Dear Editor,
We present our experience of managing two cases of SARS-CoV-2 infection in very preterm pregnancy.
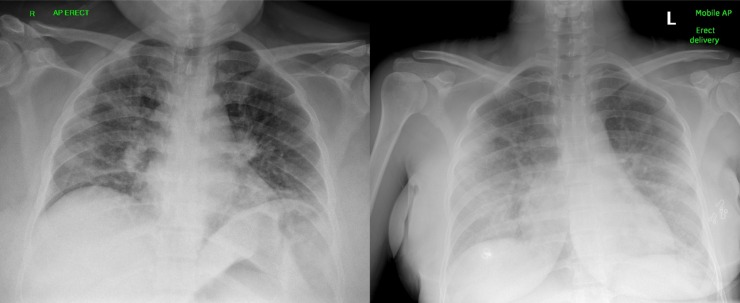
A 39 year-old primigravida presented with 5 days of dyspnoea, cough and pyrexia at 28 + 4 weeks of gestation. She was Afro-Caribbean, had BMI 42 and type 2 diabetes mellitus. Her respiratory rate was 20 breaths/minute, oxygen saturations (SpO2) 92 % and arterial partial pressure of oxygen (PaO2) was 8.1 mmHg in air. Chest X-ray showed bilateral infiltrates (Fig. 1 ). SARS-CoV-2 infection causing type 1 respiratory failure was presumed. She received corticosteroids for fetal maturation. After 24 h she deteriorated and was admitted to ICU for high-flow nasal oxygen and then non-invasive ventilation 3 h later. A multi-disciplinary (obstetric, anaesthetic and intensivist) decision was made for delivery by caesarean section, to facilitate invasive ventilation of the woman. This followed magnesium sulphate for fetal neuroprotection. Maternal airway pressures and oxygen requirements were high throughout surgery. After surgery she was positioned flat for central venous cannulation and deteriorated acutely post-procedure, with high airway pressures and SpO2 of 35 % despite fractional inspired oxygen (FiO2) of 1.0. Needle chest decompression was performed to exclude iatrogenic tension pneumothorax, although no gas escape was heard, and subsequent ultrasound excluded pneumothorax. Endotracheal tube position was confirmed, air entry was bilateral. Bedside echocardiogram did not suggest right heart strain due to embolism. The acute post-partum hypoxaemia was managed by positioning the patient prone in theatre prior to transfer to ICU, with immediate improvement. Chest X-ray after proning showed endobronchial tube migration causing left upper lobe collapse, which was corrected. She improved rapidly and was de-proned later that day, extubated on day three and discharged on day six. SARS-CoV-2 RNA swab from the patient was positive, and from the baby was negative. Her baby’s Apgar scores were 6 at 1 min and 8 at 5 min. The baby weighed 1.53 kg. The baby was intubated shortly after birth, diagnosed with a spontaneous bowel perforation on day 6 and transferred to a tertiary unit. Following a bowel resection the baby is recovering well.
Fig. 1.
Chest X-rays on admission from first case (left) and second case (right).
A 28 year-old primigravida presented at 28 + 6 weeks of gestation with five days of fever, cough, diarrhoea and vomiting. She was Asian and had gestational diabetes. She was tachypnoeic, and bibasal pulmonary infiltrates supported a presumed SARS-CoV-2 diagnosis (Fig. 1). Corticosteroids for fetal maturation were administered. After 38 h, deteriorating respiratory failure prompted multidisciplinary (obstetric, anaesthetic and intensivist) discussions. Non-invasive ventilation was ruled out as it risked unscheduled delivery for maternal respiratory deterioration. Instead she was intubated for caesarean section 42 h after admission (and following magnesium sulphate administration). She was extubated 7 h post-operatively and discharged home on day six. SARS-CoV-2 RNA swab from the mother was positive, and from the baby was negative. Her baby’s Apgar scores were 1 at 1 min and 3 at 5 min. The baby weighed 1.4 kg. The baby continues to make a good recovery (appropriate for gestational age).
To date 3 cases of severe SARS-CoV-2 infection in very preterm pregnancy (<32 weeks) have been published; all underwent caesarean section for maternal resuscitation; one woman died [[1], [2], [3]]. We offer six reflections from our practice:
-
1
Both women deteriorated within 24 h of presentation: we recommend early administration of corticosteroids for fetal maturation.
-
2
Regular multi-disciplinary assessments enabled prompt decision-making.
-
3
Operative delivery improved maternal respiratory mechanics and gas exchange.
-
4
Both women recovered rapidly following operative delivery: this is different from the clinical course of influenza in pregnancy and the recovery of non-pregnant patients with SARS-CoV-2 infection following intubation.
-
5
Prone positioning immediately post-operatively improved acute post-partum hypoxaemia.
-
6
Both women experienced psychiatric sequelae post-operatively: close monitoring is recommended.
Consent
Both women provided written informed consent for publication of this article and the accompanying images.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Zamaniyan M., Ebadi A., Aghajanpoor Mir S., Rahmani Z., Haghshenas M., Azizi S. Preterm delivery in pregnant woman with critical COVID ‐19 pneumonia and vertical transmission. Prenat Diagn. 2020 doi: 10.1002/pd.5713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang X., Zhou Z., Zhang J., Zhu F., Tang Y., Shen X. A case of 2019 Novel Coronavirus in a pregnant woman with preterm delivery. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yan J., Guo J., Fan C., Juan J., Yu X., Li J. Coronavirus disease 2019 (COVID-19) in pregnant women: a report based on 116 cases. Am J Obstet Gynecol. 2020 doi: 10.1016/j.ajog.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]