Dear Editor
We were interested to read about environmental contamination by SARS-CoV-2 by Ye et al.1 However, this study only investigated surface contamination and did not explore airborne contamination, which may also have led to surface contamination via settling.
Currently, in the context of COVID-19, nebuliser use is not considered as aerosol-generating procedure (AGP) by the World Health Organization (WHO)2 or UK Public Health England (PHE),3 though the US Centers for Disease Control and Prevention (CDC) does list nebulisation as an AGP.4 Yet, when such masks are used, there are clearly visible ‘smoke’ plumes emanating from the mask side-vents during patient exhalations, which may act as a source of aerosols.5
We therefore tested this possibility, experimentally, using a licensed live-attenuated influenza vaccine (LAIV, Fluenz Tetra, AstraZeneca, Espoo, Finland) as a surrogate virus tracer.
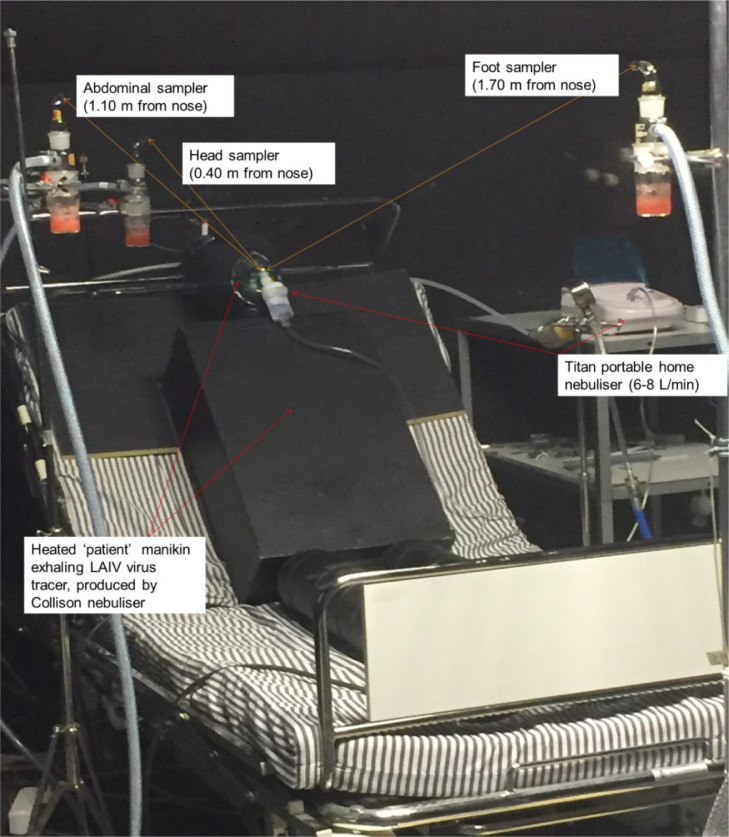
We simulated a human patient using a heated manikin on a hospital bed in a full-scale mock isolation room with mixed ventilation at 12 air changes per hour (Fig. 1 ), wearing a home nebuliser mask (Titan Portable Home Nebuliser, 0.2 ml/min fluid, 6–8 L/min) nebulising distilled water.
Fig. 1.
Experimental layout of the heated ‘patient’ manikin, reclining on a bed. The positions of the three SKC biosamplers mimic healthcare worker positions during a typical ward round. LAIV – live-attenuated influenza virus.
The manikin was modified to continuously exhale at 10 L/min air, to simulate tidal breathing at a respiratory rate of ∼14 breaths/min with a tidal volume of ∼700 ml air. This exhalation flow was generated using a Collison nebuliser,6 containing aerosols of the LAIV at a flow rate of 10 L/min.
Simultaneous air-sampling for 10 min, using three SKC biosamplers (SKC Ltd., Dorset, UK) running at 12 L/min, collected air samples into virus 20 ml transport medium (VTM) from three different locations around the bed. These positions were selected to simulate typical healthcare worker positions around a patient's bed during a clinical ward round, i.e. at distances of: 0.40 m (near the head), 1.10 m (near the abdomen) and 1.70 m (near the feet), from the manikin's nose and mouth (Fig. 1).
After sampling for 10 min (the duration of a typical nebuliser session) at 12 L/min (totalling 120 L air collected), the mean airborne viral load captured within the liquid VTM samples was detected and quantified using an influenza-specific digital polymerase chain reaction (PCR) assay (further details available upon request).
The experiment was run a total of 5 times over two days to give average viral loads at each of the SKC sampling locations: 7.34 ± 0.28 × 104 copies/ml VTM (head), 2.09 ± 0.41 × 104 copies/ml VTM (abdomen), and 1.41 ± 0.23 × 104 copies/ml VTM (feet). Converting these averaged viral loads in copies/ml VTM to copies/L air (given that each air sample was obtained from a total air volume collection of 120 L), this gives approximately: 612 viruses/L (head), 174 viruses/L (abdomen), 118 viruses/L (feet).
These results show that aerosols from a nebulizer mask can spread throughout the room at a decreasing concentration with increasing distance from the source. This experiment was performed within a ventilated experimental chamber with 12 ACH, which is typical of hospital, single-bedded isolation rooms.7 However, in less well ventilated rooms, the airborne virus concentration may gradually increase over time,8 potentially posing a hazard to healthcare workers entering the room to attend to the patient.
The use of nebulisers (and the very similar simple oxygen masks) is routine and widespread for patients presenting with respiratory problems on many general medical wards. The incoming oxygen airflow from these respiratory assist devices will periodically collide with the patient's outgoing virus-laden exhaled breath, causing plumes of mixed clean and contaminated air to be vented from the sides of these masks.
These findings indicate these respiratory assist devices, as per the US CDC guidelines,4 should be considered as potential AGPs, as they can generate aerosols of airborne virus that can travel at least the length of a patient bed - further than those likely generated by normal breathing,9 to potentially expose and infect others.
This is especially important during the current COVID-19 pandemic where large numbers of healthcare workers may be exposed to patients using these respiratory assist devices, and potentially become infected from aerosolised SARS-CoV-2.5
Acknowledgements
This study was funded by a grant from the Institution of Occupational Safety and Health (IOSH, R15152), awarded to Tang JW and Koskela H.
References
- 1.Ye G., Lin H., Chen L. Environmental contamination of SARS-COV-2 in healthcare premises. J Infect. 2020 doi: 10.1016/j.jinf.2020.04.034. Apr 30pii: S0163-4453(20)30260-7[Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health organisation (WHO). Infection prevention and control during health care when novel coronavirus (nCoV) infection is suspected. Updated 19 March2020. https://www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125(Accessed 6 May 2020)
- 3.Public Health England (PHE). COVID-19: infection prevention and control guidance. Updated 27 April2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/881489/COVID-19_Infection_prevention_and_control_guidance_complete.pdf(Accessed 6 May 2020).
- 4.US Centers for Disease Control and prevention (CDC). Interim US. guidance for risk assessment and public health management of healthcare personnel with potential exposure in a healthcare setting to patients with coronavirus disease 2019 (COVID-19). 15 April2020.
- 5.Ferioli M., Cisternino C., Leo V., Pisani L., Palange P., Nava S. Protecting healthcare workers from SARS-CoV-2 infection: practical indications. Eur Respir Rev. 2020;29(155) doi: 10.1183/16000617.0068-2020. pii: 200068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brown J.R., Tang J.W., Pankhurst L. Influenza virus survival in aerosols and estimates of viable virus loss resulting from aerosolization and air-sampling. J Hosp Infect. 2015;91(3):278–281. doi: 10.1016/j.jhin.2015.08.004. [DOI] [PubMed] [Google Scholar]
- 7.Airborne infection isolation room (AIIR). Centers for Disease Control and Prevention website. Updated 5 Nov, 2015. https://www.cdc.gov/infectioncontrol/guidelines/isolation/glossary.html(Accessed 6 May 2020).
- 8.Qian H., Zheng X. Ventilation control for airborne transmission of human exhaled bio-aerosols in buildings. J Thorac Dis. 2018;10(Suppl 19):S2295–S2304. doi: 10.21037/jtd.2018.01.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tang J.W., Nicolle A.D., Klettner C.A. Airflow dynamics of human jets: sneezing and breathing - potential sources of infectious aerosols. PLoS ONE. 2013;8(4):e59970. doi: 10.1371/journal.pone.0059970. [DOI] [PMC free article] [PubMed] [Google Scholar]