Abstract
Background: Fractures of the hook of the hamate are rare. Nonoperative management has historically been immobilization in a short arm cast (SAC) without thumb immobilization with a high reported incidence of nonunion. The high prevalence of nonunion following nonoperative treatment may be secondary to motion at the fracture site. The transverse carpal ligament’s attachment to the hook of the hamate results in movement at the fracture site during thumb motion. Methods: A cadaveric study using 8 fresh frozen cadaver arms amputated at the mid-humeral level was performed. Computed tomography (CT) imaging was used to assess the bony anatomy and assure no preexisting fractures were present. Osteotomy of the hook of the hamate was performed through a skin incision proximal to the hook of the hamate and the transverse carpal ligament. Each arm was then mounted in a jig designed to hold and stabilize the arm and hand in supination. CT scans were performed without cast immobilization with the thumb in extension and abduction, with SAC without thumb carpometacarpal joint immobilization, and SAC with thumb carpometacarpal joint immobilization. Results: Motion of the fractured hook of the hamate was found to occur in all noncasted specimens, greatest with base fractures. SAC without thumb immobilization had little to no effect in eliminating fracture motion. SAC including the thumb reduced fracture motion in all specimens. Conclusions: Previous poor experience with nonoperative management of fractures of the hook of the hamate may be partially due to inability to adequately immobilize the fracture fragment. Fracture motion of the hamate hook occurs during thumb movement, likely from traction on the fracture fragment by the transverse carpal ligament.
Keywords: hamate fracture, hook of hamate, thumb immobilization, thumb spica cast, transverse carpal ligament
Introduction
Fracture of the hook of the hamate is an infrequent injury and is estimated to account for approximately 2% of all carpal fractures.4,42 Several mechanisms of injury may result in a hamate hook fracture. Such reported mechanisms include a direct force such as a fall on the palm of the hand, a crushing injury, shearing force of the extrinsic flexor tendons of the ring and small fingers as they move ulnarly, and sports-related microtrauma from forceful gripping of a racquet, bat, or golf club.8,9,33,37,41,44 With the increasing popularity of sports activities such as golf and tennis, the incidence of these fractures is increasing.3,9,15,16,24,27,37,38,41,45 Stark et al37,38 have described this injury in golfers, baseball players, and tennis players resulting from force transmitted through a racquet, club, or bat to the hand, fracturing the hook of the hamate. More recently, there have been reported incidences in underwater rugby players,34 professional football players,30 as well as basketball and hockey players.17
Although various treatment modalities, both operative and nonoperative, are available, the optimal treatment for this fracture remains unclear.6 Due to the difficulty in diagnosis of these fractures and the subsequent delay in its recognition, treatment selection is often challenging.3,10,22,28,33,37 The recommended initial treatment of acute fractures has historically been immobilization in a short arm cast (not including the thumb). Although there have been reports of successful bony union, the reported nonunion rate is high and often anticipated.3,4,6-8,11,14,27,33,36,41,46 Because of the rarity of this fracture, a true consensus for the most appropriate form of immobilization and treatment has not been reached. The nonunion rate after acute fracture has been high regardless of treatment, and some authors now recommend immediate excision of the fracture fragment to relieve pain and prevent late flexor tendon rupture.19,24,37 For chronic or previously untreated fractures, excision of the fracture fragment and bone grafting with or without internal fixation has been recommended.3,5,14,22,28,36,37,44 However, biomechanical studies have demonstrated decrease in flexor tendon forces following excision of the hamate hook, signifying a decrease in power grip.9 Conflictingly, excision of the hamate hook in athletes has demonstrated successful return to preinjury performance levels of activity and resolution of symptoms.2,3,8,10,15,27,36,38
The high prevalence of nonunion of the hamate hook following nonoperative treatment may be secondary to motion at the fracture site. The hamate hook has several musculo-ligamentous attachments. It serves as the origin of the hypothenar muscles, is influenced by the flexor carpi ulnaris via the pisohamate ligament, and is one of the attachment sites of the transverse carpal ligament. The transverse carpal ligament is also attached to the trapezium and the scaphoid tuberosity. Therefore, movement of the thumb may promote motion at the fracture site and prevent osseous union. To our knowledge, no previously published study has reported the effect of thumb immobilization on acute fractures of the hook of the hamate. The purpose of this study is to determine the importance of thumb immobilization in preventing motion at the fracture site in an acute fracture of the hook of the hamate.
Materials and Methods
Eight fresh frozen cadaver arms amputated at the level of the mid-humerus were used. All arms were thoroughly thawed prior to use and inspected for any anatomic abnormalities or evidence of previous trauma or surgery. All hands had x-ray and computed tomography (CT) imaging to assess the bony anatomy and assure that no preexisting fracture of the hook of the hamate was present.
Osteotomy of the hook of the hamate was performed using a ¼-inch osteotome inserted through a 1-cm skin incision proximal to both the hook of the hamate and the transverse carpal ligament. The edge of the osteotome was abutted deeply against the palpable hook of the hamate, deep to the attachments of the pisohamate ligament and the flexor digiti minimi brevis and opponens digiti minimi muscles. None of the stabilizing soft tissue attachments were detached from the hook of the hamate during the procedure. A fracture of the hook was completed without damage to the soft tissues structures attaching to the hamate, and the skin and subcutaneous tissues were then sutured closed.
Each arm was then mounted in a jig specially designed for this study to hold and stabilize the arm and hand. The arm was held supinated, and immobilized to prevent hand and forearm motion and then inserted into the CT scanner. CT scan confirmed the fracture level and initial displacement. CT scans using 2-mm cuts of the hook of the hamate were then performed. The first was a scout study with the hand in a relaxed position to confirm the fracture position and to be sure that a complete fracture had been made.
An elastic band was then wrapped securely around the distal phalanx of the thumb passively holding the thumb in the desired position (Figure 1). The second CT scan was performed without cast immobilization. During this CT scan, the thumb was held in maximal extension and abduction. Changes in fracture alignment and the maximal motion of the fracture fragment were then determined.
Figure 1.

An elastic band is wrapped securely around the distal phalanx of the thumb passively holding the thumb in the desired position.
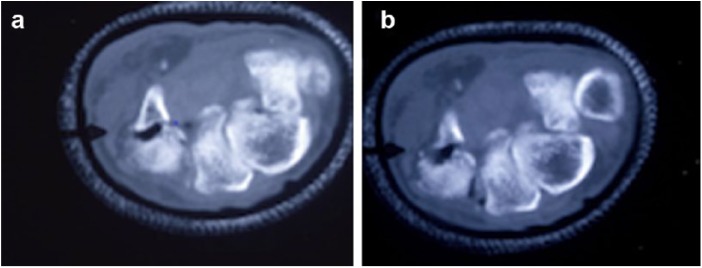
The third phase scans were done with the hand and forearm immobilized in a short arm plaster cast leaving the carpometacarpal (CMC), metacarpophalangeal, and interphalangeal joints of the thumb free (Figure 2). The thumb was then again placed into maximal abduction and extension and CT scans were repeated to determine the fracture motion and displacement (Figure 3).
Figure 2.

The third phase scans were done with the hand and forearm immobilized in a short arm plaster cast leaving the carpometacarpal, metacarpophalangeal, and interphalangeal joints of the thumb free.
Figure 3.
(a) Computed tomography scan immediately after osteotomy. (b) Thumb extension in short arm cast with thumb free allows displacement of the fracture fragment.
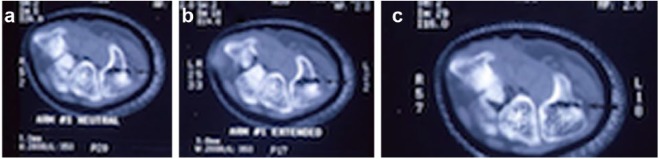
During that last phase scans, the hand and wrist were placed into a short arm plaster cast, which held the CMC joint of the thumb immobilized, while leaving the metacarpophalangeal and interphalangeal joints free. This last phase of the study was done only on one-half of the specimens (Figure 4).
Figure 4.
Computed tomography scan (a) with thumb in neutral and (b) with thumb extended and abducted shows motion of the fracture fragment. (c) Carpometacarpal joint immobilization with the thumb pulled into abduction and extension.
Statistical Methods
Calculations of fracture displacement were made using the measurement cursor on either a Picker INTL 1200 CT scanner or a GE Hi-speed Advantage CT scanner and measured to the nearest tenth of a millimeter. The greatest amount of displacement was then recorded.
Results
Fracture position was classified as previously described by Stark et al.37 There was one fracture of the volar 1/3 of the hook, 3 fractures of the middle 1/3, and 4 fractures that occurred at the base. The variety of fracture levels is attributed to the difficulty encountered in trying to consistently fracture the hook at the same level.
Motion of the fractured hook of the hamate was found to occur in all noncasted specimens. The greatest motion of the fracture fragment occurred in specimens E, F, G, and H, all of which were base fractures (Table 1). The short arm cast (with the thumb left free) provided only minimal restriction of motion in one specimen (H), but had no effect in eliminating fracture motion in the remainder of the specimens.
Table 1.
Hook of Hamate Fracture Motion Versus Immobilization.
| Specimen | Osteotomy level | Initial displacement (mm) | Fracture motion (mm) | ||
|---|---|---|---|---|---|
| No cast thumb in extension/abduction | Short arm cast thumb in extension/abduction | Short arm cast carpometacarpal immobilized pulled into extension/abduction | |||
| A | Volar 1/3 | 0.0 | 1.7 | 1.7 | 0.0 |
| B | Middle 1/3 | 0.5 | 1.5 | 1.5 | NT |
| C | Middle 1/3 | 0.0 | 1.5 | 1.5 | NT |
| D | Middle 1/3 | 0.0 | 1.7 | 1.8 | 0.0 |
| E | Base | 0.5 | 2.0 | 2.0 | NT |
| F | Base | 0.5 | 3.7 | 3.7 | 1.8 |
| G | Base | 0.0 | 2.5 | 2.5 | NT |
| H | Base | 0.0 | 2.3 | 1.9 | 1.0 |
Note. NT = not tested.
Although immobilization of the thumb CMC joint eliminated almost all of the motion in the specimens tested with fractures distal to the base, there was still some measureable motion in those specimens tested with fracture at the base of the hook. All specimens, however, did demonstrate a significant reduction in motion when treated with thumb immobilization.
Discussion
Results of this cadaveric study demonstrate that nonoperative management of acute fractures of the hook of the hamate treated with thumb spica immobilization minimized or eliminated motion at the fracture site. This is likely due to limiting the effect of traction on the hamate hook fragment caused by the attachment of the transverse carpal ligament to the trapezium and base of the thumb. It can easily be seen from the results (Table 1) that a short arm cast alone, without thumb immobilization, did not provide adequate fracture stabilization.
The anatomy of the hook of the hamate and its attachments has been well described.7,18,22,37,38,43 The hook is palpable as a bony prominence of the palmar surface of the hand at the intersection of a line along the ulnar border if the ring finger and a line drawn from the proximal aspect of the first web space (Kaplan’s cardinal line). It may also be located along a line projected from the pisiform to the center of the head of the index metacarpal, 1.5 to 3.0 cm distal to the pisiform.7 The hook is a long, thin osseous prominence with average dimensions of 1.3 by 1.0 by 0.5 cm.37 In addition, Panagis et al25 have shown that the entire hamate bone including the hook enjoys a rich blood supply; however, nonunion due to avascular necrosis has been reported.13 In a study of the blood supply to the hook, it was found that fractures through the base could potentially result in compromised vascularity of the hook.12
There are several soft tissue attachments to the hook of the hamate.18 The ulnar aspect of the transverse carpal ligament, the pisohamate ligament, and the muscular origins of the flexor digiti minimi brevis and opponens digiti minimi are all soft tissue attachments to the hook of the hamate. The extrinsic flexor tendons of the ring and small fingers abut the hook as they travel through the carpal canal.9,10,43 The hook of the hamate has been previously demonstrated as an important component of the ulnar carpal canal.43 In a cadaveric study of upper limb specimens, Wang et al43 reported that a fracture of the hook of the hamate may jeopardize the integrity of the deep branch of the ulnar nerve, the ring, and small flexor tendons. In addition, in a biomechanical study to determine flexor tendon function following a hook of the hamate excision, Demirkan et al9 demonstrated a flexor tendon force decrease of 11% to 15%, suggestive of a reduction in power grip.
Nonoperative management for fractures of the hook of the hamate has ranged from using no immobilization,7 a splint only,44 to casts that immobilize various joints of the hand including the small and ring metacarpophalangeal,11,46 and proximal interphalangeal joints.41 Documentation of union by splint or cast immobilization has been sparse.3,6,11,23,31,38,46 Failure to achieve union even in acute fractures treated for up to 6 weeks by immobilization is well described.11,28,37,38,44
Because of the poor results with nonoperative treatment, many authors now recommend immediate operative treatment with excision or bone grafting (with or without internal fixation) for treatment of the acute fracture to allow for earlier return to sports and prevent further complications.6,8,10,15,37,38,44 To date, Stark et al37 have published the largest single series of fractures of the hook of the hamate and reviewed the outcomes in 62 patients. Fractures were classified based on 3 anatomical locations with the hook divided into thirds: proximal (base), middle, and volar. There were 7 volar, 8 middle, and 47 proximal or base fractures in their series. Three of 10 acute fractures were treated in a short arm cast for 6 weeks, but failed to heal and subsequently underwent excision of the fracture fragment. The remaining 7 acute fractures underwent immediate excision of the fragment. Forty-nine of the remaining 52 fractures were diagnosed more than 2 weeks after the injury and were treated by excision of the fracture fragment. Fifty-seven of 59 patients resumed their usual activities and regained normal grip strength by 6 months. Carter et al7 reported 6 base fractures in the 9 patients in his series; all were treated by excision and returned to the preinjury status. More recently, various treatment modalities have been utilized for hamate hook fractures; these include low-intensity pulsed ultrasound,32,40 use of a breakaway screw,21 hook plate,39 or dorsal percutaneous cannulated mini-screw fixation,35 all with variable success.
The poor results after nonoperative treatment are likely due to both the natural history of this fracture and a lack of understanding of the physiology and biomechanics involved. One of the main difficulties remains delay in diagnosis. Often diagnosis is delayed until nonunion is already present. A high index of suspicion should lead to the use one of the many special radiographic views as well as CT scans to aid to early diagnosis.3,7,20,23,26,28,29,37,38,42
It remains unclear why it is so difficult to establish bony union in the hook of the hamate fracture by immobilization in a cast or splint. Most acute fractures treated nonoperatively have been immobilized for 6 weeks.6 It may be that the hook of the hamate, like the scaphoid, requires a longer period of immobilization to achieve union. Whalen et al46 have reported union after an average of 8 weeks in 6 acute fractures treated in a short arm cast with immobilization of the metacarpophalangeal joints of the ring and small fingers.
Several authors have suggested that motion of the fracture fragment due to inadequate immobilization may be responsible for nonunion.4,28,37,44 Assuming that a major cause of nonunion is fracture motion, it is important to identify sources of this motion. There are several musculo-ligamentous structures attached to the hook that may be responsible for this motion.14,44 Watson and Rogers44 have shown that importance of the hook as a pulley for the flexor profundus tendons during grip. This pulley effect combined with the attachments of the flexor digiti minimi brevis and opponens digiti minimi may be another cause of fracture motion and displacement during finger motion. He recommends bone grafting the fracture rather than excision because of the importance of the hook in maintaining grip strength. In addition, the hypothenar muscles originate on the hook and may move the hook during motion of the small finger. The flexor carpi ulnaris may also pull on the fracture fragment through attachments to the pisiform and pisohamate ligament. The transverse carpal ligament is another important structure attaching to the hook of the hamate that may contribute to motion of the fracture fragment. Foucher et al14 and Andress and Peckar1 have suggested that avulsion fractures may occur through the attachment to the transverse carpal ligament or from forced contraction of the flexor carpi ulnaris. Bony attachments of the transverse carpal ligament include the trapezium, and the scaphoid tuberosity, the hook of the hamate, as well as the pisiform. Movement of the thumb would therefore be expected to pull on the fracture fragment resulting in fracture motion and nonunion. Results of this study support this theory. Fractures of the base of the hook of the hamate were the most difficult to immobilize and were found to have the greatest amount of motion at the fracture site. One explanation for this observation may be that the soft tissue attachments on the ulnar side may have a strong enough attachment to the volar 1/3 of the fracture fragment so that motion is restricted. This lack of greater motion supports the “mast of a ship” concept where the soft tissue attachments act by stabilizing the hook at the top but not at the bottom.37
There are several limitations of this study. First, the small sample size of the specimens used may not adequately represent the general population. Anatomical variations and ligamentous integrity of the specimens used may influence fracture motion. In addition, fracture levels varied in this study. Although this allowed for a broader spectrum of fracture possibilities, it reduced the reproducibility of outcomes following nonoperative treatment modalities. In addition, not all specimens were tested with thumb immobilization. Cadaveric arms were not obtained all at once, and initially thumb immobilization was not evaluated. Evaluation of thumb immobilization in all specimens would further strengthen the findings of this study. Last, this study was designed to investigate thumb immobilization and its influence of fracture motion of the hook of the hamate. Several factors that may influence motion of the fracture site were not investigated.
In conclusion, previous poor experience with nonoperative management of fractures of the hook of the hamate may be in part due to inadequate immobilization of the fracture fragment. Surrounding soft tissues may exert sufficient force to cause motion and prevent union. We have found that motion of the hamate hook fracture occurs during thumb movement. Anatomically, it appears this is due to traction on the fracture fragment caused by the attachment of the transverse carpal ligament pulling on the hook during thumb motion. While we have only investigated the effect of one structure attaching to the hook of the hamate, results of this study suggest that to adequately treat acute fractures of the hook of the hamate nonoperatively, complete thumb immobilization in a thumb spica cast is necessary. This will prevent the motion at the fracture site, which occurs during thumb motion, particularly abduction and extension.
Footnotes
Ethical Approval: This was a cadaveric study. No institutional review board approval was needed.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: This study involves no human participants, so informed consent was not sought or required.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Andress MR, Peckar VG. Fracture of the hook of the hamate. Br J Radiol. 1970;43(506):141-143. [DOI] [PubMed] [Google Scholar]
- 2. Arons JA, Smith AA. “High five” hamate fracture. J Hand Surg Am. 1994;19(5):884. [DOI] [PubMed] [Google Scholar]
- 3. Bishop AT, Beckenbaugh RD. Fracture of the hamate hook. J Hand Surg Am. 1988;13(1):135-139. [DOI] [PubMed] [Google Scholar]
- 4. Boulas HJ, Milek MA. Hook of the hamate fractures. Diagnosis, treatment, and complications. Orthop Rev. 1990;19(6):518-529. [PubMed] [Google Scholar]
- 5. Bryan RS, Dobyns JH. Fractures of the carpal bones other than lunate and navicular. Clin Orthop Relat Res. 1980(149):107-111. [PubMed] [Google Scholar]
- 6. Carroll RE, Lakin JF. Fracture of the hook of the hamate: acute treatment. J Trauma. 1993;34(6):803-805. [DOI] [PubMed] [Google Scholar]
- 7. Carter PR, Eaton RG, Littler JW. Ununited fracture of the hook of the hamate. J Bone Joint Surg Am. 1977;59(5):583-588. [PubMed] [Google Scholar]
- 8. David TS, Zemel NP, Mathews PV. Symptomatic, partial union of the hook of the hamate fracture in athletes. Am J Sports Med. 2003;31(1):106-111. [DOI] [PubMed] [Google Scholar]
- 9. Demirkan F, Calandruccio JH, Diangelo D. Biomechanical evaluation of flexor tendon function after hamate hook excision. J Hand Surg Am. 2003;28(1):138-143. [DOI] [PubMed] [Google Scholar]
- 10. Devers BN, Douglas KC, Naik RD, et al. Outcomes of hook of hamate fracture excision in high-level amateur athletes. J Hand Surg Am. 2013;38(1):72-76. [DOI] [PubMed] [Google Scholar]
- 11. Egawa M, Asai T. Fracture of the hook of the hamate: report of six cases and the suitability of computerized tomography. J Hand Surg Am. 1983;8(4):393-398. [DOI] [PubMed] [Google Scholar]
- 12. Failla JM. Hook of hamate vascularity: vulnerability to osteonecrosis and nonunion. J Hand Surg Am. 1993;18(6):1075-1079. [DOI] [PubMed] [Google Scholar]
- 13. Failla JM. Osteonecrosis associated with nonunion of the hook of the hamate. Orthopedics. 1993;16(2):217-218. [DOI] [PubMed] [Google Scholar]
- 14. Foucher G, Schuind F, Merle M, et al. Fractures of the hook of the hamate. J Hand Surg Br. 1985;10(2):205-210. [DOI] [PubMed] [Google Scholar]
- 15. Futami T, Aoki H, Tsukamoto Y. Fractures of the hook of the hamate in athletes. 8 cases followed for 6 years. Acta Orthop Scand. 1993;64(4):469-471. [DOI] [PubMed] [Google Scholar]
- 16. Guha AR, Marynissen H. Stress fracture of the hook of the hamate. Br J Sports Med. 2002;36(3):224-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Husband JB. Hook of hamate and pisiform fractures in basketball and hockey players. Hand Clin. 2012;28(3):303. [DOI] [PubMed] [Google Scholar]
- 18. Kaplan E, Spinner M. Kaplan’s functional and surgical anatomy of the hand. Philadelphia: Lippincott; 1984. [Google Scholar]
- 19. Milek MA, Boulas HJ. Flexor tendon ruptures secondary to hamate hook fractures. J Hand Surg Am. 1990;15(5):740-744. [DOI] [PubMed] [Google Scholar]
- 20. Murray WT, Meuller PR, Rosenthal DI, et al. Fracture of the hook of the hamate. AJR Am J Roentgenol. 1979;133(5):899-903. [DOI] [PubMed] [Google Scholar]
- 21. Naito K, Yoshikawa K, Kaneko K, et al. Hamate hook non-union treated with a break-away screw: a case report. Hand Surg. 2013;18(3):417-420. [DOI] [PubMed] [Google Scholar]
- 22. Nisenfield FG, Neviaser RJ. Fracture of the hook of the hamate: a diagnosis easily missed. J Trauma Inj Infect Crit Care. 1974;14(7):612-616. [DOI] [PubMed] [Google Scholar]
- 23. Norman A, Nelson J, Green S. Fractures of the hook of hamate: radiographic signs. Radiology. 1985;154(1):49-53. [DOI] [PubMed] [Google Scholar]
- 24. O’Shea K, Weiland AJ. Fractures of the hamate and pisiform bones. Hand Clin. 2012;28(3):287-300. [DOI] [PubMed] [Google Scholar]
- 25. Panagis JS, Gelberman RH, Taleisnik J, et al. The arterial anatomy of the human carpus. Part II: the intraosseous vascularity. J Hand Surg Am. 1983;8(4):375-382. [DOI] [PubMed] [Google Scholar]
- 26. Papilion JD, DuPuy TE, Aulicino PL, et al. Radiographic evaluation of the hook of the hamate: a new technique. J Hand Surg Am. 1988;13(3):437-439. [DOI] [PubMed] [Google Scholar]
- 27. Parker RD, Berkowitz MS, Brahms MA, et al. Hook of the hamate fractures in athletes. Am J Sports Med. 1986;14(6):517-523. [DOI] [PubMed] [Google Scholar]
- 28. Polivy KD, Millender LH, Newberg A, et al. Fractures of the hook of the hamate—a failure of clinical diagnosis. J Hand Surg Am. 1985;10(1):101-104. [DOI] [PubMed] [Google Scholar]
- 29. Posner MA, Greenspan A. Trispiral tomography for the evaluation of wrist problems. J Hand Surg Am. 1988;13(2):175-181. [DOI] [PubMed] [Google Scholar]
- 30. Rettig AC. Hamate and pisiform fractures in the professional football player. Hand Clin. 2012;28(3):305. [DOI] [PubMed] [Google Scholar]
- 31. Roach JJ. Compound incomplete dislocation of the trapezium and compound fractured hamate hook. J Natl Med Assoc. 1978;70(11):841-842. [PMC free article] [PubMed] [Google Scholar]
- 32. Sakuma Y, Iwamoto T, Momohara S. Ununited fracture of the hook of hamate treated with low-intensity pulsed ultrasound in an older middle-aged patient. Clin J Sport Med. 2014;24(4):358-359. [DOI] [PubMed] [Google Scholar]
- 33. Scheufler O, Andresen R, Radmer S, et al. Hook of hamate fractures: critical evaluation of different therapeutic procedures. Plast Reconstr Surg. 2005;115(2):488-497. [DOI] [PubMed] [Google Scholar]
- 34. Scheufler O, Kamusella P, Tadda L, et al. High incidence of hamate hook fractures in underwater rugby players: diagnostic and therapeutic implications. Hand Surg. 2013;18(3):357-363. [DOI] [PubMed] [Google Scholar]
- 35. Scheufler O, Radmer S, Andresen R. Dorsal percutaneous cannulated mini-screw fixation for fractures of the hamate hook. Hand Surg. 2012;17(2):287-293. [DOI] [PubMed] [Google Scholar]
- 36. Smith P, III, Wright TW, Wallace PF, et al. Excision of the hook of the hamate: a retrospective survey and review of the literature. J Hand Surg Am. 1988;13(4):612-615. [DOI] [PubMed] [Google Scholar]
- 37. Stark HH, Chao EK, Zemel NP, et al. Fracture of the hook of the hamate. J Bone Joint Surg Am. 1989;71(8):1202-1207. [PubMed] [Google Scholar]
- 38. Stark HH, Jobe FW, Boyes JH, et al. Fracture of the hook of the hamate in athletes. J Bone Joint Surg Am. 1977;59(5):575-582. [PubMed] [Google Scholar]
- 39. Taleb C, Murachowsky J, Ruggiero GM. Hamate hook nonunion treated with a hook plate: case report and surgical technique. Tech Hand Up Extrem Surg. 2012;16(4):194-197. [DOI] [PubMed] [Google Scholar]
- 40. Tomaru M, Osada D, Fujita S, et al. Treatment of hook of the hamate fractures in adults using low-intensity pulsed ultrasound. Hand Surg. 2014;19:433-436. [DOI] [PubMed] [Google Scholar]
- 41. Torisu T. Fracture of the hook of the hamate by a golfswing. Clin Orthop Relat Res. 1972;83:91-94. [DOI] [PubMed] [Google Scholar]
- 42. Walsh JJ, Bishop AT. Diagnosis and management of hamate hook fractures. Hand Clin. 2000;16(3):397-403. [PubMed] [Google Scholar]
- 43. Wang B, Hu J, Zhang X, et al. [Anatomic study on hook of hamate bone]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2010;24(1):60-63. [PubMed] [Google Scholar]
- 44. Watson HK, Rogers WD. Nonunion of the hook of the hamate: an argument for bone grafting the nonunion. J Hand Surg Am. 1989;14(3):486-490. [DOI] [PubMed] [Google Scholar]
- 45. Weiland AJ. Treatment of fracture of hook of the hamate in baseball players. Hand Clin. 2012;28(3):301. [DOI] [PubMed] [Google Scholar]
- 46. Whalen JL, Bishop AT, Linscheid RL. Nonoperative treatment of acute hamate hook fractures. J Hand Surg Am. 1992;17(3):507-511. [DOI] [PubMed] [Google Scholar]