Abstract
These best practice recommendations for ENT consultations during the COVID-19 pandemic have been drawn up because ENT examinations and treatments are at risk of contamination by the SARS-Cov-2 virus in certain instances. Thus, ENT specialists are among the professionals who are most exposed to this infection. During the pandemic, insofar as an asymptomatic patient may be infected and contagious, the same precautions must be employed whether the patient is ill with, suspected of having, or without any clinical evidence of COVID-19 infection. According to the scientific data available, the examinations and procedures potentially exposing to projections/aerosolizations of organic material of human origin are considered to be at risk of staff contamination. For ENT examinations and procedures without exposure to such projections/aerosolizations, the professional is advised to a long sleeve clean outfit, a surgical mask and gloves in case of contact with the patient's mucosa. ENT examinations and procedures with exposure to these projections/aerosolizations require the so-called “airborne”, “contact”, and “droplets” additional precautions: FFP2/N95 respiratory protection device, eye protection, disposable headwear and long sleeve overgown.
Keywords: COVID-19 pandemic, Otolaryngology, SARS-CoV-2, Personal protective equipment (PPE), FFP2/N95 Mask
1. Introduction
In the context of the COVID-19 pandemic, the French government decided to implement a lockdown of the population, reducing ENT activities to emergency treatments and those that could not be deferred without constituting a real loss of chance for the patient's recovery or survival (https://solidarites-sante.gouv.fr/IMG/pdf/guide-covid-19-phase-epidemique-v15-16032020.pdf. 16 March 2020). Practical sheets for patients (Fig. 1 ) and practitioners (Fig. 2 ) were drawn up jointly by the French ENT Society (SFORL), the French ENT National Union, the French ENT College, and the French National Professional ENT Council to guide the choice between calling the French emergency services (dialling 15), teleconsultation, face-to-face consultation, and postponing the consultation. To allow the population to visit ENT practices confidently and avoid postponing urgent treatments, enhanced protective measures were laid out by the Health Ministry in conjunction with the French Public Health Council and the French Society for Hospital Hygiene. These were circulated in town-based practices and in regional healthcare facilities by the network of Support Centres for the Prevention of Healthcare-associated Infections. As the independent and apolitical French organization called Institut de Santé (“Health Institute”) points out, some treatments of ENT diseases that could have been deferred by a few weeks are now becoming urgent at the risk of constituting a real loss of chance for the patient's recovery or survival (https://www.institut-sante.org/covid19-plan-de-sortie-de-crise-de-linstitut-sante/). The protective measures applied during the lockdown period will be maintained once the lockdown is over to allow the resumption of treatments and to prevent their cessation and delay. ENT specialists in private practices and in hospitals have a proactive role to play for their patients (https://solidarites-sante.gouv.fr/IMG/pdf/organisation_soins-hospitaliers_covid-19.pdf). The best practice recommendations for ENT consultations during the COVID-19 pandemic have been drawn up because ENT examinations and treatments risk the practitioner being exposed to SARS-CoV-2 contamination in certain instances [1]. Thus, ENT specialists are among the professionals who are most exposed to COVID-19.
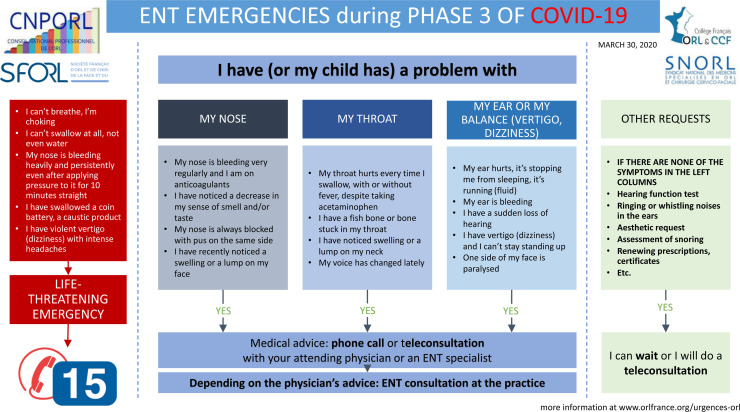
Fig. 1.
Information sheet for patients with ENT symptoms or pathologies in phase 3 of the COVID-19 epidemic (issued March 31, 2020).
Fig. 2.
Sheet for ENT specialists. Organization of patient care according to their ENT symptoms or pathology (emergency call, teleconsultation, face-to-face consultation or postponement of consultation) in phase 3 of the COVID-19 epidemic (issued April 6, 2020).
2. Organisation of the ENT practice
The recommended hygiene measures and set up of separate pathways for patients infected with SARS-Cov-2 and for non-infected patients imply specific adaptations of the organization and equipment of the ENT practice (https://solidarites-sante.gouv.fr/IMG/pdf/consignes-hygiene-cabinets-ville-covid19.pdf). These adaptations encompass the provision of the protection devices necessary for professionals and patients, identified access points, waiting room layouts, and staggering consultation time slots (https://solidarites-sante.gouv.fr/IMG/pdf/organisation_soins-hospitaliers_covid-19.pdf). The conditions for resuming activity are organized within each region by the Regional Health Agencies and are based on mobilising all ENT specialists in public and private healthcare facilities.
2.1. Advice to patients
It is advised to give your patients the link to the “Maladie Coronavirus” website co-developed by the Institut Pasteur research institute and the Assistance publique–Hôpitaux de Paris (university hospital trust operating in Paris and its surroundings) (https://maladiecoronavirus.fr). This website is intended to inform them of what they should do in the event that they have symptoms suggestive of COVID-19 (Box 1 ). The face-to-face ENT consultation appointment must be postponed if the patient shows the symptoms on the Maladie Coronavirus website. In this case, the patient must contact their attending physician or the emergency services. Emergency treatment can justify referring the patient to an ENT clinic suitable for the care of COVID positive patients. The patient is advised to go to the ENT consultation alone and at the exact time of the appointment. For specific circumstances (children, dependent people, etc.), it is advised that only one person accompany them. They are advised to bring their own pen and to pay for the consultation by card. On arriving at the ENT practice, they will be asked to rub their hands with a virucidal hydro-alcoholic solution (HAS) corresponding to the European norm 14476 or to wash their hands with soft soap followed by drying their hands with single-use hand towels. Depending on the decision of the consultant or the facility, the decision may also be taken to have each patient wear a surgical mask, or only the most vulnerable ones.
Box 1. Symptoms informing the patient population about the Coronavirus Disease, from the Maladie Coronavirus website (https://maladiecoronavirus.fr, co-developed by the Institut Pasteur and the Assistance publique–Hôpitaux de Paris).
-
•
Your temperature is high in the last 48 h
-
•
You have a cough, or your usual cough has gotten worse in the last few days
-
•
You have noticed a large decrease or loss in your sense of taste or smell in the last few days
-
•
You have had a sore throat and/or muscle pains and/or unusual aches in the last few days
-
•
You have had diarrhoea, with at least three loose stools, in the last 24 h
-
•
You have been unusually tired in the last few days
-
•
You have been unable to eat or drink in the last 24 hor more
-
•
You have noticed an unusual shortness of breath when you talk or when you lightly exert yourself in the last 24 h
2.2. Secretary/Reception
Distancing measures must be implemented from the beginning of the ENT consultation. The measures can be adapted depending on the layout of the premises: floor markings for a distance of at least 1 metre with the reception desk, counter window or transparent panel, mask or visor covering the assistant's face, HAS before dealing with a new patient and after handling objects (health insurance card, paper documents, payment card, etc.). It is recommended to remove any objects present on the work surface (there will be no pen available for the patient). It is advised to rub hands with HAS after handling health insurance and bank cards. Likewise, hands must be rubbed with HAS after handling cash.
2.3. Waiting room
Adapting to the layout of the premises, the waiting room is arranged to guarantee the appropriate hygiene precautions and social distancing (https://solidarites-sante.gouv.fr/IMG/pdf/consignes-hygiene-cabinets-ville-covid19.pdf). Standard hygiene measures are effective at limiting the spread of SARS-CoV-2. A distance of at least one meter must be maintained between patients seated in the waiting room. Information signs must be placed in the waiting room (posters). The following must be provided in the waiting room: single-use tissues, bins with bags and lids, HAS for disinfecting hands, a sink with soft liquid soap and single-use hand towels for washing hands. Any superfluous furniture, papers, and toys should be removed from the waiting room. Waste from potentially ill people must be eliminated.
Regarding disinfection techniques, the risk that contaminated aerosols originating from droplets emitted by COVID-19 positive patients could contaminate the waiting room (chairs, furniture, work surfaces, floor, etc.) must be taken into account. As per the recommendations of the French Society for Hospital Hygiene, the usual measures for bio-cleaning health care premises are effective for inactivation of SARS-CoV-2, once the products used are adapted (https://solidarites-sante.gouv.fr/IMG/pdf/consignes-hygiene-cabinets-ville-covid19.pdf; https://www.sf2h.net/wp-content/uploads/2020/02/Avis-SF2H-05-avril-2020-Désinfection-scanner-et-autres-appareils-dimagerie.pdf). Human coronaviruses can be effectively inactivated by surface disinfection procedures with solutions containing 62–71% ethanol, 0.5% hydrogen peroxide or 0.1% sodium hypochlorite with a minimum contact time of 1 min. By analogy with other enveloped viruses, disinfectant cleaners meeting European virucidal standard EN 14476 for enveloped viruses (Vaccinia test strain) would inactivate SARS-CoV-2 (https://www.sf2h.net/wp-content/uploads/2020/02/Avis-SF2H-05-avril-2020-Désinfection-scanner-et-autres-appareils-dimagerie.pdf). In practice, it is recommended to clean frequently touched surfaces with 14476-standard virucidal disinfectant cleaning wipes at least twice a day, paying particular attention to surfaces in direct contact with patients (door handles, furniture, toilet flush, sink, etc.), to ventilate the premises extensively and regularly, and to schedule a complete bio-cleaning once a day (preferably in the evening).
2.4. Consultation premises
As for the waiting room, it is advisable to remove from the consultation room any useless furniture or object (toys…). Single-use tissues, bins with bags and lids, and HAS for disinfecting hands must be available. The patient will use their own pen to fill out documents such as a surgery consent form. The room disinfection and ventilation techniques are identical to those described in the previous paragraph.
2.5. Personal protective equipment of staff members not directly involved in healthcare
Staff not dedicated to healthcare but responsible for welcoming and orienting the patient, as well as taking information, wears professional attire. They keep a distance of at least 1 metre from patients. As a precaution and depending on the decision of the consultant or the facility, the decision may be taken to have each team member wear a surgical mask. Lastly, the decision may be taken not to rely on non-medical staff.
2.6. Personal protective equipment of ENT medical teams outside of the current COVID-19 pandemic period
ENT medical team already take the standard precautions assuming that each individual is potentially a carrier of, colonised by, or infected by micro-organisms that can be transmitted during treatment (https://www.sf2h.net/publications/actualisation-precautions-standard-2017). During ENT examinations or procedures without exposure to projection/aerosolization of organic material of human origin (PAOM) (Table 1 ), the ENT medical team wear clean outfits as well as single-use gloves in case of contact with a mucosa (Table 2 ). For examinations and procedures with exposure to PAOM (Table 1), protection must be supplemented by wearing a surgical mask, protective goggles (glasses do not ensure this protection), a single-use plastic apron, and single-use gloves (Table 2). For patients who are known carriers of or infected by certain pathogens, protection can be supplemented in three different ways according to the type of infectious agents. As part of “contact” precautions, wearing a single-use plastic apron (Methicillin-resistant Staphylococcus aureus, Extended spectrum β-Lactamase producing enterobacteriaceae, Enterococcus faecalis of intermediate sensitivity or resistant to vancomycin, cutaneous staphylococci and streptococci, herpes, hepatitis A and E, Rotavirus, etc.) or a long-sleeved overgown (scabies, Clostridium difficile infection, acute gastroenteritis) is recommended. As part of “droplet” precautions, which are necessary in particular in case of seasonal flu, respiratory syncytial virus infection, pharyngitis, scarlet fever, rubella, whooping cough, meningococcus infection, and bronchiolitis, a surgical mask (ENT care without PAOM) or an FFP2/N95-type respiratory protection device (RPD) (ENT care with PAOM) and protective goggles should be worn. An FFP2/N95 RPD and protective goggles are also recommended for pathogens requiring “airborne” precautions (measles, Severe Acute Respiratory Syndrome SARS, Middle East respiratory syndrome-related coronavirus MERSCoV, pulmonary tuberculosis, chicken pox, tuberculoid leprosy, avian flu, etc.).
Table 1.
Classification of ENT consultation examinations and procedures with exposure to projection/aerosolization of organic material of human origin (PAOM).
| At risk of PAOM | Not at risk of PAOM |
|---|---|
| Examination and procedure in the oral cavity and the oropharynx | Otoscopy with an endoscope or microscope |
| Examination and procedure on the nasal cavities, the sinuses, and the nasopharynx with or without rigid (nasal) endoscopy | Head and Neck examination |
| Examination and procedure on the pharynx and the larynx with a laryngeal mirror, a nasal endoscope, or an epipharyngoscope | Functional exploration of hearing |
| Tracheotomy and tracheostomy treatments | Functional exploration of the vestibular apparatus |
| Sleep study |
Table 2.
ENT precautions for all patients, outside of the COVID-19 pandemic (standard precautions) and during phases 3 and 4 of the COVID-19 pandemic (standard and additional precautions) (https://www.sf2h.net/publications/actualisation-precautions-standard-2017).
| ENT care without exposure to PAOM |
ENT care with exposure to PAOM |
|||
|---|---|---|---|---|
| Standard precautions outside of the COVID-19 pandemic [1] | Standard and additional precautions during the COVID-19 pandemic | Standard precautions outside of the COVID-19 pandemic [1] | Standard and additional precautions during the COVID-19 pandemic | |
| Clean clothing | Yes | Yes | Yes | Yes |
| Single-use gloves | Yes in case of contact with a mucosa | Yes in case of contact with a mucosa | Yes | Yes |
| Eye protection | No | No | Yes | Yes |
| Mask/RPD [2] | No | Surgical | Surgical | FFP2/N95 |
| Single-use apron | No | No | Yes | Yes [3] |
| Long-sleeved disposable overgown | No | No | No | Yes [3] |
| Hair cap | No | No | No | Yes |
PAOM: projection/aerosolization of organic material of human origin; RPD: respiratory protection device (FFP2/N95). [1]. For the precautions to be taken outside the COVID-19 pandemic period, only the standard precautions are described in this table. The so-called “contact”, “droplets” and “airborne” additional precautions, necessary for some pathogens, are detailed in the text. [2] The maximum duration of wearing surgical masks is 4 h and that of RPD FFP2/N95 is theoretically 8 h even if, in practice, it is difficult to resist as many hours with an RPD because of the respiratory discomfort caused by this device. [3]. For ENT care with exposure to PAOM in the context of a COVID-19 pandemic, you can choose either to change your gown between each patient, or to keep your gown and wear it over a single-use apron that you can change between each patient.
2.7. Personal protective equipment of ENT medical teams during the COVID-19 pandemic
Insofar as an asymptomatic patient may be infectious, the same precautions must be employed whether the patient is ill with, suspected of having, or without any clinical evidence of COVID-19 infection. The professional's choice of PPE depends on the type of examination or procedure carried out during ENT consultation and its propensity to generate PAOM (https://www.inspq.qc.ca/sites/default/files/covid/2905-evaluation-risque-exposition-ts-lors-de-soins-covid19.pdf). According to the scientific data available, particularly on exposure to SARS-CoV-2 while breathing, speaking, coughing and sneezing, and despite the absence of specific studies on aerosol generation or micro-organism transmission while conducting ENT procedures, the examinations and procedures potentially at risk of transmitting infectious aerosols are listed in Table 1 (https://www.inspq.qc.ca/sites/default/files/covid/chuq-imga-covid.pdf) [2]. For ENT examinations and treatments without PAOM, the professional wears a long sleeve outfit, a surgical mask, and gloves in case of contact with a mucosa (Table 2). For ENT treatments with exposure to PAOM, their conduct requires additional precautions taking contact, droplets and airborne into account (Table 2). These additional measures deal with the type of mask to use (surgical mask or FFP2/N95 RPD), eye protection, and the standard gown (long sleeves). It is possible to extend the use of the FFP2/N95 RPD for several patient consultations when their supply is low, during which period the allocation set out by the national crisis unit changes weekly (https://www.sf2h.net/avis-du-14-mars-2020-prolongation-utilisation-des-masques; https://dgs-urgent.sante.gouv.fr/dgsurgent/inter/detailsMessageBuilder.do?id=30751&cmd=visualiserMessage). It is thus possible to do one 4-hour shift with an FFP2/N95 RPD. Disposable overgowns and hair caps will be changed between each patient and immediately in the case of soiling (through sprays of blood, saliva, aerosolization, etc.). So as not to have to change the overgown, it is possible to protect it with a single-use plastic apron, and to change the apron between two patients.
2.8. Programming of ENT consultations during the COVID-19 pandemic
During the lockdown of the population in France, ENT activities have been reduced to emergency treatments and those that could not be deferred without constituting a real loss of chance for the patient's recovery or survival. Surgical activity has been reorganised [3]. After the end of the lockdown, the provision of ENT treatment is resuming in town-based practices and hospitals with the objective of avoiding any delayed diagnosis and any loss of chance for the patient's recovery or survival (https://solidarites-sante.gouv.fr/IMG/pdf/organisation_soins-hospitaliers_covid-19.pdf). It is recommended that ENT specialists actively contact patients and parents of children with chronic pathologies whose consultations have been postponed in order to encourage them to attend an ENT consultation. This resumption of ENT diagnostic, screening, and consultation activities must be organized within the framework of a coordinated action between private structures, public hospitals, medical analysis laboratories and radiology centres, and must continue to rely in part on teleconsultation (https://solidarites-sante.gouv.fr/IMG/pdf/organisation_soins-hospitaliers_covid-19.pdf). Considering the significant risk of SARS-CoV-2 transmission during their conduct, these high-risk ENT examinations and procedures will be limited to those, which are absolutely necessary for a COVID-19 patient. They may be postponed to when the patient is no longer contagious. As far as possible, the ENT specialist will attempt to plan these high-risk procedures in advance to avoid having to carry them out in an emergency situation. Confinement entailed a risk of disorganized screening, surveillance and monitoring of ENT cancers. Regarding neonatal screening for deafness, its disorganisation is linked to very short stays in maternity hospitals, which compromises the thoroughness of retesting. The resumption of ENT activity in centres specialising in paediatric audiology must avoid any loss of chance for the patient.
Other adaptations to the scheduling of consultations are recommended. Specific time slots for COVID-19 patients and patients who are a priori free of it can be set up in order to avoid them being in the same place. Patient appointment times should be sufficiently spaced to avoid overcrowding in the waiting room.
2.9. Precautions during flexible nasal, pharyngeal or laryngeal endoscopy
Flexible ENT endoscopy is a typical example of an ENT examination at risk of exposure to PAOM. During its realization, it is advisable to avoid the presence in the room of any person whose presence is not necessary. The endoscope should be placed on a dedicated, easily cleanable table. It should be protected by a single-use protective sheath (https://www.hcsp.fr/Explore.cgi/avisrapportsdomaine?clefr=21). This sheath should be removed immediately after use and eliminated in the Infectious Medical Waste (IMW) system (https://www.hcsp.fr/Explore.cgi/avisrapportsdomaine?clefr=21). The endoscope should be disinfected as per the standard procedure as the virus is susceptible to the disinfectant products usually used: careful wiping of the nasal endoscope with a wet (or pre-soaked) single-use 14476-standard virucidal disinfectant-cleaning wipe (https://www.hcsp.fr/Explore.cgi/avisrapportsdomaine?clefr=21). The disinfection is conducted along the whole length of the scope, including the proximal sections that have not been in direct contact with the patient's nasal cavities. The use of a fiberscope camera is advised to allow for distancing between the patient and the ENT physician. After the endoscopy, the surfaces located near where the endoscopy was carried out (tables, floor, etc.) must be cleaned with a virucidal disinfectant detergent EN 14476 to remove any contaminating projections. If a sheath was not used, the disinfection of the device must comply with the best practice rules laying down the standard procedures for treating thermosensitive endoscopes without an operating channel using bactericidal and virucidal products (https://www.hcsp.fr/Explore.cgi/avisrapportsdomaine?clefr=21). After the examination, the professional must carefully disrobe in compliance with hygiene rules, with the immediate elimination of gloves, mask, hair cap, and overgown in the IMW system for treatments in healthcare facilities, or as per the system for non-infected medical waste for doctors’ offices (domestic waste stream, double-bagged with 24 hours’ storage before elimination) (https://solidarites-sante.gouv.fr/IMG/pdf/guide-covid-19-phase-epidemique-v15-16032020.pdf). The room where the examination is carried out must undergo air renewal as per the legislation. The room should have additional aeration or a rest period depending on the flow of ventilation.
2.10. ENT teleconsultation and COVID-19
Meeting a general objective for better access to treatment, the current context of managing COVID-19 highlights the benefit of remote consulting. ENT teleconsultation allows physicians to continue taking care of patients who cannot travel and makes it possible to ensure continuity of care while limiting the preventable risks of spreading the coronavirus within ENT private practices and healthcare facilities (https://solidarites-sante.gouv.fr/IMG/pdf/covid-19_teleconsultation-fiche-medecin.pdf; https://solidarites-sante.gouv.fr/soins-et-maladies/maladies/maladies-infectieuses/coronavirus/professionnels-de-sante/article/teleconsultation-et-covid-19-qui-peut-pratiquer-a-distance-et-comment). It also allows the ENT specialist to select patients who can be counselled or treated without the need for a face-to-face consultation (leaving the possibility of a follow-up telephone callback) and those who must be received at the doctor's office. This teleconsultation may include an interview, an inspection of the head and neck region, a self-palpation of the patient, the commented reading of results of biological tests or radiological reports, and the renewal or adaptation of treatments already prescribed. This remote consulting arrangement was made available to all patients and all ENT specialists with 100% coverage by the French social security system. Communication without video is accepted for the following patients: those aged 70 or over, those being monitored for a long-term health condition, those living in areas with no signal, and those ill with or suspected of having COVID-19. This new organisation in the field of healthcare is not adapted to all situations. Wherever the ENT specialist deems it necessary, they may interrupt the teleconsultation and suggest a physical consultation.
Technical solutions are now being developed for remote hearing tests for adult patients, and more cautiously for older children where audiometry without conditioning is possible [4]. Medical tele-audiology can be seen as a three-level scale. The first level involves self-screening tests (tone audiometry or vocal audiometry test in noise), the result of which may or may not lead to advising consultation with a physician. It is important that the self-administered test be carried out in a quiet environment. The second level involves the caregiver managing the patient in their everyday life. Finally, the third level allows the ENT specialist to interact directly with the patient to carry out tone audiometry with masking of the non-test ear, vocal audiometry using lists of words, phonemes, or validated pseudo-words in French, or even vocal audiometry in noise. The tele-audiometry data must be stored on a server labelled HDS (Healthcare Data Hosting).
3. Conclusions
Most of these best practice recommendations do not rely on scientific data specifically established for the COVID-19 infection, but on the extrapolation of what is known about other viral respiratory infections as well as on precautionary principles. They will probably be modified in the future according to the evolution of the epidemic, the development of new protective equipment or diagnostic tools and new knowledge on SARS-CoV-2 virus contamination routes. In addition, compliance with these recommendations raises the double challenge of slowing down the flow of consultations, which should not incur loss-of-chance for patients who require prompt treatment, and the additional costs brought about for the ENT practitioner as well as for society as a whole.
Disclosure of interest
The authors declare that they have no competing interest.
References
- 1.Givi B., Schiff B.A., Chinn S.B. Safety Recommendations for Evaluation and Surgery of the Head and Neck During the COVID-19 Pandemic. JAMA Otolaryngol Head Neck Surg. 2020 doi: 10.1001/jamaoto.2020.0780. [DOI] [PubMed] [Google Scholar]
- 2.Meselson M. Droplets and Aerosols in the Transmission of SARS-CoV-2. N Engl J Med. 2020 doi: 10.1056/NEJMc2009324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Couloigner V., Schmerber S., Nicollas R. COVID-19 and ENT Surgery. Eur Ann Otorhinolaryngol Head Neck Dis. 2020 doi: 10.1016/j.anorl.2020.04.012. [pii: S1879-7296(20)30102-2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thai-Van H., Bakhos D., Bouccara D. Medical teleconsultation in Audiology. Best practice recommendations from the French Audiology Society (SFA) and the French ENT Society (SFORL) Eur Ann Otorhinolaryngol Head Neck Dis. 2020 doi: 10.1016/j.anorl.2020.10.007. [In press] [DOI] [PMC free article] [PubMed] [Google Scholar]