As of April 18, a total of 2,121,675 persons in 213 countries were reported to be infected by SARS-CoV-2, which causes coronavirus disease 2019 (COVID-19), a disease that had led to 142,299 deaths [1]. Strict self-isolation of the local population is implanted to limit human-to-human transmission, leading to an extreme scarcity of blood donors and the associated allogenic blood products. In addition, more and more asymptomatic infections are being found among COVID-19 cases in endemic areas. Viral shedding in plasma or serum increases the potential risk of transmission of coronaviruses through the transfusion of labile blood products [2]. In our hospital, many of the scheduled major cancer surgeries were postponed for over a week due to a shortage of allogenic blood supplies, resulting in a failure to achieve optimal timing for these procedures and an adverse effect on prognosis. Anesthesiologists and surgeons should actively communicate and cooperate for benefit of patients facing this intractable situation [3]. Acute normovolemic hemodilution (ANH) has been confirmed to decrease perioperative allogenic blood transfusion in major surgery patients [4,5], which is applicable but often ignored by many surgeons and anesthesiologists. Therefore, we performed a retrospective study to investigate whether ANH permits major cancer surgeries to be performed safely and at the earliest in such a situation of insufficient allogenic blood supplies.
This retrospective study's protocol was approved by the Institutional Review Board of our hospital (#2020-SR-110). In our hospital, the surgical treatments of 22 cancer patients scheduled for major cancer surgeries were cancelled multiple times because of the shortage of allogenic blood supplies during February 2020. ANH was applied to these patients at the suggestion of anesthesiologists.
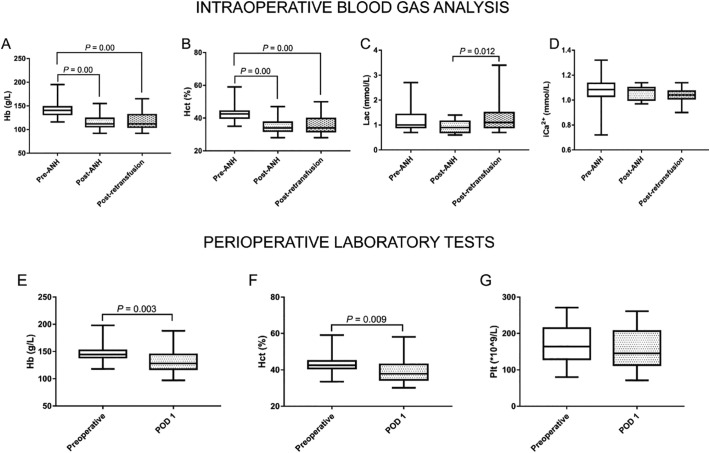
All patients examined successfully underwent the scheduled surgeries. The baseline demographics, comorbidities, and types of surgery were shown in Table 1 . The volumes of ANH blood drawn and intraoperative blood loss were 400–800 mL and 100–1300 mL, respectively. Only one patient received 2 units of erythrocytes intraoperatively. As shown in Fig. 1 , compared with levels of hemoglobin and hematocrit immediately before ANH, the levels of these parameters decreased significantly immediately after ANH and immediately after retransfusion (all P < 0.05). When the autologous blood was transfused back into the patient, the lactate level increased (median [interquartile ranges]: 1.10 mmol/L [0.90, 1.15] vs. 0.90 mmol/L [0.70, 1.15], P = 0.012), but it still remained within the normal range (<2.0 mmol/L). Hemoglobin and hematocrit at postoperative day 1 were significantly lower than the preoperative levels (median [interquartile ranges]: 128 g/L [118, 145] vs. 145 g/L [139, 152], P = 0.003; 37.9% [34.5, 43.0] vs. 42.5% [40.8, 44.9], P = 0.009, respectively). Even so, during the postoperative follow-up, none of the patients were reported to experience the following postoperative adverse events: bleeding requiring reoperation, ischemic events (including myocardial/cerebral infarction), and in-hospital death.
Table 1.
Baseline demographics, comorbidities, and types of surgery.
| Parameters | Summary statistics (n = 22) |
|---|---|
| Age (y) | 57 ± 15 |
| BMI (kg/m2) | 24.6 ± 2.8 |
| Gender (M/F) | 22/0 |
| ASA-PS | |
| 1 | 2 (9.1%) |
| 2 | 19 (86.4%) |
| 3 | 1 (4.5%) |
| Comorbidities | |
| Hypertension | 12 (54.5%) |
| Diabetes | 4 (18.2%) |
| Types of surgery | |
| Pancreatoduodenectomy | 1 (4.5%) |
| Laparoscopic radical nephrectomy | 2 (9.1%) |
| Laparoscopic radical prostatectomy | 2 (9.1%) |
| Laparoscopic radical cystectomy | 2 (9.1%) |
| Intracranial tumor resection | 1 (4.5%) |
| Thoracoscopic pulmonary resection | 1 (4.5%) |
| Radical resection of liver cancer | 9 (40.9%) |
| Esophagectomy | 3 (13.6%) |
| Malignant bone tumor resection | 1 (4.5%) |
Values were presented with mean ± standard deviation or number (%) as appropriate.
ASA-PS: Anesthesiologists physical status, BMI: body mass index.
Fig. 1.
Results of intraoperative blood gas analysis and perioperative laboratory tests. A–D) Intraoperative Hb, Hct, Lac, and iCa2+ levels. E–G) Perioperative Hb, Hct, and Plt levels. Values was presented as median and interquartile range, and analyzed with the Mann-Whitney test or Kruskal-Wallis H test as appropriate. ANH: acute normovolemic hemodilution, Hb: hemoglobin, Hct: hematocrit, iCa2+: ionized calcium, Lac: lactate, Plt: platelet, POD: postoperative day.
Because safety is a major focus of surgical and perioperative care, preoperatively acquired blood and blood products remain a routine safeguard for patients undergoing major cancer surgeries. Although the absolute risk/benefit ratio for ANH is controversial, it is crucial to protect cancer patients from experiencing acute blood loss-induced life-threatening situation. In clinical settings, we should address how anatomical features relevant to the surgery, complexity of resections, and technical skills of surgeons might induce massive intraoperative bleeding. A failure to consider these factors, without the availability of substantial allogenic blood supplies, would endanger patients.
In conclusion, anesthesiologists and surgeons must work together to surpass and overcome this intractable period. One of the beneficial procedures is to use ANH for patients with cancer to permit major surgeries to be performed at the earliest without further delays.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
IRB contact information
This retrospective study was approved by the Institutional Review Board of the First Affiliated Hospital with Nanjing Medical University on March 10, 2020 (#2020-SR-110).
Declaration of competing interest
None.
Acknowledgment
We would like to thank Editage (www.editage.com) for English language editing.
References
- 1.Coronavirus disease (COVID-19) pandemic. Geneva: World Health Organization (https://www.who.int/emergencies/diseases/novel-coronavirus-2019) [accessed 18 April 2020].
- 2.Chang L., Yan Y., Wang L. Coronavirus disease 2019: coronaviruses and blood safety. Transfus Med Rev. 2020 doi: 10.1016/j.tmrv.2020.02.003. [published online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Klein A.A., Earnshaw J.J. Perioperative care and collaboration between surgeons and anaesthetists - it’s about time. Anaesthesia. 2020;107:e6–e7. doi: 10.1002/bjs.11445. [DOI] [PubMed] [Google Scholar]
- 4.Kinoshita H., Mikami N., Saito J., Hirota K. Impact of acute normovolemic hemodilution on allogeneic blood transfusion during open abdominal cancer surgery: a propensity matched retrospective study. J Clin Anesth. 2020;64 doi: 10.1016/j.jclinane.2020.109822. [published online ahead of print] [DOI] [PubMed] [Google Scholar]
- 5.Saito J., Masui K., Noguchi S., Nakai K., Tamai Y., Midorikawa Y., et al. The efficacy of acute normovolemic hemodilution for preventing perioperative allogeneic blood transfusion in gynecological cancer patients. J Clin Anesth. 2020;60:42–43. doi: 10.1016/j.jclinane.2019.08.025. [DOI] [PubMed] [Google Scholar]