Abstract
Background. Although effective interventions for shared decision making (SDM) exist, there is a lack of uptake of these tools into clinical practice. “Nudges,” which draw on behavioral economics and target automatic thinking processes, are used by policy makers to influence population-level behavior change. Nudges have not been applied in the context of SDM interventions but have potential to influence clinician motivation, a primary barrier to long-term adoption of SDM tools. Objective. Describe, evaluate, and propose recommendations for the use of a behavioral economics framework (MINDSPACE) on clinician motivation and behavior during implementation of a validated decision aid (DA) for left ventricular assist device at nine hospitals. Methods. Qualitative thematic analysis of process notes from stakeholder meetings during the first 6 months of implementation to identify examples of how the MINDSPACE framework was operationalized. Quantitative implementation progress was evaluated using the RE-AIM framework. Results. MINDSPACE components were translated into concrete approaches that leveraged influential stakeholders, fostered ownership over the DA and positive emotional associations, spread desirable norms across sites, and situated the DA within established default processes. DA reach to eligible patients increased from 9.8% in the first month of implementation to 70.0% in the sixth month. Larger gains in reach were observed following meetings using MINDSPACE approaches. Limitations. The MINDSPACE framework does not capture all possible influences on behavior and responses to nudges may differ across populations. Conclusions. Behavioral economics can be applied to implementation science to foster uptake of SDM tools by increasing clinician motivation. Our recommendations can help other researchers effectively apply these approaches in real-world settings when there are often limited incentives and opportunities to change organizational- or structural-level factors.
Keywords: decision aids, shared decision making, behavioral economics, implementation
Introduction
Shared decision making (SDM) involves clinicians and patients together evaluating evidence of intervention risks and benefits, considering patients’ preferences, goals, values, and concerns, and arriving at a decision.1,2 Interventions to promote SDM, such as patient decision aids (DAs), have been developed and tested, particularly for elective surgery, cancer screening, and other preference sensitive decisions.3–5 Research shows that patient access to an evidence-based DA during decision making improves patient experiences, enhances informed consent, and can eliminate unwanted treatment.3 Despite the utility of many DAs, an “implementation gap” exists between their development and uptake in practice.6 A sizable literature, including three systematic reviews,7–9 has identified key barriers to implementing DAs in real-world contexts, namely, time constraints and a lack of applicability to patient characteristics and clinical situations, lack of physician training, physicians’ reluctance to utilize SDM, and lack of a supportive clinic culture. Previous research has shown that effective implementation strategies to move beyond these “many barriers” include making DA use “routine,” involving other members of the clinical team in delivering DAs,9,10 and identifying the complex interactions of structural and cultural influences on how and why DAs become routinely embedded in health care settings.8,11,12
At the intersection of these factors are individual actors responding in ways that are so far not well understood.9,13 There is a need for sustainable incentives for individuals to engage in adoption and use of a DA, but it should also be recognized that even successful behavioral changes can disappear once incentives are removed.14 To counter this, Elwyn and collegues9 argue that implementation methods must incorporate better understandings of what motivates individuals to use DAs in practice.
Application of Existing Implementation Frameworks in Research on Patient Decision Aids
Current implementation science frameworks have so far had little success in tackling the enduring challenges to successful implementation outlined above. While models like the Behavior Change Wheel,15 Theoretical Domains Framework,16 and Theory of Planned Behavior17 are useful for conceptualizing influences on behavior, we believe that many of them do not offer a clear set of “tools” for implementation (backed by theory) that can be easily understood and applied. For example, the Behavior Change Wheel framework does not offer ideas about how to use the intervention functions it highlights (e.g., education, restrictions, persuasion, etc.), leading to practical uncertainties about how to effectively apply the model. Despite the existence of numerous conceptual frameworks for implementation science, few have been used to evaluate DA implementation,9 and little evidence exists as to how they can be leveraged to create tangible strategies for interventions targeting SDM.18
Furthermore, many existing intervention functions operate in an “outside-in” fashion. Intervention tools such as “education,”“training,” and “persuasion” are mechanisms of an external environment that are assessed and acted upon by an individual, most often involving conscious reflection. A vast and growing literature in behavioral economics and decision-making psychology, however, suggests that more lasting behavioral changes enlist dynamics that are internal to an individual, involving “automatic” thought processes. In line with the widely endorsed dual process theory,19–22 the automatic system is one of two cognitive systems we use to process information and is faster, more unconscious, and more associative than our reflective system that is more time- and resource-intensive, as it requires conscious reflection and hypothesis testing.20–22 Implementation approaches that appeal to the reflective rather than automatic system—for example, “informational” interventions that primarily rely on “education” or “persuasion”—are likely to encounter resistance from default, habitual ways of thinking and behaving (the “bounded rationality”)23 of actors in the implementation environment. Working against these entrenched mental and behavioral pathways is precisely what makes affecting behavioral change such an enduring challenge.
Behavioral Economics and Nudges
A potentially more effective and sustainable approach to implementation of SDM programs comes from a growing literature on “nudging.” According to Thaler and Sunstein,24 nudges are choices and strategies for presenting them in ways that alter people’s behavior in predictable ways without forbidding options or significantly changing economic incentives. Nudges target automatic thinking processes in ways that are sometimes outside of conscious awareness but can be influential for long-term behavioral changes.25 While nudging has been effectively used by governments to influence population health- and environment-related behaviors,26,27 it has not been widely applied in implementation research.
We propose applying the MINDSPACE behavior change toolkit to target behavior change (in this case, use of SDM and DAs) in the implementation context. MINDSPACE builds on decades of empirical findings from behavioral economics about factors that are most influential in bringing about positive behavioral changes and explicitly focuses on automatic or context-based drivers of behavior. This approach is based on a robust literature demonstrating that actors do not always respond in “rational” ways to information intended to influence their behaviors. Instead, influencing the automatic system via altering contextual influences may be more long-lasting and cost-effective than relying exclusively on information-based interventions.28 The toolkit contains nine noncoercive influences, including Messenger, Incentives, Norms, Defaults, Salience, Priming, Affect, Commitment, and Ego (Table 1).26 While these elements do not exhaust the full range of behavior change tools, they do incorporate the primary tools of nudging described above, which are elaborated below with regard to how they may be used in the implementation context.
Table 1.
Elements of the MINDSPACE Toolkita
| Messenger | We are heavily influenced by who communicates information |
| Incentives | Our responses to incentives are shaped by predictable mental shortcuts such as strongly avoiding losses |
| Norms | We are strongly influenced by what others do |
| Defaults | We “go with the flow” of preset options |
| Salience | Our attention is drawn to what is novel and seems relevant to us |
| Priming | Our acts are often influenced by subconscious cues |
| Affect | Our emotional associations can powerfully shape our actions |
| Commitments | We seek to be consistent with our public promises, and reciprocate acts |
| Ego | We act in ways that make us feel better about ourselves |
Reproduced from Dolan et al.26(p8)
Why Nudge?
Expanding on this rationale, we chose a nudging approach targeted at clinician stakeholders for two main reasons. First, implementing a DA requires physicians and clinic staff to do more than simply “hand out” the DA to patients and caregivers. To implement with fidelity and efficacy, clinicians and staff must review it with patients in a context supportive of SDM entailing significant buy-in and motivation among clinicians and staff.29 Enhancing these two crucial elements may be more effectively accomplished using intervention tools that operate on automatic rather than reflective thought processes, as the former have been shown to have more lasting effects on behavior change.30
Second, given that it is not always realistically feasible to provide continuous, short-term (e.g., monetary) incentives to sustain actors’ motivations, nor to institute large-scale changes to organizational structures that would promote use of DAs, our “best shot” at changing physicians’ and clinic staff members’ long-term engagement is to try to positively affect their motivations for using a DA. The MINDSPACE tools allow implementers to initiate small attitudinal, emotional, or behavioral responses that can collectively help bring about lasting, positive behavioral change.
This article aims to describe how we used the MINDSPACE approach with clinicians to implement a validated DA for left ventricular assist device (LVAD) therapy for advanced heart failure (www.lvaddecisionaid.com).31–33 We offer concrete examples of how we applied MINDSPACE tools to systematically identify and act upon clinician stakeholder motivations to accept, use, and integrate our DA into standard clinical care. Based on these experiences, we make concrete recommendations for other researchers seeking to generalize these strategies to other implementation projects in different fields and settings.
Methods
Description of Implementation Project and Data Sources
Our current project involves implementing a validated DA for LVAD34 with goals to 1) build capacity with key clinicians (physicians and LVAD nurse coordinators) to implement the DA through an initial “Capacity Building Webinar”35 and reinforcement sessions; 2) collaborate with “physician champions” to support LVAD nurse coordinators in their efforts to implement the DA during patient education and to use the DA themselves; and 3) provide ongoing support to LVAD coordinators to facilitate development of sustainable practices for long-term DA use in their programs. The implementation setting includes nine US hospitals, including five that participated in our original randomized controlled trial (RCT) of the DA and four that had no prior experience with the LVAD DA. None of the nine sites were actively using the DA at the beginning of the dissemination and implementation (D&I) project due to staff turnover since the RCT. We engaged LVAD nurse coordinators as primary staff to disseminate and review the DA with patients. Coordinators generally provide LVAD education and have frequent contact with patient candidates during LVAD evaluation.
Evaluation of D&I progress and success is based on the RE-AIM framework (reach, effectiveness, adoption, implementation, maintenance),36 tracking outcomes using an “Implementation Tracking Sheet” (ITS) that allowed us to calculate “reach” (proportion of eligible patients receiving the DA) and thereby monitor basic changes in DA use after implementing MINDSPACE approaches. The ITS also measured other aspects of RE-AIM, specifically “effectiveness” (i.e., amount of DA viewed: none, some, all) as well as fidelity (“implementation,” in the language of RE-AIM) to the intended use of our DA in the context of SDM, using a 10-item measure. The two remaining RE-AIM variables, acceptance and maintenance, were not outcome targets for the purposes of this article. We employed MINDSPACE strategies throughout our interactions with key staff engaged in implementation, most commonly in monthly phone conversations (site-specific and cross-site, as appropriate) to elicit feedback and collaboratively troubleshoot challenges, and occasionally in on-site visits.
We documented these strategies and interactions in detailed process notes of all interactions with key staff (n = 42) taken by our project coordinator (MT) over the first quarter (0–6 months) of a 2-year project (see Table 2). Using qualitative thematic analysis37 and MAXQDA 2018 software,38 we deductively identified information related to each of the MINDSPACE elements. These nine elements (e.g., Messenger, Incentives) became “codes” to thematically query the process notes, resulting in consolidated examples of how we used each tool to address early implementation challenges, including specific instantiations, considerations, and lessons learned for using these tools in the context of implementing interventions that require clinician buy-in and behavioral change. Coding was done by the first author (KK), a medical anthropologist with extensive expertise in qualitative analysis. All three authors engaged in consensus-reaching discussions about thematic content drawing from independent interpretations of the implementation process notes.
Table 2.
Process Notes Reviewed for MINDSPACE Strategies
| Process Note Type | Total |
|---|---|
| Physician champion meeting minutes | 5 |
| In-person meeting with patient stakeholder | 2 |
| Site visit observations and reflections | 3 |
| Capacity building webinar minutes | 11 |
| LVAD coordinator/manager meeting minutes | 10 |
| Post–capacity building webinar reinforcement session minutes | 10 |
| Working notes of best practices for sustainability | 1 |
| Total | 42 |
LVAD, left ventricular assist device.
The Institutional Review Board at Baylor College of Medicine determined that this project did not constitute human subjects research. Financial support for this project was provided by an award from the Patient Centered Outcomes Research Institute. The funding source had no role in the study and the views expressed in this article are solely the responsibility of the authors.
Results
How We Used MINDSPACE to Motivate Use of a DA Intervention
Messenger
Research tells us that individuals are more likely to act on information if experts and other influential individuals deliver it.39–41 We expected that coordinators would be more motivated to use the DA if they receive encouragement and support from a supervising “physician champion” at each site.
We mobilized physicians before and during implementation to serve as key influencers. Given our experience with clinics participating in our RCT, we expected that physicians would have decision-making authority and direct interaction with coordinators and would continuously advocate for the importance of using the DA in practice.
In addition to enlisting one physician champion at each site, we worked with one key physician “champion of champions” with connections to physician champions across sites. His esteemed reputation and status in the field made him effective at rallying other physicians to monitor and facilitate dissemination at their own sites. He also helped relay messages (e.g., quarterly statistics from RE-AIM evaluations) from our research team to enhance their receptivity to requests for information. This drew on the key aspect of the “messenger” tool by recognizing that busy physicians would be much more receptive to messages from another well-known physicians than they would from nonclinical decision science researchers. Most communication occurred over email, but also fruitful were 30-minute quarterly calls between our “champion of champions” and physician champions at each site to review implementation progress.
Incentives
Research shows that the type, magnitude, and timing42,43 of incentives matter and that individuals are motivated more by avoiding loss (e.g., of resources or power) than by being rewarded with gains.22,44,45 In our case, we recognized that the institution of new approaches to education could potentially be interpreted by coordinators as a disincentivizing loss of independence and self-direction in one’s daily work activities. To counter this perception and to incentivize DA use, we sought to promote ownership and self-direction in how key staff use the DA, encouraging them to make choices in how to use it in practice. We ensured that messages never gave an impression that clinic staff are “required” to use the DA. Some coordinators in managerial positions feared that “forcing” their clinical team to use the DA would be counterproductive, and preferred that they to use the DA voluntarily, recognizing this approach as more satisfying and sustainable. During the initial Capacity Building Webinar and bimonthly check-in calls, we encouraged coordinators to tell us how they thought the DA might be used to enhance patient education and decision making.
The literature also shows that certain types of gains—for example, monetary gains—can disincentivize or “cheapen” desired behaviors that may be linked to more intrinsic motivations such as altruism or self-determination.46,47 We found this to be true among our coordinators, who say that their fundamental motivation to use the DA stems from a desire to help patients make informed decisions. Thus, our second use of “incentives” was to identify and draw attention to coordinators’ own internal motivations for using the DA by asking them to recall specific experiences in which they felt administering the DA had benefitted patients during check in calls. In doing so, coordinators were often made explicitly aware that their use of the DA led to feelings of personal satisfaction that they were genuinely helping patients to inform their decision making.
Norms
A substantial literature demonstrates that people are likely to do what others around are already doing.39,48,49 Given the powerful influence of norms on behavior, we sought to spread desirable norms that facilitate use of our DA. Studies suggest that desirable norms will grow if people are made aware that many others are already engaging in them.50,51 We found that sharing information across sites was crucial for establishing positive norms. We shared site statistics regarding “reach” (dissemination) of our DA in regular meetings with coordinators and physicians and highlighted success stories, including successful methods and procedural flows for integrating the DA with standard education materials. This helped sites situate themselves within cross-site norms and to motivate underperformers (see also “Ego” below). It helped for each site to see and hear exactly how other sites were doing things. We found that our top sites were especially happy to have reach statistics above of the norm and were motivated to maintain this status. Lower performing sites, on the other hand, became more motivated to attain levels closer to the norm when they were able to accurately contextualize their reach numbers in relation others’. Exemplifying sites where coordinators use the DA with confidence helped to establish a positive norm across sites.
Defaults
Research shows that individuals behave in ways that are convenient and are often resistant to change.52,53 Individuals often align with preselected options, or a “status quo” that does not require them to make active choices. For this reason, strategies for behavior change often include “opt-out” instead of “opt-in” approaches.54,55 In our case, we observed attachment to the status quo in that some coordinators were more willing than others to integrate the DA with educational materials (“standard education”). To counter resistance to change, we worked to integrate our DA into existing defaults. We were careful not to convey that coordinators needed to discard existing practices and materials that they found useful. Instead, we helped coordinators to identify gaps in the utility of current defaults particularly which aspects of standard education were the most versus least useful and where our intervention (DA) could potentially replace less useful or missing aspects.
Second, we aimed to change the default itself by instituting an opt-out rather than opt-in approach to administering the DA. Our goal was to make use of the DA an automatic/default process (see also “Norms” above) by standardizing how and when the DA is administered. We encourage coordinators to administer the DA consistently across all eligible patients at a standardized time (i.e., during consent for LVAD evaluation). Coordinators provided feedback that doing so made them less likely to forget to administer the DA, one of the biggest reported challenges to implementation (see also “Salience” below).
Third, we decided to distribute defaults across relevant staff. We encouraged coordinators to opt-out of using sections that were outside the scope of their regular clinical duties and approached the relevant specialists at these sites (e.g., palliative care specialists, social workers, financial advisors) to incorporate those sections (i.e., Values Clarification Exercise) into their routine interactions with patients.
Salience
Research shows that we are more likely to register stimuli that are novel, accessible, and simple.22,56,57 We therefore aimed to make the use of our DA as simple and accessible as possible. First, we aimed to raise as much awareness of the intervention as possible. Our research team contacted coordinators frequently in the earliest stages of implementation to remind them to use the DA with patients. We also encouraged coordinators to put DAs in a visible place with other educational materials and forms to counter against forgetting to use the DA (see “Defaults” above).
Second, we tried to highlight relevant parts of the intervention that serve site-specific needs. We encouraged key staff to identify and use parts of the DA that fill gaps in existing standard education materials and make their specific efforts toward patient education easier and more effective (see also “Defaults” above). For example, several sites reported that their existing education materials lacked pictures. As such, these sites were drawn toward using the Patient Stories section of the DA, which includes diverse photos of LVAD patients in their homes. In some cases, we also modified the DA to make it more relevant for site-specific needs. For example, after a new LVAD device was granted Food and Drug Administration approval, sites wanted to ensure they gave patients the most up-to-date information. In response, we created an informational insert to help coordinators explain the risk profile of this new device within the context of their overall decision making about LVAD treatment.
Priming
Research shows that the environments we construct are constantly priming individuals and that behavior can be altered if we are exposed to certain sights, words, or sensations, even if outside of conscious awareness.58,59 Based on these insights, we used priming by repeatedly and consistently using key words to reinforce a focus on the nature of our intervention, including terms like “shared decision making,”“patient-centeredness,” and “patient partners.” These terms were first explicitly defined in our early Capacity Building Webinars and then reinforced in meetings with key staff, with the intention to prime physicians and coordinators with a focus on patient-centeredness in their efforts.
In priming key staff in this way, we aimed to institute a culture of mutual support for key staff engaging in SDM using our DA. When sites reported low DA reach, we framed conversations positively by first highlighting other achievements and opportunities to try something new. We thus tried to create an undercurrent of support for SDM as a whole, to minimize feelings of failure, and thereby continue to elevate positive associations with using our DA (see “Affect” below).
Affect
Research shows that emotional associations powerfully shape our actions.60,61 Emotional reactions and moods, rather than deliberate decisions, often influence judgments. Using this insight, we sought to invoke positive emotional associations with using our intervention. While staff at some sites were eager to use our DA, others perceived a number of challenges—and therefore potentially negative associations—with using the DA. They emphasized barriers such as lack of time, lack of expertise, and uncertainty about how to integrate with existing materials. To counter these associations, we shared positive experiences across all sites from coordinators—as well as from acceptability testing of our DA during the RCT.33 We emphasized its ability to 1) benefit patients with information developed according to patients’ informational needs (including diverse patient experiential narratives that showed “the good and the bad of LVAD”), 2) to present information in a balanced manner that discouraged clinicians from biasing patients with anecdotal information, and 3) to empower patients to take a lead in decision making, including posing questions to physicians. In this way, coordinators came to associate the DA with patient empowerment and satisfaction, which often also boosted their own self-esteem as educators and care providers. We further added to these positive associations by urging physicians to provide praise and encouragement to clinic staff using the DA (see also “Ego” below).
Commitments
Research shows that we seek to be consistent with our public promises.39 Because commitments become more effective as the costs for failure increase,62 making (especially documented) commitments public can lead people to keep them at the risk of reputational damage or loss of status.63 We therefore utilized the tool of “commitment” by seeking to invite public and documented commitments from key actors for implementation, namely, our physician champions at each site. These involved written pledges of support during development phases of our project, which later became (voluntary, unpaid) formal obligations once funding was received. All of our physician champions made public commitments before one another in group calls, comprising a group of esteemed cardiologists. There was thus a collective, normative aspect to these commitments (see also “Norms” above).
Second, we aimed to institute consistency and reinforcement of commitments through reciprocity. Research demonstrates that individuals strive to reciprocate commitments;64 as such, we set up an informal system of reciprocal expectations. Specifically, we offered encouragement, capacity building,35 and logistical support, and expected in turn to receive consistent feedback and insights from key coordinators in regular calls and meetings, as well as active engagement from physicians whom we reciprocally invited as coauthors in publications and conference presentations. We aimed to be consistent about what types of information we sought, including how and when to send it (e.g., monthly reach statistics and return of Implementation Tracking Sheets). We continued to offer further opportunities for capacity building, including retraining whenever requested, as well as site visits to support and help troubleshoot emergent challenges. This reciprocal arrangement, we believe, increased their inclination to maintain their stated commitments.
Ego
A vast literature shows that we act in ways that make us feel better about ourselves and engage in behavior that we think will give us a positive image in the eyes of important others, as well as build personal sense of self-efficacy and self-esteem.65,66 One aspect of this “ego-building” strategy was to create a subtle (and, we hope, innocuous) sense of competition between sites (see also “Norms” above). We did so by conveying site-specific reach statistics during quarterly calls with individual sites, letting each site know their “rank” in comparison to other sites, which remained anonymous. This had the effect of motivating top-performers to take active steps to maintain their identity as top performers and motivating lower performers to “get up to speed” with what they perceived as normative reach levels. This ego-drive to “beat” other sites’ reach numbers served to bring the DA into more patients’ hands.
Research also suggests we prefer to view ourselves as self-consistent,67 and are likely to change our behaviors to match what we say or believe or to change our beliefs to fit our behaviors.68 In line with this tendency, we implemented a “foot in the door” approach to behavior change by setting small implementation goals (e.g., “use the DA with at least one patient before end of month”), which might then be followed by larger, similar efforts to maintain consistency with that achieved goal. We hoped that bringing public attention to a staff member’s new “image” as a person who now actively utilizes the DA might further influence him/her to continue behaviors consistent with that image. In addition, when a site’s overall reach decreased, we reminded them that they had previously performed at a higher level. We encouraged them to pinpoint factors underlying the decrease and strategize ways help them increase their reach and strategize solutions to be consistent with their previous level of success. This conveyed an expectation that implementers continue in their efforts to use the intervention, further influencing behavior in line with findings that the greater the expectation placed on people, the better they perform.69,70
Preliminary Associations With RE-AIM Outcomes
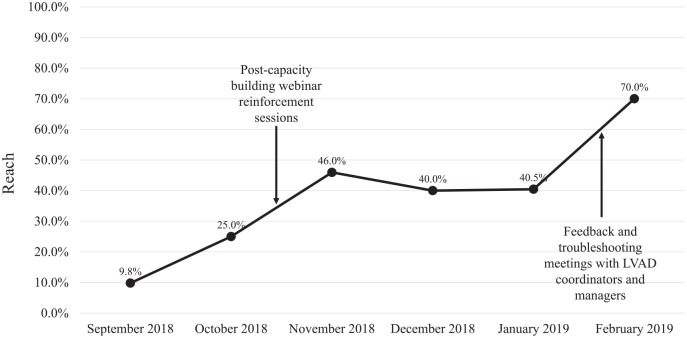
During the first 6 months of implementation, 171 DAs were distributed among 433 LVAD candidates across nine D&I sites (range among individual sites: 6–53 DAs). The average reach for all sites over 6 months was 39.5% with a range of 10.9% to 94.1% among individual sites. Overall reach increased from 9.8% in the first month of implementation to 70.0% in the last month of quarter 1 (Figure 1). Larger increases in reach were observed during the time period of the post-webinar reinforcement sessions and first structured coordinator follow-up calls in which strategically employed site-specific configurations of the MINDSPACE tools were used to troubleshoot and maintain clinicians’ motivation to use the DA. We did not observe any upward trends in our other two relevant RE-AIM variables, namely, effectiveness (amount viewed) and implementation (fidelity).
Figure 1.
Left ventricular assist device (LVAD) decision aid monthly reach across nine clinical sites during the first 6 months of implementation (September 2018 to February 2019).
Discussion
At the recent 10th Annual International Shared Decision Making conference in July 2019, a number of implementation scientists voiced an eagerness for concrete, evidence-based tools to influence behaviors targeted by their interventions. They lamented that effective decision support tools rarely make their way into real-world clinical use. Their enduring search for new implementation techniques suggests either a lack of widespread awareness of existing implementation frameworks or persistent gaps in their perceived utility. We believe that the MINDSPACE toolkit helps fill this gap by offering nine evidence-based tools from behavioral economics to enact change in behavior in ways demonstrated to be effective, low-cost, and sustainable. In an effort to facilitate generalizability, we offer recommendations (Table 3) for implementation scientists seeking to apply these tools in their own implementation projects.
Table 3.
Recommendations for Applications of MINDSPACE in Implementation Science
| Tool | Recommendations |
|---|---|
| Messenger39–41 | • Enlist individuals with not only status and influence over key actors involved in implementation but also with regular contact and direct oversight over their activities. • Select messengers with the time and willingness to directly and consistently liaison between your implementation team and key actors. |
| Incentives22,42–45 | • Make room for key actors to enact self-determination74 in performing implementation procedures. In practice, this may involve strategic trade-offs with certain aspects of fidelity to encourage ownership and internalization of intervention objectives. • Conduct formative research or early discussions with key actors to identify feasible incentives. |
| Norms38,48,49 | • Identify when information about implementation metrics should be shared anonymously or using identifiers. While not appropriate in every case, identifiers may strategically reward top performers as well as motivate underperformers to meet normative goals. • Anonymous feedback on implementation progress can help calibrate key actors’ self-expectations in relation to others’ performance. Highlight key “exemplary” actors (with their permission) to establish positive norms. |
| Defaults52,53 | • Identify how key actors are emotionally or practically invested in default (existing) approaches. Focus communication with these actors on integration (rather than replacement) of existing practices or materials with the new intervention. • Where actors are not attached to existing defaults, efforts should focus more on “routinization” of the new intervention (e.g., timing of delivery) so that actors need not make conscious choices to engage or “opt in” to new procedures. |
| Salience22,56.57 | • From early implementation onward, ensure that intervention materials (e.g., a decision aid, or step-by-step guidelines for new clinical procedures) are highly visible and easily consulted by key actors. Even small search efforts can act as deal-breaking disincentives. • Identify (systematically or informally) which aspects of an intervention (e.g., sections of a decision aid) matter most to key actors. Their utility should be highlighted regularly in communications between key actors and messengers and/or implementers. Accept partial implementation as a potential step toward full fidelity. |
| Priming58,59 | • Identify important terms or images that remind actors of key aims or principles of an intervention, and communicate them regularly and consistently. • Terms or images may be associated heuristically with earlier elaborations during initial training orientations, so that brief references to them (e.g., patient-centeredness) evoke a larger corpus of learned relevant associations (e.g., shared decision making practices). |
| Affect60,61 | • Associate positive emotions like joy, contentment, gratitude, pride, or empowerment with enacting key elements of an intervention to internally motivate key actors to engage in implementation. • Identify (through formative research or early discussions with key actors) which emotions are motivational in their target activities as a first step to associating affect with intervention features (e.g., feeling “empowered” as a patient educator when using a decision aid that conveys patient-preferred information). • Create opportunities for actors to share their experiences so others might be similarly motivated. |
| Commitments39 | • Create forums in which key actors express commitments to participate in implementation in front of peers and/or other influential partners in implementation. • Identify (early) key actors’ expectations for reciprocity for their commitments. While some actors participate expecting nothing in return, others’ participation may be contingent on reciprocal commitments from the implementation team (e.g., for training, certification, credit or recognition, etc.). • Reinforce commitments regularly in both private meetings and peer-to-peer forums. |
| Ego65,66 | • To motivate pro-implementation behaviors, it may be useful to create a (limited) sense of ego-driven competition among key actors. Where appropriate, publicly share actor- or site-level performance in order to institute meritocracy and accountability (see “Norms”). • Identify early (even small) accomplishments to foster a self-image of capability and positive performance among key actors and/or sites. |
In applying MINDSPACE to motivate pro-implementation behaviors among key participating clinic staff, we respond to calls by Elwyn and collegues9 to address two understudied stages that precede “acceptance” in the “Five Stages of Achieved Implementation” model,71,72 now widely used in implementation research. These two preliminary stages include “orientation” (awareness and interest in innovation) and “insight” (understanding impacts of an implementation for existing routines). Despite their importance for framing and motivating behavior, little is known about how to shape orientation and insight in ways that lead to positive and sustainable behavioral change. Through our use of MINDSPACE’s evidence-based strategies, we have taken active steps to 1) enhance awareness and interest (“orientation”) among key actors involved in implementation activities and 2) situate our DA as a new default centerpiece in patient education while monitoring its impacts on existing routines (“insight”) through constant feedback from coordinators and physicians actively using the DA in practice. We believe that these two elements correspond to the two “peaks” in our “reach” timeline (Figure 1) whereby an initial “Capacity Building Webinar” and reinforcement sessions helped generate awareness and interest, while Feedback and Troubleshooting sessions were used to collaboratively gain insight into the impacts of our newly implemented DA on clinic routines, coordinator and physician roles, and patient experiences.
Using MINDSPACE in a Context of Limited Resources for Implementation
An additional advantage of the MINDSPACE toolkit is that it narrows the operational scope for implementation scientists. While we do believe there is a requisite place in implementation science for addressing larger structural factors,8 in practice it is not always feasible to address or affect change in structural or organizational dimensions of behavior. Because more resources are spent on the development of interventions than on their implementation or scale-up,3 implementers are left to generate changes in environments over which they have little control and with actors over who they have little to no influence. For this reason, we believe that the MINDSPACE approach outlined in this article provides a more proximate and achievable toolkit by which to influence uptake of a DA or other intervention, by generating minor alterations to the choices and environment in which people act, thereby working directly with factors over which implementers can hope to have immediate influence at little cost.
Limitations
While exerting influence on the automatic versus reflective thought systems is said to generate longer lasting behavioral changes,30 some MINDSPACE effects are rapid and even subconscious, generating uncertainty over how lasting the effects are. Dolan et al.26 argue that while surface-level effects may seem fleeting, such behaviors and decisions may translate into longer lasting changes. These effects may better be thought of as self-sustaining “triggers.” While we agree with this in principle, we also suspect that some triggers may need reinforcement, and (in our experience) encouragement from implementers to build in reinforcements that sustain initial nudging effects. We believe this is illustrated by the effects shown in Figure 1. Notably, we did not see similar upward trends in other RE-AIM variables including implementation (fidelity) and effectiveness (amount of DA viewed). This suggest that 1) we may have focused our MINDSPACE messaging narrowly on increasing reach rather than on enhancing the breadth and/or fidelity of using the DA; or 2) the MINDSPACE tools may be better equipped to enact broad changes in use rather than in the subtleties of how the DA is used. More research is needed to explore this issue, including quantitative explorations of the independent and/or combined impacts of the MINDSPACE strategies on RE-AIM measures.
Second, Michie et al.15 argue that MINDSPACE does not appear to encompass all the important intervention types. We believe that the enduring focus of those who wish to use MINDSPACE should be on its utility, not necessarily on how exhaustive the range of its influences is. The tools represent major categories of influence in behavioral economics but do not encompass all possible modes of influence over human behavior.
A third concern is generalizability across contexts and across populations. Individuals’ responses to nudges are likely to differ across institutional, social, economic, and cultural contexts.73 We found that formative research with key informants from the target population (LVAD patients, physicians, and clinical staff) significantly helped us identify relevant motivations and tailor the MINDSPACE strategies accordingly.
Conclusion
MINDSPACE tools show great promise for bringing innovative research from behavioral economics into the realm of implementation science with the aim of effecting positive behavioral change. In this article, we have provided recommendations for how these tools can be adapted to an implementation context to help close the “implementation gap” by encouraging uptake of an evidence-based patient DA in real-world contexts. MINDSPACE helps address the enduring challenges of implementation by offering concrete solutions to influence individual motivations for engaging in positive behaviors targeted during implementation. Our preliminary results illustrate the promise of this approach, though further research is needed to better understand the impacts of distinct nudging approaches in the MINDSPACE toolkit in other implementation contexts.
Supplemental Material
Supplemental material, 7._Appendix_1_online_supp for Using Nudges to Enhance Clinicians’ Implementation of Shared Decision Making With Patient Decision Aids by Kristin M. Kostick, Meredith Trejo, Robert J. Volk, Jerry D. Estep and J.S. Blumenthal-Barby in MDM Policy & Practice
Acknowledgments
The authors would like to thank the following physicians and LVAD coordinators that championed use of the decision aid at their hospitals: Arvind Bhimaraj, Barry Trachtenberg, Douglas Horstmanshof, Andrew Civitello, Vinay Thohan, Mandeep Mehra, Matthias Loebe, Ulrich Jorde, Nir Uriel, Ida Solomon, Maggie Mendenhall, Margaret Whitehead, Kathy Princer, Maryclare Hickey, Cecilia Wu, Kristina Belkova, Tiffany Buda, Carolyne Castillo, Maria Taveras, Daphenie Fauvel, and Annalyse Chinco. The authors would also like to thank Sarah Smati for her help with data analysis, and Mary Yorgensen and Brenda Mays for their patient perspectives on decision aid development and implementation.
Footnotes
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Jerry D. Estep serves as a medical advisor at Medtronic and a consultant and speaker for Abbott. Neither company was involved in the design or conduct of the project. None of the other authors declare any potential conflicts of interest.
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Financial support for this study was provided entirely by an award from the Patient Centered Outcomes Research Institute (DI-2017C2-7726). The views in this publication are solely the responsibility of the authors and do not necessarily represent the views of the Patient-Centered Outcomes Research Institute, its Board of Governors or Methodology Committee.
Authors’ Note: This work was conducted at: Center for Medical Ethics and Health Policy, Baylor College of Medicine; Department of Cardiovascular Medicine, Cleveland Clinic; DeBakey Heart & Vascular Center, Houston Methodist Hospital; Texas Heart Institute, Baylor St. Luke’s Medical Center; Heart & Vascular Center, Brigham and Women’s Hospital; Center for Heart and Vascular Care, Montefiore Medical Center; Miami Transplant Institute, Jackson Health System; Advanced Cardiac Care Program, INTEGRIS Baptist Medical Center; Center for Advanced Heart Failure Therapies, Aurora St. Luke’s Medical Center; Heart and Vascular Center, University of Chicago Medicine.
Preliminary data for this project were presented at the 2018 and 2019 PCORI Annual Meeting and the 2019 International Shared Decision Making Conference.
ORCID iDs: Kristin M Kostick  https://orcid.org/0000-0003-2510-0174
https://orcid.org/0000-0003-2510-0174
Meredith Trejo  https://orcid.org/0000-0003-2719-6050
https://orcid.org/0000-0003-2719-6050
Robert J Volk  https://orcid.org/0000-0001-8811-5854
https://orcid.org/0000-0001-8811-5854
Supplemental Material: Supplementary material for this article is available on the Medical Decision Making Policy & Practice website at https://journals.sagepub.com/home/mpp.
Contributor Information
Kristin M. Kostick, Center for Medical Ethics and Health Policy, Baylor College of Medicine, Houston, Texas.
Meredith Trejo, Center for Medical Ethics and Health Policy, Baylor College of Medicine, Houston, Texas.
Robert J. Volk, Department of Health Services Research, University of Texas MD Anderson Cancer Center, Houston, Texas
Jerry D. Estep, Department of Cardiovascular Medicine, Cleveland Clinic, Cleveland, Ohio
J.S. Blumenthal-Barby, Center for Medical Ethics and Health Policy, Baylor College of Medicine, Houston, Texas
References
- 1. Barry MJ, Edgman-Levitan P, Sepucha K. Shared decision-making: staying focused on the ultimate goal [cited February 20, 2018]. NEJM Catalyst. Available from: https://catalyst.nejm.org/shared-decision-making-patient-decision-aids/
- 2. Barry MJ, Edgman-Levitan S. Shared decision making—the pinnacle of patient-centered care. N Engl J Med. 2012;366(9):780–1. [DOI] [PubMed] [Google Scholar]
- 3. Stacey D, Légaré F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2017;(4):CD001431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Stacey D, Légaré F, Lewis KB. Patient decision aids to engage adults in treatment or screening decisions. JAMA. 2017;318(7):657–8. [DOI] [PubMed] [Google Scholar]
- 5. Boss EF, Mehta N, Nagarajan N, et al. Shared decision making and choice for elective surgical care: a systematic review. Otolaryngol Neck Surg. 2016;154(3):405–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gayer CC, Crowley MJ, Lawrence WF, et al. An overview and discussion of the Patient-Centered Outcomes Research Institute’s decision aid portfolio. J Comp Eff Res. 2016;5(4):407–15. [DOI] [PubMed] [Google Scholar]
- 7. Gravel K, Légaré F, Graham ID. Barriers and facilitators to implementing shared decision-making in clinical practice: a systematic review of health professionals’ perceptions. Implement Sci. 2006;1(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Scholl I, LaRussa A, Hahlweg P, Kobrin S, Elwyn G. Organizational-and system-level characteristics that influence implementation of shared decision-making and strategies to address them—a scoping review. Implement Sci. 2018;13(1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Elwyn G, Scholl I, Tietbohl C, et al. “Many miles to go . . . ”: a systematic review of the implementation of patient decision support interventions into routine clinical practice. BMC Med Inform Decis Mak. 2013;13(Suppl. 2):S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lin GA, Halley M, Rendle KA, et al. An effort to spread decision aids in five California primary care practices yielded low distribution, highlighting hurdles. Health Aff (Millwood). 2013;32(2):311–20. [DOI] [PubMed] [Google Scholar]
- 11. Holmes-Rovner M, Valade D, Orlowski C, Draus C, Nabozny-Valerio B, Keiser S. Implementing shared decision-making in routine practice: barriers and opportunities. Health Expect. 2000;3(3):182–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82(4):581–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Elwyn G, Légaré F, van der Weijden T, Edwards A, May C. Arduous implementation: does the normalisation process model explain why it’s so difficult to embed decision support technologies for patients in routine clinical practice. Implement Sci. 2008;3(1):57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Uy V, May SG, Tietbohl C, Frosch DL. Barriers and facilitators to routine distribution of patient decision support interventions: a preliminary study in community-based primary care settings. Health Expect. 2014;17(3):353–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Michie S, Van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6(1):42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. 2012;7(1):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. [Google Scholar]
- 18. Tan AS, Mazor KM, McDonald D, et al. Designing shared decision-making interventions for dissemination and sustainment: can implementation science help translate shared decision making Into routine practice? MDM Policy Pract. 2018;3(2):2381468318808503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chaiken S, Trope Y. Dual-Process Theories in Social Psychology. New York: Guilford Press; 1999. [Google Scholar]
- 20. Evans JSB. Heuristic and analytic processes in reasoning. Br J Psychol. 1984;75(4):451–68. [Google Scholar]
- 21. Evans JS. Dual-processing accounts of reasoning, judgment, and social cognition. Annu Rev Psychol. 2008;59:255–78. [DOI] [PubMed] [Google Scholar]
- 22. Kahneman D. Thinking, Fast and Slow. New York: Farrar, Straus & Giroux; 2011. [Google Scholar]
- 23. Simon HA. Administrative Behavior: A Study of Decision-Making Processes in Administrative Organization. 4th ed. New York: Free Press; 1997. [Google Scholar]
- 24. Thaler RH, Sunstein CR. Nudge: Improving Decisions About Health, Wealth, and Happiness. New Haven: Yale University Press; 2008. [Google Scholar]
- 25. Allcott H, Rogers T. The short-run and long-run effects of behavioral interventions: Experimental evidence from energy conservation. Am Econ Rev. 2014;104(10):3003–37. [Google Scholar]
- 26. Dolan P, Hallsworth M, Halpern D, King D, Vlaev I. MINDSPACE: Influencing Behaviour for Public Policy. London: Institute of Government; 2010. [Google Scholar]
- 27. Halpern D, Sanders M. Nudging by government: progress, impact, and lessons learned. Behav Sci Policy. 2016;2(2):52–65. [Google Scholar]
- 28. Sheeran P. Intention-behaviour relations: a conceptual and empirical review. Eur Rev Soc Psychol. 2002;12(1):1–36. [Google Scholar]
- 29. Feibelmann S, Yang TS, Uzogara EE, Sepucha K. What does it take to have sustained use of decision aids? A programme evaluation for the breast cancer initiative. Health Expect. 2011;14(Suppl. 1):85–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hofmann W, Friese M, Wiers RW. Impulsive versus reflective influences on health behavior: a theoretical framework and empirical review. Health Psychol Rev. 2008;2(2):111–37. [Google Scholar]
- 31. Blumenthal-Barby JS, Kostick KM, Delgado ED, et al. Assessment of patients’ and caregivers’ informational and decisional needs for left ventricular assist device placement: implications for informed consent and shared decision-making. J Heart Lung Transplant. 2015;34(9):1182–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kostick K, Delgado ED, Wilhelms LA, et al. Development and pilot-testing of a patient decision aid for left ventricular assist device placement. VAD J. 2016;2(1):1. [Google Scholar]
- 33. Kostick KM, Minard CG, Wilhelms LA, et al. Development and validation of a patient-centered knowledge scale for left ventricular assist device placement. J Heart Lung Transplant. 2016;35(6):768–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kostick KM, Bruce CR, Minard CG, et al. A multisite randomized controlled trial of a patient-centered ventricular assist device decision aid (VADDA trial). J Card Fail. 2018;24(10):661–71. [DOI] [PubMed] [Google Scholar]
- 35. Elwyn G, Durand MA, Song J, et al. A three-talk model for shared decision making: multistage consultation process. BMJ. 2017;359:j4891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89(9):1322–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Schilling J. On the pragmatics of qualitative assessment. Eur J Psychol Assess. 2006;22(1):28–37. [Google Scholar]
- 38. VERBI Software. MAXQDA Software for Qualitative Data Analysis. Berlin: VERBI Software; 1989. [Google Scholar]
- 39. Cialdini RB. Influence: The Psychology of Persuasion. New York: William Morrow; 1993. [Google Scholar]
- 40. Freed GL, Clark SJ, Butchart AT, Singer DC, Davis MM. Sources and perceived credibility of vaccine-safety information for parents. Pediatrics. 2011;127(Suppl. 1):S107–S112. [DOI] [PubMed] [Google Scholar]
- 41. Waller J, Macedo A, Von Wagner C, et al. Communication about colorectal cancer screening in Britain: public preferences for an expert recommendation. Br J Cancer. 2012;107(12):1938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kahneman D, Tversky A. Choices, values, and frames. Am Psychol. 1984;39(4):341–50. [Google Scholar]
- 43. Lussier JP, Heil SH, Mongeon JA, Badger GJ, Higgins ST. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction. 2006;101(2):192–203. [DOI] [PubMed] [Google Scholar]
- 44. Mantzari E, Vogt F, Shemilt I, Wei Y, Higgins JP, Marteau TM. Personal financial incentives for changing habitual health-related behaviors: a systematic review and meta-analysis. Prev Med. 2015;75:75–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Patel MS, Asch DA, Rosin R, et al. Framing financial incentives to increase physical activity among overweight and obese adults: a randomized, controlled trial. Ann Intern Med. 2016;164(6):385–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Deci EL, Koestner R, Ryan RM. A meta-analytic review of experiments examining the effects of extrinsic rewards on intrinsic motivation. Psychol Bull. 1999;125(6):627–68. [DOI] [PubMed] [Google Scholar]
- 47. Kuvaas B, Buch R, Weibel A, Dysvik A, Nerstad CG. Do intrinsic and extrinsic motivation relate differently to employee outcomes? J Econ Psychol. 2017;61(C):244–58. [Google Scholar]
- 48. Cialdini RB. Crafting normative messages to protect the environment. Curr Dir Psychol Sci. 2003;12(4):105–9. [Google Scholar]
- 49. Perkins HW, Berkowitz AD. Perceiving the community norms of alcohol use among students: some research implications for campus alcohol education programming. Int J Addict. 1986;21(9–10):961–76. [DOI] [PubMed] [Google Scholar]
- 50. Burger JM, Shelton M. Changing everyday health behaviors through descriptive norm manipulations. Soc Influence. 2011;6(2):69–77. [Google Scholar]
- 51. Perkins HW, Craig DW. A successful social norms campaign to reduce alcohol misuse among college student-athletes. J Stud Alcohol. 2006;67(6):880–9. [DOI] [PubMed] [Google Scholar]
- 52. Halpern SD, Ubel PA, Asch DA. Harnessing the power of default options to improve health care. N Engl J Med. 2007;357:1340–4. [DOI] [PubMed] [Google Scholar]
- 53. Samuelson W, Zeckhauser R. Status quo bias in decision making. J Risk Uncertainty. 1988;1(1):7–59. [Google Scholar]
- 54. Johnson EJ, Goldstein D. Medicine. Do defaults save lives? Science. 2003;302(5649):1338–9. [DOI] [PubMed] [Google Scholar]
- 55. Moseley A, Stoker G. Putting public policy defaults to the test: the case of organ donor registration. Int Public Manag J. 2015;18(2):246–64. [Google Scholar]
- 56. Broers VJ, De Breucker C, Van den Broucke S, Luminet O. A systematic review and meta-analysis of the effectiveness of nudging to increase fruit and vegetable choice. Eur J Public Health. 2017;27(5):912–20. [DOI] [PubMed] [Google Scholar]
- 57. Kahneman D, Thaler RH. Anomalies: utility maximization and experienced utility. J Econ Perspect. 2006;20(1):221–34. [Google Scholar]
- 58. Bargh JA, Chen M, Burrows L. Automaticity of social behavior: direct effects of trait construct and stereotype activation on action. J Pers Soc Psychol. 1996;71(2):230–44. [DOI] [PubMed] [Google Scholar]
- 59. Bargh JA, Schwader KL, Hailey SE, Dyer RL, Boothby EJ. Automaticity in social-cognitive processes. Trends Cogn Sci. 2012;16(12):593–605. [DOI] [PubMed] [Google Scholar]
- 60. Loewenstein GF, Weber EU, Hsee CK, Welch N. Risk as feelings. Psychol Bull. 2001;127(2):267–86. [DOI] [PubMed] [Google Scholar]
- 61. Slovic P, Finucane ML, Peters E, MacGregor DG. The affect heuristic. Eur J Oper Res. 2007;177(3):1333–52. [Google Scholar]
- 62. Giné X, Karlan D, Zinman J. Put your money where your butt is: a commitment contract for smoking cessation. Am Econ J Appl Econ. 2010;2(4):213–35. [Google Scholar]
- 63. Cialdini RB, Goldstein NJ. Social influence: compliance and conformity. Annu Rev Psychol. 2004;55:591–621. [DOI] [PubMed] [Google Scholar]
- 64. Nowak M, Highfield R. SuperCooperators: Altruism, Evolution, and Why We Need Each Other to Succeed. New York: Free Press; 2011. [Google Scholar]
- 65. Landry CE, Lange A, List JA, Price MK, Rupp NG. Toward an understanding of the economics of charity: evidence from a field experiment. Q J Econ. 2006;121(2):747–82. [Google Scholar]
- 66. Tajfel H, Turner JC, Austin WG, Worchel S. An integrative theory of intergroup conflict. In: Austin WG, Worchel S, eds. The Social Psychology of Intergroup Relations. Monterey: Brooks/Cole; 1979:56–65. [Google Scholar]
- 67. Locke KD, Church AT, Mastor KA, et al. Cross-situational self-consistency in nine cultures: the importance of separating influences of social norms and distinctive dispositions. Pers Soc Psychol Bull. 2017;43(7):1033–49. [DOI] [PubMed] [Google Scholar]
- 68. Copper J, Carlsmith KM. Cognitive dissonance. In: Wright JD, ed. International Encyclopedia of the Social & Behavioral Sciences. 2nd ed. Oxford: Elsevier; 2015:76–78. [Google Scholar]
- 69. Rosenthal R. Pygmalion effects: existence, magnitude, and social importance. Educ Res. 1987;16(9):37–40. [Google Scholar]
- 70. Rosenthal R. On the Social Psychology of Self-Fulfilling Prophecy: Further Evidence for Pygmalion Effects and Their Mediating Mechanisms [Module 52]. New York: MSS Modular. [Google Scholar]
- 71. Grol RP, Bosch MC, Hulscher ME, Eccles MP, Wensing M. Planning and studying improvement in patient care: the use of theoretical perspectives. Milbank Q. 2007;85(1):93–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Grol R, Wensing M. What drives change? Barriers to and incentives for achieving evidence-based practice. Med J Aust. 2004;180(S6):S57–S60. [DOI] [PubMed] [Google Scholar]
- 73. Bovens L. Nudges and cultural variance: a note on Selinger and Whyte. Knowledge Technol Policy. 2010;23(3–4):483–6. [Google Scholar]
- 74. Ryan RM, Deci EL. Self-Determination Theory: Basic Psychological Needs in Motivation, Development, and Wellness. New York: Guilford Press; 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, 7._Appendix_1_online_supp for Using Nudges to Enhance Clinicians’ Implementation of Shared Decision Making With Patient Decision Aids by Kristin M. Kostick, Meredith Trejo, Robert J. Volk, Jerry D. Estep and J.S. Blumenthal-Barby in MDM Policy & Practice