Abstract
Patient: Female, 53-year-old
Final Diagnosis: Calcified esophageal leiomyoma
Symptoms: Dysphagia
Medication:—
Clinical Procedure: Right video-assisted thoracoscopic enucleation
Specialty: Surgery
Objective:
Rare disease
Background:
Benign esophageal tumors are considered rare, and most commonly are leiomyomas with the incidence of 0.005%. They arise intramurally in the distal two-thirds of the esophagus and are multiple in about 5% of patients. Leiomyoma lesions can mimic esophageal cancer making the diagnosis more challenging. Many cases are asymptomatic, up to 15%–50%, and most cases are discovered incidentally during esophagogastroduodenoscopy (EGD) and other procedures. The treatment of choice for symptomatic leiomyomas to relieve the compression is surgical enucleation with either an open thoracotomy, submucosal tunneling endoscopic resection, a video-assisted thoracoscopic approach (VATS), or with robotic techniques.
Case Report:
Here we report a case of a 53-year-old Saudi female patient who presented with dysphagia which had been ongoing for a long time. There were no other associated symptoms such as dyspepsia, nausea, or vomiting. She was diagnosed with a calcified leiomyoma of the esophagus based on a computed tomography (CT) scan and an endoscopic ultrasound (EUS) finding. After thorough investigations and workups, the management plan was taken at King Faisal Specialist Hospital and Research Centre by preforming a right video-assisted thoracoscopic enucleation.
Conclusions:
The aim of this case report was to add to the literature by reporting the satisfactory outcomes of right video-assisted enucleation contrary to other surgical approaches that have been discussed in the literature.
MeSH Keywords: Esophageal Neoplasms; Leiomyoma; Thoracic Surgery; Thoracic Surgery, Video-Assisted
Background
Leiomyomas are considered common benign esophageal lesions with the incidence of 0.005% [1]. They arise intramurally most commonly in the distal two-thirds of the esophagus and are multiple in about 5% of patients. Leiomyoma lesions can mimic esophageal cancer making the diagnosis more challenging [2]. Many cases are asymptomatic up, to 15–50%, and most cases are discovered incidentally during esophagogastroduodenoscopy (EGD) and other procedures. On the other hand, massively large and calcified lesions present with dysphagia, dyspepsia, chest pain, and weight loss [1]. The treatment of choice for symptomatic leiomyomas is surgical enucleation with either an open thoracotomy, submucosal tunneling endoscopic resection, a video-assisted thoracoscopic approach (VATS), or with robotic techniques, while small and asymptomatic lesions are left untreated with repeated endoscopies in every follow-up [2–5].
Case Report
A 53-year-old Saudi female patient presented with a progressive dysphagia which had been ongoing for a long time. There were no other associated symptoms such as dyspepsia, nausea, or vomiting. She was diagnosed with a calcified leiomyoma of the esophagus based on a computed tomography (CT) scan and an endoscopic ultrasound (EUS) finding. She had a known case of fibromyalgia for which she was taking acetaminophen (650 mg, orally, as needed) and amitriptyline (5 mg, orally, daily). She was otherwise healthy and medically free. She did not smoke nor is a second-hand smoker. There was no history of drug abuse, and travel history was insignificant. The rest of her history was unremarkable. Physical examinations were all within the normal limits.
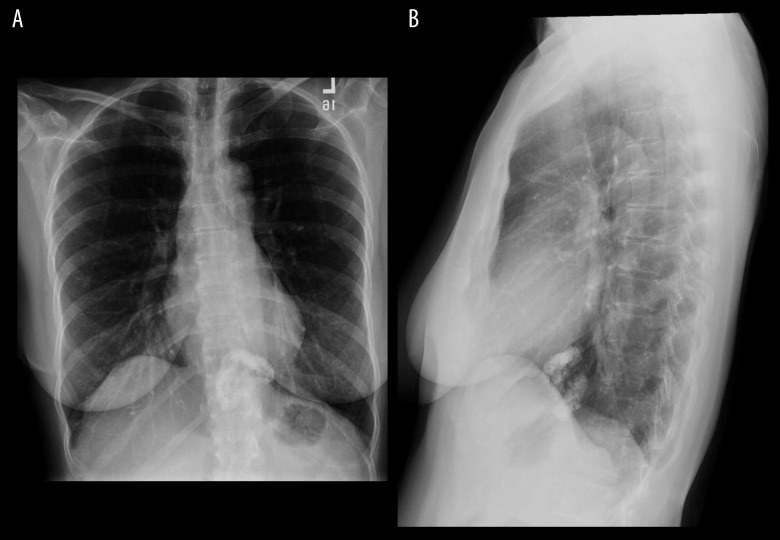
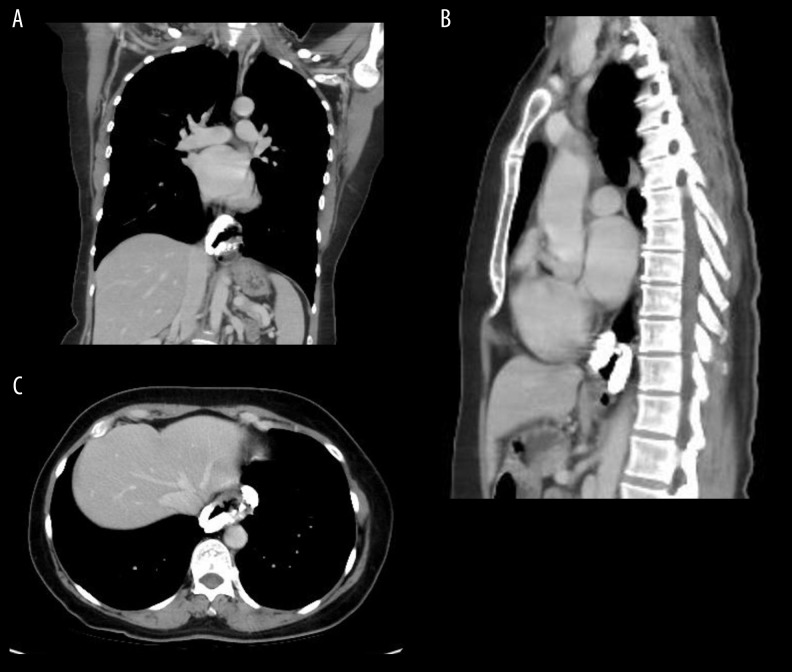
For further investigation, the patient underwent a chest x-ray that showed a thick ring like calcification in the lower esophagus (Figure 1A, 1B). A CT scan of the chest was ordered to confirm the findings and showed a ring like calcifications surrounding the lower esophagus near to the gastroesophageal junction with maximum thickness of 1 cm. The calcification was probably within the submucosal space without intraluminal extension (Figure 2A–2C). On May 20, 2019, the patient underwent a right video-assisted thoracoscopic surgery (VATS), which was made with a 3 cm utility incision at the 8th intercostal space just above the diaphragm and a 5 mm port at the 4th intercostal space to retract the lung anteriorly.
Figure 1.
(A, B) Chest x-ray shows a thick ring like calcification in the lower esophagus.
Figure 2.
(A–C) Computed tomography scans show calcifications surrounding the lower esophagus near to the gastroesophageal junction.
The diaphragmatic suture was made to retract the diaphragm and to visualize the hiatus and lower esophagus clearly. Before closing up, an endoscopy was inserted after the enucleation that showed an intact mucosa with no esophageal perforation (Figure 3). Postoperatively, the procedure was tolerated very well, and the patient was on NPO (nothing by mouth) for 48 hours. After that, a contrast swallow was done before starting the oral diet in order to shift the patient onto a soft diet safely, which resulted in significant improvement. She was discharged 3 days later on a soft diet for 3 weeks and was prescribed Tylenol (650 mg, orally), and codeine (650 mg, orally). On the pathological report, smooth muscle actin (SMA) immunohistochemistry showed positive desmin and SMA.
Figure 3.

Gross calcified esophageal leiomyoma specimen (7×5×2 cm).
Discussion
Benign esophageal tumors are considered rare, and most commonly are leiomyomas with the incidence of 0.005%. Many cases are asymptomatic, up, to 15–50%; thus, the exact incidence ratio may be higher [1]. Leiomyomas are discovered incidentally during esophagogastroduodenoscopy (EGD) procedures and the presence of calcifications within the tumor is a useful finding to prove that it is a benign lesion [1,6]. However, large and calcified tumors will be symptomatic, causing the patient to present with dysphagia, dyspepsia, chest pain, and weight loss. Surgical enucleation of the tumor to relieve the compression symptoms is curative, including an open thoracotomy, submucosal tunneling endoscopic resection, a video-assisted thoracoscopic approach (VATS), and robotic techniques [1,3,5]. Among all approaches, the literature recommends the VAS enucleation as it decreases the pain post-operatively and the length of hospital stay, contrary to other approaches [7].
One of the first cases of calcified leiomyoma was reported in the literature during the year 1972 in the United States. Unfortunately, the patient died after 4 hours of admission, hence no investigations nor surgical interventions were made. The postmortem examination revealed an intramural calcified leiomyoma in the distal esophagus at the anterior wall [8]. Apart from that case, 3 more cases of a massive calcified esophageal leiomyomas were reported and managed successfully with different surgical approaches in the United States in the years 2013, 2014, and 2016. The first of these three cases was managed uneventfully with a surgical myotomy resection and was followed up for 1 year with no complications. The second case underwent a minimally invasive thoracoscopic approach with the possibility of converting to a minimally esophagectomy. For the third a laparoscopic robotic distal paraoesophageal mass excision with an esophago-myotomy repair was performed. All thoracic procedures aforementioned were successful with no complications reported postoperatively [1,7,8]. Meanwhile, a completely calcified esophageal leiomyoma case was conducted in Italy in 2011. The patient underwent a right video-assisted mini-thoracotomy and a large leiomyoma was removed by dissection within the muscular wall of the esophagus leaving the mucosa intact and no complications reported [5].
Conclusions
The aim of this case report was to add more to the literature by reporting the satisfactory outcomes of right video-assisted enucleation contrary to other surgical approaches that were discussed in the literature [4]. It highlights the advantages of this technique as it decreases the pain post-operatively and the length of hospital stay, contrary to other approaches [7].
Footnotes
Conflict of interest
None.
References:
- 1.Jehangir A, Le B, Shogbesan O, Rosenzweig SE. Esophageal leiomyoma presenting as calcified esophageal mass. ACG Case Rep J. 2017;4:e41. doi: 10.14309/crj.2017.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Punpale A, Rangole A, Bhambhani N, et al. Leiomyoma of esophagus. Ann Thorac Cardiovasc Surg. 2007;13(2):78. [PubMed] [Google Scholar]
- 3.Xu MD, Cai MY, Zhou PH, et al. Submucosal tunneling endoscopic resection: A new technique for treating upper GI submucosal tumors originating from the muscularis propria layer (with videos) Gastrointest Endosc. 2012;75(1):195–99. doi: 10.1016/j.gie.2011.08.018. [DOI] [PubMed] [Google Scholar]
- 4.Bonavina L, Segalin A, Rosati R, et al. Surgical therapy of esophageal leiomyoma. J Am Coll Surg. 1995;181(3):257–62. [PubMed] [Google Scholar]
- 5.Tsagkaropoulos S, Francioni F, Telha V, De Giacomo T. A completely calcified esophageal leiomyoma. Ann Thorac Surg. 2011;91(4):1293. doi: 10.1016/j.athoracsur.2010.09.027. [DOI] [PubMed] [Google Scholar]
- 6.Macke RA, Luketich JD, Nason KS, Schuchert MJ. Minimally invasive enucleation of a large, extensively calcified esophageal leiomyoma. Ann Thorac Cardiovasc Surg. 2014;147(4):e52–54. doi: 10.1016/j.jtcvs.2013.12.054. [DOI] [PubMed] [Google Scholar]
- 7.Walters DM, Vaughn NH, Isbell JM, et al. Leiomyoma presenting as a massive calcified circumferential esophageal mass. Ann Thorac Surg. 2013;96(5):1851–54. doi: 10.1016/j.athoracsur.2013.01.097. [DOI] [PubMed] [Google Scholar]
- 8.Gutman E. Posterior mediastinal calcification due to esophageal leiomyoma. J Gastroenterol. 1972;63(4):665–66. [PubMed] [Google Scholar]