Abstract
Colorectal cancer (CRC), a severe complication of inflammatory bowel diseases, is a common type of cancer and accounts for high mortality. CRC can be modeled in mice by application of the tumor promoter, azoxymethane (AOM), in combination with dextran sodium sulfate (DSS), which are able to induce colitis-like manifestations. Active colitis correlates with high mucosal concentrations of histamine, which, together with the histamine receptor subtype 4 (H4R), provide a pro-inflammatory function in a mouse colitis model. Here, we analyzed whether H4R is involved in the pathogenesis of AOM/DSS-induced CRC in mice. As compared to wild type (WT) mice, AOM/DSS-treated mice lacking H4R expression (TM) demonstrate ameliorated signs of CRC, i.e., significantly reduced loss of body weight, stiffer stool consistency, and less severe perianal bleeding. Importantly, numbers and diameters of tumors and the degree of colonic inflammation are dramatically reduced in TM mice as compared to WT mice. This is concomitant with a reduced colonic inflammatory response involving expression of cyclooxygenase 2 and the production of C-X-C motif chemokine ligand 1 (CXCL1) and CXCL2. We conclude that H4R is involved in the tumorigenesis of chemically-induced CRC in mice via cyclooxygenase 2 expression and, probably, CXCL1 and CXCL2 as effector molecules.
Keywords: histamine, H4 receptor, colorectal cancer, mouse model, cyclooxygenase 2
1. Introduction
The biogenic amine histamine (2-(4-imidazolyl)-ethylamine) is a profound mediator of inflammation [1]. It is recognized by the respective target cell through histamine-specific G protein-coupled receptors, which are subdivided into four subtypes: histamine H1-receptor (H1R), H2R, H3R and H4R. Out of these, the H4R is the latest one identified, due to its homology (37%) to the H3R [2,3,4,5,6]. H4R is predominantly expressed in immune cells [7,8,9,10,11] and its activation affects inflammatory and immune reactions via Gi-mediated pathways [10,12,13,14].
Inflammatory bowel diseases (IBD), including the most prevalent manifestations, ulcerative colitis and Crohn’s disease, are idiopathic, chronic-recurring disorders of the gut. They severely affect the quality of patients’ lives and eventually limit their life expectancy through complications like extra-intestinal manifestations and colorectal cancer (CRC) [15,16]. CRC is the third most common type of cancer in men and accounts for high mortality [17,18]. In addition to colitis-associated CRC, CRC appears sporadic and hereditary [19,20]. However, although inflammation rarely precedes sporadic or hereditary CRC, anti-inflammatory drugs are effective in preventing or delaying the diseases. Thus, inflammatory reactions seem to be also involved in tumorigenesis of sporadic and hereditary cases [21,22].
Dextran sodium sulfate (DSS)-induced colitis is a widely used model for ulcerative colitis. The treatment of animals with the tumor promoter azoxymethane (AOM) in combination with DSS serves as a model for CRC (AOM/DSS model). DSS is thought to induce injury of colon epithelial cells, leading to impairment of the epithelial barrier and bacterial infiltration into the colonic mucosa [23]. The subsequent local inflammatory response is dominated by innate immune mechanisms [24,25]. Neutrophilic granulocytes are massively recruited to the lamina propria [26]. Other immune cells involved in colitic inflammation are mast cells, basophils, and eosinophils [27].
The increased number of mucosal mast cells able to release histamine has been shown to correlate with active colitis [28], as does the enhanced mucosal concentration of histamine [29]. A pro-inflammatory function of histamine and the H4R in DSS-induced colitis in mice has been demonstrated in previous studies [30,31,32,33]. Thus, in the present study, we aimed at analyzing whether the H4R bears a functional role in the pathogenesis of chemically induced CRC employing the AOM/DSS model in mice.
2. Results
2.1. Clinical and Macroscopic Evaluation
Upon induction of CRC by AOM/DSS treatment (Figure 1a), the mice developed a transiently increasing and decreasing activity of intestinal disease (Figure 1b). Increases of disease activity coincided with DSS feeding, while decreases occurred during DSS-free periods. Application of the tumor promoter, AOM, at day 0 of the treatment schedule did not induce any obvious disease activity until the start of DSS treatment. Thus, control mice, which for the entire schedule were treated with AOM only and fed with water not supplemented, did not develop any significant signs of disease activity (Figure 1b). Remarkably, TM CRC mice demonstrated a significant lower disease activity as compared to WT CRC mice (Figure 1b).
Figure 1.
(a) Schematic representation of the schedule of acetoxymethan/dextran sulfate sodium (AOM/DSS) application. Control mice were treated with AOM only, but no DSS was applied (not shown). (b) Mice of either wild type (WT) or H4R−/− (TM) genotype were treated either with AOM/DSS (CRC) or with AOM only (ctr). On the days indicated, clinical disease symptoms, body weight, perianal bleeding, and stool consistency, were monitored, graded by a scoring system, and summed up to the disease activity index (DAI). Means +/− SD of n = 2–6. *, p < 0.05 (two-way ANOVA with Sidak’s post hoc test).
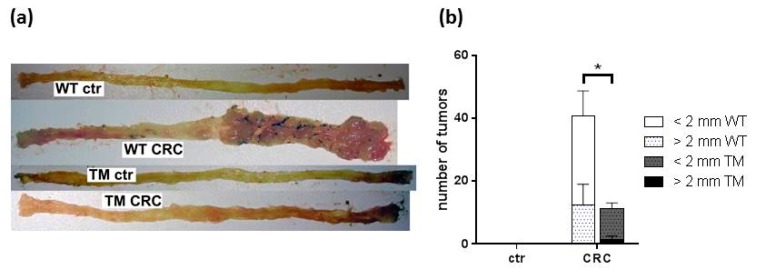
Analyzing the colon specimen of these mice at the end of the treatment schedule revealed dramatic differences between WT CRC and TM CRC mice (Figure 2a). While WT CRC mice developed a high number of large tumors at the distal part of their colons, tumors in TM CRC mice were significantly lower in number and diameter (Figure 2b). Control mice treated only with AOM developed no colon tumors (Figure 2a,b).
Figure 2.
(a) Representative photographs of the colon specimen prepared out of the mice described in Figure 1. (b) The tumors detected in the colon specimen were counted and graded according to their diameter being either smaller or larger than 2 mm. WT: wild type, TM: H4R−/−, ctr: AOM-treated mice, CRC: AOM/DSS-treated mice. Means +/- SD of n = 2–6. *, p < 0.05 (two way ANOVA with Sidak’s post hoc test).
2.2. Microscopic Evaluation of Colon Tissues
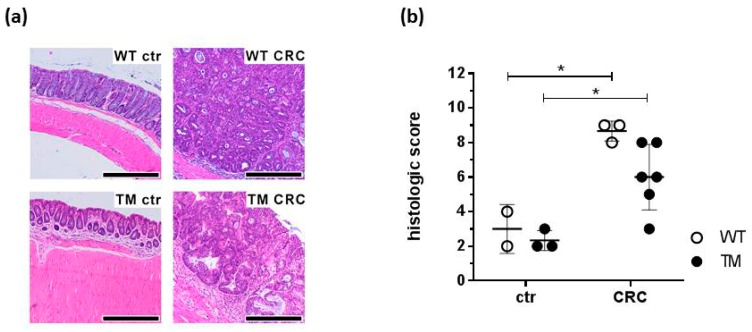
The colonic mucosa of AOM-only treated control mice demonstrated a normal histological appearance, showing no signs of tumor growth (Figure 3a) with a low inflammation score (Figure 3b). In contrast, histological colon specimens from WT CRC mice exhibited marked mucosal inflammation and tumor-adjacent mucosal hyperplasia (Figure 3a), resulting in an increased inflammation score compared to the specimen of the control mice (Figure 3b). These parameters appeared to be less pronounced in TM CRC mice as compared to WT CRC mice (Figure 3b), although the difference was not statistically significant. The inflammatory reaction was—in both WT CRC mice and TM CRC mice—pronounced in mucosal areas adjacent to the tumor, with areas far from the tumor being less affected. In addition, tumors from TM CRC mice showed a more sessile morphology, while WT CRC mice revealed a predominantly polypoid morphology. The tumor-adjacent inflammatory infiltrate consisted mainly of CD3+ lymphocytes and plasma cells (Figure S1). In direct vicinity to the infiltrate, neutrophilic granulocytes could also be found. The tumors themselves showed a broad tubular architecture with only scarce areas of cribriform or solid growth patterns with marked nuclear pleomorphy and atypia, as well as an increased mitotic activity. None of the tumors infiltrated the tunica muscularis propria, with possible infiltrations of the submucosa. Thus, carcinogenesis in our model is still at an early stage, which is most likely due to the experimental schedule that may be too short to allow full carcinoma development.
Figure 3.
Colon tissues prepared out of the mice described in Figure 1 were fixed in buffered formalin, embedded in paraffin, and sliced into histological sections. Sections were stained with hematoxilin/eosin and evaluated for inflammation and tumor morphology. (a) Representative micro-photographs of the colon sections. (b) Quantitative grading of the tumors. WT: wild type, TM: H4R−/−, ctr: AOM-treated mice, CRC: AOM/DSS-treated mice. Magnification: 40×; scale bar: 300 µm. Individual values and means +/− SD of n = 2–6. *, p < 0.05 (two-way ANOVA with Sidak’s post hoc test).
2.3. CXCL1 and CXCL2 Production
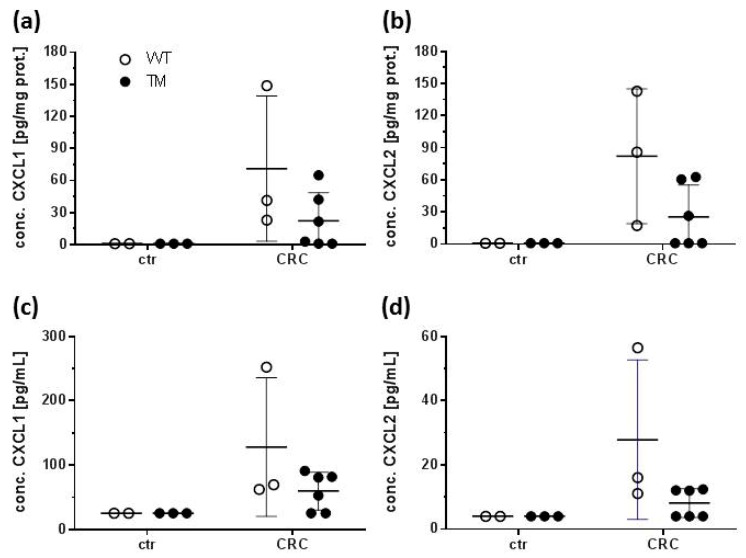
In colon homogenates and sera from control mice, C-X-C motif chemokine ligand 1 (CXCL1 and CXCL2 were barely detectable, while significant concentrations could be measured in homogenates and sera from WT CRC and TM CRC mice (Figure 4a–d). These concentrations, however, did not significantly differ between WT CRC and TM CRC mice.
Figure 4.
Colon homogenates and sera were prepared out of the mice described in Figure 1. The concentrations of CXCL1 and CXCL2 were quantified using a multiplex ELISA technique. (a,b) Concentrations of (a) CXCL1 and (b) CXCL2 in colon homogenates. (c,d) Concentrations of (c) CXCL1 and (d) CXCL2 in sera. WT: wild type, TM: H4R−/−, ctr: AOM-treated mice, CRC: AOM/DSS-treated mice. Individual values and means +/− SD of n = 2–6. No significant differences (two-way ANOVA with Sidak’s post hoc test).
2.4. COX 2 and NOS 2 Expression
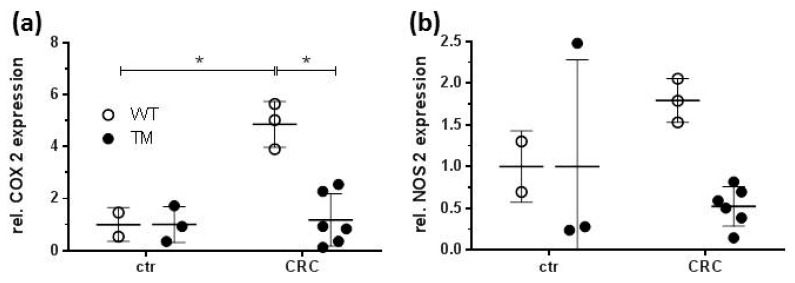
mRNA encoding cyclooxygenase 2 (COX 2), which is expressed in around 80% of human CRC, was detectable in colon specimen of control mice treated with AOM only, independent of the genotype. After CRC induction, the amount of COX 2 mRNA was significantly increased in WT CRC mice, while in TM CRC mice it remained at the level of control mice (Figure 5a). Thus, a significant difference in COX 2 mRNA accumulation was detected between colon samples of WT CRC and TM CRC mice. mRNA encoding the inducible nitric oxide synthase (nitric oxide synthase 2; NOS 2), which was reported to demonstrate an up-regulated expression in AOM/DSS-induced dysplasia in mice, in our hands, was detectable in all groups of samples but without significant differences regarding treatment or genotype (Figure 5b).
Figure 5.
RNA was isolated from colon samples out of the mice described in Figure 1. The concentrations of mRNA encoding COX 2 and NOS 2 were quantified by RT-qPCR. (a,b) Relative mRNA expression of (a) COX2 and (b) NOS2. WT: wild type, TM: H4R−/−, ctr: AOM-treated mice, CRC: AOM/DSS-treated mice. Means +/− SD of n = 2–6. *, p < 0.05 (two-way ANOVA with Sidak’s post hoc test).
3. Discussion
The present study aimed at analyzing whether or not histamine and its receptor H4R are involved in the pathogenesis of CRC, modelled by AOM/DSS treatment of mice, as already suggested by Tanaka et al. [34]. To this end, development of CRC was chemically induced in WT and TM mice, and symptoms as well as parameters indicative of intestinal disease were compared. The change in clinical symptoms analyzed in this study and reported as DAI (sum of weight loss, perianal bleeding, and reduced stool consistency) indicates colonic derangements and is significantly higher on the feeding of colitogenic DSS. Importantly, disease activity is reduced due to the absence of H4R expression, and thus confirms already reported data on the involvement of the H4R in experimental acute colitis in mice [30,33]. Moreover, it assigns H4R a function to a chronic model of colitis, beyond its recognized function to acute colitis models [30,33]. Certainly, the statistical significance of the difference between the DAI of WT CRC and TM CRC groups is limited, which is most probably due to the fact that the data of this small proof-of-concept study are based on only a very limited number of mice per group. This limitation of this study may also account for the poor or lacking significance of several other parameters that are discussed below. The rather low number of animals, however, was sufficient to reveal a significant difference when looking at the tumor burden, the primary goal of this study.
Tumor development became obvious upon brief inspection of the colon specimen. We could confirm that cancerization was strictly associated to DSS-induced colitis, since control mice treated with only the tumor promoter, AOM, did not develop any colonic tumor. Both macroscopic and microscopic evaluations reveal that the absence of H4R reduced inflammation, leading to the reduced number and diameter of tumors. This observation is highly similar to findings observed in an experimental model of breast cancer [35].
Based on our findings, two hypothetical mechanisms may be the underlying cause: (1) lack of H4R expression reduces colitis as discussed above and, subsequently, dampens inflammatory-driven, colitis-dependent tumorigenesis, or (2) lack of H4R expression abolishes a tumor cell proliferation-promoting effect of histamine-induced H4R signaling. Of course, both mechanisms in combination may also explain the observed effect.
Undoubtedly, histamine and its receptor H4R exert a pro-inflammatory function in DSS-induced colitis in mice [30,32,33], rendering hypothesis (1) feasible. This is supported by the slightly-enhanced production of CXCL1 and CXCL2 in AOM/DSS-treated mice as compared to AOM-only-treated mice. This rather modest increase is probably a consequence of the experiment’s timing (Figure 1a). If samples for expression/production analyses were generated immediately at the end of a cycle of DSS feeding, a significant increase in CXCL1 and CXCL2 expression was detected (unpublished observation), while in the present study, samples were generated roughly two weeks after the last cycle of DSS feeding. Thus, at this time point in the experimental protocol, expression of CXCL1 and CXCL2 is already declining.
On the other hand, CXCL1 [36] and CXCL2 [37], that are produced upon appropriate stimulation by a variety of cell types including monocytes/macrophages, neutrophils, epithelial cells and also tumor cells, have functions beyond attracting neutrophil granulocytes to the site of infection or damage. In colon cancer, they are associated with angiogenesis and the transition from dysplasia to carcinoma [38,39,40], indicating a possible mechanistic connection between inflammation and tumorigenesis. The expression of CXCL1 and CXCL2 in tumors is regulated, besides others, by prostaglandin E2 (PGE2) [38]. PGE2 is a lipid mediator that is generated by means of COX 2, a diagnostic marker for CRC [41]. The expression of COX 2, which is, in contrast to that of NOS 2, upregulated due to the AOM/DSS treatment, strictly depends on the presence of the H4R. Thus, H4R signaling in epithelial cells may induce COX 2 expression [42], leading to an increased production of PGE2, which, subsequently, induces the production of CXCL1 [43] and CXCL2, resulting in tumor progression. Supporting evidence comes from experiments showing that enhanced COX 2/PGE2 levels mediate the histamine-induced tumor vascularization and proliferation [42].
Myeloid-derived suppressor cells (MDSC) expressing CXCR2 can be recruited to the developing tumor by CXCL1 and CXCL2 [38], possibly induced by PGE2 [44]. MDSC are essential for tumor development, since they dampen the immune reaction against the tumor, e.g., by inhibition of CD8+ T cell activity [38]. MDSC express the histamine receptors H1R, H2R, and H3R [45]. Expression of H4R was not detected [45], while the H4R was readily detected in CRC-containing tissue [46]. Thus, a direct effect of histamine via H4R on MDSC can be excluded, suggesting that histamine via the H4R may promote tumorigenesis by indirectly enhancing the MDSC’s activity via epithelial cell-produced CXCL1 and CXCL2, or by a different mechanism not involving MDSC. Nevertheless, these hypotheses are in contrast to publications providing evidence for a MDSC-mediated CRC suppressing effect of histamine [47,48,49,50]. These studies, however, did not analyze the histamine receptor subtypes involved. Other publications indicate that histamine promotes the MDSC activity via H1R and H2R [45]. The overall role and effect of histamine on CRC development is discussed highly controversially, ranging from a proposed MDSC-mediated CRC suppression [46,47,48,49] to histamine-driven promotion of MDSC activity via H1R and H2R, which would result in hampered tumor progression [44]. Therefore, the CRC-promoting effect of the H4R we report here most probably is not mediated via an enhanced activity of MDSC.
In summary, we have provided evidence that the presence of the H4R, most likely in epithelial cells [51], is necessary for the tumorigenesis in a mouse model of chemically-induced colorectal carcinoma. The mechanisms at the heart of this observation involve COX 2 expression and probably the production of the pro-inflammatory mediators CXCL1 and CXCL2. Further details, however, still have to be explored.
4. Materials and Methods
4.1. Materials
If not stated otherwise, all chemicals were obtained from Sigma-Aldrich (Munich, Germany).
4.2. Animals
BALB/cJRj (WT) mice were purchased from Janvier Labs. Mice with deletion of functional H4R expression due to a targeted mutation of the H4R gene (TM; strain: C.129HrH4tm1Lex), generated by Lexicon Genetics (Woodlands, TX, USA) and described by Hofstra et al. [11], were backcrossed for more than 10 generations onto the BALB/cJRj strain. All animals were bred and maintained at the central animal facility of Hannover Medical School in a standardized environment (temperature: 21 °C +/− 1 °C; 14/10-h day/night cycle). They had access to standard diet (Altromin 1310, Altromin special diet, Lage, Germany) and drinking water ad libitum. The hygienic status of the mice was determined routinely according to the FELASA-guidelines to ensure absence of mouse pathogens. For the experiments, female mice of 10–20 weeks of age, randomly assigned to the experimental groups, were used.
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. The study was conducted in accordance with the German law for animal protection (TierSchG) and with the European Directive 2010/63/EU. All experiments were approved by the Local Institutional Animal Care and Research Advisory Committee and permitted by the local government (AZ 33.12-42502-04-16/2197; July 29, 2016).
4.3. Induction of CRC by AOM/DSS and Animal Dissection
For induction of CRC, mice were injected intraperitoneally once with AOM (10 mg/kg body weight) at day 0 and then fed for three cycles with water charged with 2.0% (w/v) DSS as depicted in Figure 1a. The first and second DSS cycle lasted for 7 days. The third cycle was terminated already after 5 days, since otherwise some mice probably would have had to be excluded from the experiment due to severely impaired health conditions. In the periods between the DSS cycles the mice received pure drinking water. AOM-treated but water-only fed mice served as control. Mice were inspected daily as detailed in Section 2.4. On day 68 the animals were euthanized with carbon dioxide insufflation and subsequent heart puncture to draw blood for sera preparation using Serum Gel Z/1.1 tubes (Sarstedt, Nümbrecht, Germany). Colon specimen were resected, washed with PBS to remove remaining feces, opened longitudinally, and photographically documented. Afterwards, colon tissues were divided longitudinally, and one part was processed for histological examination (see below), while the other part was divided into tumor-bearing and non-tumor-bearing sections and stored in RNA later (Thermo Fisher Scientific, Waltham, MA, USA).
4.4. Evaluation of Disease Activity
Mice were examined at 24-hour intervals using a common clinical score and a disease activity index (DAI, adopted from Alex et al. [52]) ranging from 0 to 12 was employed. The DAI was based on total body weight loss (0: no weight loss, 1: ≤5%, 2: ≤10%, 3: ≤15%, 4: >15%), stool consistency (0: normal, 2: soft, 4: diarrhea) and perianal bleeding (0: no bleeding, 2: little bleeding, 4: massive bleeding).
4.5. Histology
The respective parts of the colon tissues were fixed in 4% (v/v) formaldehyde (Merck, Darmstadt, Germany), embedded in paraffin, sliced, and stained with hematoxylin/eosin (H/E). Stained tissue slices were analyzed in a blinded fashion by two pathologists. A histological severity score was calculated by evaluating the severity (leukocyte density and area of affected lamina propria: 0: normal, 1: minimal (<10%), 2: mild (10–25%), 3: moderate (26–50%), 4: marked (>51%)) and the extent (expansion of leukocyte infiltration: 0: normal, 1: mucosal, 2: submucosal, 3: transmural) of the inflammatory cell infiltrate, mucosal hyperplasia (increase in epithelial cell numbers in longitudinal crypts: 0: normal, 1: minimal <25%, 2: mild 25–35%, 3: moderate 36–50%, 4: marked > 51%) and goblet cell loss (0: normal, 1: minimal: < 20%, 2: mild: 21–35%, 3: moderate: 36–50%, 4: marked >50%). The maximum theoretical score sums up to 15 points [53]. Further, the presence or absence of cancer as well as predominantly polypoid tumors was evaluated. Reported are the values obtained by the analyses of tumor-proximal areas.
4.6. Soluble Mediator Protein Quantification
Portions (~30 mg) of the RNA later-stored colon tissues were lysed in RIPA buffer containing proteases by sonification and 30 minutes of rotation at 4 °C. Aggregates were removed by centrifugation (20 min, 10,000× g, 4 °C) and protein concentration in the supernatants was measured using the Pierce BCA protein assay (Thermo Fisher Scientific). Quantification of cytokine concentrations in the supernatants was carried out using the Magnetic Luminex Screening Assay (R&D Systems, Minneapolis, MN, USA). The kit quantified the cytokines KC/CXCL1, MIP-2/CXCL2, MCP-1/CCL2, IL-12p70, IL-1β, IL-5, IL-10, IFNγ, TNF, IL-6, IL-17A, and IL-23p19.
4.7. Soluble Mediator mRNA Quantification
Portions (~30 mg) of the RNA later-stored tissues were homogenized using the FastPrep-24 device (MP Biochemicals, Irvine, CA, USA). RNA was extracted from the homogenates using the Nucleospin RNA II kit (Macherey-Nagel, Düren, Germany) essentially according to the manufacturer’s instructions. One µg RNA of each sample was reversely transcribed for 30 min at 50 °C into cDNA by means of Maxima Reverse Transcriptase (Thermo Fisher Scientific). Target gene-specific sequences were quantified proportionately to glycerin aldehyde-3-phosphate dehydrogenase (GAPDH) by real-time PCR using TaqMan Gene Expression Assays (ABI; Thermo Fisher Scientific). The reported relative gene expression data were calculated by relating the obtained qPCR data of corresponding tumor bearing and not tumor bearing sections by the ΔΔCT method.
4.8. Statistical Analysis
Data are represented as arithmetic means ± SD for each parameter. Statistical analyses were performed with GraphPad Prism version 6.07 (GraphPad Software, La Jolla, CA, USA), using ANOVA with Sidak’s post hoc test.
5. Conclusions
We conclude that histamine via the H4R promotes tumorigenesis in a mouse model of CRC. Whether this provides new therapeutic targets has to be evaluated in the future.
Acknowledgments
H4R−/− mice were generated by Lexicon Genetics, Woodland, Texas, USA, as described by Hofstra et al. (J Pharmacol Exp Ther 2003, 305:1212).
Supplementary Materials
The following are available online at https://www.mdpi.com/2072-6694/12/4/912/s1, Figure S1: Colon tissues prepared out of the mice described in Figure 1 were fixed in buffered formalin, embedded in paraffin, and sliced into histological sections. Sections were stained for either CD 3 (Dako, Code A 0452, Copenhagen, Denmark) or CD 22 (Zytomed Systems Cat.-No 503, Berlin, Germany) and counterstained with haemalaun. Shown are representative photographs of the immunohistochemical analyses. WT: wild type, TM: H4R−/−, ctr: AOM-treated mice, CRC: AOM/DSS-treated mice.
Author Contributions
Conceptualization, B.S., A.B., D.J., R.S., and D.N.; investigation, B.S., T.R., I.B., C.W., and D.N.; writing—original draft preparation, D.N.; writing—review and editing, B.S., T.R., I.B., C.W., R.S., and D.N.; project administration, A.B., D.J., and D.N. All authors have read and agreed to publish the version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Xie H., He S.H. Roles of histamine and its receptors in allergic and inflammatory bowel diseases. World J. Gastroenterol. 2005;11:2851–2857. doi: 10.3748/wjg.v11.i19.2851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Oda T., Morikawa N., Saito Y., Masuho Y., Matsumoto S. Molecular cloning and characterization of a novel type of histamine receptor preferentially expressed in leukocytes. J. Biol. Chem. 2000;275:36781–36786. doi: 10.1074/jbc.M006480200. [DOI] [PubMed] [Google Scholar]
- 3.Liu C., Ma X., Jiang X., Wilson S.J., Hofstra C.L., Blevitt J., Pyati J., Li X., Chai W., Carruthers N., et al. Cloning and pharmacological characterization of a fourth histamine receptor (H4) expressed in bone marrow. Mol. Pharmacol. 2001;59:420–426. doi: 10.1124/mol.59.3.420. [DOI] [PubMed] [Google Scholar]
- 4.Zhu Y., Michalovich D., Wu H., Tan K.B., Dytko G.M., Mannan I.J., Boyce R., Alston J., Tierney L.A., Li X., et al. Cloning, expression, and pharmacological characterization of a novel human histamine receptor. Mol. Pharmacol. 2001;59:434–441. doi: 10.1124/mol.59.3.434. [DOI] [PubMed] [Google Scholar]
- 5.Nguyen T., Shapiro D.A., George S.R., Setola V., Lee D.K., Cheng R., Rauser L., Lee S.P., Lynch K.R., Roth B.L., et al. Discovery of a novel member of the histamine receptor family. Mol. Pharmacol. 2001;59:427–433. doi: 10.1124/mol.59.3.427. [DOI] [PubMed] [Google Scholar]
- 6.Morse K.L., Behan J., Laz T.M., West R.E., Greenfeder S.A., Anthes J.C., Umland S., Wan Y., Hipkin R.W., Gonsiorek W., et al. Cloning and characterization of a novel human histamine receptor. J. Pharmacol. Exp. Ther. 2001;296:1058–1066. [PubMed] [Google Scholar]
- 7.Reher T.M., Neumann D., Buschauer A., Seifert R. Incomplete activation of human eosinophils via the histamine H4-receptor: Evidence for ligand-specific receptor conformations. Biochem. Pharmacol. 2012;84:192–203. doi: 10.1016/j.bcp.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 8.Jutel M., Akdis M., Akdis C.A. Histamine, histamine receptors and their role in immune pathology. Clin. Exp. Allergy. 2009;39:1786–1800. doi: 10.1111/j.1365-2222.2009.03374.x. [DOI] [PubMed] [Google Scholar]
- 9.Jutel M., Watanabe T., Klunker S., Akdis M., Thomet O.A., Malolepszy J., Zak-Nejmark T., Koga R., Kobayashi T., Blaser K., et al. Histamine regulates T-cell and antibody responses by differential expression of H1 and H2 receptors. Nature. 2001;413:420–425. doi: 10.1038/35096564. [DOI] [PubMed] [Google Scholar]
- 10.Cowden J.M., Yu F., Banie H., Farahani M., Ling P., Nguyen S., Riley J.P., Zhang M., Zhu J., Dunford P.J., et al. The histamine H4 receptor mediates inflammation and Th17 responses in preclinical models of arthritis. Ann. Rheum. Dis. 2014;73:600–608. doi: 10.1136/annrheumdis-2013-203832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hofstra C.L., Desai P.J., Thurmond R.L., Fung-Leung W.-P.P. Histamine H4 receptor mediates chemotaxis and calcium mobilization of mast cells. J. Pharmacol. Exp. Ther. 2003;305:1212–1221. doi: 10.1124/jpet.102.046581. [DOI] [PubMed] [Google Scholar]
- 12.Hartwig C., Munder A., Glage S., Wedekind D., Schenk H., Seifert R., Neumann D. The histamine H4-receptor (H4R) regulates eosinophilic inflammation in ovalbumin-induced experimental allergic asthma in mice. Eur. J. Immunol. 2015;45:1129–1140. doi: 10.1002/eji.201445179. [DOI] [PubMed] [Google Scholar]
- 13.Gutzmer R., Mommert S., Gschwandtner M., Zwingmann K., Stark H., Werfel T. The histamine H4 receptor is functionally expressed on TH2 cells. J. Allergy Clin. Immunol. 2009;123:619–625. doi: 10.1016/j.jaci.2008.12.1110. [DOI] [PubMed] [Google Scholar]
- 14.Cowden J.M., Zhang M., Dunford P.J., Thurmond R.L. The histamine H4 receptor mediates inflammation and pruritus in Th2-dependent dermal inflammation. J. Invest. Dermatol. 2010;130:1023–1033. doi: 10.1038/jid.2009.358. [DOI] [PubMed] [Google Scholar]
- 15.Bernstein C.N., Blanchard J.F., Kliewer E., Wajda A. Cancer risk in patients with inflammatory bowel disease: A population-based study. Cancer. 2001;91:854–862. doi: 10.1002/1097-0142(20010215)91:4<854::AID-CNCR1073>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 16.Bernstein C., Blanchard J., Rawsthorne P., Yu N. The prevalence of extraintestinal diseases in inflammatory bowel disease: A population-based study. Am. J. Gastroenterol. 2001;96:1116–1122. doi: 10.1111/j.1572-0241.2001.03756.x. [DOI] [PubMed] [Google Scholar]
- 17.Ferlay J., Soerjomataram I., Dikshit R., Eser S., Mathers C., Rebelo M., Parkin D.M., Forman D., Bray F. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer. 2015;136:E359–E386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 18.Favoriti P., Carbone G., Greco M., Pirozzi F., Pirozzi R.E.M., Corcione F. Worldwide burden of colorectal cancer: A review. Updates Surg. 2016;68:7–11. doi: 10.1007/s13304-016-0359-y. [DOI] [PubMed] [Google Scholar]
- 19.Groden J., Thliveris A., Samowitz W., Carlson M., Gelbert L., Albertsen H., Joslyn G., Stevens J., Spirio L., Robertson M., et al. Identification and characterization of the familial adenomatous polyposis coli gene. Cell. 1991;66:589–600. doi: 10.1016/0092-8674(81)90021-0. [DOI] [PubMed] [Google Scholar]
- 20.Rowan A.J., Lamlum H., Ilyas M., Wheeler J., Straub J., Papadopoulou A., Bicknell D., Bodmer W.F., Tomlinson I.P.M. APC mutations in sporadic colorectal tumors: A mutational “hotspot” and interdependence of the “two hits”. Proc. Natl. Acad. Sci. USA. 2000;97:3352–3357. doi: 10.1073/pnas.97.7.3352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Burn J., Gerdes A.M., MacRae F., Mecklin J.P., Moeslein G., Olschwang S., Eccles D., Evans D.G., Maher E.R., Bertario L., et al. Long-term effect of aspirin on cancer risk in carriers of hereditary colorectal cancer: An analysis from the CAPP2 randomised controlled trial. Lancet. 2011;378:2081–2087. doi: 10.1016/S0140-6736(11)61049-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chan A.T., Lippman S.M. Aspirin and colorectal cancer prevention in Lynch syndrome. Lancet. 2011;378:2051–2052. doi: 10.1016/S0140-6736(11)61216-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Johansson M.E.V. Mucus layers in inflammatory bowel disease. Inflamm. Bowel Dis. 2014;20:2124–2161. doi: 10.1097/MIB.0000000000000117. [DOI] [PubMed] [Google Scholar]
- 24.Wirtz S., Neufert C., Weigmann B., Neurath M.F. Chemically induced mouse models of intestinal inflammation. Nat. Protoc. 2007;2:541–546. doi: 10.1038/nprot.2007.41. [DOI] [PubMed] [Google Scholar]
- 25.Eichele D.D., Kharbanda K.K. Dextran sodium sulfate colitis murine model: An indispensable tool for advancing our understanding of inflammatory bowel diseases pathogenesis. World J. Gastroenterol. 2017;23:6016–6029. doi: 10.3748/wjg.v23.i33.6016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fournier B.M., Parkos C.A. The role of neutrophils during intestinal inflammation. Mucosal Immunol. 2012;5:354–366. doi: 10.1038/mi.2012.24. [DOI] [PubMed] [Google Scholar]
- 27.Roberts-Thomson I.C., Fon J., Uylaki W., Cummins A.G., Barry S. Cells, cytokines and inflammatory bowel disease: A clinical perspective. Expert Rev. Gastroenterol. Hepatol. 2011;5:703–716. doi: 10.1586/egh.11.74. [DOI] [PubMed] [Google Scholar]
- 28.Sasaki Y., Tanaka M., Kudo H. Differentiation between ulcerative colitis and Crohn’s disease by a quantitative immunohistochemical evaluation of T lymphocytes, neutrophils, histiocytes and mast cells. Pathol. Int. 2002;52:277–285. doi: 10.1046/j.1440-1827.2002.01354.x. [DOI] [PubMed] [Google Scholar]
- 29.Raithel M., Matek M., Baenkler H.W., Jorde W., Hahn E.G. Mucosal histamine content and histamine secretion in Crohn’s disease, ulcerative colitis and allergic enteropathy. Int. Arch. Allergy Immunol. 1995;108:127–133. doi: 10.1159/000237129. [DOI] [PubMed] [Google Scholar]
- 30.Wechsler J.B., Szabo A., Hsu C.L., Krier-Burris R.A., Schroeder H.A., Wang M.Y., Carter R.G., Velez T.E., Aguiniga L.M., Brown J.B., et al. Histamine drives severity of innate inflammation via histamine 4 receptor in murine experimental colitis. Mucosal Immunol. 2018;11:861–870. doi: 10.1038/mi.2017.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schirmer B., Bringmann L., Seifert R., Neumann D. In vivo evidence for partial activation of eosinophils via the histamine H4-receptor: Adoptive transfer experiments using eosinophils from H4R−/− and H4R+/+ mice. Front. Immunol. 2018;9:2119. doi: 10.3389/fimmu.2018.02119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bene L., Sápi Z., Bajtai A., Buzás E., Szentmihályi A., Arató A., Tulassay Z., Falus A. Partial protection against dextran sodium sulphate induced colitis in histamine-deficient, histidine decarboxylase knockout mice. J. Pediatr Gastroenterol. Nutr. 2004;39:171–176. doi: 10.1097/00005176-200408000-00009. [DOI] [PubMed] [Google Scholar]
- 33.Schirmer B., Rezniczek T., Seifert R., Neumann D. Proinflammatory role of the histamine H4 receptor in dextrane sodium sulfate-induced acute colitis. Biochem. Pharmacol. 2015;98:102–109. doi: 10.1016/j.bcp.2015.09.006. [DOI] [PubMed] [Google Scholar]
- 34.Tanaka T., Kochi T., Shirakami Y., Mori T., Kurata A., Watanabe N., Moriwaki H., Shimizu M. Cimetidine and clobenpropit attenuate inflammation-associated colorectal carcinogenesis in male ICR Mice. Cancers (Basel) 2016;8:25. doi: 10.3390/cancers8020025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sterle H.A., Nicoud M.B., Massari N.A., Táquez Delgado M.A., Herrero Ducloux M.V., Cremaschi G.A., Medina V.A. Immunomodulatory role of histamine H4 receptor in breast cancer. Br. J. Cancer. 2018;120:128–138. doi: 10.1038/s41416-018-0173-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Oppenheim J.J., Zachariae C.O.C., Mukaida N., Matsushima K. Properties of the Novel Proinflammatory Supergene “Intercrine” Cytokine Family. Annu. Rev. Immunol. 2003;9:317–348. doi: 10.1146/annurev.iy.09.040191.003153. [DOI] [PubMed] [Google Scholar]
- 37.Van Damme J., Wuyts A., Froyen G., Van Coillie E., Struyf S., Billiau A., Proost P., Wang J.M., Opdenakker G. Granulocyte chemotactic protein-2 and related CXC chemokines: From gene regulation to receptor usage. J. Leukoc. Biol. 1997;62:563–569. doi: 10.1002/jlb.62.5.563. [DOI] [PubMed] [Google Scholar]
- 38.Katoh H., Wang D., Daikoku T., Sun H., Dey S.K., DuBois R.N. CXCR2-Expressing Myeloid-Derived Suppressor Cells Are Essential to Promote Colitis-Associated Tumorigenesis. Cancer Cell. 2013;24:631–644. doi: 10.1016/j.ccr.2013.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sipos F., Germann T.M., Wichmann B., Galamb O., Spisák S., Krenács T., Tulassay Z., Molnár B., Muzes G. MMP3 and CXCL1 are potent stromal protein markers of dysplasia-carcinoma transition in sporadic colorectal cancer. Eur. J. Cancer Prev. 2014;23:336–343. doi: 10.1097/CEJ.0000000000000058. [DOI] [PubMed] [Google Scholar]
- 40.Jamieson T., Clarke M., Steele C.W., Samuel M.S., Neumann J., Jung A., Huels D., Olson M.F., Das S., Nibbs R.J.B., et al. Inhibition of CXCR2 profoundly suppresses inflammation-driven and spontaneous tumorigenesis. J. Clin. Invest. 2012;122:3127–3144. doi: 10.1172/JCI61067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jaén R.I., Prieto P., Casado M., Martín-Sanz P., Boscá L. Post-translational modifications of prostaglandin-endoperoxide synthase 2 in colorectal cancer: An update. World J. Gastroenterol. 2018;24:5454–5461. doi: 10.3748/wjg.v24.i48.5454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cianchi F., Cortesini C., Schiavone N., Perna F., Magnelli L., Fanti E., Bani D., Messerini L., Fabbroni V., Perigli G., et al. The role of cyclooxygenase-2 in mediating the effects of histamine on cell proliferation and vascular endothelial growth factor production in colorectal cancer. Clin. Cancer Res. 2005;11:6807–6815. doi: 10.1158/1078-0432.CCR-05-0675. [DOI] [PubMed] [Google Scholar]
- 43.Wang D., Wang H., Brown J., Daikoku T., Ning W., Shi Q., Richmond A., Strieter R., Dey S.K., DuBois R.N. CXCL1 induced by prostaglandin E2 promotes angiogenesis in colorectal cancer. J. Exp. Med. 2006;203:941–951. doi: 10.1084/jem.20052124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sinha P., Clements V.K., Fulton A.M., Ostrand-Rosenberg S. Prostaglandin E2 promotes tumor progression by inducing myeloid-derived suppressor cells. Cancer Res. 2007;67:4507–4513. doi: 10.1158/0008-5472.CAN-06-4174. [DOI] [PubMed] [Google Scholar]
- 45.Martin R.K., Saleem S.J., Folgosa L., Zellner H.B., Damle S.R., Nguyen G.-K.T., Ryan J.J., Bear H.D., Irani A.-M., Conrad D.H. Mast cell histamine promotes the immunoregulatory activity of myeloid-derived suppressor cells. J. Leukoc. Biol. 2014;96:151–159. doi: 10.1189/jlb.5A1213-644R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fang Z., Yao W., Xiong Y., Li J., Liu L., Shi L., Zhang W., Zhang C., Nie L., Wan J. Attenuated expression of HRH4 in colorectal carcinomas: A potential influence on tumor growth and progression. BMC Cancer. 2011;11:1–11. doi: 10.1186/1471-2407-11-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yang J.J., Ma Y.L., Zhang P., Chen H.Q., Liu Z.H., Qin H.L. Histidine decarboxylase is identified as a potential biomarker of intestinal mucosal injury in patients with acute intestinal obstruction. Mol. Med. 2011;17:1323–1337. doi: 10.2119/molmed.2011.00107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chen X., Churchill M.J., Nagar K.K., Tailor Y.H., Chu T., Rush B.S., Jiang Z., Wang E.B.C., Renz B.W., Wang H., et al. IL-17 producing mast cells promote the expansion of myeloid-derived suppressor cells in a mouse allergy model of colorectal cancer. Oncotarget. 2015;6:32966–32979. doi: 10.18632/oncotarget.5435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gao C., Ganesh B.P., Shi Z., Shah R.R., Fultz R., Major A., Venable S., Lugo M., Hoch K., Chen X., et al. Gut microbe–mediated suppression of inflammation-associated colon carcinogenesis by luminal histamine production. Am. J. Pathol. 2017;187:2323–2336. doi: 10.1016/j.ajpath.2017.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Grauers Wiktorin H., Nilsson M.S., Kiffin R., Sander F.E., Lenox B., Rydström A., Hellstrand K., Martner A. Histamine targets myeloid-derived suppressor cells and improves the anti-tumor efficacy of PD-1/PD-L1 checkpoint blockade. Cancer Immunol. Immunother. 2019;68:163–174. doi: 10.1007/s00262-018-2253-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schirmer B., Lindemann L., Bittkau K.S., Isaev R., Bösche D., Juchem M., Seifert R., Neumann D. Mouse colonic epithelial cells functionally express the histamine H4 receptor. J. Pharmacol. Exp. Ther. 2020 doi: 10.1124/jpet.119.264408. [DOI] [PubMed] [Google Scholar]
- 52.Alex P., Zachos N.C., Nguyen T., Gonzales L., Chen T.E., Conklin L.S., Centola M., Li X. Distinct cytokine patterns identified from multiplex profiles of murine DSS and TNBS-induced colitis. Inflamm. Bowel Dis. 2009;15:341–352. doi: 10.1002/ibd.20753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Erben U., Loddenkemper C., Doerfel K., Spieckermann S., Haller D., Heimesaat M.M., Zeitz M., Siegmund B., Kühl A.A. A guide to histomorphological evaluation of intestinal inflammation in mouse models. Int. J. Clin. Exp. Pathol. 2014;7:4557–4576. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.