Abstract
Helicobacter pylori (H. pylori) is one of the most common human pathogens, affecting half of the world’s population. Approximately 20% of the infected patients develop gastric ulcers or neoplastic changes in the gastric stroma. An infection also leads to the progression of epithelial–mesenchymal transition within gastric tissue, increasing the probability of gastric cancer development. This paper aims to review the role of H. pylori and its virulence factors in epithelial–mesenchymal transition associated with malignant transformation within the gastric stroma. The reviewed factors included: CagA (cytotoxin-associated gene A) along with induction of cancer stem-cell properties and interaction with YAP (Yes-associated protein pathway), tumor necrosis factor α-inducing protein, Lpp20 lipoprotein, Afadin protein, penicillin-binding protein 1A, microRNA-29a-3p, programmed cell death protein 4, lysosomal-associated protein transmembrane 4β, cancer-associated fibroblasts, heparin-binding epidermal growth factor (HB-EGF), matrix metalloproteinase-7 (MMP-7), and cancer stem cells (CSCs). The review summarizes the most recent findings, providing insight into potential molecular targets and new treatment strategies for gastric cancer.
Keywords: Helicobacter pylori infection, EMT, epithelial–mesenchymal transition, gastric cancer, virulence factors
1. Introduction
Helicobacter pylori (H. pylori) is a helix-shaped, Gram-negative, microaerophilic, flagellated bacterium that is capable of biofilm formation and converting from spiral to coccoid form [1,2,3,4,5,6]. It is a highly invasive microorganism responsible for one of the highest prevalences of chronic infections worldwide, even though over 80% of infected patients remain asymptomatic [7,8,9,10,11,12,13]. H. pylori pathogenesis is due to several virulence factors including urease, cytotoxin-associated gene A (CagA), vacuolating cytotoxin (VacA), outer inflammatory protein A (OipA), duodenal ulcer promoting gene A (DupA), neutrophil-activating protein A (NAP), heat shock proteins (Hsp10, Hsp60), and sialic acid-binding adhesin (SabA) [14,15,16,17,18,19,20,21,22,23,24].
H. pylori is classified as a “group 1” carcinogen according to the World Health Organization (WHO) [25]. Gastric cancer is one of the most common diseases related to H. pylori infection, responsible for approximately 75% of gastric cancer incidents worldwide [26,27,28,29]. The discrepancy in the severity of gastric cancer is associated with many factors and mechanisms, among which various genotypes of H. pylori strains play a role [30,31,32,33,34,35,36,37,38,39,40]. H. pylori induces other diseases of the alimentary tract, including gastritis, peptic ulcer disease, mucosa-associated lymphoid tissue lymphoma, GERD symptoms, and dyspepsia [41,42,43,44,45,46]. There is an increasing interest in the role of H. pylori in the pathogenesis of ischemic heart disease, diabetes mellitus, and Alzheimer’s disease [47,48,49,50].
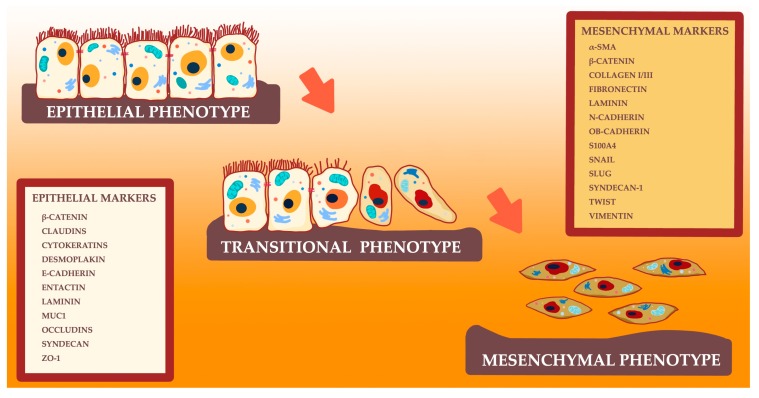
Epithelial–mesenchymal transition (EMT) is the process of acquisition of the mesenchymal properties by epithelial cells involved in metastasis, invasion, and progression of various cancers (Figure 1) [51].
Figure 1.
Schematic of the epithelial–mesenchymal transition and chosen epithelial and mesenchymal markers.
As a physiological process, EMT is observed during organogenesis, tissue development, remodeling, and wound healing [52,53,54]; contrarily, any deregulations might induce carcinogenesis [55,56]. EMT-induced carcinogenesis is the prevalent cause of various malignancies including head and neck squamous cell carcinoma, papillary thyroid carcinoma, lung, pancreatic, gastric, ovarian, prostate, and breast cancer [57,58,59,60,61,62,63,64,65,66,67,68].
During this process, epithelial cells undergo a series of biochemical changes, which lead to the loss of polarity and migratory capacity of cells, resulting in cell shape changes (cell elongation). EMT promotes the transformation of immobile epithelial cells into motile mesenchymal cells, enhancing the metastatic properties [69,70]. Further, adherens and tight junctions become impaired, resulting in a mesenchymal phenotype [12,71,72,73]. Altered E-and N-cadherin levels and the following β-catenin activation promote the expression of many tumor-associated proteins, including cyclin D1, CD44, or c-MYC [54,74,75,76,77,78,79]. A transformation of cell phenotype enhances the migratory properties, invasiveness, and apoptosis resistance of cells [80]. Moreover, EMT is involved in the induction of cancer stem cell properties, which leads to chemoresistance and tumor dormancy [81,82,83].
H. pylori infection significantly affects the gastric microenvironment by induction of several inflammatory responses via infiltrating macrophages, neutrophils, regulatory T-cells, and natural killer cells [84,85]. Inflammatory mediators such as cytokines, chemokines, and metalloproteinases that are released by gastric and infiltrating cells promote the EMT process within gastric cells; transforming growth factor β (TGF-β) is probably one of the most relevant EMT inducers [86,87,88]. Thus, chronic inflammation might significantly contribute to EMT progression and carcinogenesis [89,90,91]. A significant number of H. pylori virulence factors are considered being associated with the promotion of EMT in gastric cells, which consequently causes neoplasia and malignant transformation. This review summarizes several mechanisms associated with epithelial–mesenchymal transition, gastric tumor microenvironment, and the influence of H. pylori infection, although some described mechanisms are not only H. pylori-specific. Even though H. pylori-induced carcinogenesis is not fully understood, several mechanisms have already been deciphered.
2. Cytotoxin-Associated Gene A
2.1. CagA and EMT
Among many virulence factors of H. pylori, cag pathogenicity island (cagPAI) probably plays a key role in carcinogenesis [92,93,94]. It encodes a type 4 secretion system (T4SS) and the CagA oncoprotein [95,96]. The T4SS forms a pilus that allows the injection of CagA into a cell, transforming its shape into the so-called “hummingbird phenotype” characterized by an elongated cell shape commonly observed in EMT [97,98]. Injection of the CagA into the cell via the T4SS induces signal transduction, with one of the most relevant mecahnisms being the nuclear factor κB (NF-κB) signaling pathway involving extracellular regulated kinases 1/2 (ERK-1/2) [99,100,101]. These kinases are involved in the conformational changes of the cytoskeleton, which might enhance the EMT process [102]. The inhibition of ERK and c-Jun N-terminal kinase (JNK) results in the lower expression of the ‘hummingbird’ phenotype induced by H. pylori [103]. CagA in host cells is tyrosine phosphorylated and interacts with protein tyrosine phosphatase 2 (SHP-2), also inducing the progression of the “hummingbird phenotype” [104,105]. CagA enhances EMT via the stabilization of Snail protein, which is essential in carcinogenesis, mainly by the reduction of glycogen synthase kinase-3 (GSK-3) activity [106]. CagA-positive H. pylori strains with CagA containing phosphorylation-functional EPIYA motifs present significantly higher expression of mesenchymal markers such as vimentin, Snail, and ZEB-1 and the stem cell marker CD44 [96,107,108,109,110]. Many studies have shown that CagA-positive H. pylori strains induce a higher probability of gastric carcinogenesis and induction of EMT process [111,112,113]. Incidents of CagA-positive H. pylori infection present poor clinical outcome, and higher invasion and metastatic characteristics [114]. Besides, there is an increasing interest in microRNAs (miRNAs), since these are reported to play a role in gastric carcinogenesis and progression [115,116].
2.2. CagA and Cancer Stem Cell Properties
Recent research suggests that cells that undergo EMT obtain the ability to acquire cancer stem cell (CSC) properties [117,118,119,120,121,122,123]. The main source of gastric CSCs includes stem cells and progenitor cells; other studies suggest that CSCs originate from bone marrow-derived cells [124,125]. Due to the ability of self-renewal and differentiation into a vast number of cells, CSCs have the property of tumorigenesis induction [126,127]. Gastric CSCs are primarily generated by CagA-positive H. pylori strain infection [128,129]. High expression of CD44, a compelling marker of CSCs, predisposes cells to the induction of mesenchymal phenotype and EMT [130,131,132,133,134,135,136].
Bessède et al. (2014) studied the role of H. pylori in the generation of cells with CSC properties, including several gastric epithelial cell lines (AGS, MKN-45, MKN-74) [103]. The role of CagA in the induction of CSC properties was studied on H. pylori 7.13 wild-type (WT) CagA-positive strain and its knock-out mutants—7.13CagA-negative and 7.13DCagE-negative H. pylori strains. Only the wild-type (WT) (7.13CagA-positive) strain-induced mesenchymal changes and EMT in cells; cells infected by CagA-positive strains, presented higher expression of mesenchymal markers—CD44, Snail1, vimentin, or zinc finger E-box binding homeobox 1 (ZEB1), while an expression of epithelial markers—cytokeratin 7 (CK7) or osteopontin (SSP-1) was lowered [103]. The migration and invasion properties of cells were enhanced during infection by CagA-positive H. pylori strains. The relevance of the infection by CagA-positive H. pylori strain on EMT in gastric cancer was confirmed by significantly higher expression of CD44 and mesenchymal markers in tumor samples.
The Wnt/β-catenin signaling pathway is involved in CagA-positive H. pylori EMT and the induction of CSC properties [137]. Likewise, chronic CagA-positive H. pylori infection with N-nitrosoguanidine (MNNG) stimulation causes CSC features with dysplastic lesions and mesenchymal phenotype. Amieva and Peek (2016) observed that CD44+ cells with CSC features displayed increased CagA half-life [26]. Accumulation of intracellular CagA was confirmed in CD44+ gastric CSCs [138]. H. pylori-infected (CagA-positive) gastric cancer cells exhibit CSC properties via increased expression of surface markers—CD44 and Lgr5 with Nanog, Oct4, and c-myc upregulation [139,140]. CagA impairs transcription factor CDX1 expression, promoting EMT, and CSC features in gastric epithelial cells [141].
2.3. CagA and Yes-Associated Protein Pathway
Yes-Associated-Protein (YAP) is an element of the Hippo tumor suppressor signaling pathway, which plays a crucial role in the maintenance of the proper size of organs, tissue homeostasis, cell proliferation, and stem cell maintenance [142,143,144]. Since YAP induces the progression of carcinogenesis, it is considered to be an oncogenic protein [145,146,147]. Increased expression of YAP activates several oncoproteins including connective tissue growth factor (CTGF), cysteine-rich angiogenic inducer 61 (CYR61), or MYC oncogene [148,149]. Besides, the overexpression of YAP lowers the expression of epithelial markers including E-cadherin, which induce mesenchymal changes and EMT [150].
Li et al. (2018) showed a significantly higher expression of YAP and TAZ (YAP paralog) in cancerous gastric tissues with a positive correlation between YAP, TAZ levels, and tumor size [151]. During early tumor stages, YAP is expressed mainly in the cell cytoplasm, whereas in advanced stages it is expressed in the nucleus. CagA-positive H. pylori strain induces higher YAP expression and decreases E-cadherin, N-cadherin, and Slug levels, promoting EMT.
Other studies have shown a potential role of GSK3/β-catenin or AMP-activated protein kinase (AMPK) pathways, which are regulated by CagA, in the enhancement of the YAP pathway [152,153]. Molina-Castro et al. (2020) showed that infection by CagA-positive H. pylori upregulates YAP1 and large tumor suppressor 2 (LATS2) expression in gastric epithelial cells [154]. Overexpression of the oncogenic YAP1 is associated with aggressiveness and poor prognosis [155]. Gastric cancer development and progression are further promoted by the dysregulated YAP1/SLC35B4 axis; another mechanism involves altered IL-1β levels [156,157]. These findings show that YAP might become a potential target in gastric cancer treatment.
3. Tumor Necrosis Factor α-Inducing Protein of H. pylori in EMT
H. pylori strains produce a high quantity of tumor necrosis factor-α (TNF-α)-inducing protein (Tipα protein), which binds to the cell surface nucleolin and induces carcinogenic alterations [158,159,160,161,162,163]. It makes up one of the potential markers of H. pylori virulence [164,165]. By combining with the nucleolin receptor, Tipα induces mesenchymal changes of cells via EMT progression [166,167,168]. Tipα, as a carcinogenic factor, activates NF-κB, promoting gastric carcinogenesis by inhibiting miR-3178 expression [169,170]. Besides TNF-α release, Tipα also induces the expression of several chemokines, including chemokine (C-C motif) ligand 2 (Ccl2), chemokine (C-C motif) ligand 7(Ccl7), chemokine (C-C motif) ligand 20 (Ccl20), C-X-C motif chemokine 11 (Cxc11), chemokine (C-X-C motif) ligand 2 (Cxcl2), C-X-C motif chemokine 5 (Cxcl5), and C-X-C motif chemokine 10 (Cxcl10) [171,172,173,174]. EMT is promoted by TGF-β, hepatocyte growth factor (HGF), tumor necrosis factor-α (TNF-α), or hypoxia-inducible factor 1α (HIF1α) [175,176]. In gastric carcinogenesis, Tipα, along with CagA and VacA, plays an underlying role primarily in mucosal damage [177,178].
Suganuma et al. showed that H. pylori infection increases the quantity of Tipα protein in gastric cancer tissue, inducing tumor progression in H. pylori carcinogenesis [161]. Tipα reduces cell stiffness and phosphorylates various oncoproteins; it also enhances filopodia formation, morphological, and conformational changes within cells, and expression of vimentin via MEK-ERK phosphorylation, confirming its role in EMT progression [179,180].
Researchers have suggested the role of Tipα and nucleolin receptor (88 kDa) on the migration properties of gastric cancer cells [161,181]. Fujiki et al. showed that EMT phenotype induced by Tipα could be inhibited via small interfering RNAs targeted for the nucleolin receptor, showing its role in EMT progression [182]. Thus, potential ligands of nucleolin receptors (e.g., lactoferrin) might inhibit H. pylori infection by inhibiting Tipα and nucleolin interaction [183,184].
Tipα induces the formation of filopodia and a reduction of cell stiffness, predisposing cells to higher motility [185]. It has been reported that Tipα induces higher levels of IL-1β, TNF-α, and IL-8 in SGC7901 cells [164]. Furthermore, H. pylori infection promotes the Il-6/STAT3 signaling pathway in AGS cells, which is one factor promoting EMT [186]. Inoue et al. observed that vaccinations with Tipα did successfully eradicate H. pylori infection [187].
Antigenic Lpp20 Protein
The Lpp20 protein plays an important role as an H. pylori virulence factor, promoting its colonization and survival properties [188]. Lpp20 is a lipoprotein embedded in the external membrane of H. pylori, which enhances the stimulation of cell proliferation. Lpp20 expression is increased in the acidic pH of stomach juice and during iron depletion [189,190].
Lpp20 (a structural homologue of Tipα), is one of the carcinogenic factors released by H. pylori via NF-κB pathway activation [183]. Tipα and Lpp20 induce EMT mainly by stimulating cell proliferation, migratory properties of cells, and filopodia formation [191].
Even though Lpp20 and Tipα have different locations within the bacterium (external and inner membranes respectively), these proteins show similar effects on gastric cancer cells by stimulating EMT and gastric cancer progression.
4. Afadin Protein Downregulation
Afadin is a cytoplasmic actin-filament-binding protein responsible for the formation and stabilization of tight and adherens junctions [192,193,194,195]. Marques et al. (2018) observed that infection by H. pylori lowered the expression of Afadin protein independently of CagA and VacA in MKN74 and NCI-N87 cell lines [196]. Downregulation of Afadin resulted in dysregulation of tight junctions and adherens junctions, which caused inappropriate cell permeability, stiffness, and impaired transepithelial electrical resistance. The decreased level of Afadin induced higher expression of Snail (EMT marker) and increased actin stress fiber formation; no changes were observed in Slug, ZEB1, vimentin, and N-cadherin levels. So far, this is the first study suggesting a role of Afadin in the EMT induction in gastric cancer cells infected by H. pylori.
5. Penicillin-Binding Protein 1A
Penicillin-binding protein (PBP) is a specialized acyl serine transferase released by H. pylori with an affinity for penicillin binding; any modifications within PBP might induce resistance to β-lactam antibiotics (amoxicillin, penicillin G, ampicillin) [197]. These mainly include either mutations or mosaics (or both) of PBP2X, PBP2B, and PBP1A [198]. It was shown that H. pylori PBPs might present unique characteristics because of several putative genes encoding PBPs.
Huang et al. (2019) showed significant differences between PBP1A mutation-positive H. pylori (H. pylori CagA+/P+) strain and CagA+/P− in terms of clinicopathological characteristics of gastric cancer and EMT induction [199]. H. pylori CagA+/P+ infection resulted in progressive and clinically significant EMT and gastric cancer severity. Researchers have observed decreased levels of E-cadherin and increased α-smooth muscle actin (α-SMA) levels; likewise, it was observed that PBP1A mutation is associated with decreased miR-134 levels. MiR-134 suppresses gastric carcinogenesis by targeting the KRAS gene and Golgi phosphoprotein 3 (GOLPH3) downregulation; another essential target gene of miR-134 is FoxM1 [200,201]. The inhibition of PBP via paepalantine is suggested to be a promising method of H. pylori activity decline [202]. Marcus et al. showed that at pH 3.0, the expression of PBPs genes is significantly decreased [203].
6. Upregulation of MicroRNA-29a-3p
Micro-RNAs constitute a family of small noncoding RNAs, which are regulators of posttranscriptional gene expression by binding to the 3′-untranslated region of mRNA, promoting an inappropriate translation of targeted mRNA. There is an increasing interest in micro-RNA involvement in many diseases and malignancies [204,205,206,207]. A vast number of micro-RNAs are directly associated with the progression of gastric cancer, including microRNA-4513, microRNA-95, and microRNA-4268 [208,209,210].
Sun et al. presented the relevance of upregulation of microRNA-29a-3p and its role in the decreased expression of A20 in patients infected by H. pylori [211]. A20 is the ubiquitin-editing enzyme, which negatively regulates the NF-kB pathway, controlling proper cellular activation, development, and differentiation [212]. H. pylori infection induced the overexpression of microRNA-29a-3p in gastric cancer tissue samples, which resulted in an enhanced ability of the migration of gastric epithelial cells. Furthermore, the silencing of A20 increased the EMT markers Snail, vimentin, and N-cadherin, and decreased E-cadherin levels. The authors have suggested that the overexpression of micro-RNA-29a-3p might be associated with a higher probability of EMT induction in gastric cells.
7. Downregulation of Programmed Cell Death Protein 4
Programmed cell death protein 4 (PDCD4) is a tumor suppressor responsible for the inhibition of cell growth, tumor invasion, metastasis, or induction of apoptosis [213]. It is localized in the nucleus of proliferating cells and binds to the eukaryotic initiation factor-4A (eIF4A) or eukaryotic translation initiation factor 4 G (eIF4G), inhibiting translation [214,215]. PDCD4 controls the inhibition of cancer invasion by regulating the expression of mitogen-activated protein 4 kinases 1 or urokinase plasminogen activator receptor [216]. It is also responsible for the inhibition of the Y-box binding protein expression and connecting with the DNA-binding domain of the TWIST1 gene [217].
PDCD4 is one factor responsible for the induction of carcinogenesis [218]. Yu et al. showed that the downregulation of PDCD4 expression resulted in a decreased level of E-cadherin, increased TWIST1, and vimentin levels in gastric cancerous tissues [219]. PDCD4 downregulation and subsequent alterations in epithelial–mesenchymal markers were induced by CagA-positive H. pylori strain infection. PDCD4 overexpression reduced EMT. MicroRNA-21 overexpression in gastric cancer modulates the expression of the tumor suppressors phosphatase and tensin homolog (PTEN) and PDCD4, altering molecular pathways associated with cell growth, invasion, migration, and apoptosis [220].
8. Upregulation of lysosomal-Associated Protein Transmembrane 4β
Lysosomal-associated protein transmembrane 4β (LAPTM4B) is a proto-oncogene relevant in the progression of tumorigenesis, regulating molecular mechanisms, and cellular functioning, including proliferation, migration, and invasion [221]. LAPTM4B upregulation has been observed in various cancers, including hepatocellular carcinoma, breast cancer, and lung adenocarcinoma [222,223,224].
It has been reported that H. pylori infection leads to the aberrant expression of LAPTM4B in gastric epithelial cells, which eventually induces the EMT process and further malignant transformation [225]. Researchers have observed that LAPTM4B upregulation by H. pylori infection increases the levels of EMT markers (N-cadherin, vimentin) while lowering E-cadherin levels and dysregulating cell–cell junctions. Additionally, there was a noticeable increase of ZEB1, β-catenin, Snail, and Slug markers, whereas tight junction protein-1 (zonula occludens-1, ZO-1) level was decreased. LAPTM4B seems to be a factor strictly associated with EMT induction since it is responsible for regulating cells’ filopodia, increasing motility of gastric cancer cells, and a higher invasion potential [226]. Overexpression of LAPTM4B results in poorer prognosis in various cancers [227].
9. Cancer-Associated Fibroblasts
Physiologically, natural gastric stroma contains only a few fibroblasts, and those are mainly myofibroblasts. The number of fibroblasts is significantly increased in tissues affected by inflammation or neoplasm [228,229,230,231]. In a gastric cancer microenvironment, macrophages via interaction with mesenchymal stem cells induce differentiation of cancer-associated fibroblasts (CAFs) [232,233,234]. CAFs are crucial in the initiation, growth, and migration properties of gastric cancer cells [235,236]. They are responsible for the release of carcinogenic and proinflammatory factors including interleukin-6 (Il-6), cyclooxygenase-2 (COX-2), chemokine (C-X-C motif) ligand 1 (Cxcl1), chemokine (C-X-C motif) ligand 9 (Cxcl9), interferon gamma-induced protein 10 (Cxcl10), stromal cell-derived factor 1 (Cxcl12), and fibroblast-specific protein 1 (FSP1), which promote the EMT process and induce carcinogenesis, promoting migration and invasion [237,238,239]. Activation of death receptor 4 (TRAIL receptor 1, TRAILR1) and ensuing activation of caspase 8 by CAFs induce apoptosis in gastric cells [240,241]. CAFs also facilitate angiogenesis via the production of proangiogenic factors-fibroblast growth factor (FGF), vascular endothelial growth factor (VEGF), interleukin-8 (IL-8), and stromal cell-derived factor 1 (SDF-1) [242,243,244]. Angiogenesis is enhanced by the upregulation of HIF-1α in fibroblasts, which is common during CagA+VacA+ H. pylori infection [245].
H. pylori infection results in the transformation of fibroblasts and myofibroblasts into CAFs [233]. CagA+VacA+ H. pylori infection results in the overexpression of fibroblast activation protein (FAP), fibroblast surface protein (FSP) mRNA, and increased levels of the proinflammatory factors IL-6, IL-8, COX-2, and SDF-1 [246]. Overexpression of FAP alters the regulation of fibroblast growth, impairs tissue repair, induces EMT progression of gastric cancer cells, and epithelial carcinogenesis [247,248,249]. Krzysiek-Maczka et al. observed the overexpression of mesenchymal markers (α-SMA, N-cadherin, vimentin, Snail, Twist) and lowered levels of E-cadherin, antiapoptotic B-cell lymphoma 2 (Bcl-2), and proliferative marker Ki-67 protein within fibroblasts [246]. CagA+VacA+ H. pylori infection resulted in the aberrant apoptosis process, an increased level of collagen production, and impaired fibroblast and myofibroblast differentiation into CAFs. This induced desmoplastic reactions and EMT within gastric cells, promoting carcinogenesis. The increased levels of β1-integrin and COX-2, which are crucial in invasion, metastasis, and angiogenesis, enhanced the migration properties of the infected cells. CagA+Vac+ H. pylori infection results in the upregulation of HIF-1α and tenascin-C (TNC), enhancing EMT and tumor progression, the release of proangiogenic factors, and further CAFs activation [250,251,252]. CagA+Vac+ H. pylori infection activates gastric fibroblasts and induces the release of TGF-β [253].
The tumor-promoting ability of CAFs is enhanced by microRNA dysregulation [254]. CAFs stimulate EMT in gastric cancer cells in a microRNA-214-dependent manner—it induces tumor-promoting ability of CAFs through fibroblast growth factor 9 (FGF9) targeting [255,256]. Likewise, suppression of microRNA-149 (through regulation of IL-6 levels) induces EMT, promoting protumor activity of CAFs [257]. CAFs also promote EMT and gastric carcinogenesis via activation of erythropoietin-producing hepatocellular A2 receptor (EphA2) and IL-6-JAK2-STAT3 signaling pathways [258,259]. CAFs release a significant amount of galectin-1, which promotes EMT and gastric cancer progression by binding to β1 integrin [260]. EMT is also promoted by CAFs-derived IL-33 through the activation of the ERK1/2-SP1-ZEB2 pathway [261].
10. Heparin-Binding Epidermal Growth Factor and Matrix Metalloproteinase-7
Heparin-binding epidermal growth factor (HB-EGF) is an epidermal growth factor receptor (EGFR) cognate ligand with mitogenic and chemotactic properties for fibroblasts and smooth muscle cells [262]. H. pylori infection results in the upregulation of HB-EGF gene expression, which is a potential serological biomarker for gastric cancer [263,264,265,266,267]. HB-EGF increases cell motility, invasiveness, and metastatic properties of gastric cells [268]. HB-EGF upregulation is because of the activation of H. pylori g-glutamyltranspeptidase, activating PI3K, and p38 kinase-dependent signal transduction pathways [269].
Matrix metalloproteinase-7 (MMP-7) is an enzyme responsible for the degradation of adherence between cells in the extracellular matrix, and overexpression of MMP-7 induces a more aggressive course of gastric cancer [270,271,272,273]. MMP-7 and HB-EGF expression is upregulated by H. pylori infection and is associated with EMT [274,275]. Likewise, MMP-7 overexpression is because of increased levels of gastrin, activator protein 1 (AP-1), and NF-kB induced by H. pylori infection [276,277,278,279]. Levels of MMP-7 might correlate with the degree of rehabilitation after treatment and poor prognosis in gastric cancer survival [270,280].
Yin et al. showed that excessive gastrin secretion due to H. pylori infection results in the increased release of MMP-7 and soluble HB-EGF, promoting EMT [281]. HB-EGF might promote tumor growth and EMT by IL-4-conditioned media from macrophages [282]. Besides HB-EGF, other ErbB ligands (transforming growth factor-α (TGF-α) and amphiregulin (AREG)) have a prognostic impact on gastric cancer and might make up potential targets in cancer therapy [283,284,285]. Furthermore, trastuzumab sensitivity in gastric cancer can be predicted by HB-EGF expression [286]. Gastric cancer invasion can be increased by nuclear translocation of the cytoplasmic domain of HB-EGF [287,288]. However, Krakowiak et al. showed that MMP-7 might limit H. pylori-induced inflammation and damage via M1 macrophage polarization suppression [289].
11. Stem Cells
Mesenchymal stem cells (MSCs) present a multipotent potential to differentiate into various cell types, while keeping a capacity for self-renewal [290,291]. MSCs are recruited to the areas of H. pylori infection, neoplasia, or cancer, being involved in the migration properties of gastric cancer cells [292,293,294]. MSCs promote EMT, tumor growth, and metastasis [295,296]. Nanog Homeobox Retrogene P8 (NANOGP8) makes up the main regulator of gastric CSCs [297].
Zhang et al. showed that human umbilical cord MSCs (hucMSCs) infected by H. pylori gained a fibroblastic phenotype, enhancing EMT progression in gastric cancer cells [298]. Furthermore, hucMSCs infected by H. pylori showed a significant decrease in the levels of E-cadherin and overexpression of mesenchymal markers (N-cadherin, vimentin) and inflammatory cytokines (IL-8, IL-6, IL-1β, TNF-α, platelet-derived growth factor subunit B (PDGF-B), VEGF, epidermal growth protein (EGF), granulocyte-macrophage colony-stimulating factor (GM-CSF), and monocyte chemoattractant protein 1 (MCP-1). High concentrations of IL-15 secreted by gastric cancer MSCs contribute to tumor cell metastasis; increased IL-17 levels promote gastric cancer invasiveness [299,300].
Increased expression of SOX4 induces EMT via a release of TGF-β and contributes to the development of stem cell characteristics of gastric cancer cells [301]. Furthermore, CSCs, which display mesenchymal phenotypes, overexpress EMT markers such as Twist, Snail, or ZEB [302]. CagA-positive H. pylori infection induces EMT, and CSCs feature in gastric mucosal cells via overexpression of the Wnt/β-catenin signaling pathway [137]. The progression of CSCs is stimulated by EMT-related CD44+ cells’ emergence [303,304,305,306,307]. It was hypothesized that overexpression of the regulator of G-protein signaling pathway 1 (RGS1) might promote the transition of stem cells into CSCs [308]. Besides, CSCs are involved in EMT progression via a vast number of mechanisms, including an overactivation of KRAS, STAT3, Rac1, Wnt, Notch, PTEN, ERK, NF-κB signaling pathways, or hypoxic microenvironment [309,310,311,312,313,314,315,316,317,318]. Recently, researchers have proposed the role of CSC-associated protein, leucine-rich repeat and immunoglobulin-like domain-containing nogo receptor-interacting protein 2 (LINGO2), in gastric cancer and EMT initiation [319].
12. Conclusions
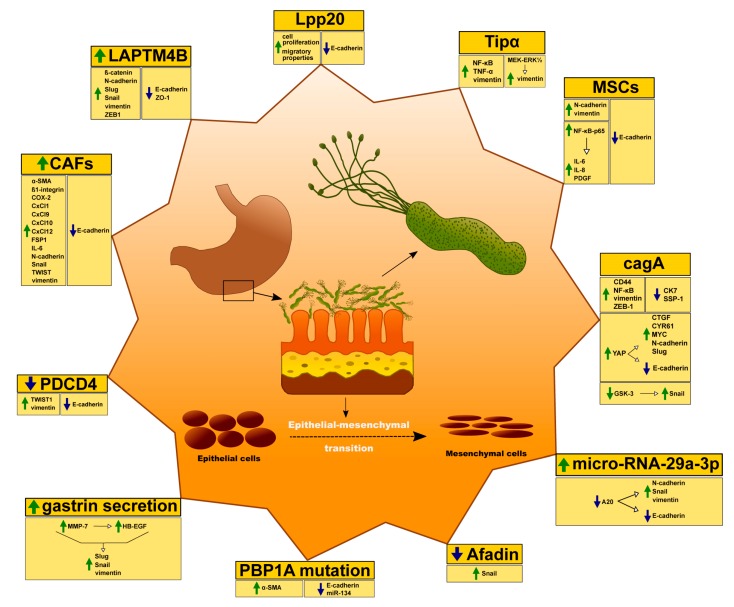
The association between H. pylori infection and gastric carcinogenesis remains controversial. In fact, some mechanisms are yet not fully understood. H. pylori infection seems to play an important role in terms of EMT induction within gastric mucosa (Figure 2).
Figure 2.
Possible mechanisms of the association between H. pylori infection and EMT.
The severity and progression of gastric cancer depends on the presence of specific H. pylori virulence factors. Likewise, cellular components that are associated with EMT progression can be influenced by H. pylori infection (Table 1). EMT and its progression depend on the particular strain of H. pylori along with its properties and virulence factors (Table 1). Specific strains may promote EMT with various intensity, thus influencing the eventual outcome of gastric cancer differently. Even though most known virulence factors, along with cellular components and their mechanisms of action, have been studied, more research should be performed to investigate the relationships between those factors, as well as to search for unknown processes and aspects. Notwithstanding, there is potential for further pharmacological research since all virulence factors constitute potential molecular targets for new medications. This may eventually provide new treatment strategies for gastric cancer, along with the possible eradication of H. pylori during the early stages of infection, which could significantly decrease the number of gastric cancer incidents.
Table 1.
Virulence factors and cellular components associated with EMT and H. pylori infection.
| Factors | Increase | Decrease |
|---|---|---|
| Afadin | actin stress fibers; Snail | ND |
| CAFs | α-SMA; Collagen I; Collagen III; COX-2; FAP; FGF-2; FSP1; HGF; HIF-1α; IL-6; IL-8; Integrin β-1; N-cadherin; SDF-1; Snail; TGF-β; TNC; TWIST; VEGF; vimentin | Bcl-2; Ki67 |
| CagA | CD44; Snail 1; vimentin; ZEB1 | CK7; SSP-1 |
| CagA & YAP pathway | CTGF; CYR61; MYC; N-cadherin; Slug; | E-cadherin |
| HB-EGF & MMP-7 | AP-1; NF-κB; Slug; Snail; vimentin | ND |
| LAPTM4B | β-catenin; N-cadherin; Slug; Snail; vimentin; ZEB1 | E-cadherin; ZO-1 |
| Lpp20 | ND | E-cadherin |
| miR-29a-3p | N-cadherin; Snail; vimentin | A20 gene; E-cadherin |
| MSCs | EGF; GM-CSF; IL-1β; IL-6; IL-8; MCP-1; N-cadherin; PDGF-B; TNF-α; VEGF; vimentin | E-cadherin |
| PBP1A mutation | α-SMA; FoxM1 | E-cadherin; miR-134 |
| PDCD4 | Twist1; vimentin | E-cadherin |
| Tipα | Ccl2; Ccl7; Ccl20; Cxcl1; Cxcl2; Cxcl5; Cxcl10; IL-1β; IL-6/STAT3 pathway; IL-8; N-cadherin; NF-κB; TNF-α; vimentin | E-cadherin |
ND—no data.
Author Contributions
All authors (J.B., I.K.-G., A.F., A.M., E.S., M.R.-H., E.R., P.P.) took part in writing, reviewing, preparing figure and table. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The author declares no conflict of interest.
Abbrevations
| α-SMA | α-smooth muscle actin |
| AMPK | AMP-activated protein kinase |
| AP-1 | Activator protein 1 |
| AREG | amphiregulin |
| Bcl-2 | B-cell lymphoma 2 |
| CAFs | cancer associated fibroblasts |
| CagA | cytotoxin-associated gene A |
| cagPAI | cag pathogenicity island |
| Ccl2 | chemokine (C-C motif) ligand 2 |
| Ccl20 | chemokine (C-C motif) ligand 20 |
| Ccl7 | chemokine (C-C motif) ligand 7 |
| CK7 | cytokeratin 7 |
| COX-2 | cyclooxygenase-2 |
| CSC | cancer stem-cell |
| CTGF | connective tissue growth factor |
| Cxc11 | C-X-C motif chemokine 11 |
| Cxcl1 | chemokine (C-X-C motif) ligand 1 |
| Cxcl10 | C-X-C motif chemokine 10 |
| Cxcl12 | stromal cell-derived factor 1 |
| Cxcl2 | chemokine (C-X-C motif) ligand 2 |
| Cxcl5 | C-X-C motif chemokine 5 |
| Cxcl9 | chemokine (C-X-C motif) ligand 9 |
| CYR61 | cysteine-rich angiogenic inducer 61 |
| DupA | duodenal ulcer promoting gene A |
| EGF | epidermal growth protein |
| EGFR | epidermal growth factor receptor |
| eIF4A | eukaryotic initiation factor-4A |
| eIF4G | eukaryotic translation initiation factor 4 G |
| EMT | epithelial–mesenchymal transition |
| EphA2 | erythropoietin-producing hepatocellular A2 receptor |
| ERK-1/2 | extracellular regulated kinases ½ |
| FAP | fibroblast activation protein |
| FGF9 | fibroblast growth factor 9 |
| FGF | fibroblast growth factor |
| FSP | fibroblast surface protein |
| FSP1 | fibroblast-specific protein 1 |
| GM-CSF | granulocyte-macrophage colony-stimulating factor |
| GOLPH3 | Golgi phosphoprotein 3 |
| GSK-3 | glycogen synthase kinase 3 |
| HB-EGF | heparin-binding epidermal growth factor |
| HGF | hepatocyte growth factor |
| HIF1α | hypoxia inducible factor 1α |
| hucMSCs | human umbilical cord MSCs |
| Il-6 | interleukin-6 |
| IL-8 | interleukin-8 |
| JNK | c-Jun N-terminal kinase |
| LAPTM4B | lysosomal-associated protein transmembrane 4β |
| LATS2 | large tumor suppressor 2 |
| MCP-1 | monocyte chemoattractant protein 1 |
| miRNA | microRNA |
| MMP-7 | matrix metalloproteinase-7 |
| MNNG | N-nitrosoguanidine |
| MSCs | mesenchymal stem cells |
| NANOGP8 | Nanog Homebox Retrogene P8 |
| NAP | neutrophil activating protein A |
| NF-κB | nuclear factor κB |
| OipA | outer inflammatory protein A |
| PBP | penicillin–binding protein |
| PDCD4 | programmed cell death protein 4 |
| PDGF-B | platelet-derived growth factor subunit B |
| PTEN | phosphatase and tensin homolog |
| SabA | sialic acid-binding adhesin |
| SDF-1 | stromal cell-derived factor 1 |
| SHP-2 | protein tyrosine phosphatase 2 |
| SSP-1 | osteopontin |
| T4SS | type 4 secretion system |
| TGF-α | transforming growth factor-α |
| TGF-β | transforming growth factor β |
| Tipα protein | tumor necrosis factor- α-inducing protein |
| TNF-α | tumor necrosis factor-α |
| TNC | tenascin-C |
| TRAIL1R | Trail receptor 1, death receptor 4 |
| VacA | vacuolating cytotoxin |
| VEGF | vascular endothelial factor |
| WT | wild-type |
| YAP | Yes-Associated-Protein |
| ZEB1 | zinc finger E-box binding homeobox 1 |
| ZO-1 | zonula occludens-1 |
References
- 1.Correia M., Machado J.C., Ristimäki A. Basic Aspects of Gastric Cancer. Helicobacter. 2009;14:36–40. doi: 10.1111/j.1523-5378.2009.00696.x. [DOI] [PubMed] [Google Scholar]
- 2.Zamani M., Ebrahimtabar F., Zamani V., Miller W.H., Alizadeh-Navaei R., Shokri-Shirvani J., Derakhshan M.H. Systematic review with meta-Analysis: The worldwide prevalence of Helicobacter pylori infection. Aliment. Pharmacol. Ther. 2018;47:868–876. doi: 10.1111/apt.14561. [DOI] [PubMed] [Google Scholar]
- 3.Hathroubi S., Servetas S.L., Windham I., Merrell D.S., Ottemann K.M. Helicobacter pylori Biofilm Formation and Its Potential Role in Pathogenesis. Microbiol. Mol. Biol. Rev. 2018;82:e00001-18. doi: 10.1128/MMBR.00001-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ferreira A.C., Isomoto H., Moriyama M., Fujioka T., Machado J.C., Yamaoka Y. Helicobacterand Gastric Malignancies. Helicobacter. 2008;13:28–34. doi: 10.1111/j.1523-5378.2008.00633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mazaheri Assadi M., Chamanrokh P., Whitehouse C.A., Huq A. Methods for Detecting the Environmental Coccoid Form of Helicobacter pylori. Front. Public Health. 2015;3:1–8. doi: 10.3389/fpubh.2015.00147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rajilic-Stojanovic M., Figueiredo C., Smet A., Hansen R., Kupcinskas J., Rokkas T., Andersen L., Machado J.C., Ianiro G., Gasbarrini A., et al. Systematic review: Gastric microbiota in health and disease. Aliment. Pharmacol. Ther. 2020;51:582–602. doi: 10.1111/apt.15650. [DOI] [PubMed] [Google Scholar]
- 7.Morais S., Costa A.R., Ferro A., Lunet N., Peleteiro B. Contemporary migration patterns in the prevalence of Helicobacter pylori infection: A systematic review. Helicobacter. 2017;22:1–11. doi: 10.1111/hel.12372. [DOI] [PubMed] [Google Scholar]
- 8.Chojnacki C., Popławski T., Błońska A., Błasiak J., Romanowski M., Chojnacki J. Expression of tryptophan hydroxylase in gastric mucosa in symptomatic and asymptomatic Helicobacter pylori infection. Arch. Med. Sci. 2019;15:416–423. doi: 10.5114/aoms.2018.76928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Seta T., Takahashi Y., Noguchi Y., Shikata S., Sakai T., Sakai K., Yamashita Y., Nakayama T. Effectiveness of Helicobacter pylori eradication in the prevention of primary gastric cancer in healthy asymptomatic people: A systematic review and meta-analysis comparing risk ratio with risk difference. PLoS ONE. 2017;12:1–18. doi: 10.1371/journal.pone.0183321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Figueiredo C., Costa S., Karameris A., Machado J.C. Pathogenesis of Gastric Cancer. Helicobacter. 2015;20:30–35. doi: 10.1111/hel.12254. [DOI] [PubMed] [Google Scholar]
- 11.Resende C., Regalo G., Durães C., Pinto M.T., Wen X., Figueiredo C., Carneiro F., Machado J.C. Interleukin-1B signalling leads to increased survival of gastric carcinoma cells through a CREB-C/EBPβ-Associated mechanism. Gastric Cancer. 2015;19:74–84. doi: 10.1007/s10120-014-0448-x. [DOI] [PubMed] [Google Scholar]
- 12.Costa A.M., Leite M., Seruca R., Figueiredo C. Adherens junctions as targets of microorganisms: A focus onHelicobacter pylori. FEBS Lett. 2012;587:259–265. doi: 10.1016/j.febslet.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 13.Costa A.C., Figueiredo C., Touati E. Pathogenesis of Helicobacter pylori Infection. Helicobacter. 2009;1:15–20. doi: 10.1111/j.1523-5378.2009.00702.x. [DOI] [PubMed] [Google Scholar]
- 14.Yamaoka Y., Graham D.Y. Helicobacter pylori virulence and cancer pathogenesis. Future Oncol. 2014;10:1487–1500. doi: 10.2217/fon.14.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kao C.-Y., Sheu B.-S., Wu J.-J. Helicobacter pylori infection: An overview of bacterial virulence factors and pathogenesis. Biomed. J. 2016;39:14–23. doi: 10.1016/j.bj.2015.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kabamba E.T., Yamaoka Y. Helicobacter pylori and Related Virulence Factors for Gastrointestinal Diseases. In: Shiotani A., editor. Gastric Cancer. Springer; Singapore: 2018. pp. 31–50. [Google Scholar]
- 17.Pormohammad A., Ghotaslou R., Leylabadlo H.E., Nasiri M.J., Dabiri H., Hashemi A. Risk of gastric cancer in association with Helicobacter pylori different virulence factors: A systematic review and meta-Analysis. Microb. Pathog. 2018;118:214–219. doi: 10.1016/j.micpath.2018.03.004. [DOI] [PubMed] [Google Scholar]
- 18.Sgouras D., Tegtmeyer N., Wessler S. Advances in Experimental Medicine and Biology. Kluwer Academic Publishers; Boston, MA, USA: 2019. Activity and Functional Importance of Helicobacter pylori Virulence Factors. [DOI] [PubMed] [Google Scholar]
- 19.Olivera-Severo D., Uberti A.F., Marques M.S., Pinto M.T., Gomez-Lazaro M., Figueiredo C., Leite M., Carlini C.R. A New Role for Helicobacter pylori Urease: Contributions to Angiogenesis. Front. Microbiol. 2017;8:1883. doi: 10.3389/fmicb.2017.01883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ferreira R.M., Machado J.C., Figueiredo C. Clinical relevance of Helicobacter pylori vacA and cagA genotypes in gastric carcinoma. Best Pract. Res. Clin. Gastroenterol. 2014;28:1003–1015. doi: 10.1016/j.bpg.2014.09.004. [DOI] [PubMed] [Google Scholar]
- 21.Guimarães N.M., Azevedo N.F., Vieira M.J., Figueiredo C. Water-Induced modulation of Helicobacter pylori virulence properties. Memórias Inst. Oswaldo Cruz. 2014;109:414–419. doi: 10.1590/0074-0276140024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ferreira R.M., Figueiredo C., Bonet C., Pardo M.L., Liso J.M.R., Alonso P., Sala N., Capella G., Sanz-Anquela J.M., Gonzalez C.A. Helicobacter pylori vacA Intermediate Region Genotyping and Progression of Gastric Preneoplastic Lesions. Am. J. Gastroenterol. 2012;107:145–146. doi: 10.1038/ajg.2011.389. [DOI] [PubMed] [Google Scholar]
- 23.Oliveira M.J., Costa A.M., Costa A.C., Machado J.C., Seruca R., Mareel M., Figueiredo C. 26 E-Cadherin and CagA Associate in a Tetrameric Complex That Suppresses Helicobacter pylori-Mediated Cell Invasion. Gastroenterology. 2008;134:A-3. doi: 10.1016/S0016-5085(08)60022-0. [DOI] [Google Scholar]
- 24.Peleteiro B., Lunet N., Figueiredo C., Carneiro F., David L., Barros H. Smoking, Helicobacter pylori Virulence, and Type of Intestinal Metaplasia in Portuguese Males. Cancer Epidemiol. Biomark. Prev. 2007;16:322–326. doi: 10.1158/1055-9965.EPI-06-0885. [DOI] [PubMed] [Google Scholar]
- 25.Choi I.J., Kook M.-C., Kim Y.-I., Cho S.-J., Lee J.Y., Kim C.G., Park B., Nam B.H. Helicobacter pylori Therapy for the Prevention of Metachronous Gastric Cancer. N. Engl. J. Med. 2018;378:1085–1095. doi: 10.1056/NEJMoa1708423. [DOI] [PubMed] [Google Scholar]
- 26.Amieva M., Peek R.M. Pathobiology of Helicobacter pylori–Induced Gastric Cancer. Gastroenterology. 2016;150:64–78. doi: 10.1053/j.gastro.2015.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Machado A.M.D., Desler C., Bøggild S., Strickertsson J.A., Friis-Hansen L., Figueiredo C., Seruca R., Rasmussen L.J. Helicobacter pylori infection affects mitochondrial function and DNA repair, thus, mediating genetic instability in gastric cells. Mech. Ageing Dev. 2013;134:460–466. doi: 10.1016/j.mad.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 28.Leite M., Marques M.S., Melo J., Pinto M.T., Cavadas B., Aroso M., Gomez-Lazaro M., Seruca R., Figueiredo C. Helicobacter Pylori Targets the EPHA2 Receptor Tyrosine Kinase in Gastric Cells Modulating Key Cellular Functions. Cells. 2020;9:513. doi: 10.3390/cells9020513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sitarz R., Skierucha M., Mielko J., Offerhaus J., Maciejewski R., Polkowski W. Gastric cancer: Epidemiology, prevention, classification, and treatment. Cancer Manag. Res. 2018;10:239–248. doi: 10.2147/CMAR.S149619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pinto-Ribeiro I., Ferreira R., Batalha S., Hlaing T., Wong S., Carneiro F., Figueiredo C. Helicobacter pylori vacA Genotypes in Chronic Gastritis and Gastric Carcinoma Patients from Macau, China. Toxins. 2016;8:142. doi: 10.3390/toxins8050142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yanovich O., Doroshko M., Titov L. Helicobacter pylori genotypes among Belarus patients with gastroduodenal disorders and their association with clinical outcome. Acta Microbiol. Immunol. Hung. 2019;66:399–411. doi: 10.1556/030.66.2019.016. [DOI] [PubMed] [Google Scholar]
- 32.Hnatyszyn A., Szalata M., Skrzypczak-Zielinska M., Wielgus K., Stanczyk J., Dziuba I., Mikstacki A., Dobrowolska A., Waszak M., Hnatyszyn P.T., et al. DNA Variants in Helicobacter Pylori Infected Patients with Chronic Gastritis, Dysplasia and Gastric Cancer. Adv. Med. Sci. 2019;64:79–84. doi: 10.1016/j.advms.2018.12.002. [DOI] [PubMed] [Google Scholar]
- 33.Kakelar H.M., Barzegari A., Dehghani J., Hanifian S., Saeedi N., Barar J., Omidi Y. Pathogenicity of Helicobacter pylori in cancer development and impacts of vaccination. Gastric Cancer. 2018;22:23–36. doi: 10.1007/s10120-018-0867-1. [DOI] [PubMed] [Google Scholar]
- 34.Figueiredo C., Machado J.C., Pharoah P., Seruca R., Sousa S., Carvalho R., Capelinha A.F., Quint W., Caldas C., van Doorn L.J., et al. Helicobacter pylori and interleukin 1 genotyping: An opportunity to identify high-Risk individuals for gastric carcinoma. JNCI J. Natl. Cacncer Inst. 2002;94:1680–1687. doi: 10.1093/jnci/94.22.1680. [DOI] [PubMed] [Google Scholar]
- 35.Bakhti S.Z., Latifi-Navid S., Mohammadi S., Zahri S., Bakhti F.S., Feizi F., Yazdanbod A., Siavoshi F. Relevance ofHelicobacter pylori vacA 3’-End Region Polymorphism to Gastric Cancer. Helicobacter. 2015;21:305–316. doi: 10.1111/hel.12284. [DOI] [PubMed] [Google Scholar]
- 36.Marcos-Pinto R., Dinis-Ribeiro M.J., Carneiro F., Machado J.C., Figueiredo C., Wen X., Reis C.A., Ferreira R.M., Lopes C., Ferreira J., et al. Mo1556 High-Risk Host Genotype and H. pylori Strains in First Degree Relatives of Patients with Early-Onset Gastric Cancer. Gastroenterology. 2012;142:S-627–S-628. doi: 10.1016/S0016-5085(12)62411-1. [DOI] [Google Scholar]
- 37.González C.A., Figueiredo C., Lic B.C., Ferreira R.M., Pardo M.L., Liso R.J.M., Alonso P., Sala N., Capella G., Sanz-Anquela J.M. Helicobacter pylori cagA and vacA Genotypes as Predictors of Progression of Gastric Preneoplastic Lesions: A Long-Term Follow-Up in a High-Risk Area in Spain. Am. J. Gastroenterol. 2011;106:867–874. doi: 10.1038/ajg.2011.1. [DOI] [PubMed] [Google Scholar]
- 38.Machado A.M.D., Figueiredo C., Seruca R., Rasmussen L.J. Helicobacter pylori infection generates genetic instability in gastric cells. Biochim. Biophys. Acta Rev. Cancer. 2010;1806:58–65. doi: 10.1016/j.bbcan.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 39.Figueiredo C., Quint W., Nouhan N., Munckhof H.V.D., Herbrink P., Scherpenisse J., de Boer W., Schneeberger P., Perez-Perez G., Blaser M.J., et al. Assessment of Helicobacter pylori vacA and cagA Genotypes and Host Serological Response. J. Clin. Microbiol. 2001;39:1339–1344. doi: 10.1128/JCM.39.4.1339-1344.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nogueira C., Figueiredo C., Carneiro F., Gomes A.T., Barreira R., Figueira P., Salgado C., Belo L., Peixoto A., Bravo J.C., et al. Helicobacter pylori Genotypes May Determine Gastric Histopathology. Am. J. Pathol. 2001;158:647–654. doi: 10.1016/S0002-9440(10)64006-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Watari J. Helicobacter pyloriassociated chronic gastritis, clinical syndromes, precancerous lesions, and pathogenesis of gastric cancer development. World J. Gastroenterol. 2014;20:5461. doi: 10.3748/wjg.v20.i18.5461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lanas A., Chan F.K.L. Peptic ulcer disease. Lancet. 2017;390:613–624. doi: 10.1016/S0140-6736(16)32404-7. [DOI] [PubMed] [Google Scholar]
- 43.Thieblemont C., Zucca E. Clinical aspects and therapy of gastrointestinal MALT lymphoma. Best Pract. Res. Clin. Haematol. 2017;30:109–117. doi: 10.1016/j.beha.2017.01.002. [DOI] [PubMed] [Google Scholar]
- 44.Potamitis G.S., Axon A.T.R. Helicobacter pylori and Nonmalignant Diseases. Helicobacter. 2015;20:26–29. doi: 10.1111/hel.12253. [DOI] [PubMed] [Google Scholar]
- 45.Ferreira R.M., Pereira-Marques J., Pinto-Ribeiro I., Costa J.L., Carneiro F., Machado J.C., Figueiredo C. Gastric microbial community profiling reveals a dysbiotic cancer-associated microbiota. Gut. 2017;67:226–236. doi: 10.1136/gutjnl-2017-314205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Puculek M., Machlowska J., Wierzbicki R., Baj J., Maciejewski R., Sitarz R. Helicobacter pylori associated factors in the development of gastric cancer with special reference to the early-Onset subtype. Oncotarget. 2018;9:31146–31162. doi: 10.18632/oncotarget.25757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Jamkhande P.G., Gattani S.G., Farhat S.A. Helicobacter pylori and cardiovascular complications: A mechanism based review on role of Helicobacter pylori in cardiovascular diseases. Integr. Med. Res. 2016;5:244–249. doi: 10.1016/j.imr.2016.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bazmamoun H., Rafeey M., Nikpouri M., Ghergherehchi R. Helicobacter Pylori Infection in Children with Type 1 Diabetes Mellitus: A Case-Control Study. J. Res. Health Sci. 2016;16:68–71. [PMC free article] [PubMed] [Google Scholar]
- 49.Mortazavi E., Eslami B., Aghahosseini P., Ahron F., Amininejad A., Mahmoodi S., Satarpour H., Radmanesh N., Rassi H. Association of Mannose-Binding Lectin rs1800450 and Tumor Necrotic Factor-α rs1800620 Polymorphism with Helicobacter pylori in Type II Diabetes Mellitus. Monoclon. Antibodies Immunodiagn. Immunother. 2017;36:236–241. doi: 10.1089/mab.2017.0039. [DOI] [PubMed] [Google Scholar]
- 50.Doulberis M., Kotronis G., Thomann R., Polyzos S.A., Boziki M., Gialamprinou D., Deretzi G., Katsinelos P., Kountouras J. Review: Impact of Helicobacter pylori on Alzheimer’s disease: What do we know so far? Helicobacter. 2018;23:1–18. doi: 10.1111/hel.12454. [DOI] [PubMed] [Google Scholar]
- 51.Ribatti D. Epithelial-Mesenchymal transition in morphogenesis, cancer progression and angiogenesis. Exp. Cell Res. 2017;353:1–5. doi: 10.1016/j.yexcr.2017.02.041. [DOI] [PubMed] [Google Scholar]
- 52.Acloque H., Adams M.S., Fishwick K., Bronner-Fraser M., Nieto M.A. Epithelial-Mesenchymal transitions: The importance of changing cell state in development and disease. J. Clin. Investig. 2009;119:1438–1449. doi: 10.1172/JCI38019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Diepenbruck M., Christofori G. Epithelial–Mesenchymal transition (EMT) and metastasis: Yes, no, maybe? Curr. Opin. Cell Biol. 2016;43:7–13. doi: 10.1016/j.ceb.2016.06.002. [DOI] [PubMed] [Google Scholar]
- 54.Campbell K. Contribution of epithelial-Mesenchymal transitions to organogenesis and cancer metastasis. Curr. Opin. Cell Biol. 2018;55:30–35. doi: 10.1016/j.ceb.2018.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chen T., You Y., Jiang H., Wang Z.Z. Epithelial-Mesenchymal transition (EMT): A biological process in the development, stem cell differentiation, and tumorigenesis. J. Cell. Physiol. 2017;232:3261–3272. doi: 10.1002/jcp.25797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wong S.H.M., Fang C.M., Chuah L.-H., Leong C.O., Ngai S.C. E-Cadherin: Its dysregulation in carcinogenesis and clinical implications. Crit. Rev. Oncol. Hematol. 2018;121:11–22. doi: 10.1016/j.critrevonc.2017.11.010. [DOI] [PubMed] [Google Scholar]
- 57.Muhammad N., Bhattacharya S., Steele R., Phillips N., Ray R.B. Involvement of c-Fos in the Promotion of Cancer Stem-Like Cell Properties in Head and Neck Squamous Cell Carcinoma. Clin. Cancer Res. 2016;23:3120–3128. doi: 10.1158/1078-0432.CCR-16-2811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gugnoni M., Sancisi V., Gandolfi G., Manzotti G., Ragazzi M., Giordano D., Tamagnini I., Tigano M., Frasoldati A., Piana S., et al. Cadherin-6 promotes EMT and cancer metastasis by restraining autophagy. Oncogene. 2016;36:667–677. doi: 10.1038/onc.2016.237. [DOI] [PubMed] [Google Scholar]
- 59.Shi L., Wang Y., Lu Z., Zhang H., Zhuang N., Wang B., Song Z., Chen G., Huang C., Xu D., et al. miR-127 promotes EMT and stem-Like traits in lung cancer through a feed-Forward regulatory loop. Oncogene. 2016;36:1631–1643. doi: 10.1038/onc.2016.332. [DOI] [PubMed] [Google Scholar]
- 60.Xiao H. MiR-7-5p suppresses tumor metastasis of non-Small cell lung cancer by targeting NOVA2. Cell. Mol. Biol. Lett. 2019;24:1–13. doi: 10.1186/s11658-019-0188-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zheng X., Carstens J.L., Kim J., Scheible M., Kaye J., Sugimoto H., Wu C.C., LeBleu V.S., Kalluri R. Epithelial-To-Mesenchymal transition is dispensable for metastasis but induces chemoresistance in pancreatic cancer. Nature. 2015;527:525–530. doi: 10.1038/nature16064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Choi Y.J., Kim N., Chang H., Lee H.S., Park S.M., Park J.H., Shin C.M., Kim J.M., Kim J.S., Lee D.H., et al. Helicobacter pylori-induced epithelial-Mesenchymal transition, a potential role of gastric cancer initiation and an emergence of stem cells. Carcinogenesis. 2015;36:553–563. doi: 10.1093/carcin/bgv022. [DOI] [PubMed] [Google Scholar]
- 63.Teeuwssen F. Wnt Signaling in Ovarian Cancer Stemness, EMT, and Therapy Resistance. J. Clin. Med. 2019;8:1658. doi: 10.3390/jcm8101658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhang Y., Zhang J., Liang S., Lang G., Liu G., Liu P., Deng X. Long non-Coding RNA VIM-AS1 promotes prostate cancer growth and invasion by regulating epithelial-Mesenchymal transition. JBUON. 2019;24:2090–2098. [PubMed] [Google Scholar]
- 65.Scimeca M., Bonfiglio R., Menichini E., Albonici L., Urbano N., Caro M.T.D., Mauriello A., Schillaci O., Gambacurta A., Bonanno E. Microcalcifications Drive Breast Cancer Occurrence and Development by Macrophage-Mediated Epithelial to Mesenchymal Transition. Int. J. Mol. Sci. 2019;20:5633. doi: 10.3390/ijms20225633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Scimeca M., Antonacci C., Colombo D., Bonfiglio R., Buonomo O.C., Bonanno E. Emerging prognostic markers related to mesenchymal characteristics of poorly differentiated breast cancers. Tumor Biol. 2015;37:5427–5435. doi: 10.1007/s13277-015-4361-7. [DOI] [PubMed] [Google Scholar]
- 67.Carneiro P., Fernandes M.S., Figueiredo J., Caldeira J., Carvalho J., Pinheiro H., Leite M., Melo S., Oliveira P., Simoes-Correia J., et al. E-Cadherin dysfunction in gastric cancer-Cellular consequences, clinical applications and open questions. FEBS Lett. 2012;586:2981–2989. doi: 10.1016/j.febslet.2012.07.045. [DOI] [PubMed] [Google Scholar]
- 68.Paredes J., Figueiredo J., Albergaria A., Oliveira P., Carvalho J., Ribeiro A.S., Caldeira J., Costa A.M., Simoes-Correia J., Oliveira M.J., et al. Epithelial E- and P-Cadherins: Role and clinical significance in cancer. Biochim. Biophys. Acta Rev. Cancer. 2012;1826:297–311. doi: 10.1016/j.bbcan.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 69.Wang Y., Shi J., Chai K., Ying X., Zhou B. The Role of Snail in EMT and Tumorigenesis. Curr. Cancer Drug Targets. 2013;13:963–972. doi: 10.2174/15680096113136660102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Buhrmann C., Yazdi M., Popper B., Kunnumakkara A.B., Aggarwal B.B., Shakibaei M. Induction of the Epithelial-to-Mesenchymal Transition of Human Colorectal Cancer by Human TNF-β (Lymphotoxin) and its Reversal by Resveratrol. Nutrients. 2019;11:704. doi: 10.3390/nu11030704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Liu Y., Sun X., Feng J., Deng L.-L., Liu Y., Li B., Zhu M., Lu C., Zhou L. MT2-MMP induces proteolysis and leads to EMT in carcinomas. Oncotarget. 2016;7:48193. doi: 10.18632/oncotarget.10194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kim W.K., Kwon Y., Jang M., Park M., Kim J., Cho S., Jang D.G., Lee W.B., Jung S.H., Choi H.J., et al. β-Catenin activation down-regulates cell-Cell junction-Related genes and induces epithelial-To-Mesenchymal transition in colorectal cancers. Sci. Rep. 2019;9:1–15. doi: 10.1038/s41598-019-54890-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tan J., Zhang X., Xiao W., Liu X., Li C., Guo Y., Xiong W., Li Y. N3ICD with the transmembrane domain can effectively inhibit EMT by correcting the position of tight/adherens junctions. Cell Adhes. Migr. 2019;13:203–218. doi: 10.1080/19336918.2019.1619958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yang J., Weinberg R.A. Epithelial-Mesenchymal Transition: At the Crossroads of Development and Tumor Metastasis. Dev. Cell. 2008;14:818–829. doi: 10.1016/j.devcel.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 75.Qie S., Diehl J.A. Cyclin D1, cancer progression, and opportunities in cancer treatment. J. Mol. Med. 2016;94:1313–1326. doi: 10.1007/s00109-016-1475-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Geng B., Pan J., Zhao T., Ji J., Zhang C., Che Y., Yang J., Shi H., Li J., Zhou H., et al. Chitinase 3-like 1-CD44 interaction promotes metastasis and epithelial-To-Mesenchymal transition through β-Catenin/Erk/Akt signaling in gastric cancer. J. Exp. Clin. Cancer Res. 2018;37:208. doi: 10.1186/s13046-018-0876-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Yu W., Li L., Zheng F., Yang W., Zhao S., Tian C., Yin W., Chen Y., Guo W., Zou L., et al. β-Catenin Cooperates with CREB Binding Protein to Promote the Growth of Tumor Cells. Cell. Physiol. Biochem. 2017;44:467–478. doi: 10.1159/000485013. [DOI] [PubMed] [Google Scholar]
- 78.Shang S., Hua F., Hu Z.-W. The regulation of β-Catenin activity and function in cancer: Therapeutic opportunities. Oncotarget. 2017;8:33972–33989. doi: 10.18632/oncotarget.15687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Shi J., Wu Y.-X., Yu J.-H., Chen X., Luo X.-J., Yin Y.-R. Research of the Relationship Between β-Catenin and C-Myc-Mediated Wnt Pathway and Laterally Spreading Tumors Occurrence. Eur. Rev. Med. Pharmacol. Sci. 2017;21:252–257. [PubMed] [Google Scholar]
- 80.Suarez-Carmona M., Lesage J., Cataldo D., Gilles C. EMT and inflammation: Inseparable actors of cancer progression. Mol. Oncol. 2017;11:805–823. doi: 10.1002/1878-0261.12095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Liu X., Fan D. The Epithelial-Mesenchymal Transition and Cancer Stem Cells: Functional and Mechanistic Links. Curr. Pharm. Des. 2015;21:1279–1291. doi: 10.2174/1381612821666141211115611. [DOI] [PubMed] [Google Scholar]
- 82.Giancotti F.G. Mechanisms Governing Metastatic Dormancy and Reactivation. Cell. 2013;155:750–764. doi: 10.1016/j.cell.2013.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Begicevic R.-R., Falasca M. ABC Transporters in Cancer Stem Cells: Beyond Chemoresistance. Int. J. Mol. Sci. 2017;18:2362. doi: 10.3390/ijms18112362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ma H.-Y., Liu X.-Z., Liang C.-M. Inflammatory microenvironment contributes to epithelial-Mesenchymal transition in gastric cancer. World J. Gastroenterol. 2016;22:6619. doi: 10.3748/wjg.v22.i29.6619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Baj J., Brzozowska K., Forma A., Maani A., Sitarz E., Portincasa P. Immunological Aspects of the Tumor Microenvironemnt and Epithelial-Mesenchymal Transition in Gastric Carcinogenesis. Int. J. Mol. Sci. 2020;21:2544. doi: 10.3390/ijms21072544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Singh S., Chakrabarti R. Consequences of EMT-Driven Changes in the Immune Microenvironment of Breast Cancer and Therapeutic Response of Cancer Cells. J. Clin. Med. 2019;8:642. doi: 10.3390/jcm8050642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Soundararajan R., Fradette J., Konen J., Moulder S., Zhang X., Gibbons D., Varadarajan N., Wistuba I.I., Tripathy D., Bernatchez C., et al. Targeting the Interplay between Epithelial-to-Mesenchymal-Transition and the Immune System for Effective Immunotherapy. Cancers. 2019;11:714. doi: 10.3390/cancers11050714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zakharchenko O., Cojoc M., Dubrovska A., Souchelnytskyi S. A Role of TGFß1 Dependent 14-3-3σ Phosphorylation at Ser69 and Ser74 in the Regulation of Gene Transcription, Stemness and Radioresistance. PLoS ONE. 2013;8:e65163. doi: 10.1371/journal.pone.0065163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zhang X., Zhang P., Shao M., Zang X., Zhang J., Mao F., Qian H., Xu W. SALL4 activates TGF-β/SMAD signaling pathway to induce EMT and promote gastric cancer metastasis. Cancer Manag. Res. 2018;10:4459–4470. doi: 10.2147/CMAR.S177373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lopez-Novoa J.M., Nieto M.A. Inflammation and EMT: An alliance towards organ fibrosis and cancer progression. EMBO Mol. Med. 2009;1:303–314. doi: 10.1002/emmm.200900043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Katoh M. Dysregulation of stem cell signaling network due to germline mutation, SNP, helicobacter pylori infection, epigenetic change, and genetic alteration in gastric cancer. Cancer Biol. Ther. 2007;6:832–839. doi: 10.4161/cbt.6.6.4196. [DOI] [PubMed] [Google Scholar]
- 92.Magalhães A., Marcos N.T., Carvalho A.S., David L., Figueiredo C., Bastos J., David G., Reis C.A. Helicobacter pylori cagpathogenicity island-Positive strains induce syndecan-4 expression in gastric epithelial cells. FEMS Immunol. Med. Microbiol. 2009;56:223–232. doi: 10.1111/j.1574-695X.2009.00569.x. [DOI] [PubMed] [Google Scholar]
- 93.Oliveira M.J., Costa A.C., Costa A.M., Henriques L., Suriano G., Atherton J.C., Machado J.C., Carneiro F., Seruca R., Mareel M., et al. Helicobacter pyloriInduces Gastric Epithelial Cell Invasion in a c-Met and Type IV Secretion System-dependent Manner. J. Biol. Chem. 2006;281:34888–34896. doi: 10.1074/jbc.M607067200. [DOI] [PubMed] [Google Scholar]
- 94.Figueiredo C., Machado J.C., Yamaoka Y. Pathogenesis of Helicobacter pylori Infection. Helicobacter. 2005;10:14–20. doi: 10.1111/j.1523-5378.2005.00339.x. [DOI] [PubMed] [Google Scholar]
- 95.Backert S., Neddermann M., Maubach G., Naumann M. Pathogenesis of Helicobacter pylori infection. Helicobacter. 2016;21:19–25. doi: 10.1111/hel.12335. [DOI] [PubMed] [Google Scholar]
- 96.Ferreira R.M., Machado J.C., Leite M., Carneiro F., Figueiredo C. The number of Helicobacter pylori CagA EPIYA C tyrosine phosphorylation motifs influences the pattern of gastritis and the development of gastric carcinoma. Histopathology. 2012;60:992–998. doi: 10.1111/j.1365-2559.2012.04190.x. [DOI] [PubMed] [Google Scholar]
- 97.Hu B., Khara P., Song L., Lin A.S., Frick-Cheng A.E., Harvey M.L., Cover T.L., Christie P.J. In situ molecular architecture of the helicobacter pylori cag type IV secretion system. mBio. 2019;10:1–15. doi: 10.1128/mBio.00849-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tegtmeyer N., Wessler S., Necchi V., Rohde M., Harrer A., Rau T.T., Asche C.I., Boehm M., Loessner H., Figueiredo C., et al. Helicobacter pylori Employs a Unique Basolateral Type IV Secretion Mechanism for CagA Delivery. Cell Host Microbe. 2017;22:552–560. doi: 10.1016/j.chom.2017.09.005. [DOI] [PubMed] [Google Scholar]
- 99.Zhang X., Zeng B., Wen C., Zheng S., Chen H., She F. YWHAE is a novel interaction partner of Helicobacter pylori CagA. FEMS Microbiol. Lett. 2018;365:1–7. doi: 10.1093/femsle/fnx231. [DOI] [PubMed] [Google Scholar]
- 100.Zhu S., Soutto M., Chen Z., Peng D.F., Romero-Gallo J., Krishna U.S., Belkhiri A., Washington M.K., Peek R., El-Rifai W. Helicobacter pylori-Induced cell death is counteracted by NF-κB-Mediated transcription of DARPP-32. Gut. 2016;66:802–812. doi: 10.1136/gutjnl-2016-312141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Lee M.H., Yang J.Y., Cho Y., Woo H.J., Kwon H.J., Kim D.H., Park M., Moon C., Yeon M.J., Kim H.W., et al. Inhibitory effects of menadione on Helicobacter pylori growth and helicobacter pylori-Induced inflammation via NF-κB inhibition. Int. J. Mol. Sci. 2019;20:1169. doi: 10.3390/ijms20051169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Roskoski R. ERK1/2 MAP kinases: Structure, function, and regulation. Pharm. Res. 2012;66:105–143. doi: 10.1016/j.phrs.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 103.Bessède E., Staedel C., Acuña Amador L.A., Nguyen P.H., Chambonnier L., Hatakeyama M., Belleannee G., Megraud F., Varon C. Helicobacter pylori generates cells with cancer stem cell properties via epithelial-Mesenchymal transition-Like changes. Oncogene. 2014;33:4123–4131. doi: 10.1038/onc.2013.380. [DOI] [PubMed] [Google Scholar]
- 104.Hayashi T., Senda M., Suzuki N., Nishikawa H., Ben C., Tang C., Nagase L., Inoue K., Senda T., Hatakeyama M. Differential Mechanisms for SHP2 Binding and Activation Are Exploited by Geographically Distinct Helicobacter pylori CagA Oncoproteins. Cell Rep. 2017;20:2876–2890. doi: 10.1016/j.celrep.2017.08.080. [DOI] [PubMed] [Google Scholar]
- 105.Nagase L., Hayashi T., Senda T., Hatakeyama M. Dramatic increase in SHP2 binding activity of Helicobacter pylori Western CagA by EPIYA-C duplication: Its implications in gastric carcinogenesis. Sci. Rep. 2015;5:1–13. doi: 10.1038/srep15749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lee D.G., Kim H.S., Lee Y.S., Kim S., Cha S.Y., Ota I., Kim N.H., Cha Y.H., Yand D.H., Lee Y., et al. Helicobacter pylori CagA promotes Snail-Mediated epithelial-Mesenchymal transition by reducing GSK-3 activity. Nat. Commun. 2014;5:1–13. doi: 10.1038/ncomms5423. [DOI] [PubMed] [Google Scholar]
- 107.Sougleri I.S., Papadakos K.S., Zadik M.P., Mavri-Vavagianni M., Mentis A.F., Sgouras D.N. Helicobacter pylori CagA protein induces factors involved in the epithelial to mesenchymal transition (EMT) in infected gastric epithelial cells in an EPIYA- Phosphorylation-Dependent manner. FEBS J. 2016;283:206–220. doi: 10.1111/febs.13592. [DOI] [PubMed] [Google Scholar]
- 108.Hashi K., Imai C., Yahara K., Tahmina K., Hayashi T., Azuma T., Miyabe-Nishiwaki T., Sato H., Matsuoka M., Niimi S., et al. Evaluating the origin and virulence of a Helicobacter pylori cagA-Positive strain isolated from a non-human primate. Sci. Rep. 2018;8:15981. doi: 10.1038/s41598-018-34425-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ferreira R.M., Machado J.C., Carneiro F., Figueiredo C. T1645 the Number of Helicobacter pylori cagA EPIYA C Tyrosine Phosphorylation Motifs Is Associated with Histopathological Features of Chronic Gastritis. Gastroenterology. 2009;136:A-549. doi: 10.1016/S0016-5085(09)62525-7. [DOI] [Google Scholar]
- 110.Ferreira R.M., Machado J.C., Carneiro F., Figueiredo C. T1801 Helicobacter pylori CagA EPIYA C Tyrosine Phosphorylation Motif Influences the Risk for Gastric Carcinoma Development. Gastroenterology. 2008;134:A-566. doi: 10.1016/S0016-5085(08)62642-6. [DOI] [Google Scholar]
- 111.Naumann M., Sokolova O., Tegtmeyer N., Backert S. Helicobacter pylori: A Paradigm Pathogen for Subverting Host Cell Signal Transmission. Trends Microbiol. 2017;25:316–328. doi: 10.1016/j.tim.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 112.Noto J.M., Zackular J.P., Varga M.G., Delgado A., Romero-gallo J., Scholz M.B. Crossm Modification of the Gastric Mucosal Microbiota by a Strain-Specific Helicobacter pylori Oncoprotein and Carcinogenic. mBio. 2019;10:e00955-19. doi: 10.1128/mBio.00955-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Oliveira M.J., Costa A.M., Costa A.C., Ferreira R.M., Sampaio P., Machado J.C. CagA Associates with c-Met, E-Cadherin, and p120-Catenin in a Multiproteic Complex that Suppresses Helicobacter pylori–Induced Cell-Invasive Phenotype. J. Infect. Dis. 2009;200:745–755. doi: 10.1086/604727. [DOI] [PubMed] [Google Scholar]
- 114.Nell S., Estibariz I., Krebes J., Bunk B., Graham D.Y., Overmann J., Song Y., Sproer C., Yang I., Wex T., et al. Genome and Methylome Variation in Helicobacter pylori With a cag Pathogenicity Island During Early Stages of Human Infection. Gastroenterology. 2018;154:612–623.e7. doi: 10.1053/j.gastro.2017.10.014. [DOI] [PubMed] [Google Scholar]
- 115.Li H., He C., Wang X., Wang H., Nan G., Fang L. MicroRNA-183 affects the development of gastric cancer by regulating autophagy via MALAT1-miR-183-SIRT1 axis and PI3K/AKT/mTOR signals. Artif. Cells Nanomed. Biotechnol. 2019;47:3163–3171. doi: 10.1080/21691401.2019.1642903. [DOI] [PubMed] [Google Scholar]
- 116.Li Y., Sun H., Guan J., Ji T., Wang X. Serum microRNA-381: A Potential Marker for Early Diagnosis of Gastric Cancer. Yonsei Med. J. 2019;60:720–726. doi: 10.3349/ymj.2019.60.8.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Mani S.A., Guo W., Liao M.J., Eaton E.N., Ayyanan A., Zhou A.Y., Brooks M., Reinhard F., Zhang C.C., Shipitsin M., et al. The Epithelial-Mesenchymal Transition Generates Cells with Properties of Stem Cells. Cell. 2008;133:704–715. doi: 10.1016/j.cell.2008.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Lee S.Y., Ju M.K., Jeon H.M., Lee Y.J., Kim C.H., Park H.G., Han S.I., Kang H.S. Oncogenic Metabolism Acts as a Prerequisite Step for Induction of Cancer Metastasis and Cancer Stem Cell Phenotype. Oxidative Med. Cell. Longev. 2018;2018:1–28. doi: 10.1155/2018/1027453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Dongre A., Weinberg R.A. New insights into the mechanisms of epithelial–Mesenchymal transition and implications for cancer. Nat. Rev. Mol. Cell Biol. 2018;20:69–84. doi: 10.1038/s41580-018-0080-4. [DOI] [PubMed] [Google Scholar]
- 120.Park A.H., Shin J.E., Park H.W. The role of Hippo Pathway in Cancer Stem Cell Biology. Mol. Cells. 2018;41:83–92. doi: 10.14348/molcells.2018.2242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zhou P., Li B., Liu F., Zhang M., Wang Q., Liu Y., Yao Y., Li D. The epithelial to mesenchymal transition (EMT) and cancer stem cells: Implication for treatment resistance in pancreatic cancer. Mol. Cancer. 2017;16:52. doi: 10.1186/s12943-017-0624-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Singh M., Yelle N., Venugopal C., Singh S.K. EMT: Mechanisms and therapeutic implications. Pharmacol. Ther. 2018;182:80–94. doi: 10.1016/j.pharmthera.2017.08.009. [DOI] [PubMed] [Google Scholar]
- 123.Pradella D., Naro C., Sette C., Ghigna C. EMT and stemness: Flexible processes tuned by alternative splicing in development and cancer progression. Mol. Cancer. 2017;16:8. doi: 10.1186/s12943-016-0579-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Houghton J. Gastric Cancer Originating from Bone Marrow-Derived Cells. Science. 2004;306:1568–1571. doi: 10.1126/science.1099513. [DOI] [PubMed] [Google Scholar]
- 125.Mentis A.-F.A., Boziki M., Grigoriadis N., Papavassiliou A.G. Helicobacter pylori infection and gastric cancer biology: Tempering a double-Edged sword. Cell. Mol. Life Sci. 2019;76:2477–2486. doi: 10.1007/s00018-019-03044-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Toh T.B., Lim J.J., Chow E.K.H. Epigenetics in cancer stem cells. Mol. Cancer. 2017;16:1–20. doi: 10.1186/s12943-017-0596-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Santos J.C., Carrasco-Garcia E., Garcia-Puga M., Aldaz P., Montes M., Fernandez-Reyes M., de Oliveira C.C., Lawrie C.H., Arauzo-Bravo M.J., Ribeiro M.L., et al. SOX9 Elevation Acts with Canonical WNT Signaling to Drive Gastric Cancer Progression. Cancer Res. 2016;76:6735–6746. doi: 10.1158/0008-5472.CAN-16-1120. [DOI] [PubMed] [Google Scholar]
- 128.Wroblewski L.E., Choi E., Petersen C., Delgado A.G., Piazuelo M.B., Romero-Gallo J., Lantz T.L., Zavros Y., Coffey R.J., Goldenring J.R., et al. Targeted mobilization of Lrig1 gastric epithelial stem cell populations by a carcinogenic Helicobacter pylori type IV secretion system. Proc. Natl. Acad. Sci. USA. 2019;116:19652–19658. doi: 10.1073/pnas.1903798116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Zavros Y. Initiation and Maintenance of Gastric Cancer: A Focus on CD44 Variant Isoforms and Cancer Stem Cells. Cell. Mol. Gastroenterol. Hepatol. 2017;4:55–63. doi: 10.1016/j.jcmgh.2017.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Morath I., Hartmann T., Orian-Rousseau V. CD44: More than a mere stem cell marker. Int. J. Biochem. Cell Biol. 2016;81:166–173. doi: 10.1016/j.biocel.2016.09.009. [DOI] [PubMed] [Google Scholar]
- 131.Wang L., Zuo X., Xie K., Wei D. Methods in Molecular Biology Cancer Stem Cells. Humana Press; New York, NY, USA: 2018. The Role of CD44 and Cancer Stem Cells; pp. 31–42. [DOI] [PubMed] [Google Scholar]
- 132.Wu K., Xu H., Tian Y., Yuan X., Wu H., Liu Q., Pestell R.G., Wu K. The role of CD44 in epithelial–Mesenchymal transition and cancer development. OncoTargets Ther. 2015;8:3783. doi: 10.2147/OTT.S95470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Takaishi S., Okumura T., Tu S., Wang S.S.W., Shibata W., Vigneshwaran R., Gordon S.A., Shimada Y., Wang T.C. Identification of gastric cancer stem cells using the cell surface marker CD44. Stem Cells. 2009;27:1006–1020. doi: 10.1002/stem.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Tsugawa H., Kato C., Mori H., Matsuzaki J., Kameyama K., Saya H., Hatakeyama M., Suematsu M., Suzuki H. Cancer Stem-Cell Marker CD44v9-Positive Cells Arise from Helicobacter pylori–Infected CAPZA1-Overexpressing Cells. Cell. Mol. Gastroenterol. Hepatol. 2019;8:319–334. doi: 10.1016/j.jcmgh.2019.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Bertaux-Skeirik N., Feng R., Schumacher M.A., Li J., Mahe M.M., Engevik A.C., Javier J.E., Peek R.M., Ottemann K., Orian-Rousseau V., et al. CD44 Plays a Functional Role in Helicobacter pylori-Induced Epithelial Cell Proliferation. PLoS Pathog. 2015;11:e1004663. doi: 10.1371/journal.ppat.1004663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Lin L., Wei H., Yi J., Xie B., Chen J., Zhou C., Wang L., Yang Y. Chronic CagA-Positive Helicobacter pylori infection with MNNG stimulation synergistically induces mesenchymal and cancer stem cell-Like properties in gastric mucosal epithelial cells. J. Cell. Biochem. 2019;120:17635–17649. doi: 10.1002/jcb.29031. [DOI] [PubMed] [Google Scholar]
- 137.Tsugawa H., Suzuki H., Saya H., Hatakeyama M., Hirayama T., Hirata K., Nagano O., Matsuzaki J., Hibi T. Reactive Oxygen Species-Induced Autophagic Degradation of Helicobacter pylori CagA Is Specifically Suppressed in Cancer Stem-Like Cells. Cell Host Microbe. 2012;12:764–777. doi: 10.1016/j.chom.2012.10.014. [DOI] [PubMed] [Google Scholar]
- 138.Yong X., Tang B., Xiao Y.-F., Xie R., Qin Y., Luo G., Hu C.J., Dong H., Yang S.M. Helicobacter pylori upregulates Nanog and Oct4 via Wnt/β-Catenin signaling pathway to promote cancer stem cell-Like properties in human gastric cancer. Cancer Lett. 2016;374:292–303. doi: 10.1016/j.canlet.2016.02.032. [DOI] [PubMed] [Google Scholar]
- 139.Sigal M., Rothenberg M.E., Logan C.Y., Lee J.Y., Honaker R.W., Cooper R.L., Passarelli B., Camorlinga M., Bouley D.M., Alvarez G., et al. Helicobacter pylori Activates and Expands Lgr5 Stem Cells through Direct Colonization of the Gastric Glands. Gastroenterology. 2015;148:1392–1404. doi: 10.1053/j.gastro.2015.02.049. [DOI] [PubMed] [Google Scholar]
- 140.Choi S.I., Yoon C., Park M.R., Lee D., Kook M.C., Lin J.X., Kang J.H., Ashktorab H., Smoot D.T., Yoon S.S., et al. CDX1 Expression Induced by CagA-Expressing Helicobacter pylori Promotes Gastric Tumorigenesis. Mol. Cancer Res. 2019;17:2169–2183. doi: 10.1158/1541-7786.MCR-19-0181. [DOI] [PubMed] [Google Scholar]
- 141.Yu F.X., Zhao B., Guan K.L. Hippo Pathway in Organ Size Control, Tissue Homeostasis, and Cancer. Cell. 2015;163:811–828. doi: 10.1016/j.cell.2015.10.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Koo J.H., Guan K.-L. Interplay between YAP/TAZ and Metabolism. Cell Metab. 2018;28:196–206. doi: 10.1016/j.cmet.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 143.Chen Y.-A., Lu C.-Y., Cheng T.-Y., Pan S.-H., Chen H.-F., Chang N.-S. WW Domain-Containing Proteins YAP and TAZ in the Hippo Pathway as Key Regulators in Stemness Maintenance, Tissue Homeostasis, and Tumorigenesis. Front. Oncol. 2019;9:60. doi: 10.3389/fonc.2019.00060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Zanconato F., Cordenonsi M., Piccolo S. YAP/TAZ at the Roots of Cancer. Cancer Cell. 2016;29:783–803. doi: 10.1016/j.ccell.2016.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Sardo F.L., Strano S., Blandino G. YAP and TAZ in Lung Cancer: Oncogenic Role and Clinical Targeting. Cancers. 2018;10:137. doi: 10.3390/cancers10050137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Liu-Chittenden Y., Huang B., Shim J.S., Chen Q., Lee S.-J., Anders R.A., Liu J.O., Pan D. Genetic and pharmacological disruption of the TEAD-YAP complex suppresses the oncogenic activity of YAP. Genes Dev. 2012;26:1300–1305. doi: 10.1101/gad.192856.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Peng C., Zhu Y., Zhang W., Liao Q., Chen Y., Zhao X., Guo Q., Shen P., Zhen B., Qian X., et al. Regulation of the Hippo-YAP Pathway by Glucose Sensor O-GlcNAcylation. Mol. Cell. 2017;68:591–604. doi: 10.1016/j.molcel.2017.10.010. [DOI] [PubMed] [Google Scholar]
- 148.Santucci M., Vignudelli T., Ferrari S., Mor M., Scalvini L., Bolognesi M.L., Uliassi E., Costi M.P. The Hippo Pathway and YAP/TAZ-TEAD Protein-Protein Interaction as Targets for Regenerative Medicine and Cancer Treatment. J. Med. Chem. 2015;58:4857–4873. doi: 10.1021/jm501615v. [DOI] [PubMed] [Google Scholar]
- 149.Lei Q.-Y., Zhang H., Zhao B., Zha Z.-Y., Bai F., Pei X.-H., Zhao S., Xiong Y., Guan K.-L. TAZ Promotes Cell Proliferation and Epithelial-Mesenchymal Transition and Is Inhibited by the Hippo Pathway. Mol. Cell. Biol. 2008;28:2426–2436. doi: 10.1128/MCB.01874-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Li N., Feng Y., Hu Y., He C., Xie C., Ouyang Y., Artim S.C., Huang D., Zhu Y., Luo Z., et al. Helicobacter pylori CagA promotes epithelial mesenchymal transition in gastric carcinogenesis via triggering oncogenic YAP pathway. J. Exp. Clin. Cancer Res. 2018;37:1–15. doi: 10.1186/s13046-018-0962-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Mo J.S., Meng Z., Kim Y.C., Park H.W., Hansen C.G., Kim S., Lim D.S., Guan K.L. Cellular energy stress induces AMPK-mediated regulation of YAP and the Hippo pathway. Nat. Cell Biol. 2015;17:500–510. doi: 10.1038/ncb3111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Wang Y., Pan P., Wang Z., Zhang Y., Xie P., Geng D., Jiang Y., Yu R., Zhou X. β-Catenin-Mediated YAP signaling promotes human glioma growth. J. Exp. Clin. Cancer Res. 2017;36:1–11. doi: 10.1186/s13046-017-0606-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Molina-Castro S.E., Tiffon C., Giraud J., Boeuf H., Sifre E., Giese A., Belleannee G., Lehours P., Bessede E., Megraud F., et al. The Hippo Kinase LATS2 Controls Helicobacter pylori-Induced Epithelial-Mesenchymal Transition and Intestinal Metaplasia in Gastric Mucosa. Cell. Mol. Gastroenterol. Hepatol. 2020;9:257–276. doi: 10.1016/j.jcmgh.2019.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Zhang L., Song X., Li X., Wu C., Jiang J. Yes-Associated Protein 1 as a Novel Prognostic Biomarker for Gastrointestinal Cancer: A Meta-Analysis. BioMed Res. Int. 2018;2018:1–10. doi: 10.1155/2018/4039173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Liu J., Zhao X., Wang K., Zhang X., Yu Y., Lv Y., Zhang S., Zhang L., Guo Y., Li Y., et al. A novel YAP1/SLC35B4 regulatory axis contributes to proliferation and progression of gastric carcinoma. Cell Death Dis. 2019;10:1–13. doi: 10.1038/s41419-019-1674-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Wu Y., Shen L., Liang X., Li S., Ma L., Zheng L., Li T., Yu H., Chan H., Chen C., et al. Helicobacter pylori-Induced YAP1 nuclear translocation promotes gastric carcinogenesis by enhancing IL-1β expression. Cancer Med. 2019;8:3965–3980. doi: 10.1002/cam4.2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Watanabe T., Takahashi A., Suzuki K., Kurusu-Kanno M., Yamaguchi K., Fujiki H., Suganuma M. Epithelial-Mesenchymal transition in human gastric cancer cell lines induced by TNF-α-Inducing protein of Helicobacter pylori. Int. J. Cancer. 2014;134:2373–2382. doi: 10.1002/ijc.28582. [DOI] [PubMed] [Google Scholar]
- 158.Shafaie E., Saberi S., Esmaeili M., Karimi Z., Najafi S., Tashakoripoor M., Abdirad A., Hosseini M.E., Mohagheghi M.A., Khalaj V., et al. Multiplex serology of Helicobacter pylori antigens in detection of current infection and atrophic gastritis-A simple and cost-Efficient method. Microb. Pathog. 2018;119:137–144. doi: 10.1016/j.micpath.2018.04.018. [DOI] [PubMed] [Google Scholar]
- 159.Ashrafi H., Siraji M.I., Showva N.N., Hossain M.M., Hossan T., Hasan M.A., Shohael A.M., Shawan M.M.A.K. Structure to function analysis with antigenic characterization of a hypothetical protein, HPAG1_0576 from Helicobacter pylori HPAG1. Bioinformation. 2019;15:456–466. doi: 10.6026/97320630015456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Suganuma M., Yamaguchi K., Ono Y., Matsumoto H., Hayashi T., Ogawa T., Imai K., Kuzuhara T., Nishizono A., Fujiki H. TNF-α-Inducing protein, a carcinogenic factor secreted fromH. pylori, enters gastric cancer cells. Int. J. Cancer. 2008;123:117–122. doi: 10.1002/ijc.23484. [DOI] [PubMed] [Google Scholar]
- 161.Suganuma M., Kuzuhara T., Yamaguchi K., Fujiki H. Carcinogenic Role of Tumor Necrosis Factor-α Inducing Protein of Helicobacter pylori in Human Stomach. BMB Rep. 2006;39:1–8. doi: 10.5483/BMBRep.2006.39.1.001. [DOI] [PubMed] [Google Scholar]
- 162.Tsuge H., Tsurumura T., Utsunomiya H., Kise D., Kuzuhara T., Watanabe T., Fujiki H., Suganuma M. Structural basis for the Helicobacter pylori-Carcinogenic TNF-α-Inducing protein. Biochem. Biophys. Res. Commun. 2009;388:193–198. doi: 10.1016/j.bbrc.2009.07.121. [DOI] [PubMed] [Google Scholar]
- 163.Tang C., Hao B., Zhang G., Shi R., Cheng W. Helicobacter pylori tumor necrosis factor-α inducing protein promotes cytokine expression via nuclear factor-κB. World J. Gastroenterol. 2013;19:399–403. doi: 10.3748/wjg.v19.i3.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Kuzuhara T., Suganuma M., Oka K., Fujiki H. DNA-Binding activity of TNF-α inducing protein from Helicobacter pylori. Biochem. Biophys. Res. Commun. 2007;362:805–810. doi: 10.1016/j.bbrc.2007.08.058. [DOI] [PubMed] [Google Scholar]
- 165.Huber M.A., Beug H., Wirth T. Epithelial-Mesenchymal Transition: NF-kappaB takes center stage. Cell Cycle. 2004:1477–1480. doi: 10.4161/cc.3.12.1280. [DOI] [PubMed] [Google Scholar]
- 166.Bo F., Holzenburg J., Godek F., Kauffmann P., Moser N., Schliephake H. Influence of tumour necrosis factor alpha on epithelial–Mesenchymal transition of oral cancer cells in co-Culture with mesenchymal stromal cells. Int. J. Maxillofac. Surg. 2020;49:157–165. doi: 10.1016/j.ijom.2019.06.001. [DOI] [PubMed] [Google Scholar]
- 167.Watanabe T., Tsuge H., Imagawa T., Kise D., Hirano K., Beppu M., Takahashi A., Yamaguchi K., Fujiki H., Suganuma M. Nucleolin as cell surface receptor for tumor necrosis factor-α inducing protein: A carcinogenic factor of Helicobacter pylori. J. Cancer Res. Clin. Oncol. 2010;136:911–921. doi: 10.1007/s00432-009-0733-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Zou M., Wang F., Jiang A., Xia A., Kong S., Gong C., Zhu M., Zhou X., Zhu J., Zhu W., et al. MicroRNA-3178 ameliorates inflammation and gastric carcinogenesis promoted byHelicobacter pylorinew toxin, Tip-α, by targeting TRAF3. Helicobacter. 2016;22:e12348. doi: 10.1111/hel.12348. [DOI] [PubMed] [Google Scholar]
- 169.Suganuma M., Kurusu M., Suzuki K., Nishizono A., Murakami K., Fujioka T., Fujiki H. New tumor necrosis factor-alpha Inducing protein released from Helicobacter pylori for gastric cancer progression. J. Cancer Res. Clin. Oncol. 2004;131:305–313. doi: 10.1007/s00432-004-0652-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Kawai M., Furuta Y., Yahara K., Tsuru T., Oshima K., Handa N., Takahashi N., Yoshida M., Azuma T., Hattori M., et al. Evolution in an oncogenic bacterial species with extreme genome plasticity: Helicobacter pylori East Asian genomes. BMC Microbiol. 2011;11:104. doi: 10.1186/1471-2180-11-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Acharyya S., Oskarsson T., Vanharanta S., Malladi S., Kim J., Morris P.G., Manova-Todorova K., Leversha M., Hogg N., Seshan V.E., et al. A CXCL1 Paracrine Network Links Cancer Chemoresistance and Metastasis. Cell. 2012;150:165–178. doi: 10.1016/j.cell.2012.04.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Kuzuhara T., Suganuma M., Kurusu M., Fujiki H. Helicobacter pylori-Secreting protein Tipα is a potent inducer of chemokine gene expressions in stomach cancer cells. J. Cancer Res. Clin. Oncol. 2006;133:287–296. doi: 10.1007/s00432-006-0169-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Jang J.Y., Yoon H.J., Yoon J.Y., Kim H.S., Lee S.J., Kim K.H., Kim D.J., Jang S., Han B.G., Lee B.I. Crystal structure of the TNF-Alpha inducing protein (Tip alpha) from Helicobacter pylori: Insights into Its DNA-Binding activity. J. Mol. Biol. 2009;392:191–197. doi: 10.1016/j.jmb.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 174.Hanahan D., Weinberg R.A. Hallmarks of cancer: The next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 175.Magalhaes A., Marcos-Pinto R., Nairn A., dela Rosa M., Ferreira R.M., Junqueira-Neto S., Freitas D., Gomes J., Oliveira P., Santos M.R., et al. Helicobacter pylori chronic infection and mucosal inflammation switches the human gastric glycosylation pathways. Biochim. Biophys. Acta. 2015;1852:1928–1939. doi: 10.1016/j.bbadis.2015.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.He C., Chen M., Liu J., Yuan Y. Host genetic factors respond to pathogenic step-Specific virulence factors of Helicobacter pylori in gastric carcinogenesis. Mutat. Res. Rev. Mutat. Res. 2014;759:14–26. doi: 10.1016/j.mrrev.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 177.Ferreira R.M., Carneiro F., Letley D., Atherton J.C., Figueiredo C. T1639 Helicobacter pylori vacA Intermediate Region i1 Strains Are Associated with More Severe Histological Features of Chronic Gastritis and Increased Gastric Carcinoma Risk in Portugal. Gastroenterology. 2009;136:A-548. doi: 10.1016/S0016-5085(09)62519-1. [DOI] [Google Scholar]
- 178.Fujiki H., Sueoka E., Watanabe T., Suganuma M. The concept of the okadaic acid class of tumor promoters is revived in endogenous protein inhibitors of protein phosphatase 2A, SET and CIP2A, in human cancers. J. Cancer Res. Clin. Oncol. 2018;144:2339–2349. doi: 10.1007/s00432-018-2765-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Fujiki H., Sueoka E., Suganuma M. Tumor promoters: From chemicals to inflammatory proteins. J. Cancer Res. Clin. Oncol. 2013;139:1603–1614. doi: 10.1007/s00432-013-1455-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Devanand P., Oya Y., Sundaramoorthy S., Song K.Y., Watanabe T., Kobayashi Y., Shimizu Y., Hong S.A., Suganuma M., Lim I.K. Inhibition of TNFα-interacting protein α (Tipα)-Associated gastric carcinogenesis by BTG2/TIS21 via downregulating cytoplasmic nucleolin expression. Exp. Mol. Med. 2018;50:e449. doi: 10.1038/emm.2017.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Fujiki H., Watanabe T., Suganuma M. Cell-Surface nucleolin acts as a central mediator for carcinogenic, anti-Carcinogenic, and disease-related ligands. J. Cancer Res. Clin. Oncol. 2014;140:689–699. doi: 10.1007/s00432-014-1587-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Suganuma M., Watanabe T., Yamaguchi K., Takahashi A., Fujiki H. Human gastric cancer development with TNF-α-Inducing protein secreted from Helicobacter pylori. Cancer Lett. 2012;322:133–138. doi: 10.1016/j.canlet.2012.03.027. [DOI] [PubMed] [Google Scholar]
- 183.Watanabe T., Hirano K., Takahashi A., Yamaguchi K., Beppu M., Fujiki H., Suganuma M. Nucleolin on the Cell Surface as a New Molecular Target for Gastric Cancer Treatment. Biol. Pharm. Bull. 2010;33:796–803. doi: 10.1248/bpb.33.796. [DOI] [PubMed] [Google Scholar]
- 184.Fujiki H., Suganuma M. Tumor Promoters-Microcystin-LR, Nodularin and TNF-α and Human Cancer Development. Anti Cancer Agents Med. Chem. 2011;11:4–18. doi: 10.2174/187152011794941163. [DOI] [PubMed] [Google Scholar]
- 185.Chen G., Tang N., Wang C., Xiao L., Yu M., Zhao L., Cai H., Han L., Xie C., Zhang Y. TNF-α-Inducing protein of Helicobacter pylori induces epithelial-mesenchymal transition (EMT) in gastric cancer cells through activation of IL-6/STAT3 signaling pathway. Biochem. Biophys. Res. Commun. 2017;484:311–317. doi: 10.1016/j.bbrc.2017.01.110. [DOI] [PubMed] [Google Scholar]
- 186.Inoue K., Shiota S., Yamada K., Gotoh K., Suganuma M., Fujioka T., Ahmed K., Iha H., Nishizono A. Evaluation of a New Tumor Necrosis Factor-α-Inducing Membrane Protein of Helicobacter pylori as a Prophylactic Vaccine Antigen. Helicobacter. 2009;14:487–495. doi: 10.1111/j.1523-5378.2009.00713.x. [DOI] [PubMed] [Google Scholar]
- 187.Keenan J., Allardyce R., Roake J., Oliaro J., Domigan N., Potter H., Aitken G., Allardyce R., Roake J. Immune response to an 18-Kilodalton outer membrane antigen identifies lipoprotein 20 as a Helicobacter pylori vaccine candidate. Infect. Immun. 2000;68:3337–3343. doi: 10.1128/IAI.68.6.3337-3343.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Wen Y., Marcus E.A., Matrubutham U., Gleeson M.A., Scott D.R., Sachs G. Acid-Adaptive Genes of Helicobacter pylori. Society. 2003;71:5921–5939. doi: 10.1128/IAI.71.10.5921-5939.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Ernst F.D., Bereswill S., Waidner B., Stoof J., Mäder U., Kusters J.G., Kuipers E.J., Kist M., van Vliet A.H.M., Homuth G. Transcriptional profiling of Helicobacter pylori Fur- and iron-Regulated gene expression. Microbiology. 2005;151:533–546. doi: 10.1099/mic.0.27404-0. [DOI] [PubMed] [Google Scholar]
- 190.Vallese F., Mishra N.M., Pagliari M., Berto P., Codolo G., de Bernard M., Zanotti G. Helicobacter pylori antigenic Lpp20 is a structural homologue of Tipα and promotes epithelial-Mesenchymal transition. Biochim. Biophys. Acta Gen. Subj. 2017;1861:3263–3271. doi: 10.1016/j.bbagen.2017.09.017. [DOI] [PubMed] [Google Scholar]
- 191.Ikeda W., Nakanishi H., Miyoshi J., Mandai K., Ishizaki H., Tanaka M., Togawa A., Takahashi K., Nishioka H., Yoshida H., et al. Afadin: A key molecule essential for structural organization of cell-Cell junctions of polarized epithelia during embryogenesis. J. Cell Biol. 1999;146:1117–1132. doi: 10.1083/jcb.146.5.1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Tabariès S., Mcnulty A., Ouellet V., Annis M.G., Dessureault M., Vinette M., Hachem Y., Lavoie B., Omeroglu A., Simon H.G., et al. Afadin cooperates with Claudin-2 to promote breast cancer metastasis. Genes Dev. 2019;33:180–193. doi: 10.1101/gad.319194.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Maruo T., Sakakibara S., Miyata M., Itoh Y., Kurita S. Molecular and Cellular Neuroscience Involvement of l-Afadin, but not s-Afadin, in the formation of puncta adherentia junctions of hippocampal synapses. Mol. Cell. Neurosci. 2018;92:40–49. doi: 10.1016/j.mcn.2018.06.006. [DOI] [PubMed] [Google Scholar]
- 194.Peng Y.F., Mandai K., Nakanishi H., Ikeda W., Asada M., Momose Y., Shibamoto S., Yanagihara K., Shiozaki K., Monden M., et al. Restoration of E-Cadherin-based cell–Cell adhesion by overexpression of nectin in HSC-39 cells, a human signet ring cell gastric cancer cell line. Oncogene. 2002;21:4108–4119. doi: 10.1038/sj.onc.1205517. [DOI] [PubMed] [Google Scholar]
- 195.Marques M.S., Melo J., Cavadas B., Mendes N., Pereira L., Carneiro F., Figueiredo C., Leite M. Afadin downregulation by helicobacter pyloriInduces epithelial to mesenchymal transition in gastric cells. Front. Microbiol. 2018;9:2712. doi: 10.3389/fmicb.2018.02712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Kim B.J., Kim J.G. Substitutions in Penicillin-Binding Protein 1 in Amoxicillin-Resistant Helicobacter pylori Strains Isolated from Korean Patients. Gut Liver. 2013;7:655. doi: 10.5009/gnl.2013.7.6.655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Nagai K., Davies T.A., Jacobs M.R., Appelbaum P.C. Effects of Amino Acid Alterations in and 2× on PBP Affinities of Penicillin, Clinical Isolates of Penicillin-Susceptible, Effects of Amino Acid Alterations in Penicillin-Binding Proteins (PBPs) 1a, 2b, and 2× on PBP Affinities of Penicillin, Ampici. Antimicrob. Agents Chemother. 2002;46:1273–1280. doi: 10.1128/AAC.46.5.1273-1280.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Huang L., Wang Z.Y., Pan D.D. Penicillin-Binding protein 1A mutation-Positive Helicobacter pylori promotes epithelial-Mesenchymal transition in gastric cancer via the suppression of microRNA-134. Int. J. Oncol. 2019;54:916–928. doi: 10.3892/ijo.2018.4665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Qiu Z., He G. MicroRNA-134 functions as a tumor suppressor gene in gastric cancer. Am. J. Transl. Res. 2016;8:4320–4328. [PMC free article] [PubMed] [Google Scholar]
- 200.Liu Y., Sun Y., Zhao A. MicroRNA-134 suppresses cell proliferation in gastric cancer cells via targeting of GOLPH3. Oncol. Rep. 2017;37:2441–2448. doi: 10.3892/or.2017.5488. [DOI] [PubMed] [Google Scholar]
- 201.Li J., Chen Y., Jin M., Wang J., Li S., Chen Z.H.E., Yu W. MicroRNA-134 reverses multidrug resistance in human lung adenocarcinoma cells by targeting FOXM1. Oncol. Lett. 2017;13:1451–1455. doi: 10.3892/ol.2017.5574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Damasceno J., Rodrigues R., Gonçalves R., Kitagawa R. Anti-Helicobacter pylori Activity of Isocoumarin Paepalantine: Morphological and Molecular Docking Analysis. Molecules. 2017;22:786. doi: 10.3390/molecules22050786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Marcus E.A., Inatomi N., Nagami G.T., Sachs G., Scott D.R. The effects of varying acidity on Helicobacter pylori growth and the bactericidal efficacy of ampicillin. Aliment. Pharmacol. Ther. 2012;36:972–979. doi: 10.1111/apt.12059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Jonas S., Izaurralde E. Towards a molecular understanding of microRNA-mediated gene silencing. Nat. Rev. Genet. 2015;16:421–433. doi: 10.1038/nrg3965. [DOI] [PubMed] [Google Scholar]
- 205.Lai X., Eberhardt M., Schmitz U., Vera J. Systems biology-Based investigation of cooperating microRNAs as monotherapy or adjuvant therapy in cancer. Nucleic Acids Res. 2019;47:7753–7766. doi: 10.1093/nar/gkz638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Xu D., Dong P., Xiong Y., Yue J., Konno Y., Ihira K., Kobayashi N., Todo Y., Watari H. MicroRNA-361-Mediated Inhibition of HSP90 Expression and EMT in Cervical Cancer Is Counteracted by Oncogenic lncRNA NEAT1. Cells. 2020;9:632. doi: 10.3390/cells9030632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Sartorius K., Makarova J., Sartorius B., An P., Winkler C., Chuturgoon A., Kramvis A. The Regulatory Role of MicroRNA in Hepatitis-B Virus-Associated Hepatocellular Carcinoma (HBV-HCC) Pathogenesis. Cells. 2019;8:1504. doi: 10.3390/cells8121504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Ding H., Shi Y., Liu X., Qiu A. MircoRNA-4513 promotes gastric cancer cell proliferation and epithelial–Mesenchymal transition through targeting KAT6B. Human Gene Ther. Clin. Dev. 2019;30:142–148. doi: 10.1089/humc.2019.094. [DOI] [PubMed] [Google Scholar]
- 209.Du M., Tan P., Wang A. microRNA-95 knockdown inhibits epithelial–Mesenchymal transition and cancer stem cell phenotype in gastric cancer cells through MAPK pathway by upregulating DUSP5. J. Cell. Physiol. 2020;235:944–956. doi: 10.1002/jcp.29010. [DOI] [PubMed] [Google Scholar]
- 210.Zhao L., Xue M., Zhang L., Guo B., Qin Y., Jiang Q., Sun R., Yang J., Wang L., Liu L., et al. MicroRNA-4268 inhibits cell proliferation via AKT/JNK signalling pathways by targeting Rab6B in human gastric cancer. Cancer Gene Ther. 2019:1–12. doi: 10.1038/s41417-019-0118-6. [DOI] [PubMed] [Google Scholar]
- 211.Sun F., Ni Y., Zhu H., Fang J., Wang H., Xia J., Ding F., Shen H., Shao S. MicroRNA-29a-3p, up-Regulated in human gastric cells and tissues with H. Pylori infection, promotes the migration of GES-1 Cells via A20-Mediated EMT Pathway. Cell. Physiol. Biochem. 2018;51:1250–1263. doi: 10.1159/000495502. [DOI] [PubMed] [Google Scholar]
- 212.Fukaya M., Brorsson C.A., Meyerovich K., Catrysse L., Delaroche D., Vanzela E.C., Ortis F., Beyaert R., Nielsen L.B., Andersen M.L., et al. A20 Inhibits β-Cell Apoptosis by Multiple Mechanisms and Predicts Residual β-Cell Function in Type 1 Diabetes. Mol. Endocrinol. 2016;30:48–61. doi: 10.1210/me.2015-1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Matsuhashi S., Manirujjaman M., Hamajima H., Ozaki I. Control Mechanisms of the Tumor Suppressor PDCD4: Expression and Functions. Int. J. Mol. Sci. 2019;20:2304. doi: 10.3390/ijms20092304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Vikhreva P.N., Kalinichenko S.V., Korobko I.V. Programmed cell death 4 mechanism of action: The model to be updated? Cell Cycle. 2017;16:1761–1764. doi: 10.1080/15384101.2017.1371881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Wang Q., Yang H.-S. The role of Pdcd4 in tumour suppression and protein translation. Biol. Cell. 2018;110:169–177. doi: 10.1111/boc.201800014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Leupold J.H., Yang H., Colburn N.H., Asangani I., Post S., Allgayer H. Tumor suppressor Pdcd4 inhibits invasion/intravasation and regulates urokinase receptor (u-PAR) gene expression via Sp-Transcription factors. Oncogene. 2007;26:4550–4562. doi: 10.1038/sj.onc.1210234. [DOI] [PubMed] [Google Scholar]
- 217.Shiota M., Izumi H., Tanimoto A., Takahashi M., Miyamoto N., Kashiwagi E., Kidani A., Hirano G., Masubuchi D., Fukunaka Y., et al. Programmed Cell Death Protein 4 Down-Regulates Y-Box Binding Protein-1 Expression via a Direct Interaction with Twist1 to Suppress Cancer Cell Growth. Cancer Res. 2009;69:3148–3156. doi: 10.1158/0008-5472.CAN-08-2334. [DOI] [PubMed] [Google Scholar]
- 218.Jo S., Kim D.E., Clocchiatti A., Dotto G.P. PDCD4 is a CSL associated protein with a transcription repressive function in cancer associated fibroblast activation. Oncotarget. 2016;7:58717–58727. doi: 10.18632/oncotarget.11227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Yu H., Zeng J., Liang X., Wang W., Zhou Y., Sun Y., Liu S., Li W., Chen C., Ja J. Helicobacter pylori Promotes Epithelial–Mesenchymal Transition in Gastric Cancer by Downregulating Programmed Cell Death Protein 4 (PDCD4) PLoS ONE. 2014;9:e105306. doi: 10.1371/journal.pone.0105306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Li L., Zhou L., Li Y., Lin S., Tomuleasa C. MicroRNA-21 Stimulates Gastric Cancer Growth and Ivasion by Inhibiting the Tumor Suppressor Effects of Programmed Cell Deatg Protein 4 and Phosphatase and Tensin Homolog. J. BUON. 2014;19:228–236. [PubMed] [Google Scholar]
- 221.Rehman Z., Fahim A., Bhatti A., Sadia H., John P. Co-Expression of HIF-1α, MDR1 and LAPTM4B in peripheral blood of solid tumors. PeerJ. 2019;7:e6309. doi: 10.7717/peerj.6309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Wang F., Wu H., Zhang S., Lu J., Lu Y., Zhan P., Fang Q., Wang F., Zhang X., Xie C., et al. LAPTM4B facilitates tumor growth and induces autophagy in hepatocellular carcinoma. Cancer Manag. Res. 2019;11:2485–2497. doi: 10.2147/CMAR.S201092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Li X., Song C., Wang K., Li N., Sun S., Li N., Zhao Z., Li M. Prognostic significance of LAPTM4B and p27kip1 expression in triple-negative breast cancer. Cancer Biomark. 2019;25:19–27. doi: 10.3233/CBM-182094. [DOI] [PubMed] [Google Scholar]
- 224.Wang L., Meng Y., Zhang Q. LAPTM4B is a novel diagnostic and prognostic marker for lung adenocarcinoma and associated with mutant EGFR. BMC Cancer. 2019;19:293. doi: 10.1186/s12885-019-5506-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Zhou S., Chen H., Yuan P., Shi N., Wang X., Hu J., Liu L. Helicobacter pylori infection promotes epithelial-to-mesenchymal transition of gastric cells by upregulating LAPTM4B. Biochem. Biophys. Res. Commun. 2019;514:893–900. doi: 10.1016/j.bbrc.2019.05.036. [DOI] [PubMed] [Google Scholar]
- 226.Yilmaz M., Christofori G. EMT, the cytoskeleton, and cancer cell invasion. Cancer Metastasis Rev. 2009;28:15–33. doi: 10.1007/s10555-008-9169-0. [DOI] [PubMed] [Google Scholar]
- 227.Kong F., Gao F., Chen J., Sun Y., Zhang Y., Liu H., Li X., Yang P., Zheng R., Liu G., et al. Overexpressed LAPTM4B-35 is a risk factor for cancer recurrence and poor prognosis in non-small-Cell lung cancer. Oncotarget. 2016;7:56193–56199. doi: 10.18632/oncotarget.10907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Li Z., Zhang J., Zhou J., Lu L., Wang H., Zhang G., Wan G., Cai S., Du J. Nodal Facilitates Differentiation of Fibroblasts to Cancer-Associated Fibroblasts that Support Tumor Growth in Melanoma and Colorectal Cancer. Cells. 2019;8:538. doi: 10.3390/cells8060538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Yegodayev K.M., Novoplansky O., Golden A., Prasad M., Levin L., Jagadeeshan S., Zorea J., Dimitstein O., Joshua B.Z., Cohen L., et al. TGF-Beta-Activated Cancer-Associated Fibroblasts Limit Cetuximab Efficacy in Preclinical Models of Head and Neck Cancer. Cancers. 2020;12:339. doi: 10.3390/cancers12020339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Minna E., Brich S., Todoerti K., Pilotti S., Collini P., Bonaldi E., Romeo P., Cecco L.D., Dugo M., Perrone F., et al. Cancer Associated Fibroblasts and Senescent Thyroid Cells in the Invasive Front of Thyroid Carcinoma. Cancers. 2020;12:112. doi: 10.3390/cancers12010112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Arneth B. Tumor Microenvironment. Medicina. 2019;56:15. doi: 10.3390/medicina56010015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Zhang Q., Chai S., Wang W., Wan C., Zhang F., Li Y., Wang F. Macrophages activate mesenchymal stem cells to acquire cancer-associated fibroblast-Like features resulting in gastric epithelial cell lesions and malignant transformation in vitro. Oncol. Lett. 2019;17:747–756. doi: 10.3892/ol.2018.9703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Zhang Q., Wang M., Huang F., Yang T., Cai J., Zhang X., Zhu W., Qian H., Xu W. H. pylori infection-induced MSC differentiation into CAFs promotes epithelial-mesenchymal transition in gastric epithelial cells. Int. J. Mol. Med. 2013;32:1465–1473. doi: 10.3892/ijmm.2013.1532. [DOI] [PubMed] [Google Scholar]
- 234.Tsukada T., Fushida S., Harada S., Yagi Y., Kinoshita J., Oyama K., Tajima H., Fujita H., Ninomiya I., Fujimura T., et al. The role of human peritoneal mesothelial cells in the fibrosis and progression of gastric cancer. Int. J. Oncol. 2012;41:476–482. doi: 10.3892/ijo.2012.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Zhang W., Gu J., Chen J., Zhang P., Ji R., Qian H., Xu W., Zhang X. Interaction with neutrophils promotes gastric cancer cell migration and invasion by inducing epithelial-mesenchymal transition. Oncol. Rep. 2017;38:2959–2966. doi: 10.3892/or.2017.5942. [DOI] [PubMed] [Google Scholar]
- 236.Ning X., Zhang H., Wang C., Song X. Exosomes Released by Gastric Cancer Cells Induce Transition of Pericytes Into Cancer-Associated Fibroblasts. Med. Sci. Monit. 2018;24:2350–2359. doi: 10.12659/MSM.906641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Lim H., Moon A. Inflammatory fibroblasts in cancer. Arch. Pharmacal Res. 2016;39:1021–1031. doi: 10.1007/s12272-016-0787-8. [DOI] [PubMed] [Google Scholar]
- 238.Yokozaki H., Koma Y.-I., Shigeoka M., Nishio M. Cancer as a tissue: The significance of cancer-Stromal interactions in the development, morphogenesis and progression of human upper digestive tract cancer. Pathol. Int. 2018;68:334–352. doi: 10.1111/pin.12674. [DOI] [PubMed] [Google Scholar]
- 239.Machlowska J., Maciejewski R., Sitarz R. The Pattern of Signatures in Gastric Cancer Prognosis. Int. J. Mol. Sci. 2018;19:1658. doi: 10.3390/ijms19061658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Erdogan B., Webb D.J. Cancer-Associated fibroblasts modulate growth factor signaling and extracellular matrix remodeling to regulate tumor metastasis. Biochem. Soc. Trans. 2017;45:229–236. doi: 10.1042/BST20160387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Itoh G., Chida S., Yanagihara K., Yashiro M., Aiba N., Tanaka M. Cancer-Associated fibroblasts induce cancer cell apoptosis that regulates invasion mode of tumours. Oncogene. 2017;36:4434–4444. doi: 10.1038/onc.2017.49. [DOI] [PubMed] [Google Scholar]
- 242.Tang D., Gao J., Wang S., Ye N., Chong Y., Huang Y., Wang J., Li B., Yin W., Wang D. Cancer-Associated fibroblasts promote angiogenesis in gastric cancer through galectin-1 expression. Tumor Biol. 2016;37:1889–1899. doi: 10.1007/s13277-015-3942-9. [DOI] [PubMed] [Google Scholar]
- 243.Lin N.N., Wang P., Zhao D., Zhang F.J., Yang K., Chen R. Significance of oral cancer-associated fibroblasts in angiogenesis, lymphangiogenesis, and tumor invasion in oral squamous cell carcinoma. J. Oral Pathol. Med. 2017;46:21–30. doi: 10.1111/jop.12452. [DOI] [PubMed] [Google Scholar]
- 244.Eiro N., González L., Martínez-Ordoñez A., Fernandez-Garcia B., González L.O., Cid S., Dominguez F., Perez-Fernandez R., Vizoso F.J. Cancer-Associated fibroblasts affect breast cancer cell gene expression, invasion and angiogenesis. Cell. Oncol. 2018;41:369–378. doi: 10.1007/s13402-018-0371-y. [DOI] [PubMed] [Google Scholar]
- 245.Krzysiek-Maczka G., Targosz A., Ptak-Belowska A., Korbut E., Szczyrk U., Strzalka M., Brzozowski T. Molecular alterations in fibroblasts exposed to helicobacter pylori: A missing link in bacterial inflammation progressing into gastric carcinogenesis? J. Physiol. Pharmacol. 2013;64:77–87. [PubMed] [Google Scholar]
- 246.Krzysiek-Maczka G., Targosz A., Szczyrk U., Strzałka M., Sliwowski Z., Brzozowski T., Czyz J., Ptak-Belowska A. Role of Helicobacter pylori infection in cancer-Associated fibroblast-induced epithelial-Mesenchymal transition in vitro. Helicobacter. 2018;23:1–15. doi: 10.1111/hel.12538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Wen X., He X., Jiao F., Wang C., Sun Y., Ren X., Li Q. Fibroblast Activation Protein-α-Positive Fibroblasts Promote Gastric Cancer Progression and Resistance to Immune Checkpoint Blockade. Oncol. Res. Featur. Preclin. Clin. Cancer Ther. 2017;25:629–640. doi: 10.3727/096504016X14768383625385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Koczorowska M.M., Tholen S., Bucher F., Lutz L., Kizhakkedathu J.N., De Wever O., Wellner U.F., Biniossek M.L., Stahl A., Lassmann S., et al. Fibroblast activation protein-α, a stromal cell surface protease, shapes key features of cancer associated fibroblasts through proteome and degradome alterations. Mol. Oncol. 2016;10:40–58. doi: 10.1016/j.molonc.2015.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Liu J., Huang C., Peng C., Xu F., Li Y., Yutaka Y., Xiong B., Yang X. Stromal fibroblast activation protein alpha promotes gastric cancer progression via epithelial-Mesenchymal transition through Wnt/β-Catenin pathway. BMC Cancer. 2018;18:1099. doi: 10.1186/s12885-018-5035-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Chiavarina B., Whitaker-Menezes D., Migneco G., Martinez-Outschoorn U.E., Pavlides S., Howell A., Tanowitz H.B., Casimiro M.C., Wang C., Pestell R.G., et al. HIF1-Alpha functions as a tumor promoter in cancer associated fibroblasts, and as a tumor suppressor in breast cancer cells: Autophagy drives compartment-specific oncogenesis. Cell Cycle. 2010;9:3534–3551. doi: 10.4161/cc.9.17.12908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Nagaharu K., Zhang X., Yoshida T., Katoh D., Hanamura N., Kozuka Y., Ogawa T., Shiraishi T., Imanaka-Yoshida K. Tenascin C induces epithelial-mesenchymal transition-like change accompanied by SRC activation and focal adhesion kinase phosphorylation in human breast cancer cells. Am. J. Pathol. 2011;178:754–763. doi: 10.1016/j.ajpath.2010.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Mikula-Pietrasik J., Uruski P., Tykarski A., Ksiazek K. The Peritoneal “soil” for a Cancerous “Seed”: A Comprehensive Review of the Pathogenesis of Intraperitoneal Cancer Metastases. Cell. Mol. Life Sci. 2018;75:509–525. doi: 10.1007/s00018-017-2663-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Krzysiek-Maczka G., Targosz A., Szczyrk U., Strzalka M., Brzozowski T., Ptak-Belowska A. Involvement of Epithelial-Mesenchymal Transition-Inducing Transcription Factors in the Mechanism of Helicobacter Pylori-Induced Fibroblasts Activation. J. Physiol. Pharmacol. 2019;70:727–736. doi: 10.26402/jpp.2019.5.08. [DOI] [PubMed] [Google Scholar]
- 254.Schoepp M., Ströse A., Haier J. Dysregulation of miRNA Expression in Cancer Associated Fibroblasts (CAFs) and Its Consequences on the Tumor Microenvironment. Cancers. 2017;9:54. doi: 10.3390/cancers9060054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Wang R., Sun Y., Yu W., Yan Y., Qiao M., Jiang R., Guan W., Wang L. Downregulation of miRNA-214 in cancer-Associated fibroblasts contributes to migration and invasion of gastric cancer cells through targeting FGF9 and inducing EMT. J. Exp. Clin. Cancer Res. 2019;38:20. doi: 10.1186/s13046-018-0995-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Sun C., Fukui H., Hara K., Zhang X., Kitayama Y., Eda H., Tomita T., Oshima T., Kikuchi S., Watari J., et al. FGF9 from cancer-Associated fibroblasts is a possible mediator of invasion and anti-Apoptosis of gastric cancer cells. BMC Cancer. 2015;15:333. doi: 10.1186/s12885-015-1353-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Li P., Shan J.-X., Chen X.-H., Zhang D., Su L.-P., Huang X.-Y., Yu B.Q., Zhi G.M., Li C.L., Wang Y.Q., et al. Epigenetic silencing of microRNA-149 in cancer-Associated fibroblasts mediates prostaglandin E2/interleukin-6 signaling in the tumor microenvironment. Cell Res. 2015;25:588–603. doi: 10.1038/cr.2015.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Hong H.N., Won Y.J., Shim J.H., Kim H.J., Han S.H., Kim B.S., Kim H.S. Cancer-Associated fibroblasts promote gastric tumorigenesis through EphA2 activation in a ligand-Independent manner. J. Cancer Res. Clin. Oncol. 2018;144:1649–1663. doi: 10.1007/s00432-018-2683-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Wu X., Tao P., Zhou Q., Li J., Yu Z., Wang X., Li J., Li C., Yan M., Zhu Z., et al. IL-6 secreted by cancer-Associated fibroblasts promotes epithelial-Mesenchymal transition and metastasis of gastric cancer via JAK2/STAT3 signaling pathway. Oncotarget. 2017;8:20741. doi: 10.18632/oncotarget.15119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Chong Y., Tang D., Xiong Q., Jiang X., Xu C., Huang Y., Wang J., Zhou H., Shi Y., Wu X., et al. Galectin-1 from cancer-Associated fibroblasts induces epithelial–Mesenchymal transition through β1 integrin-Mediated upregulation of Gli1 in gastric cancer. J. Exp. Clin. Cancer Res. 2016;35:175. doi: 10.1186/s13046-016-0449-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Zhou Q., Wu X., Wang X., Yu Z., Pan T., Li Z., Chang X., Jin Z., Li J., Zhu Z., et al. The reciprocal interaction between tumor cells and activated fibroblasts mediated by TNF-α/IL-33/ST2L signaling promotes gastric cancer metastasis. Oncogene. 2019;39:1414–1428. doi: 10.1038/s41388-019-1078-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Hsieh C.H., Chou Y.T., Kuo M.H., Tsai H.P., Chang J.L., Wu C.W. A targetable HB-EGF-CITED4 axis controls oncogenesis in lung cancer. Oncogene. 2017;36:2946–2956. doi: 10.1038/onc.2016.465. [DOI] [PubMed] [Google Scholar]
- 263.Dickson J.H., Grabowska A., El-Zaatari M., Atherton J., Watson S.A. Helicobacter pylori can induce heparin-Binding epidermal growth factor expression via gastrin and its receptor. Cancer Res. 2006;66:7524–7531. doi: 10.1158/0008-5472.CAN-05-3246. [DOI] [PubMed] [Google Scholar]
- 264.Chung H.W., Kong H.Y., Lim J.-B. Clinical significance and usefulness of soluble heparin binding-Epidermal growth factor in gastric cancer. World J. Gastroenterol. 2015;21:2080–2088. doi: 10.3748/wjg.v21.i7.2080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Naef M., Yokoyama M., Friess H., Büchler M.W., Korc M. Co-Expression of heparin-binding EGF-Like growth factor and related peptides in human gastric carcinoma. Int. J. Cancer. 1996;66:315–321. doi: 10.1002/(SICI)1097-0215(19960503)66:3<315::AID-IJC8>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 266.Kim J., Kim N., Park J.H., Chang H., Kim J.Y., Lee D.H., Kim J.M., Kim J.S., Jung H.C. The Effect of Helicobacter pylori on Epidermal Growth Factor Receptor-Induced Signal Transduction and the Preventive Effect of Celecoxib in Gastric Cancer Cells. Gut Liver. 2013;7:552–559. doi: 10.5009/gnl.2013.7.5.552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Romano M., Ricci V., Popolo A.D., Sommi P., Blanco C.D.V., Bruni C.B., Ventura U., Cover T.L., Blaser M.J., Coffey R.J., et al. Helicobacter pylori upregulates expression of epidermal growth factor-Related peptides, but inhibits their proliferative effect in MKN 28 gastric mucosal cells. J. Clin. Investig. 1998;101:1604–1613. doi: 10.1172/JCI1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Murayama Y., Miyagawa J.-I., Shinomura Y., Kanayama S., Isozaki K., Yamamori K., Mizuno H., Ishiguro S., Kiyohara T., Miyazaki Y., et al. Significance of the association between heparin-Binding epidermal growth factor-Like growth factor and CD9 in human gastric cancer. Int. J. Cancer. 2002;98:505–513. doi: 10.1002/ijc.10198. [DOI] [PubMed] [Google Scholar]
- 269.Busiello I., Acquaviva R., Di Popolo A., Blanchard T.G., Ricci V., Romano M., Zarrilli R. Helicobacter pylori γ-Glutamyltranspeptidase upregulates COX-2 and EGF-related peptide expression in human gastric cells. Cell. Microbiol. 2004;6:255–267. doi: 10.1046/j.1462-5822.2004.00366.x. [DOI] [PubMed] [Google Scholar]
- 270.Lu L., Ma G.-Q., Liu X.-D., Sun R.-R., Wang Q., Liu M., Zhang P.Y. Correlation between GDF15, MMP7 and gastric cancer and its prognosis. Eur. Rev. Med. Pharmacol. Sci. 2017;21:535–541. [PubMed] [Google Scholar]
- 271.Kitoh T., Yanai H., Saitoh Y., Nakamura Y., Matsubara Y., Kitoh H., Yoshida T., Okita K. Increased expression of matrix metalloproteinase-7 in invasive early gastric cancer. J. Gastroenterol. 2004;39:434–440. doi: 10.1007/s00535-003-1316-3. [DOI] [PubMed] [Google Scholar]
- 272.Yang T.F., Guo L., Wang Q. Meta-Analysis of Associations between Four Polymorphisms in the Matrix Metalloproteinases Gene and Gastric Cancer Risk. Asian Pac. J. Cancer Prev. 2014;15:1263–1267. doi: 10.7314/APJCP.2014.15.3.1263. [DOI] [PubMed] [Google Scholar]
- 273.Long Z.-W., Wang J.-L., Wang Y.-N. Matrix metalloproteinase-7 mRNA and protein expression in gastric carcinoma: A meta-Analysis. Tumor Biol. 2014;35:11415–11426. doi: 10.1007/s13277-014-2441-8. [DOI] [PubMed] [Google Scholar]
- 274.Li G., Su Q., Liu H., Wang D., Zhang W., Lu Z., Chen Y., Huang X., Li W., Zhang C., et al. Frizzled7 Promotes Epithelial-To-Mesenchymal Transition and Stemness via Activating Canonical Wnt/β-Catenin Pathway in Gastric Cancer. Int. J. Biol. Sci. 2018;14:280–293. doi: 10.7150/ijbs.23756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Kushlinskii N.E., Gershtein E.S., Ivannikov A.A., Davydov M.M., Chang V.L., Ognerubov N.A., Stilidi I.S. Clinical Significance of Matrix Metalloproteinases in Blood Plasma of Patients with Gastric Cancer. Bull. Exp. Biol. Med. 2019;166:373–376. doi: 10.1007/s10517-019-04353-y. [DOI] [PubMed] [Google Scholar]
- 276.Naumann M., Wessler S., Bartsch C., Wieland B., Covacci A., Haas R., Meyer T.F. Activation of activator protein 1 and stress response kinases in epithelial cells colonized by Helicobacter pylori encoding the cag pathogenicity island. J. Biol. Chem. 1999;274:31655–31662. doi: 10.1074/jbc.274.44.31655. [DOI] [PubMed] [Google Scholar]
- 277.Meyer-Ter-Vehn T., Covacci A., Kist M., Pahl H.L. Helicobacter pylori activates mitogen-Activated protein kinase cascades and induces expression of the proto-Oncogenes c-Fos and c-Jun. J. Biol. Chem. 2000;275:16064–16072. doi: 10.1074/jbc.M000959200. [DOI] [PubMed] [Google Scholar]
- 278.Wu D. Isocitrate dehydrogenase 2 inhibits gastric cancer cell invasion via matrix metalloproteinase 7. Tumor Biol. 2015;37:5225–5230. doi: 10.1007/s13277-015-4358-2. [DOI] [PubMed] [Google Scholar]
- 279.Gunawardhana N., Jang S., Choi Y.H., Hong Y.A., Jeon Y.-E., Kim A., Su H., Kim J.H., Yoo Y.J., Errell S., et al. Helicobacter pylori-Induced HB-EGF Upregulates Gastrin Expression via the EGF Receptor, C-Raf, Mek1, and Erk2 in the MAPK Pathway. Front. Cell. Infect. Microbiol. 2018;7:541. doi: 10.3389/fcimb.2017.00541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Soleyman-Jahi S., Nedjat S., Abdirad A., Hoorshad N., Heidari R., Zendehdel K. Prognostic Significance of Matrix Metalloproteinase-7 in Gastric Cancer Survival: A Meta-Analysis. PLoS ONE. 2015;10:e0122316. doi: 10.1371/journal.pone.0122316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Yin F., Grabowska A.M., Clarke P.A., Whelband E., Robinson K., Argent R.H., Tobias A., Kumari R., Therton J.C., Watson S.A. Helicobacter pylori potentiates epithelial: Mesenchymal transition in gastric cancer: Links to soluble HB-EGF, gastrin and matrix metalloproteinase-7. Gut. 2010;59:1037–1045. doi: 10.1136/gut.2009.199794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Zhao G., Liu L., Peek R.M., Hao X., Polk D.B., Li H., Yan F. Activation of Epidermal Growth Factor Receptor in Macrophages Mediates Feedback Inhibition of M2 Polarization and Gastrointestinal Tumor Cell Growth. J. Biol. Chem. 2016;291:20462–20472. doi: 10.1074/jbc.M116.750182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Byeon S.-J., Lee H.S., Kim M.-A., Lee B.L., Kim W.H. Expression of the ERBB Family of Ligands and Receptors in Gastric Cancer. Pathobiology. 2017;84:210–217. doi: 10.1159/000464250. [DOI] [PubMed] [Google Scholar]
- 284.Koshikawa N., Mizushima H., Minegishi T., Iwamoto R., Mekada E., Seiki M. Membrane Type 1-Matrix Metalloproteinase Cleaves Off the NH2-Terminal Portion of Heparin-Binding Epidermal Growth Factor and Converts It into a Heparin-Independent Growth Factor. Cancer Res. 2010;70:6093–6103. doi: 10.1158/0008-5472.CAN-10-0346. [DOI] [PubMed] [Google Scholar]
- 285.Yotsumoto F., Yagi H., Suzuki S.O., Oki E., Tsujioka H., Hachisuga T., Sonoda K., Kawarabayashi T., Mekada E., Miyamoto S. Validation of HB-EGF and amphiregulin as targets for human cancer therapy. Biochem. Biophys. Res. Commun. 2008;365:555–561. doi: 10.1016/j.bbrc.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 286.Kneissl J., Hartmann A., Pfarr N., Erlmeier F., Lorber T., Keller S., Zwingenberger G., Weichert W., Luber B. Influence of the HER receptor ligand system on sensitivity to cetuximab and trastuzumab in gastric cancer cell lines. J. Cancer Res. Clin. Oncol. 2016;143:573–600. doi: 10.1007/s00432-016-2308-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Shimura T., Yoshida M., Fukuda S., Ebi M., Hirata Y., Mizoshita T., Tanida S., Kataoka H., Kamiya T., Higashiyama S., et al. Nuclear translocation of the cytoplasmic domain of HB-EGF induces gastric cancer invasion. BMC Cancer. 2012;12:205. doi: 10.1186/1471-2407-12-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Shimura T., Kataoka H., Ogasawara N., Kubota E., Sasaki M., Tanida S., Joh T. Suppression of proHB-EGF Carboxy-Terminal Fragment Nuclear Translocation: A New Molecular Target Therapy for Gastric Cancer. Clin. Cancer Res. 2008;14:3956–3965. doi: 10.1158/1078-0432.CCR-07-4794. [DOI] [PubMed] [Google Scholar]
- 289.Krakowiak M.S., Noto J.M., Piazuelo M.B., Hardbower D.M., Romero-Gallo J., Delgado A., Chaturvedi R., Correa P., Wilson K.T., Peek R.M. Matrix metalloproteinase 7 restrains Helicobacter pylori-Induced gastric inflammation and premalignant lesions in the stomach by altering macrophage polarization. Oncogene. 2014;34:1865–1871. doi: 10.1038/onc.2014.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Azizi P., Mazhari S., Tokhangibli S., Noukabadi F.N., Abkenar E.D., Shamsafzali E., Baghaei K. Paracrine Signals of Mesenchymal Stem Cells Induce Epithelial to Mesenchymal Transition in Gastric Cancer Cells. Gastroenterol. Hepatol. Bed Bench. 2019;12(Suppl. 1):S51–S57. [PMC free article] [PubMed] [Google Scholar]
- 291.Puculek M., Baj J., Portincasa P., Sitarz M., Grochowski C., Radzikowska E. The morphology and application of stem cells in digestive system surgery. Folia Morphol. 2020 doi: 10.5603/FM.a2020.0024. [DOI] [PubMed] [Google Scholar]
- 292.Li W., Zhou Y., Yang J., Zhang X., Zhang H., Zhang T., Zhao S., Zheng P., Huo J., Wu H. Gastric cancer-Derived mesenchymal stem cells prompt gastric cancer progression through secretion of interleukin-8. J. Exp. Clin. Cancer Res. 2015;34:52. doi: 10.1186/s13046-015-0172-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Pan Z., Tian Y., Zhang B., Zhang X., Shi H., Liang Z., Wu P., Li R., You B., Yang L., et al. YAP signaling in gastric cancer-Derived mesenchymal stem cells is critical for its promoting role in cancer progression. Int. J. Oncol. 2017;51:1055–1066. doi: 10.3892/ijo.2017.4101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Ferrand J., Lehours P., Schmid-Alliana A., Mégraud F., Varon C. Helicobacter pylori infection of gastrointestinal epithelial cells in vitro induces mesenchymal stem cell migration through an NF-κB-Dependent pathway. PLoS ONE. 2011;6:4–13. doi: 10.1371/journal.pone.0029007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Ridge S.M., Sullivan F.J., Glynn S.A. Mesenchymal stem cells: Key players in cancer progression. Mol. Cancer. 2017;16:31. doi: 10.1186/s12943-017-0597-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Xue Z., Wu X., Chen X., Liu Y., Wang X., Wu K., Nie Y., Fan D. Mesenchymal Stem Cells Promote Epithelial to Mesenchymal Transition and Metastasis in Gastric Cancer Though Paracrine Cues and Close Physical Contact. J. Cell. Biochem. 2015;116:618–627. doi: 10.1002/jcb.25013. [DOI] [PubMed] [Google Scholar]
- 297.Ma X., Wang B., Wang X., Luo Y., Fan W. NANOGP8 is the key regulator of stemness, EMT, Wnt pathway, chemoresistance, and other malignant phenotypes in gastric cancer cells. PLoS ONE. 2018;13:e0192436. doi: 10.1371/journal.pone.0192436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Zhang Q., Ding J., Liu J., Wang W., Zhang F., Wang J., Li Y. Helicobacter pylori-infected MSCs acquire a pro-Inflammatory phenotype and induce human gastric cancer migration by promoting EMT in gastric cancer cells. Oncol. Lett. 2016;11:449–457. doi: 10.3892/ol.2015.3897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Sun L., Wang Q., Chen B., Zhao Y., Shen B., Wang X., Zhu M., Li Z., Zhao X., Xu C. Human Gastric Cancer Mesenchymal Stem Cell-Derived IL15 Contributes to Tumor Cell Epithelial-Mesenchymal Transition via Upregulation Tregs Ratio and PD-1 Expression in CD4 T Cell. Stem Cells Dev. 2018;27:1203–1214. doi: 10.1089/scd.2018.0043. [DOI] [PubMed] [Google Scholar]
- 300.Jiang Y.-X., Yang S.-W., Li P.-A., Luo X., Li Z.-Y., Hao Y.-X., Yu P.-W. The promotion of the transformation of quiescent gastric cancer stem cells by IL-17 and the underlying mechanisms. Oncogene. 2016;36:1256–1264. doi: 10.1038/onc.2016.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Peng X., Liu G., Peng H., Chen A., Zha L., Wang Z. SOX4 contributes to TGF-β-Induced epithelial–Mesenchymal transition and stem cell characteristics of gastric cancer cells. Genes Dis. 2018;5:49–61. doi: 10.1016/j.gendis.2017.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Zhang S., Shang Y., Chen T., Zhou X., Meng W., Fan C., Lu R., Huang Q., Li X., Hong X., et al. Human circulating and tissue gastric cancer stem cells display distinct epithelial–Mesenchymal features and behaviors. J. Cancer Res. Clin. Oncol. 2017;143:1687–1699. doi: 10.1007/s00432-017-2417-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Bessède E., Dubus P., Mégraud F., Varon C. Helicobacter pylori infection and stem cells at the origin of gastric cancer. Oncogene. 2014;34:2547–2555. doi: 10.1038/onc.2014.187. [DOI] [PubMed] [Google Scholar]
- 304.Lu Y.-J., Geng Z.-J., Sun X.-Y., Li Y.-H., Fu X.-B., Zhao X.-Y., Wei B. Isoprenaline induces epithelial–Mesenchymal transition in gastric cancer cells. Mol. Cell. Biochem. 2015;408:1–13. doi: 10.1007/s11010-015-2477-0. [DOI] [PubMed] [Google Scholar]
- 305.Kim N. Chemoprevention of Gastric Cancer by Helicobacter Pylori Eradication and Its Underlying Mechanism. J. Gastroenterol. Hepatol. 2019;34:1287–1295. doi: 10.1111/jgh.14646. [DOI] [PubMed] [Google Scholar]
- 306.Shu X., Liu H., Pan Y., Sun L., Yu L., Sun L., Yang Z., Ran Y. Distinct biological characterization of the CD44 and CD90 phenotypes of cancer stem cells in gastric cancer cell lines. Mol. Cell. Biochem. 2019;459:35–47. doi: 10.1007/s11010-019-03548-1. [DOI] [PubMed] [Google Scholar]
- 307.Li L.-C., Wang D.-L., Wu Y.-Z., Nian W.-Q., Wu Z.-J., Li Y., Ma H.W., Shao J.H. Gastric tumor-Initiating CD44 cells and epithelial-Mesenchymal transition are inhibited by γ-Secretase inhibitor DAPT. Oncol. Lett. 2015;10:3293–3299. doi: 10.3892/ol.2015.3727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Tanabe S. Regulated genes in mesenchymal stem cells and gastric cancer. World J. Stem Cells. 2015;7:208. doi: 10.4252/wjsc.v7.i1.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Yoon C., Till J., Cho S.-J., Chang K.K., Lin J.-X., Huang C.-M., Ryeom S., Yoon S.S. KRAS Activation in Gastric Adenocarcinoma Stimulates Epithelial-to-Mesenchymal Transition to Cancer Stem–Like Cells and Promotes Metastasis. Mol. Cancer Res. 2019;17:1945–1957. doi: 10.1158/1541-7786.MCR-19-0077. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 310.Yoon C., Cho S.-J., Chang K.K., Park D.J., Ryeom S.W., Yoon S.S. Role of Rac1 Pathway in Epithelial-to-Mesenchymal Transition and Cancer Stem-Like Cell Phenotypes in Gastric Adenocarcinoma. Mol. Cancer Res. 2017;15:1106–1116. doi: 10.1158/1541-7786.MCR-17-0053. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 311.Xue J., Zhu Y., Sun Z., Ji R., Zhang X., Xu W., Yuan X., Zhang B., Yan Y., Yin L., et al. Tumorigenic hybrids between mesenchymal stem cells and gastric cancer cells enhanced cancer proliferation, migration and stemness. BMC Cancer. 2015;15:793. doi: 10.1186/s12885-015-1780-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Guo J., Wang B., Fu Z., Wei J., Lu W. Hypoxic Microenvironment Induces EMT and Upgrades Stem-Like Properties of Gastric Cancer Cells. Technol. Cancer Res. Treat. 2015;15:60–68. doi: 10.1177/1533034614566413. [DOI] [PubMed] [Google Scholar]
- 313.Hajimoradi M., Hassan Z.M., Ebrahimi M., Soleimani M., Bakhshi M., Firouzi J., Samani F.S. STAT3 Is Overactivated in Gastric Cancer Stem-Like Cells. Cell J. 2016;17:617–628. doi: 10.22074/cellj.2016.3834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Jung D.H., Bae Y.J., Kim J.-H., Shin Y.K., Jeung H.-C. HER2 Regulates Cancer Stem Cell Activities via the Wnt Signaling Pathway in Gastric Cancer Cells. Oncology. 2019;97:311–318. doi: 10.1159/000502845. [DOI] [PubMed] [Google Scholar]
- 315.Yang S.-W., Ping Y.-F., Jiang Y.-X., Luo X., Zhang X., Bian X.-W., Yu P.W. ATG4A promotes tumor metastasis by inducing the epithelial-Mesenchymal transition and stem-Like properties in gastric cells. Oncotarget. 2016;7:39279–39292. doi: 10.18632/oncotarget.9827. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 316.Gan L., Xu M., Hua R., Tan C., Zhang J., Gong Y., Wu Z., Weng W., Sheng W., Guo W. The polycomb group protein EZH2 induces epithelial–Mesenchymal transition and pluripotent phenotype of gastric cancer cells by binding to PTEN promoter. J. Hematol. Oncol. 2018;11:9. doi: 10.1186/s13045-017-0547-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Yang S.-W., Zhang Z.-G., Hao Y.-X., Zhao Y.-L., Qian F., Shi Y., Li P.A., Liu C.Y., Yu P.W. HIF-1α induces the epithelial-Mesenchymal transition in gastric cancer stem cells through the Snail pathway. Oncotarget. 2017;8:9535–9545. doi: 10.18632/oncotarget.14484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Yang T., Zhang X., Wang M., Zhang J., Huang F., Cai J., Zhang Q., Mao F., Zhu W., Qian H., et al. Activation of Mesenchymal Stem Cells by Macrophages Prompts Human Gastric Cancer Growth through NF-κB Pathway. PLoS ONE. 2014;9:e97569. doi: 10.1371/journal.pone.0097569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Jo J., Park S., Park S., Lee H., Kim C., Jung D.E., Song S.Y. Novel Gastric Cancer Stem Cell-Related Marker LINGO2 Is Associated with Cancer Cell Phenotype and Patient Outcome. Int. J. Mol. Sci. 2019;20:555. doi: 10.3390/ijms20030555. [DOI] [PMC free article] [PubMed] [Google Scholar]