Abstract
Lung cancer is one of the leading causes of death worldwide. Therefore, understanding the factors linked to patient survival is essential. Recently, multi-omics analysis has emerged, allowing for patient groups to be classified according to prognosis and at a more individual level, to support the use of precision medicine. Here, we combined RNA expression and miRNA expression with clinical information, to conduct a multi-omics analysis, using publicly available datasets (the cancer genome atlas (TCGA) focusing on lung adenocarcinoma (LUAD)). We were able to successfully subclass patients according to survival. The classifiers we developed, using inferred labels obtained from patient subtypes showed that a support vector machine (SVM), gave the best classification results, with an accuracy of 0.82 with the test dataset. Using these subtypes, we ranked genes based on RNA expression levels. The top 25 genes were investigated, to elucidate the mechanisms that underlie patient prognosis. Bioinformatics analyses showed that the expression levels of six out of 25 genes (ERO1B, DPY19L1, NCAM1, RET, MARCH1, and SLC7A8) were associated with LUAD patient survival (p < 0.05), and pathway analyses indicated that major cancer signaling was altered in the subtypes.
Keywords: multi-omics analysis, lung cancer, survival-associated genes
1. Introduction
Lung cancer is one of the leading causes of death worldwide, mostly due to a late diagnosis. In fact, an estimated nearly 136,000 patients are expected to die from lung cancer in 2020 in the United States [1]. Even though it only contains 9% of the world’s population, Europe accounts for 25% of the global cancer burden, with an estimated 3.9 million new cancer cases and 1.9 million expected cancer deaths in 2018 [2]. Within these cases, the most common cause of cancer death was lung cancer, and 280,000 are expected to die from lung cancer in 2019 [3]. In Asia, and especially in Japan, the number of new cases of lung cancer in 2018 was 118,971 (13.5%), which is the worst number of cases among all cancers. The same was true for the risk of death; 81,820 (20.0%), as indicated by the statistics summarized by the World Health Organization (WHO) [4].
Lung cancer can be classified into two major types: small-cell lung cancer (SCLC), which accounts for approximately 15% of cases and non-small-cell lung cancer (NSCLC), which accounts for approximately 85%. Therefore, NSCLC involves the majority of the lung cancer population, and adenocarcinoma is the most common type of NSCLC. Multiple mutations have been reported to occur in NSCLC, but needless to say, the spectrum of mutations is different between different subtypes [5,6]. Thus, knowing the clinical, pathological, and molecular biological outcomes in diverse aspects is quite important to achieve an improvement in the quality of life of cancer patients.
Recently, in the medical field, deep-learning-driven classification of cancer showed a great success [7]. After that, many images-based machine-learning and deep-learning studies demonstrated their use for cancer prediction, prognosis, or even to assess treatment response in lung cancer [8,9,10]. However, single-level omics data have limitations, particularly because cancer is a heterogeneous disease, so relying on results obtained from single-level omics data may be risky and misleading; thus, it could affect the understanding of cancer as a whole and possibly negatively affect patients.
One of the proposed approaches to overcome this problem is a multi-omics analysis, an approach that has rapidly emerged in disease-related biology. A new cancer subtyping method, with the integration of multi-omics data, has already been used to reveal molecular subtypes of cancer with TCGA dataset. Multi-omics analysis, using integrated TCGA data of RNA expression, DNA methylation, point mutations, and copy number variation, demonstrated a prediction capability for poor patient outcomes [11]. Multi-omics analysis with a TCGA hepatocellular carcinoma (LIHC) dataset was also performed, using a deep-learning-based and machine-learning-based pipeline to predict patient survival, using RNA expression, DNA methylation, and miRNA expression [12]. The authors implemented an autoencoder to reduce the dimension of multi-omics features as an unsupervised approach, and then, the reduced features were further analyzed via the Cox proportional hazards (Cox-PH) model, to select survival-associated features. A similar approach was applied by using gene expression and copy number variants to classify poor or good subtypes in neuroblastoma [13].
Here, to develop a classifier for the prediction of lung-cancer-patient prognosis and to investigate a patient risk-dependent analysis, we applied a deep-learning- and machine-learning-based pipeline for multi-omics analysis of lung cancer data. We chose data of RNA expression and miRNA expression as input data, so that the result we received could be interpretable, since RNA expression is regulated by miRNA by functional duplexes. Firstly, we developed an SVM that was able to distinguish prognosis-related subtypes from the TCGA LUAD. Secondly, we performed a risk-dependent pathway analysis that can give us relevant information and knowledge about potential mechanisms related to the different subtypes. Lastly, using differentially expressing RNAs in the subtypes, we found novel genes that are associated with patient survival, and we demonstrated that newly identified genes were associated with prognosis.
2. Materials and Methods
2.1. TCGA Set
We downloaded multi-omics LUAD data from the Genomic Data Commons (GDC) TCGA data portal (https://portal.gdc.cancer.gov), using TCGA Assembler 2 (https://github.com/compgenome365/TCGA-Assembler-2; [14] with R package (R version 3.5.1). A total of 384 patients with RNA sequencing data (RNA-seq; normalized data) and miRNA sequencing data (miRNA-seq; defined using human reference genome 19 and miRBase version 20 (http://www.mirbase.org/)) were assembled into one multi-omics dataset, in the last step of the procedure. Patients’ clinical data were manually downloaded from the GDC data portal, and a total of 364 patients were available for the next analysis step. Data were preprocessed by following previous reports to deal with zero values [12]. In the last step, zero values were removed and RNA-seq data, and miRNA-seq data were standardized against patients, followed by reassembling, to make a multi-omics dataset before being fed into an autoencoder.
2.2. Clustering to Obtain Inferred Labels from LUAD Multi-Omics Dataset
We basically followed a pipeline and the previously published autoencoder hyper parameter settings [11]. As previously described, we implemented the autoencoder with three hidden layers (500, 100, and 500 nodes) with Keras (https://keras.io; version 2.2.4). For the hyper parameter settings, L1 and L2 regulation weights were set at 0.001 and 0.0001, respectively. Learning rate was set at 0.01, with a decay of 1e-6, and epochs were set at 150, with a dropout rate of 0.5. Stochastic gradient decent (SGD) was used as an optimizer. A bottleneck feature space of dimension 100 for each patient was extracted for further analysis.
To obtain clinically associated features from the bottleneck feature space of dimension 100, we built a univariate Cox-PH model, using a survival package in R. A log-rank p-value of less than 0.05 was considered as significant to select the clinical associated features.
To cluster the survival-associated features and to obtain the inferred labels, we first performed the elbow method [15], to determine the optimal clustering number in a range from one to ten. Based on the result depicted by the elbow method, we performed further analysis, to obtain the optimal number of clusters, using the Silhouette index [16] and Calinski–Harabasz criterion [17]. In the last step, based on the above results, we performed a K-means clustering, using the K, and previously determined and visualized the result with a t-Distributed Stochastic Neighbor Embedding (t-SNE) [18]. We used the scikit-learn library to perform the aforementioned clustering, and the obtained inferred labels were used to draw a Kaplan–Meier plot and then develop the classifiers described in Section 2.3 and Section 2.4.
2.3. Kaplan–Meier Analysis
Inferred labels obtained at clustering were used for the Kaplan–Meier analysis, to evaluate the prognosis significance of LUAD patients. Survival analysis was performed by using the R survival package, and the survival curve was drawn by using the R survminer package.
2.4. ANOVA Feature Ranking of miRNA and RNA Expression to Develop SVM Classifier and LUAD Prognosis-Dependent Classifiers
The multi-omics data used to draw a Kaplan–Meier plot were split into 60% for a training dataset and 40% for a test dataset. Analysis of Variance (ANOVA) method was applied to 60% training dataset to rank miRNA and RNA contributing to the subtypes. ANOVA method with the inferred labels was conducted by using the R limma package [19].
Ranked miRNAs from 5 to 20 and ranked RNAs from 5 to 30 were systematically used to develop SVM. A fixed number of miRNA and RNA were then applied to develop another three classifiers (k-nearest neighbors (KNN), Random Forest (RF), and Logistic Regression (LR)), to compare the accuracy with SVM.
2.5. Clinical Characterization
Two distinct populations clustered by K-means algorism were estimated, using their prognosis with their clinical information by Kaplan–Meier analysis. Clinical data used were obtained from previous reports [20], LUAD data were extracted from TCGA-CDR-Supplementary Table S1, and smoking history indicator was downloaded from the GDC data portal website [21] by selecting the “bcr biotab” option on the “Data Format” list, under the “Files” tab. On the “Cases” tab, we selected the Exposures Environmental Tobacco Smoke Exposure with the project TCGA-LUAD (file name; nationwidechildren.org_clinical_patient_luad.txt).
2.6. Somatic Mutation Analysis (SNPs and Small Indels)
LUAD somatic mutation data were downloaded from University of California, Santa Cruz (UCSC) Xena server (https://xenabrowser.net/datapages/) and analyzed for mutations occurring in each patient.
2.7. Copy Number Analysis
Log2 transformed LUAD copy number dataset was downloaded from UCSC Xena server (https://xenabrowser.net/datapages/). Copy number variant was analyzed with the platform of Affymetrix SNP 6.0 platform and assembled by hg38.
2.8. Pathway Analysis Enrichment in the Poor Prognosis Subtype
Gene set enrichment analysis (GSEA), Kyoto Encyclopedia of Genes and Genomes (KEGG) analysis, and Gene Ontology (GO) analysis were performed by using DESeq2, fgsea, and tidyquant packages in R, to analyze enriched pathways in the poor survival subtype.
2.9. Identification of the Novel Genes Associated with LUAD Patient Survival
Expression analysis was performed between the two subtypes, using the R DESeq2 package. Then, the top 25 statistically significant RNAs between the subtypes obtained from the analysis were used to analyze whether one was associated with patient survival. To draw the Kaplan–Meier plot and to obtain p-values from each analysis, OncoLnc web server (http://www.oncolnc.org) was used [22]. Then, 25% from the high-expression subgroup (n = 123) and 25% from the low-expression subgroup (n = 123) were used to compute prognosis. The remaining 50%, forming the intermediate-expression subgroup was excluded from the analysis.
3. Results
3.1. Subtypes Obtained from Unsupervised Approach
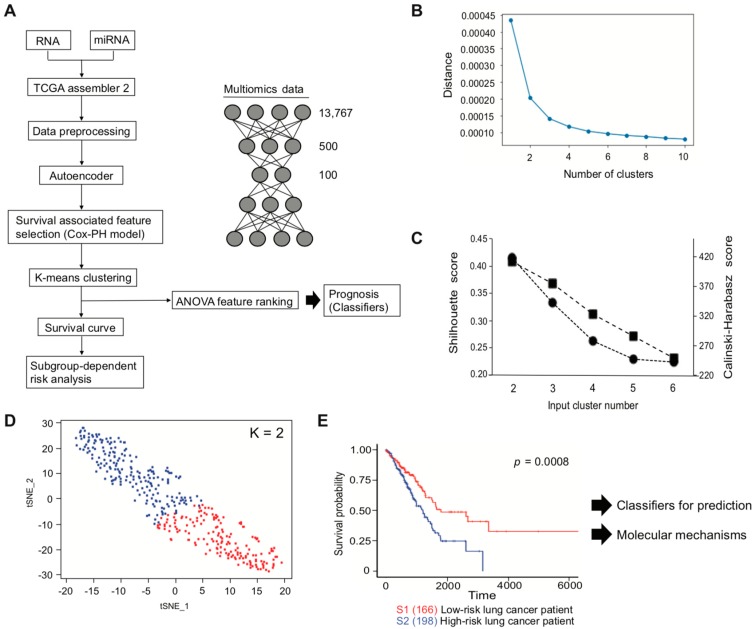
We used TCGA LUAD data for multi-omics analysis, to identify prognosis-related genes. Multi-omics data were generated by TCGA assembler 2, and the data were preprocessed before conducting the omics analysis described in the Materials and Methods section. A total of 13,767 features from RNA-seq and miRNA-seq data were used as an input, which were then encoded to bottleneck feature space of dimension 100 through the autoencoder (Figure 1A). To select the clinically associated features from the bottleneck features, univariate Cox-PH model was performed. In total, 33 out of 100 features showed a statistical significance by log-rank test (p < 0.05, Supplementary Table S1). Therefore, the 33 features were further interrogated, to determine whether they could be subcategorized depending on survival outcome. We first roughly estimated the number of clusters through the elbow method (Figure 1B) and then refined the result with more precise analyses, using the Silhouette index and Calinski–Harabasz criterion (Figure 1C; black circle (Silhouette index) and black square (Calinski–Harabasz criterion)). Both of them indicated cluster number two as an optimal number for clustering. Thus, K-means clustering was conducted with K = 2, which showed a reasonable clustering result, using t-SNE for visualization (Figure 1D). The inferred labels obtained from K-means clustering were applied to estimate patient survival, and patients were successfully sub-classed into either a poor (high-risk) or a good (low-risk) survival subtype (Figure 1E).
Figure 1.
Overall workflow for classification of lung-cancer subtypes. (A) Multi-omics analysis pipeline. (B) Clustering result of elbow method. (C) Clustering results of the Silhouette index and Calinski–Harabasz criterion. (D) Clustering result of K-means clustering. Red dot represents S1, and blue dot represents S2 subtype in Figure 1E. (E) Kaplan–Meier plot using patient labels obtained from Figure 1D.
3.2. Performance of Four Classifiers Using Inferred Labels
To predict lung-cancer-patient survival, we developed several supervised classifiers for which inputs were obtained from the unsupervised autoencoder. We first considered developing an SVM model because of the previously reported prediction success using multi-omics data from TCGA LIHC [12] and the neuroblastoma project combined from Therapeutically Applicable Research to Generate Effective Treatment (TARGET) with Sequencing Quality Control [13].
For a rigorous evaluation, the multi-omics data we used to draw the Kaplan–Meier plot in Figure 1E were split into a training dataset and a test dataset. With the inferred labels, an ANOVA method was applied to the training dataset, to rank the miRNA and RNA that contribute to the subtypes (Supplementary Table S2, ranked top 20 miRNAs and top 30 RNAs). As we expected and initially speculated on obtaining the interpretable results, top ranked miRNAs were matched to the sequences of top ranked genes analyzed by TargetScanHuman web server [23] (http://www.targetscan.org/vert_72/). We then systematically used high-ranking miRNAs and RNAs, to build the SVM. The developed SVM was evaluated by using the test dataset, to estimate its accuracy. The combination of the top 20 miRNA and top 25 RNA expressions gave the best prediction results and had an accuracy of 0.82 with the test dataset (Table 1). The result of confusion matrix is as shown in Table 2.
Table 1.
Evaluation of SVM model performance.
| Number of Features (miRNA Expression + RNA Expression) |
Train Score Accuracy | Test Score Accuracy |
|---|---|---|
| 10 (5 + 5) | 0.61 | 0.57 |
| 20 (10 + 10) | 0.81 | 0.66 |
| 30 (15 + 15) | 0.89 | 0.71 |
| 40 (20 + 20) | 0.94 | 0.82 |
| 45 (20 + 25) | 0.95 | 0.82 |
| 50 (20 + 30) | 0.97 | 0.80 |
Table 2.
Confusion matrix of SVM.
| Predicted Positive | Predicted Negative | |
|---|---|---|
| Positive class | 62 | 10 |
| Negative class | 17 | 57 |
Although the combination of the feature selection by ANOVA, followed by the development of an SVM model, gave the best performance of cancer-patient-survival prediction [13]. In this case, we investigated three additional classifiers, KNN performed with either a hyperparameter of Manhattan or Euclidean distance, RF with either a hyperparameter of Entropy or Gini impurity, and LR with either L1 or L2 regression. The best test score of KNN was 0.76, 0.67 for RF and 0.75 for LR (Table 3). As we expected, these results suggested that SVM is the best classifier if we follow the multi-omics-autoencoder-clinical-associated feature selection by Cox-PH pipeline.
Table 3.
Evaluation of KNN, RF, and LR performance.
| KNN | RF | LR | ||||||
|---|---|---|---|---|---|---|---|---|
| Class | Manhattan | Euclidean | Tree | Entropy | Gini | C | L1 | L2 |
| 1 | 0.72 | 0.70 | 1 | 0.54 | 0.54 | 1 | 0.75 | 0.74 |
| 2 | 0.71 | 0.68 | 2 | 0.64 | 0.64 | 5 | 0.72 | 0.75 |
| 3 | 0.76 | 0.73 | 3 | 0.64 | 0.66 | 10 | 0.71 | 0.74 |
| 4 | 0.73 | 0.74 | 4 | 0.64 | 0.67 | 50 | 0.70 | 0.71 |
| 5 | 0.74 | 0.75 | 5 | 0.66 | 0.67 | 100 | 0.70 | 0.71 |
| 6 | 0.71 | 0.72 | 6 | 0.66 | 0.66 | 500 | 0.70 | 0.69 |
| 7 | 0.73 | 0.75 | 7 | 0.67 | 0.65 | 1000 | 0.70 | 0.70 |
| 8 | 0.71 | 0.75 | 8 | 0.67 | 0.65 | |||
| 9 | 0.73 | 0.75 | 9 | 0.67 | 0.65 | |||
| 10 | 0.73 | 0.75 | 10 | 0.67 | 0.65 | |||
3.3. Insight into the Genes that Are Associated with Patient Prognosis
Identifying the types of biological features is of interest, and thus, we first investigated the clinical data in the different subtypes. Table 4 shows that there were more new tumor events in the high-risk group (41.9%; (83/198)), as compared with the low-risk group (28.9%; (48/166)) (Fisher test p = 0.01), and that female patients tended to be in the high-risk group (58.0%; (115/198) versus 50.6%; (84/166) in the low-risk group, Fisher test p = 0.15). On the other hand, ages at diagnosis, tumor stages, and smoking history indicator seem to be similar in percentage in the two subtypes.
Table 4.
Clinical characterization in LUAD low-risk and high-risk subtypes.
| Low-Risk (n = 166) | High-Risk (n = 198) | ||
|---|---|---|---|
| Age at initial pathologic diagnosis (age) | 65.5 ± 9.8 | Age at initial pathologic diagnosis (age) | 65.6 ± 10.2 |
| Tumor stage * | (No.) | Tumor stage * | (No.) |
| Discrepancy | 1 | Discrepancy | 2 |
| Stage I | 2 | Stage I | 2 |
| Stage IA | 47 | Stage IA | 50 |
| Stage IB | 48 | Stage IB | 53 |
| Stage II | 0 | Stage II | 1 |
| Stage IIA | 20 | Stage IIA | 19 |
| Stage IIB | 14 | Stage IIB | 29 |
| Stage IIIA | 21 | Stage IIIA | 31 |
| Stage IIIB | 3 | Stage IIIB | 4 |
| Stage IV | 10 | Stage IV | 7 |
| Gender | (No.) | Gender | (No.) |
| Male | 82 | Male | 79 |
| Female | 84 | Female | 119 |
| Vital state | (No.) | Vital state | (No.) |
| Alive | 116 | Alive | 117 |
| Dead | 50 | Dead | 81 |
| Overall survival time (days) | 996.0 ± 967.2 | Overall survival time (days) | 730.5 ± 560.0 |
| New tumor event | (No.) | New tumor event | (No.) |
| Yes | 48 | Yes | 83 |
| No | 118 | No | 115 |
| Days to event | 588.9 ± 539.0 | Days to event | 503.7 ± 444.4 |
| Progression-free interval | (No.) | Progression-free interval | (No.) |
| Available | 59 | Available | 88 |
| Progression-free interval time (days) | 836.9 ± 874.2 | Progression-free interval time (days) | 605.8 ± 518.3 |
| Smoking history indicator | (No.) | Smoking history indicator | (No.) |
| 1 | 22 | 1 | 29 |
| 2 | 39 | 2 | 45 |
| 3 | 46 | 3 | 48 |
| 4 | 54 | 4 | 69 |
| 5 | 0 | 5 | 4 |
| NA or unknown | 5 | NA or unknown | 3 |
* American Joint Committee on Cancer (AJCC) pathology states.
Next, we aimed to examine if the subtypes have well-investigated gene mutations, and if so, whether these vary between subtypes. We decided to analyze 18 gene mutations that were found through a comprehensive molecular profiling of TCGA LUAD [6,24]. The result is summarized in Table 5. Our findings indicate that NF1, a tumor-suppressor gene that negatively regulates the RAS signaling pathway was more often mutated in the high-risk subtype (14.1% versus 6.0% in the low-risk subtype, Fisher test p = 0.01). However, other genes, such as TP53, which is frequently mutated in human cancers [25], or EGFR, KRAS, and BRAF, which are mutations that often inform patient therapy [26], were not highly mutated in the high-risk subtype, suggesting that there may be other factors that can distinguish the different subtypes.
Table 5.
Gene mutations analysis of 18 genes reported as having a statistically significant mutation in the LUAD dataset. Gene names and number of mutations (number of patients) are summarized.
| Genes | Low-Risk | High-Risk |
|---|---|---|
| TP53 | 64 (63) | 83 (80) |
| KRAS | 42 (41) | 40 (38) |
| KEAP1 | 26 (26) | 27 (26) |
| STK11 | 20 (18) | 17 (16) |
| EGFR | 17 (13) | 17 (13) |
| NF1 | 12 (10) | 29 (28) |
| BRAF | 12 (10) | 8 (8) |
| SETD2 | 11 (10) | 12 (10) |
| RBM10 | 10 (9) | 11 (10) |
| MGA | 10 (9) | 17 (14) |
| MET | 4 (4) | 5 (5) |
| ARID1A | 9 (8) | 10 (7) |
| PIK3CA | 8 (8) | 9 (8) |
| SMARCA4 | 12 (11) | 18 (18) |
| RB1 | 7 (6) | 6 (6) |
| CDKN2A | 7 (5) | 6 (6) |
| U2AF1 | 0 (0) | 0 (0) |
| RIT1 | 4 (3) | 2 (2) |
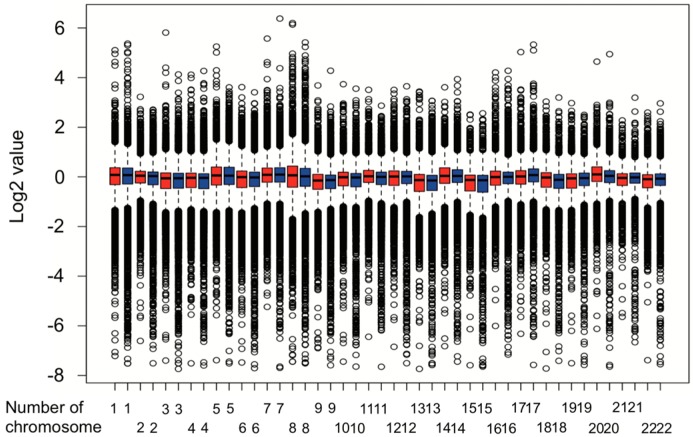
Therefore, we carried out a copy number variation analysis. Results from the copy number variation analysis were shown as Figure 2. Chromosome 2, 6, 8, 10, 11, 17, 18, 19, 20, and 22 had a different copy numbers (p < 0.05, Mann–Whitney U-test).
Figure 2.
Copy number variation analysis in two subtypes. Red box represents low-risk subtype, and blue box represents high-risk subtype.
3.4. GSEA, KEGG Pathway Analysis, and GO Analysis
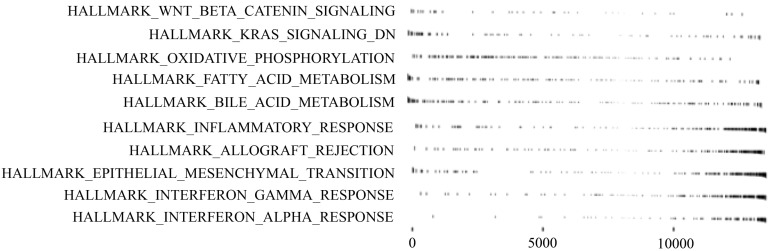
Next, to explore the molecular mechanism that underlies the subtypes, differentially expressing RNA was extracted, using DESeq2 [27]. We performed a GSEA, KEGG pathway analysis, and GO analysis [28,29,30,31] to elucidate enriched pathways in the subtypes. The result of GSEA is shown in Figure 3, and the results of the KEGG and GO analyses are summarized in Table 6.
Figure 3.
Subtype-specific signaling pathways obtained from GSEA. The left represents pathway names, and the right represents gene ranks.
Table 6.
Summary of KEGG pathway, miRNA, and GO analysis.
| KEGG Pathway | p-Value | Adjusted p-Value |
| Fatty acid metabolism | 1.64 × 10−3 | 2.00 × 10−3 |
| Oxidative phosphorylation | 1.49 × 10−3 | 2.00 × 10−3 |
| Valine, leucine and isoleucine degradation | 1.61 × 10−3 | 2.00 × 10−3 |
| Arachidonic acid metabolism | 1.69 × 10−3 | 2.00 × 10−3 |
| Pyruvate metabolism | 1.64 × 10−3 | 2.00 × 10−3 |
| KEGG miRNA | p-Value | Adjusted p-Value |
| miR-501_AAAGGAT | 1.45 × 10−3 | 0.319 |
| miR-26a/miR-26b_TACTTGA | 8.44 × 10−3 | 0.481 |
| miR-507_GTGCAAA | 8.71 × 10−3 | 0.481 |
| miR-33_CAATGCA | 6.05 × 10−3 | 0.481 |
| miR-200b/miR-200c/miR-429_CAGTATT | 2.03 × 10−2 | 0.660 |
| GO Analysis | p-Value | Adjusted p-Value |
| Spinal cord development | 1.61 × 10−3 | 5.97 × 10−2 |
| Neuromuscular junction development | 1.64 × 10−3 | 5.97 × 10−2 |
| Cytoplasmic translation | 3.08 × 10−3 | 5.97 × 10−2 |
| Positive regulation of calcium ion transport | 2.87 × 10−3 | 5.97 × 10−2 |
| Regulation of antigen receptor mediated signaling pathway | 2.62 × 10−3 | 5.97 × 10−2 |
GSEA revealed that Wnt/β-catenin-signaling KRAS-signaling genes downregulated by KRAS activation that could be regulated by NF1 (Table 5), oxidative phosphorylation, and fatty acid metabolism were upregulated. Meanwhile, epithelial-mesenchymal transition (EMT) and inflammatory response, such as interferon gamma response and interferon alpha response, were downregulated in the high-risk subtype, as compared with the low-risk subtype (Figure 3). Notably, above pathways are one of the typical pathways of cancer [32,33].
KEGG pathway analysis showed that fatty acid metabolism, oxidative phosphorylation, valine, leucine, and isoleucine degradation pathways were significantly different. For the miRNA, miR-501 that activates Wnt/β-catenin signaling in gastric cancer and colorectal cancer [34,35] and tumor suppressor miR-26 that has been reported to regulate the Wnt/β-catenin signaling in prostate cancer and cholangiocarcinoma [36] were significance between subtypes. Intriguingly, miR-26 is also known to contribute TGF-β-induced EMT [37] and inflammation response [38], which could be associated with the low-risk subtype. Furthermore, miR-507 targets KDR (kinase insert domain receptor or VEGF receptor), and VEGF receptor is regulated by Wnt/β-catenin signaling and KRAS pathways [39]. The VEGF receptor is required in response to VEGF-dependent cell survival via EMT in colon carcinoma cell lines [40,41]. Additionally, miR-200 families are well-known miRNAs that regulate Wnt/β-catenin signaling [34] and also directly regulate EMT by targeting transcriptional repressors of ZEB1 and ZEB2, which regulate CDH1 expression [42,43]. These results indicate that the miRNAs we identified may play an important role in both high- and low-risk subtypes.
The top five GO were summarized in Table 6. Spinal cord development (GO:0021510): the spinal cord primarily conducts sensory and motor nerve impulses in the central nervous systems. The spinal cord development is co-annotated with cell–cell signaling by Wnt (GO:0198738) that is in the 6th place of 1505 co-occurring terms. Neuromuscular junction development (GO:0007528): the neuromuscular junction is the process to organize a neuromuscular junction at the cellular level. The neuromuscular junction development is co-annotated with blood vessels morphogenesis (GO:0048514) that could be associated with tumor angiogenesis in the 9th place of 1341 co-occurring terms and Wnt signalosome (GO:1990909) is also co-annotated in the 16th place of the same co-occurring therms. Cytoplasmic translation (GO:0002181); cytoplasmic translation is linked with translation (GO:0006412) and the translation is further linked with gene expression (GO:0010467), which is concordant with widely accepted knowledge that gene expression and protein synthesis are upregulated in cancer. Positive regulation of calcium ion transport (GO:0051928) is any process that activates calcium ion efflux. Cytosolic calcium ion concentration is well known to be associated with cellular functions such as gene expression, proliferation, differentiation, migration, metabolism, apoptosis, and angiogenesis [44]. Regulation of antigen receptor-mediated signaling pathway (GO:0050854) is any process that regulates signaling pathways by the cross-linking of an antigen receptor on immune cells. In particular, the relation between neuromuscular junction and cancer development has been previously demonstrated. Yes-associated protein (YAP) and β-catenin regulate synaptic differentiation and the YAP activation induced by the suppression of Hippo pathways promotes liver cancer development [45].
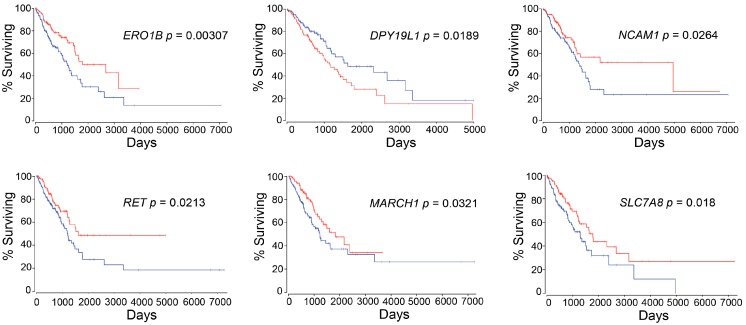
3.5. Identification of the Novel Genes Associated with LUAD Patient Survival
We focused on the top 25 differentially expressing RNAs that were extracted by using DESeq2, as shown in Table 7 and the RNA expression levels of the top 25 genes were investigated by using OncoLnc, whether they were associated with LUAD patient survival or not. Interestingly, six out of 25 genes, which are ERO1B (endoplasmic reticulum oxidoreductase 1 beta), DPY19L1 (dpy-19 like C-mannosyltransferase 1), NCAM1 (neural cell adhesion molecule 1), RET (ret proto-oncogene), MARCH1 (membrane associated ring-CH-type finger 1), and SLC7A8 (solute carrier family 7 member 8), were identified as survival-associated genes that can affect patient prognosis (Figure 4).
Table 7.
Top 25 RNAs with statistical significance between the two subtypes.
| Rank | Gene Name | Log2 Fold Change | p-Value | Adjusted p-Value |
|---|---|---|---|---|
| 1 | H19 | 3.45 | 3.01 × 10−40 | 4.08 × 10−36 |
| 2 | CBR1 | 1.71 | 3.98 × 10−27 | 2.69 × 10−23 |
| 3 | ENO3 | 1.93 | 1.47 × 10−20 | 6.64 × 10−17 |
| 4 | POLR3H | 0.89 | 1.22 × 10−18 | 4.12 × 10−15 |
| 5 | GREB1 | 1.49 | 2.39 × 10−18 | 6.47 × 10−15 |
| 6 | ERO1B | 1.18 | 2.20 × 10−16 | 4.97 × 10−13 |
| 7 | KCNE4 | 1.40 | 2.81 × 10−15 | 5.44 × 10−12 |
| 8 | ODC1 | 1.32 | 5.12 × 10−15 | 8.68× 10−12 |
| 9 | DPY19L1 | −0.72 | 2.38 × 10−14 | 3.58 × 10−11 |
| 10 | WNT4 | 1.22 | 5.19 × 10−14 | 7.03 × 10−11 |
| 11 | NCAM1 | 1.37 | 1.48 × 10−13 | 1.82 × 10−10 |
| 12 | RET | 1.82 | 3.39 × 10−13 | 3.83 × 10−10 |
| 13 | ESR1 | −1.17 | 1.93 × 10−12 | 2.02 × 10−9 |
| 14 | MARCH1 | 0.94 | 2.54 × 10−12 | 2.45 × 10−9 |
| 15 | SLIT1 | 1.28 | 2.98 × 10−12 | 2.70 × 10−9 |
| 16 | ZNF710 | 0.82 | 4.35 × 10−12 | 3.68 × 10−9 |
| 17 | GID8 | 0.38 | 7.25 × 10−12 | 5.78 × 10−9 |
| 18 | CLU | 1.06 | 9.22 × 10−12 | 6.94 × 10−9 |
| 19 | AREG | −1.37 | 1.07 × 10−11 | 7.66 × 10−9 |
| 20 | ALDH3A2 | 0.72 | 1.15 × 10−11 | 7.80 × 10−9 |
| 21 | MMP11 | −1.30 | 1.33 × 10−11 | 8.61 × 10−9 |
| 22 | FAM105A | 0.98 | 2.33 × 10−11 | 1.43 × 10−8 |
| 23 | SLC7A8 | 0.88 | 3.19 × 10−11 | 1.88 × 10−8 |
| 24 | BATF2 | −0.68 | 4.27 × 10−11 | 2.41 × 10−8 |
| 25 | ST3GAL3 | 0.53 | 4.99 × 10−11 | 2.71 × 10−8 |
Figure 4.
Newly identified survival-associated genes. The red line represents high-expression subtype, and the blue line represents low-expression subtype.
3.6. Co-Expression Analysis Reveals ERO1B, ENO3, and KCNE4 Genes Are Directed to Upregulate
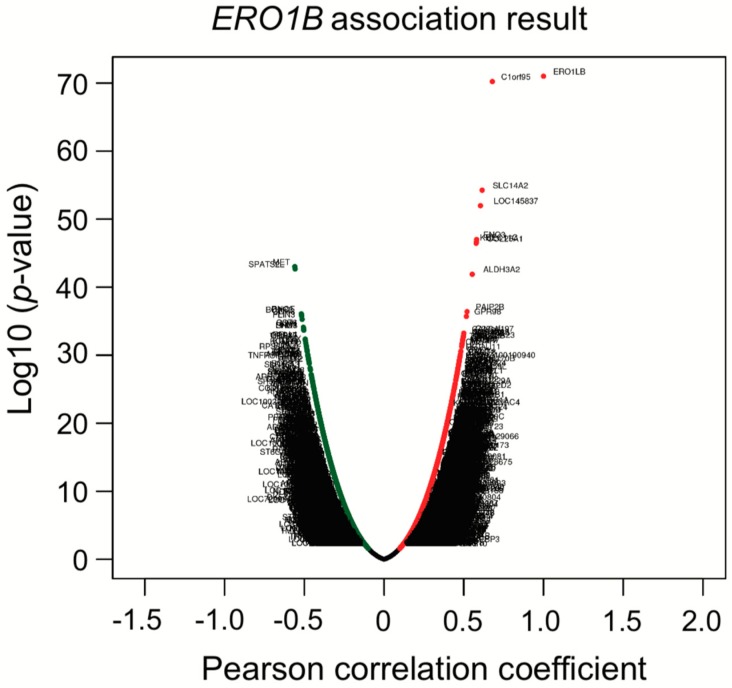
To further investigate whether the identified six genes are associated with, or potentially show, synergistic effects, a co-expression analysis was conducted with the TCGA LUAD dataset, using LinkedOmics, an interactive web-based tool [46] (http://www.linkedomics.org/login.php). Intriguingly, ERO1B was co-expressed with ENO3 that is in the third place of top 25 genes, KCNE4 that is in the seventh place, and RET that is in the 12th place (Figure 5; Table 7 and Table 8). Although we do not know the detailed mechanisms behind why these genes are co-expressed, epigenetic regulations or even miRNAs that can regulate multiple target genes, even with one miRNA only, may be involved. To address the abovementioned hypothesis, a miRNA target gene search was performed to find out miRNAs with a sequence that matches to the ERO1B, ENO3, KCNE4, and RET transcripts. The TargetScanHuman web server was used for the analysis, and we found that miR-6838 had a predicted to consequential pairing of ENO3 and KCNE4. This suggests that the mechanism of co-expression regulation of ENO3 and KCNE4 may be related to the miRNA expression.
Figure 5.
Co-expression analysis of ERO1B. Correlation analysis was performed with Pearson correlation test against ERO1B gene.
Table 8.
Summary of co-expression genes.
| Rank | Target Gene | Pearson Correlation | p-Value | FDR * | |
|---|---|---|---|---|---|
| 1 | C1orf95 | 0.679 | 6.11 × 10−71 | 6.12 × 10−67 | |
| 2 | SLC14A2 | 0.615 | 5.63 × 10−55 | 3.75 × 10−51 | |
| 3 | LOC145837 | 0.605 | 1.07 × 10−52 | 5.36 × 10−59 | |
| 4 | ENO3 |

|
0.581 | 9.89 × 10−48 | 3.95 × 10−44 |
| 5 | SEC11C | 0.578 | 2.53 × 10−47 | 7.47 × 10−44 | |
| 6 | KIT | 0.578 | 2.67 × 10−47 | 7.47 × 10−44 | |
| 7 | COL25A1 | 0.578 | 3.55 × 10−47 | 8.86 × 10−44 | |
| 8 | MET | −0.559 | 9.74 × 10−44 | 2.16 × 10−40 | |
| 9 | SPATS2L | −0.558 | 2.06 × 10−43 | 4.11 × 10−40 | |
| 10 | ALDH3A2 | 0.553 | 1.28 × 10−42 | 2.33 × 10−39 | |
| 46 | RET |

|
0.482 | 2.91 × 10−31 | 1.24 × 10−28 |
| 77 | KCNE4 |

|
0.462 | 1.50 × 10−28 | 3.85 × 10−26 |
* False discovery rate (Benjamini–Hochberg procedure). Red arrows indicate ones of top 25 RNA shown in Table 7.
4. Discussion
Here, we developed a pipeline, using a TCGA LUAD dataset, with the aim of efficiently identifying genes of interest that are associated with the lung cancer patients survival. Pipeline development started with multi-omics data to implement an autoencoder, followed by clinical associated feature selection by Cox-PH. Selected features were then labeled depending on the result of K-means clustering, which is later demonstrated to be associated with patient survival. The inferred labels, or two subtypes classed by K-means clustering, were applied to plot a Kaplan–Meier survival estimation, to visualize whether the labels were associated with a poor or a good patient survival subtype and used to develop an SVM that can successfully predict patient prognosis.
During autoencoder optimization, batch size, epochs, and activation function varied. Based on our results, a batch size of 1 and epochs of 150, or even between 100 and 150, gave reasonable results, while avoiding overfitting by early stopping [47] and/or Rectified Linear Unit (ReLU) function replacing tanh function at the last layer [48] did not work well in our autoencoder. Clustering analyses applied with clinically associated features demonstrated that K = 2 was the optimal number, and this is concordant with the previous report performing with the 10 TCGA cancer dataset [49].
The multi-omics analysis with TCGA LIHC showed more TP53 gene mutations in the high-risk subtype (Fisher test p = 0.042), but unfortunately, other genes such as EGFR were not investigated [12]. In our case, TP53 was slightly more mutated in the high-risk subtype (0.42%), compared with the low-risk subtype (0.39%), but not significance (Fisher test p = 0.633). Whole-exome sequencing data of LUAD were analyzed independently in the oncogene-positive subset (KRAS, EGFR, ERBB2, BRAF, MET, ALK, RET, ROS, HRAS, NRAS, and MAP2K1 driver mutations) and the oncogene-negative subset [24]. The authors found that TP53 and NF1 co-mutations were enriched in the oncogene-negative subset. Additionally, RNA profiling provided new subtypes that the proximal-inflammatory subtype (formerly squamoid) was co-mutated with TP53 and NF1 [6,24]. In our analysis, we found NF1 mutations were more enriched in the high-risk subtype, suggesting that the high-risk subtype we identified might correspond to the subset that has TP53 and NF1 co-mutations in [24].
ERO1B was first reported as an endoplasmic reticulum disulfide oxidase [50]. Later, additional biological functions, such as insulin biogenesis and glucose homeostasis, were demonstrated [51]. In relation to lung cancer, ERO1B has been recently identified as a gene that, together with an additional three genes identified using TCGA LUAD dataset, is able to predict patient prognosis [52] and has been suggested to be a biomarker for pancreatic cancer [53,54]. DPY19L1 was firstly identified as an unclassified gene from human brain cDNA libraries in 1998 [55]. Still, its function remains unknown, and no evidence has been reported so far on the link between DPY19L1 and cancer prognosis. Therefore, to the best of our knowledge, this is the first report to reveal the association between DPY19L1 expression and the prognosis in lung cancer patients. NCAM1 or CD56 is a member of the immunoglobulin superfamily involved in cell–cell interaction and cell–matrix interactions during the development. Additionally, it plays a fundamental role in processes such as cell migration and cell survival, in specific phenotypes of neural cells [56]. NCAM1 may play an important role in EMT not only in intrahepatic cholangiocarcinoma but also in lung cancer via miR-200 (Table 6 and [57]). Recently, antibody-based anticancer treatment was analyzed with the expression levels of NCAM1. The phase 1/2 study is ongoing, since NCAM1 is expressed on several malignancies, including SCLC [58,59,60], or could be available to predict prognosis in adult acute lymphoblastic leukemia patient [61]. RET was identified in 1985. RET is a receptor-type tyrosine kinase with multiple domains. RET was first discovered in papillary thyroid carcinoma, and later in sporadic tumors, neurodegenerative diseases, and Hirschsprung’s disease [62]. RET can be found in the rearrangement of genes generating RET fusion proteins in many cancers, including lung cancer, and thus an inhibitor was recently approved by the FDA for cancer therapy [63]. It is important to note that, not only genetic factors, but also epigenetic factors, affect RET expression that influences the probability of patient survival [64]. It suggests that multi-omics analysis, including epigenetic data, could improve availability of output, in terms of precision medicine or personalized medicine, as we recently reported [65]. The E3 ubiquitin ligase MARCH1 plays an important role in immunology [66], although only a few publications have focused on MARCH1 in the context of cancer [67,68]. Therefore, further studies in this area are required and could have the potential to contribute to the field of cancer research, and more particularly lung cancer. SLC7A8 or LAT-2 is an L-type amino acid transporter-2 protein that binds and regulates mechanistic target of rapamycin kinase (mTOR) activation in pancreatic cancer [69]. L-type amino acid transporters are known to be novel targets for cancer therapy [70,71]. However, as is the case for DPY19L1 and MARCH1, no publications have demonstrated the link between lung cancers.
We identified six genes with expression levels that were associated with patient survival, using the autoencoder, followed by bioinformatics analysis. The practice guidelines in oncology illustrate a strategy of patient treatment based on the result of gene mutations, such as EGFR, ALK, ROS1, and PD-L1 [72], but not considering RNA or miRNA expression levels. It might be of great help to estimate survival outcome and to make treatment strategy for patients if several RNA-expression levels, such as ERO1B, DPY19L1, NCAM1, RET, MARCH1, and/or SLC7A8, are also examined at the time when patients are diagnosed.
To elucidate whether six genes were only associated with LUAD patient prognosis or whether these genes were key regulators of other types of NSCLC prognosis, survival analysis against TCGA lung squamous cell carcinoma (LUSC) was performed. The p-values for high expression and low expression of genes of interest were from 0.106 to 0.674, suggesting that the genes we identified were LUAD-specific survival-related genes. This result gave us confidence that the multi-omics analysis we developed truly identified input-data-specific survival-associated features. In other words, if we would like to identified genes of interest that are associated with LUSC patient survival, we need to use a LUSC dataset as an input.
Co-expression analysis showed that ERO1B, ENO3, RET, and KCNE4 were co-upregulated. Later, we showed that ENO3 and KCNE4 have a target sequence for miR-6838. The functional role of miR-6838 has been recently investigated, showing that miR-6838 regulates EMT in triple-negative breast cancer by inhibiting the Wnt pathway [73]. KEGG miRNA target analysis in Table 6 indicated that miR-26 families were enriched in the high-risk subtype. Based on the TargetScanHuman analysis, miR-26 is one of four miRNAs that was predicted to bind to the ERO1B transcript and suppress gene expression. As we mentioned in Section 3.4, KEGG miRNA analysis revealed that miR-501, miR-26, miR-507, miR-33, and miR-200/miR-429 were involved in lung-cancer subtypes. The miRNAs we identified have been previously reported as regulating Wnt/β-catenin signaling and/or contributing EMT signaling. Taken together, not only KEGG analysis, but also co-expression analysis, gave us insight into the molecular mechanisms that underlie patient prognosis.
A limitation of this study is the difficulty with preparing the validation dataset. The SVM model we developed uses 20 miRNA and 25 RNA expressions. Thus, we need a validation dataset that includes miRNA expression, RNA expression, and clinical information. There are datasets available that include miRNA expression (GSE63805) and RNA expression (GSE63459), together with clinical information. However, some of the miRNA expression and RNA expression for the top 20 miRNA and top 25 RNAs used to develop the SVM model were missing, and therefore we were not able to evaluate the SVM with the abovementioned publicly available dataset. This constitutes a technical limitation of the study, since it makes it difficult to assess the robustness of the developed classifier. Therefore, we decided to use the TCGA dataset again, for the validation. All data (364 patients) were randomly split into 75% and 25%, and the 25% of patient data were used for validation. Result of the accuracy score of the developed SVM model was 0.92.
The second limitation of this study is the fact the frequency of certain gene mutations can vary depending on the patients’ race. For example, EGFR mutation is more often found in Asian American patients than Caucasian or African American patients [74]. Therefore, the SVM model we developed may not be able to distinguish a high-risk subtype from a low-risk subtype if the model is applied to a different distributed dataset such as on containing an Asian population. In that case, the SVM model will need to be redeveloped.
5. Conclusions
Lung cancer is one of the leading causes of death worldwide. Understanding the factors that are linked with patient prognosis is essential to enhance the effectiveness of patient therapy. Recently, multi-omics analysis has emerged, allowing to classify groups of patients based on prognosis and at a more individual scale, in the context of precision medicine. Here, we only combined RNA expression, miRNA expression, and clinical information, to develop an SVM to predict patient survival in lung cancer. This enables us to significantly reduce the input omics data size, since DNA methylation data are by far bigger than other omics data; it also enables us to become interpretable.
Using bioinformatics, we established that (1) the NF1 gene was more mutated, and (2) Wnt/β-catenin, as well as KRAS signaling pathways, can occur in the high-risk subtype. On the other hand, (3) pathways of KRAS, Wnt/β-catenin, and/or TGF-β derived EMT pathways, together with the combination of miRNA expression, could be the ones associated with low-risk subtype.
Acknowledgments
We would like to thank Daisuke Okanohara and Kouya Shiraishi for their helpful feedback. We would also like to thank all members of Hamamoto laboratory for their kind help.
Supplementary Materials
The following are available online at https://www.mdpi.com/2218-273X/10/4/524/s1. Table S1: Survival associated 33 features extracted by log-rank test. Table S2: ANOVA ranked miRNA and genes (top 20 and 25, respectively) used for SVM. Computer code: Keras code we implemented an autoencoder algorithm.
Author Contributions
K.A. performed and analyzed the experiments and wrote the manuscript; K.A., K.K., S.J., M.T., S.T., K.T., M.K., S.K., J.S., and R.H. discussed data; R.H. supervised the experiments and edited the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by JST CREST (Grant Number JPMJCR1689), JSPS Grant-in-Aid for Scientific Research on Innovative Areas (Grant Number JP18H04908), and the Public/Private R&D Investment Strategic Expansion Program (PRISM), Cabinet Office, Japan.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Siegel R.L., Miller K.D., Jemal A. Cancer statistics, 2020. CA Cancer J. Clin. 2020;70:7–30. doi: 10.3322/caac.21590. [DOI] [PubMed] [Google Scholar]
- 2.Ferlay J., Colombet M., Soerjomataram I., Dyba T., Randi G., Bettio M., Gavin A., Visser O., Bray F. Cancer incidence and mortality patterns in Europe: Estimates for 40 countries and 25 major cancers in 2018. Eur. J. Cancer. 2018;103:356–387. doi: 10.1016/j.ejca.2018.07.005. [DOI] [PubMed] [Google Scholar]
- 3.Malvezzi M., Carioli G., Bertuccio P., Boffetta P., Levi F., La Vecchia C., Negri E. European cancer mortality predictions for the year 2019 with focus on breast cancer. Ann. Oncol. 2019;30:781–787. doi: 10.1093/annonc/mdz051. [DOI] [PubMed] [Google Scholar]
- 4.WHO The Global Cancer Observatory. [(accessed on 28 March 2020)]; Available online: https://gco.iarc.fr/today/data/factsheets/populations/392-japan-fact-sheets.pdf.
- 5.Mok T.S. Personalized medicine in lung cancer: What we need to know. Nat. Rev. Clin. Oncol. 2011;8:661–668. doi: 10.1038/nrclinonc.2011.126. [DOI] [PubMed] [Google Scholar]
- 6.Inamura K. Lung Cancer: Understanding Its Molecular Pathology and the 2015 WHO Classification. Front. Oncol. 2017;7:193. doi: 10.3389/fonc.2017.00193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Esteva A., Kuprel B., Novoa R.A., Ko J., Swetter S.M., Blau H.M., Thrun S. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017;542:115–118. doi: 10.1038/nature21056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ardila D., Kiraly A.P., Bharadwaj S., Choi B., Reicher J.J., Peng L., Tse D., Etemadi M., Ye W., Corrado G., et al. End-to-end lung cancer screening with three-dimensional deep learning on low-dose chest computed tomography. Nat. Med. 2019;25:954–961. doi: 10.1038/s41591-019-0447-x. [DOI] [PubMed] [Google Scholar]
- 9.Xu Y., Hosny A., Zeleznik R., Parmar C., Coroller T., Franco I., Mak R.H., Aerts H. Deep Learning Predicts Lung Cancer Treatment Response from Serial Medical Imaging. Clin. Cancer Res. 2019;25:3266–3275. doi: 10.1158/1078-0432.CCR-18-2495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hosny A., Parmar C., Coroller T.P., Grossmann P., Zeleznik R., Kumar A., Bussink J., Gillies R.J., Mak R.H., Aerts H. Deep learning for lung cancer prognostication: A retrospective multi-cohort radiomics study. PLoS Med. 2018;15:e1002711. doi: 10.1371/journal.pmed.1002711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ramazzotti D., Lal A., Wang B., Batzoglou S., Sidow A. Multi-omic tumor data reveal diversity of molecular mechanisms that correlate with survival. Nat. Commun. 2018;9:4453. doi: 10.1038/s41467-018-06921-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chaudhary K., Poirion O.B., Lu L., Garmire L.X. Deep Learning-Based Multi-Omics Integration Robustly Predicts Survival in Liver Cancer. Clin. Cancer Res. 2018;24:1248–1259. doi: 10.1158/1078-0432.CCR-17-0853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang L., Lv C., Jin Y., Cheng G., Fu Y., Yuan D., Tao Y., Guo Y., Ni X., Shi T. Deep Learning-Based Multi-Omics Data Integration Reveals Two Prognostic Subtypes in High-Risk Neuroblastoma. Front. Genet. 2018;9:477. doi: 10.3389/fgene.2018.00477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wei L., Jin Z., Yang S., Xu Y., Zhu Y., Ji Y. TCGA-assembler 2: Software pipeline for retrieval and processing of TCGA/CPTAC data. Bioinformatics. 2018;34:1615–1617. doi: 10.1093/bioinformatics/btx812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yuan C., Yang H. Research on K-Value Selection Method of K-Means Clustering Algorithm. J—Multidiscip. Sci. J. 2019;2:16. doi: 10.3390/j2020016. [DOI] [Google Scholar]
- 16.Rousseeuw P.J. Silhouettes: A graphical aid to the interpretation and validation of cluster analysis. J. Comput. Appl. Math. 1987;20:13. doi: 10.1016/0377-0427(87)90125-7. [DOI] [Google Scholar]
- 17.Calinski T., Harabasz J. A dendrite method for cluster analysis. Commun. Stat. - Theory Methods. 1974;3:27. doi: 10.1080/03610927408827101. [DOI] [Google Scholar]
- 18.Laurens van der Maaten G.H. Visualizing Data using t-SNE. J. Mach. Learn. Res. 2008;9:2579–2605. [Google Scholar]
- 19.Ritchie M.E., Phipson B., Wu D., Hu Y., Law C.W., Shi W., Smyth G.K. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015;43:e47. doi: 10.1093/nar/gkv007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu J., Lichtenberg T., Hoadley K.A., Poisson L.M., Lazar A.J., Cherniack A.D., Kovatich A.J., Benz C.C., Levine D.A., Lee A.V., et al. An Integrated TCGA Pan-Cancer Clinical Data Resource to Drive High-Quality Survival Outcome Analytics. Cell. 2018;173:400–416 e11. doi: 10.1016/j.cell.2018.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.GDC data portal website. [(accessed on 28 March 2020)]; Available online: https://portal.gdc.cancer.gov/repository.
- 22.Anaya J. OncoLnc: Linking TCGA survival data to mRNAs, miRNAs, and lncRNAs. Peer J. Comput. Sci. 2016;2:11. doi: 10.7717/peerj-cs.67. [DOI] [Google Scholar]
- 23.Agarwal V., Bell G.W., Nam J.W., Bartel D.P. Predicting effective microRNA target sites in mammalian mRNAs. Elife. 2015;4 doi: 10.7554/eLife.05005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cancer Genome Atlas Research N. Comprehensive molecular profiling of lung adenocarcinoma. Nature. 2014;511:543–550. doi: 10.1038/nature13385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Petitjean A., Achatz M.I., Borresen-Dale A.L., Hainaut P., Olivier M. TP53 mutations in human cancers: Functional selection and impact on cancer prognosis and outcomes. Oncogene. 2007;26:2157–2165. doi: 10.1038/sj.onc.1210302. [DOI] [PubMed] [Google Scholar]
- 26.Shaw A.T., Engelman J.A. ALK in lung cancer: Past, present, and future. J. Clin. Oncol. 2013;31:1105–1111. doi: 10.1200/JCO.2012.44.5353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Love M.I., Huber W., Anders S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014;15:550. doi: 10.1186/s13059-014-0550-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ashburner M., Ball C.A., Blake J.A., Botstein D., Butler H., Cherry J.M., Davis A.P., Dolinski K., Dwight S.S., Eppig J.T., et al. Gene ontology: Tool for the unification of biology. The Gene Ontology Consortium. Nat. Genet. 2000;25:25–29. doi: 10.1038/75556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.The Gene Ontology Consortium The Gene Ontology Resource: 20 years and still GOing strong. Nucleic Acids Res. 2019;47:D330–D338. doi: 10.1093/nar/gky1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sergushichev A.A. An algorithm for fast preranked gene set enrichment analysis using cumulative statistic calculation. bioRxiv. 2016 [Google Scholar]
- 31.Kanehisa M., Goto S. KEGG: Kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 2000;28:27–30. doi: 10.1093/nar/28.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hanahan D., Weinberg R.A. The hallmarks of cancer. Cell. 2000;100:57–70. doi: 10.1016/S0092-8674(00)81683-9. [DOI] [PubMed] [Google Scholar]
- 33.Hanahan D., Weinberg R.A. Hallmarks of cancer: The next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 34.Fan D., Ren B., Yang X., Liu J., Zhang Z. Upregulation of miR-501-5p activates the wnt/beta-catenin signaling pathway and enhances stem cell-like phenotype in gastric cancer. J. Exp. Clin. Cancer Res. 2016;35:177. doi: 10.1186/s13046-016-0432-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wu F., Xing T., Gao X., Liu F. miR5013p promotes colorectal cancer progression via activation of Wnt/betacatenin signaling. Int. J. Oncol. 2019;55:671–683. doi: 10.3892/ijo.2019.4852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Peng Y., Zhang X., Feng X., Fan X., Jin Z. The crosstalk between microRNAs and the Wnt/beta-catenin signaling pathway in cancer. Oncotarget. 2017;8:14089–14106. doi: 10.18632/oncotarget.12923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cai Z.G., Wu H.B., Xu X.P., Li W. Down-regulation of miR-26 plays essential roles in TGFbeta-induced EMT. Cell Biol. Int. 2018 doi: 10.1002/cbin.11029. [DOI] [PubMed] [Google Scholar]
- 38.Kwon Y., Kim Y., Eom S., Kim M., Park D., Kim H., Noh K., Lee H., Lee Y.S., Choe J., et al. MicroRNA-26a/-26b-COX-2-MIP-2 Loop Regulates Allergic Inflammation and Allergic Inflammation-promoted Enhanced Tumorigenic and Metastatic Potential of Cancer Cells. J. Biol. Chem. 2015;290:14245–14266. doi: 10.1074/jbc.M115.645580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang X., Gaspard J.P., Chung D.C. Regulation of vascular endothelial growth factor by the Wnt and K-ras pathways in colonic neoplasia. Cancer Res. 2001;61:6050–6054. [PubMed] [Google Scholar]
- 40.Jia L., Liu W., Cao B., Li H., Yin C. MiR-507 inhibits the migration and invasion of human breastcancer cells through Flt-1 suppression. Oncotarget. 2016;7:36743–36754. doi: 10.18632/oncotarget.9163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bates R.C., Goldsmith J.D., Bachelder R.E., Brown C., Shibuya M., Oettgen P., Mercurio A.M. Flt-1-dependent survival characterizes the epithelial-mesenchymal transition of colonic organoids. Curr. Biol. 2003;13:1721–1727. doi: 10.1016/j.cub.2003.09.002. [DOI] [PubMed] [Google Scholar]
- 42.Korpal M., Kang Y. The emerging role of miR-200 family of microRNAs in epithelial-mesenchymal transition and cancer metastasis. RNA Biol. 2008;5:115–119. doi: 10.4161/rna.5.3.6558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Park S.M., Gaur A.B., Lengyel E., Peter M.E. The miR-200 family determines the epithelial phenotype of cancer cells by targeting the E-cadherin repressors ZEB1 and ZEB2. Genes Dev. 2008;22:894–907. doi: 10.1101/gad.1640608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Berridge M.J., Lipp P., Bootman M.D. The versatility and universality of calcium signalling. Nat. Rev. Mol. Cell Biol. 2000;1:11–21. doi: 10.1038/35036035. [DOI] [PubMed] [Google Scholar]
- 45.Xiong W.C., Mei L. Agrin to YAP in Cancer and Neuromuscular Junctions. Trends Cancer. 2017;3:247–248. doi: 10.1016/j.trecan.2017.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vasaikar S.V., Straub P., Wang J., Zhang B. LinkedOmics: Analyzing multi-omics data within and across 32 cancer types. Nucleic Acids Res. 2018;46:D956–D963. doi: 10.1093/nar/gkx1090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Raskutti G., Wainwright M.J., Yu B. Early stopping for non-parametric regression: An optimal data-dependent stopping rule; Proceedings of the IEEE 2011 49th Annual Allerton Conference; Monticello, IL, USA. 28–30 September 2011. [Google Scholar]
- 48.Li P., Nguyen P.-M. On Random Deep Weight-Tied Autoencoders: Exact Asymptotic Analysis, Phase Transitions, and Implications to Training; Proceedings of the ICLR 2019 Conference; New Orleans, LA, USA. 6–9 May 2019. [Google Scholar]
- 49.Rappoport N., Shamir R. Multi-omic and multi-view clustering algorithms: Review and cancer benchmark. Nucleic Acids Res. 2018;46:10546–10562. doi: 10.1093/nar/gky889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pagani M., Fabbri M., Benedetti C., Fassio A., Pilati S., Bulleid N.J., Cabibbo A., Sitia R. Endoplasmic reticulum oxidoreductin 1-lbeta (ERO1-Lbeta), a human gene induced in the course of the unfolded protein response. J. Biol. Chem. 2000;275:23685–23692. doi: 10.1074/jbc.M003061200. [DOI] [PubMed] [Google Scholar]
- 51.Zito E., Chin K.T., Blais J., Harding H.P., Ron D. ERO1-beta, a pancreas-specific disulfide oxidase, promotes insulin biogenesis and glucose homeostasis. J. Cell. Biol. 2010;188:821–832. doi: 10.1083/jcb.200911086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang W., Shen Y., Feng G. Predicting the survival of patients with lung adenocarcinoma using a four-gene prognosis risk model. Oncol. Lett. 2019;18:535–544. doi: 10.3892/ol.2019.10366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Xie J., Zhu Y., Chen H., Shi M., Gu J., Zhang J., Shen B., Deng X., Zhan X., Peng C. The Immunohistochemical Evaluation of Solid Pseudopapillary Tumors of the Pancreas and Pancreatic Neuroendocrine Tumors Reveals ERO1Lbeta as a New Biomarker. Medicine (Baltimore) 2016;95:e2509. doi: 10.1097/MD.0000000000002509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhu T., Gao Y.F., Chen Y.X., Wang Z.B., Yin J.Y., Mao X.Y., Li X., Zhang W., Zhou H.H., Liu Z.Q. Genome-scale analysis identifies GJB2 and ERO1LB as prognosis markers in patients with pancreatic cancer. Oncotarget. 2017;8:21281–21289. doi: 10.18632/oncotarget.15068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nagase T., Ishikawa K.-i., Suyama M., Kikuno R., Hirosawa M., Miyajima N., Tanaka A., Kotani H., Nomura N., Ohara O. Prediction of the coding sequences of unidentified human genes. XII. The complete sequences of 100 new cDNA clones from brain which code for large proteins in vitro. DNA Res. 1998;5:10. doi: 10.1093/dnares/5.6.355. [DOI] [PubMed] [Google Scholar]
- 56.Maness P.F., Schachner M. Neural recognition molecules of the immunoglobulin superfamily: Signaling transducers of axon guidance and neuronal migration. Nat. Neurosci. 2007;10:19–26. doi: 10.1038/nn1827. [DOI] [PubMed] [Google Scholar]
- 57.Oishi N., Kumar M.R., Roessler S., Ji J., Forgues M., Budhu A., Zhao X., Andersen J.B., Ye Q.H., Jia H.L., et al. Transcriptomic profiling reveals hepatic stem-like gene signatures and interplay of miR-200c and epithelial-mesenchymal transition in intrahepatic cholangiocarcinoma. Hepatology. 2012;56:1792–1803. doi: 10.1002/hep.25890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Socinski M.A., Kaye F.J., Spigel D.R., Kudrik F.J., Ponce S., Ellis P.M., Majem M., Lorigan P., Gandhi L., Gutierrez M.E., et al. Phase 1/2 Study of the CD56-Targeting Antibody-Drug Conjugate Lorvotuzumab Mertansine (IMGN901) in Combination With Carboplatin/Etoposide in Small-Cell Lung Cancer Patients With Extensive-Stage Disease. Clin. Lung Cancer. 2017;18:68–76 e2. doi: 10.1016/j.cllc.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 59.Yoshida T., Ri M., Kinoshita S., Narita T., Totani H., Ashour R., Ito A., Kusumoto S., Ishida T., Komatsu H., et al. Low expression of neural cell adhesion molecule, CD56, is associated with low efficacy of bortezomib plus dexamethasone therapy in multiple myeloma. PLoS ONE. 2018;13:e0196780. doi: 10.1371/journal.pone.0196780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Crossland D.L., Denning W.L., Ang S., Olivares S., Mi T., Switzer K., Singh H., Huls H., Gold K.S., Glisson B.S., et al. Antitumor activity of CD56-chimeric antigen receptor T cells in neuroblastoma and SCLC models. Oncogene. 2018;37:3686–3697. doi: 10.1038/s41388-018-0187-2. [DOI] [PubMed] [Google Scholar]
- 61.Aref S., Azmy E., El-Bakry K., Ibrahim L., Mabed M. Prognostic impact of CD200 and CD56 expression in adult acute lymphoblastic leukemia patients. Hematology. 2018;23:263–270. doi: 10.1080/10245332.2017.1404276. [DOI] [PubMed] [Google Scholar]
- 62.Jhiang S.M. The RET proto-oncogene in human cancers. Oncogene. 2000;19:5590–5597. doi: 10.1038/sj.onc.1203857. [DOI] [PubMed] [Google Scholar]
- 63.Anonymous. First RET Inhibitor on Path to FDA Approval. Cancer Discov. 2019;9:1476–1477. [Google Scholar]
- 64.Griseri P., Garrone O., Lo Sardo A., Monteverde M., Rusmini M., Tonissi F., Merlano M., Bruzzi P., Lo Nigro C., Ceccherini I. Genetic and epigenetic factors affect RET gene expression in breast cancer cell lines and influence survival in patients. Oncotarget. 2016;7:26465–26479. doi: 10.18632/oncotarget.8417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hamamoto R., Komatsu M., Takasawa K., Asada K., Kaneko S. Epigenetics Analysis and Integrated Analysis of Multiomics Data, Including Epigenetic Data, Using Artificial Intelligence in the Era of Precision Medicine. Biomolecules. 2019;10:62. doi: 10.3390/biom10010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Liu H., Mintern J.D., Villadangos J.A. MARCH ligases in immunity. Curr. Opin. Immunol. 2019;58:38–43. doi: 10.1016/j.coi.2019.03.001. [DOI] [PubMed] [Google Scholar]
- 67.Meng Y., Hu J., Chen Y., Yu T., Hu L. Silencing MARCH1 suppresses proliferation, migration and invasion of ovarian cancer SKOV3 cells via downregulation of NF-kappaB and Wnt/beta-catenin pathways. Oncol. Rep. 2016;36:2463–2470. doi: 10.3892/or.2016.5076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Xie L., Dai H., Li M., Yang W., Yu G., Wang X., Wang P., Liu W., Hu X., Zhao M. MARCH1 encourages tumour progression of hepatocellular carcinoma via regulation of PI3K-AKT-beta-catenin pathways. J. Cell Mol. Med. 2019;23:3386–3401. doi: 10.1111/jcmm.14235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Feng M., Xiong G., Cao Z., Yang G., Zheng S., Qiu J., You L., Zheng L., Zhang T., Zhao Y. LAT2 regulates glutamine-dependent mTOR activation to promote glycolysis and chemoresistance in pancreatic cancer. J. Exp. Clin. Cancer Res. 2018;37:274. doi: 10.1186/s13046-018-0947-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hayashi K., Anzai N. Novel therapeutic approaches targeting L-type amino acid transporters for cancer treatment. World J. Gastrointest. Oncol. 2017;9:21–29. doi: 10.4251/wjgo.v9.i1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Wang Q., Holst J. L-type amino acid transport and cancer: Targeting the mTORC1 pathway to inhibit neoplasia. Am. J. Cancer Res. 2015;5:1281–1294. [PMC free article] [PubMed] [Google Scholar]
- 72.Ettinger D.S., Wood D.E., Aisner D.L., Akerley W., Bauman J., Chirieac L.R., D’Amico T.A., DeCamp M.M., Dilling T.J., Dobelbower M., et al. Non-Small Cell Lung Cancer, Version 5.2017, NCCN Clinical Practice Guidelines in Oncology. J. Natl. Compr. Canc. Netw. 2017;15:504–535. doi: 10.6004/jnccn.2017.0050. [DOI] [PubMed] [Google Scholar]
- 73.Liu G., Wang P., Zhang H. MiR-6838-5p suppresses cell metastasis and the EMT process in triple-negative breast cancer by targeting WNT3A to inhibit the Wnt pathway. J. Gene. Med. 2019:e3129. doi: 10.1002/jgm.3129. [DOI] [PubMed] [Google Scholar]
- 74.Bauml J., Mick R., Zhang Y., Watt C.D., Vachani A., Aggarwal C., Evans T., Langer C. Frequency of EGFR and KRAS mutations in patients with non small cell lung cancer by racial background: Do disparities exist? Lung Cancer. 2013;81:347–353. doi: 10.1016/j.lungcan.2013.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.