COVID-19 confirmed cases | ≥1,000 <10,000 | ≥100 <1,000 |
≥100 <1,000 |
≥10,000 | ≥1,000 <10,000 | ≥100 <1,000 |
≥100 <1,000 |
≥100 <1,000 |
≥10,000 | ≥10 <100 |
≥10 <100 |
≥10 <100 |
≥1,000 <10,000 | ≥100 <1,000 |
≥10,000 | ≥1,000 <10,000 | ≥1,000 <10,000 | ≥1,000 <10,000 |
| No. of total COVID-19 confirmed deaths | ≥10 <100 |
<10 | <10 | ≥100 <1,000 |
≥10 <100 |
<10 | <10 | <10 | ≥ 1,000 | <10 | <10 | <10 | ≥100 <1,000 |
<10 | ≥1,000 | ≥10 <100 |
≥10 <100 |
≥100 <1,000 |
| No. of total pediatric COVID-19 confirmed cases | ≥10 <100 |
≥10 <100 |
≥10 <100 |
≥1,000 <10,000 | ≥100 <1,000 |
≥10 <100 |
≥10 <100 |
<10 | ≥100 <1,000 |
<10 | <10 | <10 | <10 | ≥10 <100 |
Not reported | ≥10 <100 |
≥100 <1,000 |
Not reported |
UK, United Kingdom; PED, Pediatric ED.
Number of eligible EDs was less than the predetermined number of 5 expected participating centers for countries with a population of less than 20 million inhabitants.
Referral ED for children.
Malta: general referral ED treating children; Portugal: 2 secondary care PEDs in a hospital for adults and children; Spain: secondary care PED in a hospital for adults and children; Sweden: secondary care PED for medical conditions. A secondary care PED provides specialist care on referral by primary care, out-of-hospital emergency services, or other smaller hospitals, but does not include highly specialized medical care, which may involve advanced and complex procedures and treatments performed by medical specialists in a tertiary care state-of-the-art facility.
Belgium: 3 centers did not know; Germany: 2 centers did not know; Switzerland: 1 center did not know; UK: 1 center did not know.
Figure 1.
Map of participating countries and number of EDs participating in the survey per country.
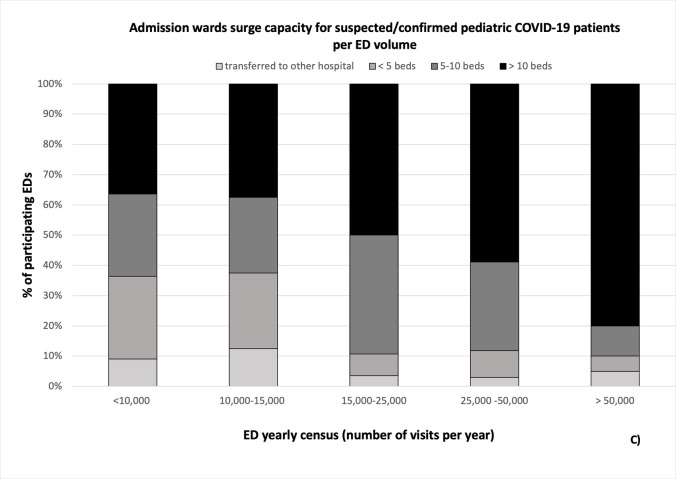
Approximately one third of centers (34%) did not have an ED contingency plan for pandemics and 36% had never organized simulations for such events. The majority of centers (76%) had not experienced mass casualty disasters or pandemics during the past 5 years. Nearly all institutions had established a formal ED management plan for suspected or confirmed pediatric COVID-19 cases, with daily updates in 69% of centers. Surge capacity for pediatric suspected COVID-19 cases was variable between centers at an ED, admission ward, and intensive care level in terms of number of available rooms or beds (Table 2 ). In one fifth of the institutions, there was no intensive care available for pediatric COVID-19 patients. Only admission ward surge capacity increased according to ED volume (Figure E1, available online at http://www.annemergmed.com). Adjustments implemented to best manage suspected or confirmed COVID-19 patients included cancellation of planned activity (ie, outpatient visits, surgery, or hospital admissions) in 90% or more of participating centers, reorganization of beds in other pediatric wards in 75%, and telemedicine in nearly 70%.
Table 2.
Contingency plans, guidelines, and capacity.
| Survey Question | Response Options | Centers (n=102) | % | 95% CI |
|---|---|---|---|---|
| As of March 20, does your hospital have a written and documented contingency plan in the event of a prolonged mass incident event as observed in pandemic infections? | Yes No Do not know |
73 23 6 |
71 23 6 |
62–79 15–32 3–13 |
| As of March 20, does your ED/PED have a written and documented contingency plan in the event of a prolonged mass incident event as observed in pandemic infections? | Yes No Do not know |
64 35 3 |
63 34 3 |
53–71 26–44 1–8 |
| When was the last time you conducted a simulation in your ED/PED on how to manage a mass casualty/epidemic? | Less than a week ago Between a week and a month ago More than a month ago, but less than a year ago More than a year ago Never done |
8 4 34 19 37 |
8 4 33 19 36 |
4–15 1–9 25–43 12–27 28–46 |
| Has your ED/PED managed a mass casualty or epidemic in the last 5 years? | Yes No Do not know |
23 78 1 |
23 76 1 |
15–31 67–83 0.1–5 |
| When did your institution distribute a formal management plan for suspected/confirmed pediatric COVID-19 for your ED? | Between Jan 15 and 31 Between Feb 1 and 15 Between Feb 15 and 29 Between Mar 1 and 15 No formal plan yet I do not remember |
7 15 37 39 2 2 |
7 15 36 38 2 2 |
3–13 9–23 28–64 29–48 0.5–7 0.5–7 |
| Was the management plan above updated regularly? | No formal plan yet No, only 1 plan distributed so far Yes, daily Yes, weekly Yes every 2 wk Yes, but at a different pace from above Do not know |
3 1 70 20 1 5 2 |
3 1 69 19 1 5 2 |
1–8 0.1–5 59–77 13–28 0.1–5 2–11 0.5–7 |
| What is the surge capacity of your ED/PED to assess suspected/confirmed pediatric COVID-19 cases simultaneously? | 1 room 2 rooms 3–5 rooms >5 rooms |
7 19 36 40 |
7 19 35 39 |
3–13 12–27 27–45 30–49 |
| What is the surge capacity at your institution to admit pediatric patients with suspected/confirmed COVID-19 who need admission to the hospital but not intensive care? | I cannot admit these patients in my institution; they are transferred to another hospital <5 beds 5–10 beds >10 beds Do not know |
5 11 28 57 1 |
5 11 27 56 1 |
2–11 6–18 20–37 46–65 0.1–5 |
| What is the surge capacity at your institution to admit pediatric patients with suspected/confirmed COVID-19 cases in (pediatric) intensive care? | No PICU/ICU availability for COVID-19 at my institution <5 beds 5–10 beds >10 beds Do not know |
26 33 20 20 3 |
26 32 20 20 3 |
18–35 24–42 13–28 13–28 1–8 |
| Does your hospital have a formal plan to increase capacity (bed availability) for pediatric patients with suspected/confirmed COVID-19? | Yes No Do not know |
78 22 2 |
77 21 2 |
67–83 15–30 0.5–7 |
| Which of the following adjustments/measures has your hospital taken to be able to best manage pediatric COVID-patients in terms of staff resources/bed availability? [>1 answer possible] | Cancellation of planned outpatient visits Cancellation of planned surgery Cancellation of planned hospital admissions Modification of current accommodation (ie, reorganization of beds in other pediatric wards) Telemetry, remote outpatient clinics, or both by phone/teleconferencing Do not know Other |
94 97 93 76 69 1 8 |
92 95 90 75 68 1 8 |
85–96 89–98 84–95 65–82 58–76 0.1–5 4–15 |
| As part of the hospitalwide contingency COVID-19 plan, is there the possibility that COVID-19 adult patients will be admitted to pediatric beds? | No, we are a stand-alone children’s hospital No, this is not part of the current plan Yes, this is part of the plan if in need to increase capacity for adult COVID-19 patients Do not know Other |
7 46 43 4 2 |
7 45 42 4 2 |
3–13 36–55 33–52 1–9 0.5–7 |
CI, Confidence interval; PICU, pediatric ICU.
The distribution of responses showed variation in the timing of pretriage setup and training on PPE. Variation was also observed in the recommended use of PPE to be worn during pretriage and during patient assessment. For recommended mask use during pretriage, surgical masks were used in 52% of centers, FFP2/N95 masks in 27%, and FFP3/N100 masks in 8%, whereas during patient examination, 49% of centers used FFP2/N95 masks, 43% surgical masks, and 11% FFP3/N100 masks. Recommended PPE use for patients was more consistent across centers, with a surgical mask to be worn by patients in 82% of EDs. Recommended duration of filtering masks use was also variable. A shortage of both basic and aerosol-generating protective PPE items was experienced by nearly two thirds of centers, with FFP2/N95 masks being the items most frequently missing (Table E3, available online at http://www.annemergmed.com). Contagion of health care workers was frequently reported at an institution level (69%), but less so at the ED level (25%). Only 18% of sites endorsed a periodic active surveillance of ED staff. Disposition of health care workers who had been in close contact with a patient with confirmed COVID-19 varied between centers, with approximately one third allowing staff to work while asymptomatic and one third recommending quarantine at home. Overall, emergency physicians shift work had been rearranged in nearly two thirds of centers, with variable adjustments including both increase and reduction in staff, as well as different shift schemes to prevent cross infection among staff (Table E4, available online at http://www.annemergmed.com).
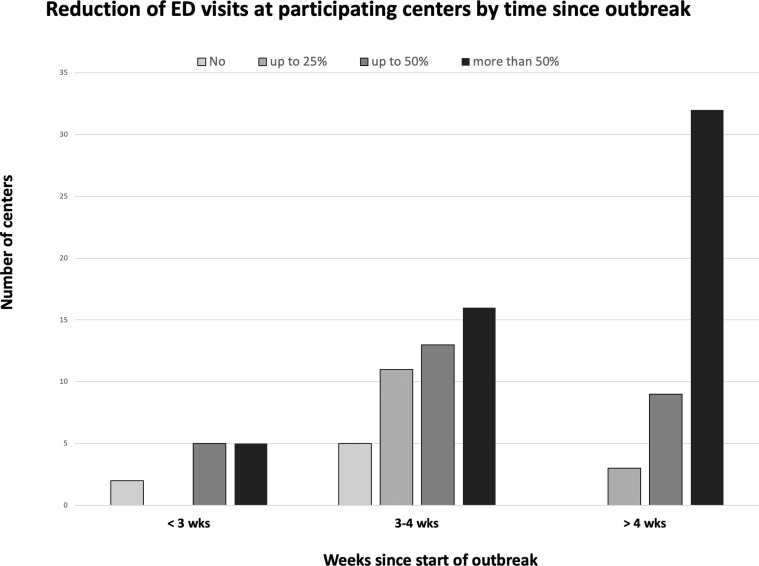
EDs limited caregiver and parent presence to only one person in the majority of centers (84%) and reorganized patient flow to accommodate patients with suspected cases in separate dedicated areas. Less than 20% of EDs had isolation rooms with negative pressure. Most EDs performed swab testing for severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) (78%). However, asymptomatic children with a history of close contact, who could be otherwise discharged, were not tested in the ED in the majority of centers (75%). At most sites, patients with suspected cases who were tested but were fit for discharge were sent home and swab results communicated to the family when they became available. In cases of positive test results for discharged patients, half of the centers could count on specific outpatient services to provide telephone follow-up. Most EDs experienced a substantial reduction in pediatric presentations, by more than 50% in half of the centers (Table E5, available online at http://www.annemergmed.com). Centers farther into the infection spread wave more frequently reported a larger reduction in the number of pediatric presentations (Figure 2 ). Overall, 46% of centers agreed (36%) or strongly agreed (10%) about the statement “My hospital was ready and prepared to handle COVID-19 when the outbreak started in our country” and 54% agreed (39%) or strongly agreed (15%) when the statement referred to ED pediatric care.
Figure 2.
Reported reduction in pediatric ED visits of participating EDs by time since first reported COVID-19 case in their country of origin. Participating EDs were at different time in the pandemic spread.
Limitations
The results of our study should be interpreted in light of its limitations. Although we included a large number of European countries, our survey does not provide a pan-European perspective. However, to our knowledge this is the first European data set that provides a detailed description of pediatric emergency care from within the pandemic, at a more granular level than any institutional channel has been able to provide so far. While the pandemic evolves in each country and accompanying adjustments are made, a repeated focused survey will capture the dynamic progress made from an organizational and operational perspective. We arbitrarily decided, as a research team, the number of centers to be included in each country to ensure a balanced representativeness and to obtain timely completion of the survey. The participating centers represent a subset of EDs caring for children in Europe and include referral centers for children; thus, our findings may not be generalizable across different settings. Although some countries exceeded the expected number of recruited centers, we were able to obtain a reasonable balance in terms of country representativeness. In addition, the objective of this survey was to explore common challenges and common learning points and not to compare responses between countries. Last, although we refined questions through review processes, the survey questions did not undergo a formal content validation procedure. Given that most of the answers required fixed quantitative responses on practice in use or recommended at participating EDs, a formal content validation would have likely had limited influence on the reliability of our findings.
Discussion
Our survey provides a description of preparedness and response of EDs caring for children from 17 European countries and a European-associated country at 1 month after the COVID-19 outbreak started in Northern Italy. Overall, the findings of our study show high variation in time and in level of organizational responses to COVID-19 of EDs caring for children across Europe and identified a few gaps that still need to be optimized to improve preparedness and inform responses to future pandemics. Our data show that a written and documented contingency plan was still missing in approximately one third of centers 1 month after the onset of the outbreak in Europe. Although the majority of EDs had not faced an epidemic or a mass casualty event in the past 5 years, nearly 40% had never run a simulation on how to manage such a crisis in the ED. A striking finding of our point-prevalence survey was the wide variation in reported PPE use at pretriage and for the assessment of suspected COVID-19 cases, with 62% of centers experiencing shortage in one or more PPE items. In addition, a high percentage of centers reported infection in staff members, which may affect the sustainability of care provided. From a structural perspective, the low percentage of EDs with negative-pressure isolation rooms (17%) highlights opportunities for improvement should renovation work be undertaken or new hospitals be built.
Although participating countries were at different stages in the outbreak spread, the different pace in the pandemic advancement represents an opportunity for health care systems to learn from one another by sharing experience and identifying areas for improvement. This may ensure a more rapid response in terms of implementation of infection prevention and control measures within health care in countries that lag the spread wave. This is important at all levels of care within an integrated health care system, but it is paramount for frontline services such as EDs.20 , 21 By March 20, nearly all participating centers had received a formal plan for the management of pediatric suspected or confirmed COVID-19 cases in the ED; however, many faced common challenges: the lack of unequivocal definition of pediatric suspected cases and the need for continuous adjustments as a result of the rapid change of definitions and management plan; the late training in PPE use and shortage in PPE supplies; the need for extra resources to set up a pretriage; the rearrangement of staff shift work to minimize infection spread or to cover for sick colleagues; the lack of negative-pressure isolation rooms; the lack of outpatient services to follow up discharged children with confirmed COVID-19, with possible avoidable representations to the ED; the possibility to admit adult COVID-19 patients into pediatric beds; and the difficult balance of resource use.
Although children have been shown to be relatively spared from this pandemic,5 , 6 , 22 , 23 timely preparation and appropriate response are essential to minimize the transmission of the infection to both patients and health care professionals. Health care facilities have played an unwillingly significant role in increasing viral transmission in this pandemic.24 For physicians taking care of children in the ED, COVID-19 has rightfully been defined a logistic rather than a clinical emergency because a much greater effort was necessary to rapidly reorganize care pathways to prevent infection to patients and staff, rather than to actually provide clinical care to sick children with COVID-19. Not only was the number of confirmed pediatric patients treated at participating EDs at the survey very low (approximately 200 overall) but also ED presentations were substantially reduced, further decreasing the clinical burden.25
Appropriate PPE use is paramount for staff safety and to reduce the risk of viral transmission.26 , 27 Although intubation, manual ventilation, and noninvasive ventilation are rarely needed for pediatric patients with COVID-19,5 , 6 , 22 nearly 80% of participating EDs performed swabbing, which is classified as an aerosol-generating procedure. Although our survey question on use of PPE might have been misinterpreted with respect to assessment by the emergency physician about whether this included aerosol-generating procedures, suboptimal reported practice still emerged from responses. The PPEs recommended by the interim guidance of the European Center for Disease Prevention and Control and the World Health Organization for health care professionals performing aerosol-generating procedures are gown, respirator (N95 or FFP2 standard or equivalent), gloves, eye protection (goggles or face shield), and apron, whereas those providing direct care to patients with COVID-19 should wear a gown, surgical mask, gloves, and eye protection. Health care workers at triage should maintain a distance of at least 1 m and provide the patient with a medical mask (if tolerated); no PPE is required if preliminary screening does not involve direct patient contact.28 , 29 Nearly half of the centers reported a shortage of PPE, most often FFP2/N95 masks. PPE use should be maximized to avoid shortage of supplies, which ultimately exposes staff and the broader community to an increased transmission risk. One third of respondents stated that respirators (N95/FFP2 or FFP3/N100) are disposed of after the assessment of each patient with a suspected case of COVID-19. This practice may contribute to shortage of supplies because the same respirator could be used for more than one patient, as long as it is not damaged or soiled.29
Approximately 70% of respondents were aware of infected health care workers at their institution, whereas one fourth reported infected staff in the ED. Unfortunately, infection of health care workers has been reported as a major threat to the sustainability of health care in this pandemic.26 In fact, the disposition of health care professionals who had been in close contact with a patient with confirmed COVID-19 varied between centers, possibly because of concerns regarding service provisions.
Implementation of appropriate PPE use can be easily done and should occur in a timely manner. This is in contrast to barriers related to structural limitations and constraints affecting the organization of ED patient flow and isolation capacity, which may be difficult to overcome in a short time frame. Infection control measures were more consistently reported in the survey, including rearrangement of ED patient flow, changing of staff work shift to optimize resource use, reduction in the number of care givers allowed with the child, and home quarantine for pediatric patients with confirmed COVID-19 who were fit for discharge.
Another interesting finding from our survey is the substantial reduction in pediatric ED presentations during the pandemic. Centers from countries with a longer time since first case experienced higher reductions in the number of ED presentations. Parents’ fear of contagion in a health care environment, improved hygiene measures, reduced community transmission of communicable diseases, reduced opportunities to sustain injuries owing to the strict containment measures enforced by governments, and reduction in stress-related functional diseases may be the reasons underlying this phenomenon. Reports from previous epidemics also showed an overall decrease in pediatric ED attendances.30 , 31 The Middle East respiratory syndrome (MERS) outbreak had resulted in a significantly higher proportion of high-acuity ED pediatric presentations and an increase in delayed presentations.9 , 32
Despite its limitations, the provision of a timely report on preparedness and response in pediatric emergency care during the pandemic is useful to inform practice and policymakers to properly reorganize health systems while the crisis is still evolving. It provides an accurate objective historical data set from which lessons can be learned, including for adult EDs. The collaboration of the REPEM and PERUKI European networks was instrumental in ensuring wide representation of European countries and timely completion of this multinational point-prevalence survey. The data provided highlight the importance of European multinational research collaborations to provide the best care to children in the front line.
In summary, we identified variability and gaps in preparedness and response to the COVID-19 epidemic across European referral EDs for children at 1 month since the start of the outbreak in Northern Italy. A lack of early availability of a written and documented contingency plan including detailed infection control measures, in the provision of simulation training, appropriate use of PPE, and appropriate isolation facilities emerged as gaps that should be optimized to improve the preparedness and inform responses to future pandemics.
Country leads list (country leads collaborated closely with the research team and were instrumental in the dissemination and completion of the survey)
Said Hachimi-Idrissi, Ghent University Hospital, Ghent, Belgium; Marianne Sjølin Frederiksen, Copenhagen University Hospital, Herlev, Denmark; Ulle Uustalu, Tallinn Children's Hospital, Estonia; Gerard Cheron, Necker enfants malades, Universitè de Paris, France; Florian Hoffmann, von Hauner University Children's Hospital Munich, Germany; Valtyr Thors, Childreńs hospital Iceland. Landspitali University Hospital, Iceland; Michael J Barrett, Children's Health Ireland at Crumlin, Ireland; Itai Shavit, Rambam Health Care Campus, Israel; Zanda Pucuka, BKUS Children clinical university hospital, Latvia; Lina Jankauskaite, Hospital of Lithuanian University of Health Sciences Kauno Klinikos, Lithuania; Patrícia Mação, Hospital Pediátrico, Centro Hospitalar e Universitário de Coimbra, Portugal; Ioannis Orfanos, Skane University Hospital, Sweden; and Laurence Lacroix, Geneva University Hospitals, Switzerland.
Acknowledgments
The authors acknowledge all the respondents to the survey who gave permission for their names to be included: Carlos Luaces Cubells, Head Pediatric Emergency Department Hospital Sant Joan de Deu, Barcelona, Spain; Aline Malterre, Center Hospitalier Intercommunal de Créteil, France; Anne Louise Bischoff, Hilleroed Hospital the Capital Region of Denmark, Denmark; Letitia Pantalone, GHT NOVO, CH René Dubos, Pontoise, France; Silvia Oliva Rodriguez-Pastor, Hospital Regional Universitario Málaga, Spain; Elias Ossam, Center Hospitalier de Gonesse, France; Sheena Durnin, Children's Health Ireland at Tallaght University Hospital, Dublin, Ireland; Arístides Rivas, Gregorio Marañón University Hospital, Madrid, Spain; Antón Castaño-Rivero, Hospital Universitario de Cabueñes, Gijón, Asturias, Spain; Mercedes de la Torre, Hospital infantil universitario Niño Jesús, Madrid, Spain; Orla Neylon, University Hospital Limerick, Ireland; Donatella De Martiis, Pronto Soccorso Pediatrico, ASST Spedali Civili Brescia, Italy; Vincenzo Tipo and Angela Mauro, Pediatric Emergency Department, Santobono-Pausilipon Children's Hospital, Naples, Italy; Antonio Chiaretti, Pediatric Emergency Department, Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy; Marcello Lanari, Pediatric Emergency Department, Bologna, Italy; Claudio Germani, Pediatric Emergency Department, Institute for Maternal and Child Health IRCCS, Burlo Garofolo, Trieste, Italy; Antonio Francesco Urbino, Pediatria d'Urgenza–AOU Città della Salute e della Scienza, Turin, Italy; Olivier Richer, Emergency Department, Hopital des Enfants CHU, Bordeaux, France; Faraaz Bhatti, Department of Emergency Medicine, Gozo General Hospital, Malta; Patricia Mação, Pediatric Emergency Service, Hospital Pediátrico, Centro Hospitalar e Universitário de Coimbra, Portugal; Roberto Velasco, Pediatric Emergency Unit, Rio Hortega Universitary Hospital, Valladolid, Spain; Teresa Castro, Hospital Espírito Santo de Évora, Portugal; Fuchs Hans, Center for Pediatrics, University of Freiburg, Germany; Kathryn Allison and Asim Ijaz, Children's Research Practitioner Royal Lancaster, Lancaster, United Kingdom; Isabelle Claudet, Pediatric Emergency Department, Children Hospital, Toulouse University Hospital, Toulouse, France; Anne Cavau, and Mélusine Kiener, Pediatric Emergency Department, Armand Trousseau University Hospital, Paris, France; Rouget Sebastien, Service de pediatrie Center Hospitalier Sud-Francilien, Corbeil-Essonnes, France; Mia Ferch, Pediatric Department, Aarhus University Hospital, Denmark; Shrouk Messahel, Alder Hey Children's Hospital NHS Foundation Trust, Liverpool, United Kingdom; Grosse Lordemann Anja, Altoner Kinderkrankenhaus, Hamburg, Germany; Vanda Anacleto Bento, Hospital Fernando Fonseca, Amadora, Portugal; Mark D. Lyttle, Emergency Department, Bristol Royal Hospital for Children, Bristol, United Kingdom; Rikke Møller Andersen, Pediatric Department Hospital of Lillebelt, Kolding, Denmark; Jorge Sotoca Fernández and Ingunn Olafsdotter, Skåne University Hospital, Malmö & Lund, Sweden; Andrés Gonzalez Hermosa, Pediatric Emergency, Basurto University Hospital, Bilbao, Spain; Escoda Simon, Pediatric Emergency Department, Center Hospitalier Delafontaine de Saint-Denis, France; Cosette Pharisa Rochat, HFR-Fribourg, Fribourg, Switzerland; Paddy Fitzpatrick, Children’s Health Ireland at Temple Street, Dublin, Ireland; Emily Walton, Royal Alexandra Children's Hospital, Brighton, United Kingdom; Idanna Sforzi, Emergency Department, Meyer Children's Hospital, Florence, Italy; Hoeffe Julia, Pediatric Emergency Department, Inselspital University Hospital Bern, Switzerland; Marta Romanengo, Pediatric Emergency, Ospedale Gaslini, Genova, Italy; Susana Castanhinha, Hospital Dona Estefânia–Centro Hospitalar Lisboa Central, Portugal; Helle Christiansen, Department of Pediatrics, Hvidovre Hospital, Denmark; Barbara Maria Cantoni, Dipartimento delle Professioni Sanitarie, IRCCS Ca Granda Ospedale Maggiore Policlinico, Milan, Italy; Sofia Reis, Centro Hospitalar Tondela-Viseu, Viseu, Portugal; Eich Christoph Bernhard, Pediatric Intensive Care and Emergency Medicine, Auf der Bult Children's Hospital, Hannover, Germany; Georg Staubli, Universitiy Hospital Zürich, Zürich, Switzerland; Wolf Pauline, Antoine Béclère Hospital, Clamart, France; Rachel Pellaton, Hôpital de l'Enfance de Lausanne, Lausanne, Switzerland; Kurt Anseeuw, ZNA Stuivenberg, Antwerp, Belgium; Davide Silvagni and Pietro Soloni, Pediatric Emergency Department and Critical Care Unit, Azienda Ospedaliera Universitaria integrata, Verona, Italy; Higuet Adeline, Emergency Sint Maria Halle, Belgium; Mirjam van Veen, Groene hart ziekenhuis, Gouda, the Netherlands; Gerlant van Berler, Department of Emergency and Disaster Medicine, Universitair Ziekenhuis Brussels, Brussels, Belgium; Giora Weiser, Pediatric Emergency Department, Shaare Zedek Medical Center, Jerusalem, Israel; Nicolas Mpotos, St Lucas General Hospital, Ghent, Belgium; Nir Friedman, Pediatric Emergency Medicine, Safra Children's Hospital, Sheba Medical Center, Tel Hashomer, Israel; Michal Maimon, Pediatric Emergency Medicine, Soroka University Medical Center, Beer Sheva, Israel; Uri Balla, Pediatric Emergency Department of Kaplan Medical Center, Rehovot, Israel; Ayelet Rimon, Division of Pediatric Emergency Medicine, Department of Pediatrics, Dana-Dwek Children Hospital, Sackler School of Medicine, University of Tel Aviv, Israel; Karin Biswanger, Department of Pediatrics, Södra Älvsborgs Hospital, Sweden; and Virginia Gómez Barrena, Pediatric Emergency, Hospital Universitario Miguel Servet, Zaragoza, Spain.
Footnotes
Please see page 789 for the Editor’s Capsule Summary of this article.
Supervising editor: Jocelyn Gravel, MD. Specific detailed information about possible conflict of interest for individual editors is available at https://www.annemergmed.com/editors.
Author contributions: SB and SM were responsible for conceiving the study. SB obtained and analyzed the data and wrote the initial draft of the article. DB, RF, NP, RO, LT, DR, RGN, IM, LDD, and SM critically revised the draft of the article. DB designed the draft of the survey. All authors designed the study, interpreted the data, gave final approval for publishing, and agreed to be accountable for all aspects of the work. SB takes responsibility for the paper as a whole.
All authors attest to meeting the four ICMJE.org authorship criteria: (1) Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND (2) Drafting the work or revising it critically for important intellectual content; AND (3) Final approval of the version to be published; AND (4) Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding and support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). The authors have stated that no such relationships exist.
Readers: click on the link to go directly to a survey in which you can provide feedback to Annals on this particular article.
A podcast for this article is available at www.annemergmed.com.
Contributor Information
Country Leads:
Said Hachimi-Idrissi, Marianne Sjølin Frederiksen, Ulle Uustalu, Gerard Cheron, Florian Hoffmann, Valtyr Thors, Michael J. Barrett, Itai Shavit, Zanda Pucuka, Lina Jankauskaite, Patrícia Mação, Ioannis Orfanos, and Laurence Lacroix
Supplementary Data
Containment/restrictive measures enforced in participating countries as of March 20
Table E3. Personal protective equipment and pretriage.
Table E4. ED Staff safety and service sustainability
Table E5. Logistics and organization of ED management
Figure E1.
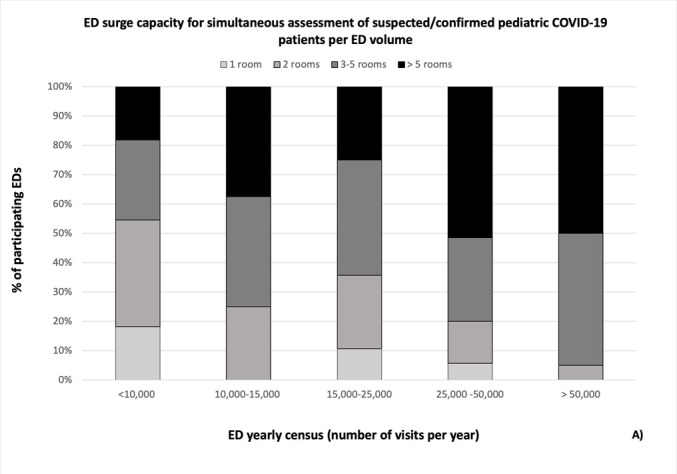
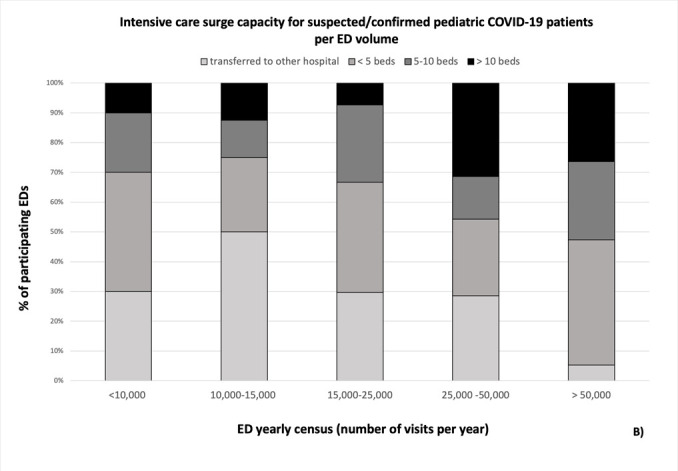
Percentage distribution of ED (A), ICU (B) and admission ward (C) surge capacity according to ED volume
References
- 1.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Porcheddu R., Serra C., Kelvin D. Similarity in case fatality rates of Covid-19/SARS-COV-2 in Italy and China. J Infect Dev Ctries. 2020;14:125–128. doi: 10.3855/jidc.12600. [DOI] [PubMed] [Google Scholar]
- 3.Garcia-Castrillo L., Petrino R., Leach R. European Society for Emergency Medicine position paper on emergency medical systems response to COVID-19. Eur J Emerg Med. 2020;27:174–177. doi: 10.1097/MEJ.0000000000000701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The Lancet. COVID-19: learning from experience. Lancet. 2020;395:1011. doi: 10.1016/S0140-6736(20)30686-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Qiu H., Wu J., Hong L. Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID-19) in Zhejiang, China: an observational cohort study. Lancet Infect Dis. 2020;20:689–696. doi: 10.1016/S1473-3099(20)30198-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dong Y., Mo X., Hu Y. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics. 2020;145:e20200702. [Google Scholar]
- 7.Zimmermann P., Curtis N. Coronavirus infections in children including COVID-19. Pediatr Infect Dis J. 2020;39:355–368. doi: 10.1097/INF.0000000000002660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen Z.M., Fu J.F., Shu Q. Diagnosis and treatment recommendations for pediatric respiratory infection caused by the 2019 novel coronavirus. World J Pediatr. 2020 doi: 10.1007/s12519-020-00345-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jeong H., Jeong S., Oh J. Impact of Middle East respiratory syndrome outbreak on the use of emergency medical resources in febrile patients. Clin Exp Emerg Med. 2017;4:94–101. doi: 10.15441/ceem.16.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adams J.G., Walls R.M. Supporting the health care workforce during the COVID-19 global epidemic. JAMA. 2020 doi: 10.1001/jama.2020.3972. [DOI] [PubMed] [Google Scholar]
- 11.European Society for Emergency Medicine https://eusem.org/ Available at:
- 12.Bressan S., Titomanlio L., Gomez B. Research priorities for European pediatric emergency medicine. Arch Dis Child. 2019;104:869–873. doi: 10.1136/archdischild-2019-316918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hartshorn S., O'Sullivan R., Maconochie I.K. Establishing the research priorities of pediatric emergency medicine clinicians in the UK and Ireland. Emerg Med J. 2015;32:864–868. doi: 10.1136/emermed-2014-204484. [DOI] [PubMed] [Google Scholar]
- 14.Mintegi S., Shavit I., Benito J. Pediatric emergency care in Europe: a descriptive survey of 53 tertiary medical centers. Pediatr Emerg Care. 2008;24:359–363. doi: 10.1097/PEC.0b013e318177a762. [DOI] [PubMed] [Google Scholar]
- 15.Burns K.E., Duffett M., Kho M.E. A guide for the design and conduct of self-administered surveys of clinicians. CMAJ. 2008;179:245–252. doi: 10.1503/cmaj.080372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harris P.A., Taylor R., Minor B.L. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.European Center for Disease Prevention and Control. https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases COVID-19 situation update worldwide, as of 5 June 2020. Available at:
- 18.World Meter. Reported Cases and Deaths by Country, Territory, or Conveyance. Available at: https://www.worldometers.info/coronavirus/#countries. Accessed March 21, 2020.
- 19.von Elm E., Altman D.G., Egger M., for the STROBE Initiative The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147:573–577. doi: 10.7326/0003-4819-147-8-200710160-00010. [DOI] [PubMed] [Google Scholar]
- 20.Filice C.E., Vaca F.E., Curry L. Pandemic planning and response in academic pediatric emergency departments during the 2009 H1N1 influenza pandemic. Acad Emerg Med. 2013;20:54–62. doi: 10.1111/acem.12061. [DOI] [PubMed] [Google Scholar]
- 21.Morton M.J., Kirsch T.D., Rothman R.E. Pandemic influenza and major disease outbreak preparedness in US emergency departments: a survey of medical directors and department chairs. Am J Disaster Med. 2009;4:199–206. [PubMed] [Google Scholar]
- 22.Sinha I.P., Harwood R., Semple M.G. COVID-19 infection in children. Lancet Respir Med. 2020;8:446–447. doi: 10.1016/S2213-2600(20)30152-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Castagnoli R., Votto M., Licari A. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review. JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.1467. [DOI] [PubMed] [Google Scholar]
- 24.Wang C., Horby P.W., Hayden F.G. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chidini G., Villa C., Calderini E. SARS-CoV-2 infection in a pediatric department in Milan: a logistic rather than a clinical emergency. Pediatr Infect Dis J. 2020;39:e79–e80. doi: 10.1097/INF.0000000000002687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lancet. COVID-19: protecting health-care workers. Lancet. 2020;395:922. doi: 10.1016/S0140-6736(20)30644-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schwartz J., King C.C., Yen M.Y. Protecting health care workers during the COVID-19 coronavirus outbreak: lessons from Taiwan’s SARS response. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.European Center for Disease Prevention and Control Infection prevention and control for COVID-19 in healthcare settings—first update. https://www.ecdc.europa.eu/en/publications-data/infection-prevention-and-control-covid-19-healthcare-settings-copy-to-clipboard Available at:
- 29.World Health Organization Rational use of personal protective equipment for coronavirus disease (COVID-19): interim guidance. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/infection-prevention-and-control Available at:
- 30.Stevenson E., Barrios L., Cordell R. Pandemic influenza planning: addressing the needs of children. Am J Public Health. 2009;99(suppl 2):S255–260. doi: 10.2105/AJPH.2009.159970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lee S.Y., Khang Y.H., Lim H.K. Impact of the 2015 Middle East respiratory syndrome outbreak on emergency care utilization and mortality in South Korea. Yonsei Med J. 2019;60:796–803. doi: 10.3349/ymj.2019.60.8.796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pek S.H., Kim D.K., Lee J.H. The impact of Middle East respiratory syndrome outbreak on trends in emergency department utilization patterns. J Korean Med Sci. 2017;32:1576–1580. doi: 10.3346/jkms.2017.32.10.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Containment/restrictive measures enforced in participating countries as of March 20
Table E3. Personal protective equipment and pretriage.
Table E4. ED Staff safety and service sustainability
Table E5. Logistics and organization of ED management