Abstract
Recommendations for the safe and optimized resumption of cardiac surgery care, research, and education during the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) era were developed by a cardiovascular research consortium, based in 19 countries and representing a wide spectrum of experience with COVID-19. This guidance document provides a framework for restarting cardiac surgery in the outpatient and inpatient settings, in accordance with the current understanding of SARS-CoV-2, the risks posed by interrupted cardiovascular care, and the available recommendations from major societies.
In a survey of 60 cardiac surgery centers in North and South America, Europe, Asia, and Australia, undertaken on March 23, 2020, during the peak of the coronavirus disease 2019 (COVID-19) pandemic and encompassing more than 600 cardiac surgeons, nearly complete cessation of elective cardiac surgery was reported.1 The median reduction in cardiac surgery case volume was 50% to 75%, as most centers indicated not performing any elective surgery, 5% of centers performed no cardiac surgery at all, and one-third of centers reported more than 50% reductions in intensive care capacity.1
However, such acute disruptions, caused by a massive and unexpected spike in demand for critical care beds, an inadequate supply of therapeutic and personal protective equipment (PPE), and widespread risks of infection among patients and health care workers, are already shifting to a chronic state of disease prevalence, for which new ways of providing cardiac surgical care will be needed. The focus of the present document is, therefore, to provide guidance around safely resuming cardiac surgery, research, and education in the described context.
The recommendations presented in this document were developed by committee discussions within a cardiovascular research consortium, based in 19 countries and representing a broad international spectrum of cardiac surgery experience with COVID-19. We aimed to provide a framework for restarting cardiac surgery in the outpatient and inpatient settings, in accordance with the current understanding of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the risks posed by interrupted cardiovascular care, and the available recommendations from major societies.2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12 Our practical recommendations, summarized in Tables 1 and 2 , are intended to support local decision making according to governmental requirements, regional disease prevalence, institutional capacity, and ethics.
Table 1.
Summary of Recommendations for Resuming Cardiac Surgery in the SARS-CoV-2 Era
| Recommendation | Class of Recommendation | Level of Evidence | Relevant Society Recommendation |
|---|---|---|---|
| Restarting cardiac surgery in SARS-CoV-2 era | |||
| The cardiovascular service line, including cardiac surgery, should be among the first clinical services supported to resume elective inpatient and outpatient care as soon as critical care capacity becomes available. | I | C | |
| Flexible institutional triggers and plans for scaling cardiac service line activity up or down in response to government regulations, hospital capacity, and disease burden should be agreed and widely communicated with clinicians to minimize the adverse impact on patients of abrupt changes in clinical practice. | I | C | |
| Reduced cardiac critical care capacity mandates safe and effective triage of elective cardiac surgery patients: such triage should be led by specialists in cardiac surgery, using formal guidelines agreed by the heart team. | I | C | |
| Clear, accurate, and timely information and guidance should be provided to referring physicians, patients, and the community on the availability of cardiovascular services and how to access them. | I | C | |
| A regional response may be a reasonable strategy to ensure appropriate delivery of elective cardiac surgery. | IIa | C | |
| It is reasonable to substitute a less invasive approach if insufficient hospital capacity precludes planned cardiac surgery and patient preference, informed by a shared decision-making approach with the heart team, supports the balance of risk and benefit. | IIa | C | |
| Cardiac surgery care provision | |||
| All cardiac surgery patients should be screened preoperatively for COVID-19 and consideration given to deferring care or other care modalities for patients that test positive. | I | C | |
| Cardiac surgery intensive care should be structured so that cardiac surgical patients with SARS-CoV-2 may be cohorted within the unit and infection risk to other patients and health care workers is minimized. | I | C | |
| Surgical procedures on patients with SARS-CoV-2 should be minimized and performed with strict adherence to protocols designed to mitigate risk posed to health care workers. | I | C | |
| Discharging postoperative cardiac surgery patients to nursing facilities where increased prevalence of SARS-CoV-2 infection and mortality has been observed is not beneficial and may cause harm. | III (no benefit) | C | |
| Cardiac surgery research and education: Recommendations | |||
| Remote working and telemedicine may be used to provide close and convenient patient follow-up and minimize the exposure of patients and health care workers to infection. | IIa | C | |
| It is reasonable to revise resident rotations to address reduced operative experience and support research programs halted or suspended during the pandemic response. | IIa | C |
SARs-CoV-2, severe acute respiratory syndrome coronavirus 2.
Table 2.
Guidance for Adapting Cardiac Surgery Care Delivery in Response to Government Requirements, Hospital Capacity, and Infectious Disease Burden4, 5, 6,10
| Tier | Tier 3 | Tier 2a | Tier 1a |
|---|---|---|---|
| Government advisory | No cardiac surgery Mandatory shelter at home | Priority elective surgery only Social distancing | Resume all elective surgery |
| Critical care capacity | No ICU capacity Most ventilated patients have COVID Ventilated patients > ICU beds | Major restriction Many ventilated patients have COVID | Close to normal capacity No or few ventilated patients have COVID |
| SARS-CoV-2 prevalence | High or rapid increase in prevalence | Moderate or decreasing | Low |
| Coronary | |||
| Shock/OHCA | Medical management | PCI | PCI |
| STEMI | Thrombolysis | PCI with/without mechanical support | CABG/PCI as indicated |
| NSTEMI | Medical management | CABG/PCI as indicated | CABG/PCI as indicated |
| Unstable angina | Medical management | Medical management preferred unless critical left main stem lesion or equivalent, ischemic cardiomyopathy | CABG/PCI as indicated |
| Stable angina | Outpatient management | Medical management unless: Critical left main stem lesion or equivalent, ischemic cardiomyopathy | CABG/PCI as indicated |
| Valve | |||
| Aortic stenosis | Defer TAVR /SAVR Consider outside referral if symptomatic, cardiomyopathy, valve area <0.6cm2 | Defer TAVR /SAVR unless symptomatic, cardiomyopathy, valve area <0.6 cm2 | TAVR/SAVR as indicated |
| Aortic insufficiency | Defer SAVR Consider outside referral if symptomatic, cardiomyopathy, AF | Defer SAVR unless symptomatic, cardiomyopathy, increasing LV size, AF | SAVR as indicated |
| Mitral stenosis | Defer mitral intervention Consider outside referral if symptomatic, cardiomyopathy, AF | Defer mitral intervention unless symptomatic, cardiomyopathy, increasing LV size, AF | MVR /MBV as indicated |
| Mitral insufficiency | |||
| Endocarditis | Medical management Consider outside referral if heart failure, uncontrolled sepsis, conduction block, prosthetic IE | Defer surgery unless heart failure, uncontrolled sepsis, conduction block, prosthetic IE | Surgery as indicated |
| Aorta | |||
| Type A dissection | Emergency surgery if critical care bed available, otherwise seek alternate care at peer institutions with capacity | Surgery as indicated | Surgery as indicated |
| Type B dissection | Medical management unless malperfusion indicates TEVAR | ||
| Aortic aneurysm | Defer unless symptomatic, rapid growth (>0.5 cm/6 months) large size (>6 cm) | ||
| Complex | |||
| Mechanical support | Outside referral with exception of ECMO if capacity and experience permits | Defer unless decompensating heart failure | |
| Transplant | Medical management | UNOS status 1-3 only | |
| Congenital | Outside referral or medical management | Defer unless decompensating heart failure, failure to thrive | Surgery as indicated |
| Emergency (eg, coronary dissection, tamponade) | Emergency surgery if critical care bed available otherwise seek alternate care at peer institutions with capacity | Surgery as indicated | Surgery as indicated |
| Outpatient | |||
| Outpatient clinics | Limit to urgent assessment deferred and deteriorating patients, use video visits where possible | Increase use of video visits for early postoperative follow-up, close follow-up of all deferred patients | |
| Noninvasive imaging | Urgent assessment only | Assessment priority patients | Imaging as indicated |
| Invasive imaging | Emergency evaluation only | Assessment priority patients | Imaging as indicated |
AF, atrial fibrillation; CABG, coronary artery bypass grafting; COVID-19, coronavirus disease 2019; ECMO, extracorporeal membrane oxygenation; ICU, intensive care unit; IE, infectious endocarditis; LV, left ventricular; MBV, mitral balloon valvuloplasty; MVR, mitral valve replacement; NSTEMI, non-ST segment elevation myocardial infarction; OHCA, out of hospital cardiac arrest; PCI, percutaneous coronary intervention; SAVR, surgical aortic valve replacement; STEMI, ST segment elevation myocardial infarction; TAVR, transcatheter aortic valve replacement; TEVAR, thoracic endovascular aortic repair; UNOS, United Network for Organ Sharing.
Tier 1 and 2 differ from those in guidance describing pre-peak response. The late phase recommendations reflect the likelihood of prolonged phase of persistent COVID-19 prevalence in hospital and community after peak phase, during which time adapting practice is preferable to deferring elective patients indefinitely.
A. Guidance on Restarting Cardiac Surgery Activity
Class I Recommendations
-
1.
The cardiovascular service line, including cardiac surgery, should be among the first clinical services supported to resume elective inpatient and outpatient care as soon as critical care capacity becomes available. (Level of evidence: C)
The incremental mortality associated with suspending all elective cardiac surgery within a wide geographic region for 6 to 8 weeks may be estimated from studies of health care systems where surgery is routinely deferred for many weeks because of lack of capacity. For example, in 5864 patients waiting for elective or urgent coronary bypass surgery in Sweden, the risk of death increased by 11% per month.13 A New Zealand study demonstrated significant incremental operative mortality in the nearly 20% of patients readmitted with acute coronary syndromes while waiting for bypass surgery.14 A coordinated approach with cardiology services, including invasive cardiology is essential, because these are an integral part of the cardiovascular patient evaluation and management. Supporting references: 13, 14.
-
2.
Triggers and contingency plans for modifying cardiac service line activity in response to government regulations, hospital capacity, and disease burden should be agreed upon and clearly communicated with clinicians to minimize adverse events due to abrupt changes in clinical practice. (Level of evidence: C)
A clear response framework, such as the one outlined in Table 2,4 , 6, 7, 8, 9, 10 enables the cardiac service line to adapt more safely and effectively to changes in governmental requirements, critical care capacity, and prevalence of disease in the community. If advisories conflict, federal and state mandates take priority over hospital policy and local assessment of disease burden. Cardiac specialists triaging patients within a resource allocation of critical care and floor beds, operating room, and outpatient time, may allow a more efficient response to evolving constraints than attempting to redefine which patients should be prioritized at each stage. Supporting references: 4-6.
-
3.
Reduced cardiac critical care capacity mandates safe and effective triage of elective cardiac surgery patients. Such triage should be led by specialists in cardiac surgery, using formal guidelines as agreed by the heart team (Table 2). (Level of evidence: C)
The incremental mortality in patients whose cardiac surgery is deferred during this pandemic may be partially mitigated by effective triage with careful attention to risk factors such as symptoms, ventricular dysfunction, arrhythmias, and age, considering percutaneous coronary or valve intervention and optimizing medical therapy with frequent follow-up. For example, risk factors for death while waiting for coronary bypass included left main stem disease, reduced ejection fraction, unstable angina, and atrial fibrillation.13 Untreated aortic stenosis is associated with higher mortality. In a recent analysis of 823 patients waiting an average of 3 weeks for transcatheter or surgical aortic valve replacement, the mortality was 4% at 1 month in both groups.15 Patients who died were significantly older and more likely to have left ventricular dysfunction or New York Heart Association Functional Classification II or IV symptoms.
Involving cardiac surgeons early in the development of specific guidance and triage committees is essential, particularly when cancer, trauma, and other urgent care needs must be balanced, because the methods routinely used to allocate resources and prioritize patients across multiple specialties are aimed at optimizing normal daily resource use and are not designed to balance risks of deferring surgery. Very complex and high-risk cases should be performed when critical care capacity is adequate with resources for extended support, whereas if those resources are scarce the utility and ethics may be less justifiable. Supporting references: 4-6, 12-15.
-
4.
Clear, accurate, and timely information on the availability of cardiovascular services and how to access them should be provided to referring physicians, patients, and the community. (Level of evidence: C)
The substantial decrease in elective and emergency cardiovascular presentations to outpatients and the emergency departments observed in most centers can be attributed, firstly, to reduced access to primary care offices, and secondly, to necessary triage by emergency responders, and thirdly, to high levels of patient concern about visiting hospitals. Initial reports suggest this may account for significant incremental non-COVID cardiac mortality.16 Consistent, accurate, and effective communication with primary care and cardiology providers is essential to ensure that their approach is aligned with the availability of inpatient cardiac care and that patient concerns are allayed. This may usefully be supported by direct patient messaging, without which news stories in the lay media provide the sole information for patients making decisions about their health care options. Supporting reference: 16.
Class IIa Recommendations
-
1.
A regional response is a reasonable strategy to ensure appropriate delivery of elective cardiac surgery. (Level of evidence: C)
A regional response entails a coordinated effort to increase and optimize critical care capacity, expertise, and personnel between hospitals, preserving the ability of selected centers to provide cardiac surgery services on behalf of an expanded population while other centers divert resources to managing SARS-CoV-2. In Italy and the United Kingdom, this type of regional response has enabled continuous provision of cardiac surgery at selected high-volume centers and coordination of effort and experience for extracorporeal membrane oxygenation (ECMO) support.17 In comparison, disaster planning in the United States is primarily organized at an individual hospital level, with governmental agencies issuing mandates to hospitals restricting elective surgery, leading to complete cessation of elective cardiac surgery for several weeks in most regions. Supporting reference: 17.
-
2.
It is reasonable to substitute a less-invasive approach when insufficient hospital capacity precludes planned cardiac surgery, and when patient preference informed by a shared-decision-making approach with the Heart Team also supports the balance of risks. (Level of evidence: C)
Most low-risk elective patients may safely wait up to 4 weeks for planned cardiac surgery.4, 5, 6 However, mortality and complications may occur in apparently low-risk patients.6 If urgent surgery is not possible, any clinical deterioration indicating a need for more urgent intervention should trigger a discussion with the heart team to review alternative therapeutic strategies, including surgery at another peer center, transcatheter valve intervention, or percutaneous coronary intervention, or a combination of these.10 Supporting references: 4-6, 10.
B. Guidance on Adapting Cardiac Surgery Care
Class I Recommendations
-
1.
All cardiac surgery patients should be screened preoperatively for COVID-19 and strong consideration be given to deferring care or using other care modalities for patients that test positive. (Level of evidence: C)
All cardiac surgery patients should be tested 48 hours preoperatively for COVID-19, until the prevalence of asymptomatic community spread is minimal. Anecdotal reports indicate that COVID-19 infection in the perioperative period is associated with significant morbidity and mortality, so cardiac surgery should be deferred where possible until the patient tests negative. In a patient with active COVID-19 infection who cannot safely be deferred, percutaneous and transcatheter therapies may be the safer option. Lung and heart transplant donors and recipients should be screened and no transplants performed in positive patients. An important additional rationale for screening cardiac surgery patients for SARS-CoV-2 is the risk posed to health care workers during intubation, extubation, disconnection of the ventilator, and bronchoscopy from aerosolization.8 Supporting references: 5, 8.
-
2.
Cardiac surgery intensive care should be structured so that cardiac surgical patients with CoV-SARS-2 may be regrouped at one dedicated area within the unit and infection risks to other patients and health care workers minimized. (Level of evidence: C)
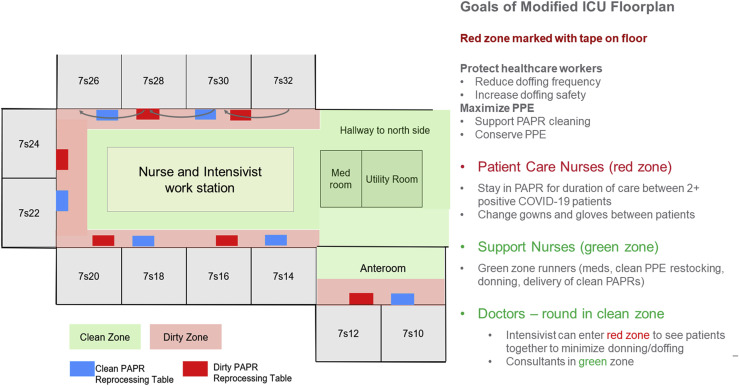
It may not be feasible to cohort patients in whom SARS-CoV-2 is identified after cardiac surgery or COVID-19 patients on venoarterial ECMO on a separate COVID unit, because of the specialized nursing and intensivist care required perioperatively. Negative pressure bays within the cardiac surgery intensive care unit should therefore be dedicated to the care of cardiac surgery patients with SARS-CoV-2. Immunocompromised patients, including transplant recipients, should be cohorted in the intensive care unit area most distant from this. Epidemiology and infection protocols should guide designation of clean and contaminated space in the COVID area (Figure 1 ). Limitations on visitors, in-room rounding, and care pathways should be redesigned to minimize traffic through the COVID area. Careful and frequent education of nursing, intensivist staff, and consultant staff in use of PPE, virtual rounding, and dedicated teams for high-risk procedures, such as intubations, will minimize the risk of cross-infection. Every effort should be made to cohort nursing, respiratory technicians, physiotherapists, imaging technicians, and other staff to care of either COVID or non-COVID patients during a single shift. Specific protocols for postoperative emergencies (cardiac arrest) in COVID-19–positive patients who have undergone cardiac surgery should be developed according to local resources and may include restricting the indications for return to the operating room and a dedicated emergency equipment cart to facilitate bedside emergency resternotomy, ECMO, chest tube, or catheter placement. Supporting references: 5, 6.
-
3.
Surgical procedures on patients with SARS-CoV-2 should be minimized and performed with strict adherence to protocols designed to mitigate risk posed to health care workers. (Level of evidence: C)
Figure 1.
Intensive care unit floor plan modified to facilitate management of patients with severe acute respiratory syndrome coronavirus 2 (SARS-COV-2). (COVID-19, coronavirus disease 2019; ICU, intensive care unit; PAPR, powered air respiratory protection; PPE, personal protective equipment.) (Modified with permission from Peter Chen, MD.)
At the time of this writing, more than 19% of patients infected with SARS-CoV2 and 60 deaths in Italy alone were health care workers. Intubation and extubation, disconnection from the ventilator, bronchoscopy, and tracheostomy expose the health care team to the greatest risk of viral transmission. This was recognized at a relatively early stage in a joint position statement from the American Society of Anesthesiologists, which recommended full-powered air-purifying respirators for induction and extubation of patients in endemic areas.8
There are noticeable disparities between PPE protocols between different centers in different regions and countries.8 , 18, 19, 20, 21 The American College of Surgeons recommends N95 respirators, particularly when operating on patients with confirmed or suspected COVID-19.9 Thus, for individuals at highest risk of exposure at institutions that are unable to provide N95 masks to all members of the operating team, the American College of Surgeons recommends that all surgeons and other personnel who are not wearing N95s leave the operating room during intubation, extubation, and other necessary adjunct procedures that can generate aerosolized small particles.8 Team simulations to practice in advance of these common clinical scenarios may improve safety. Procedural aspects of the procedures should be modified in patients with SARS CoV-2 to decrease aerosolization, including using lower coagulation settings for electrocautery, avoiding endoscopic vein harvesting to minimize aerosolization with CO2 insufflation and avoiding ventilator tubing disconnection. Supporting references: 8, 9, 18-21.
Class III Recommendation
-
1.
It may be harmful to discharge postoperative cardiac surgery patients to nursing facilities where increased prevalence of SARS-CoV-2 infection and mortality has been observed. (Level of evidence: C)
The prevalence of SARS-CoV-2 and associated mortality in long-term community nursing facilities in the United States was especially high, and it is therefore not advisable to discharge postoperative patients to facilities where increased risk of SARS-CoV-2 remains a concern. Where institutions have relied on these facilities, it will be necessary to develop new discharge strategies to avoid the risk of community infection after hospital discharge. These should include extended hospital admission to maximize independence and planning for skilled home nursing support. Educating all patients and family members preoperatively in social distancing, use of PPE, and recognizing when to seek medical advice is essential.
C. Guidance on Managing Cardiac Surgery Research and Education
Class I Recommendations
-
1.
Remote working and telemedicine should be used to provide close and convenient patient follow-up and minimize exposure of patients and health care workers to infection. (Level of evidence: C)
Telemedicine for outpatient visits and remote working, including video conferencing, is a potentially helpful practice change to emerge from the pandemic response. In the United States, many states and health care payers approved payment for clinical consultations and follow-up conducted by video (although not phone only). Effective, early roll-out of secure, patient confidentiality-compliant video consultations will help mitigate the reluctance of patients with advanced cardiac morbidity to seek appropriate care and allow closer follow-up of patients deferred for surgery. For postoperative patients, community primary care or cardiology practices may be willing to provide in-person visits where suture removal and incision checks can be performed. Hospital workflow may also use remote working in the form of video rounds and conferences that facilitate team-based decision making, education, and administrative meetings while social distancing.
Class IIa Recommendation
-
1.
It is reasonable to revise resident rotations to address reduced operative experience, and support research programs halted or suspended during the pandemic response. (Level of evidence: C)
Educational activity was suspended or reduced in 50% of cardiac surgery centers that responded to a survey that also showed a reduction of 50% to 75% in operative cases.1 This may have the greatest effect in countries such as the United States where the total time spent in cardiac surgery training may be as little as 12 months and could explain why half of centers were still allowing residents to operate, even at the expense of prolonging surgery times. Research activity was similarly impacted, which may hamper efforts to obtain early data and underlines the need for real-time data collection and analysis that could inform practice in real time. The reallocation of funding activity and journal focus to research on SARS-CoV-2 may divert resources from equally impactful cardiac research. Coordinated follow-up of all cardiac surgery patients to quantify the incidence and outcomes of the COVID-19 infection and the outcomes related to deferred surgery in this population is essential to inform future policy and individual consent.
Conclusions
The above practice recommendations provide an expert-based framework for restarting cardiac surgery in the outpatient and inpatient settings in a health care environment characterized by a low-grade long-term prevalence of SARS-CoV-2. Although the applicability of these recommendations may vary according to local context and as new information becomes available, we anticipate that this guidance document will assist centers in managing the 2 simultaneous threats—COVID-19 and death/morbidity in patients awaiting cardiac surgery—that institutions providing cardiac surgical care must now constantly balance.
Acknowledgments
Dr Fremes is supported in part by the Bernard S. Goldman Chair in Cardiovascular Surgery. The authors wish to thank the Cornell Joint Clinical Trial Office for its support in this project.
References
- 1.Gaudino M, Chikwe J, Hameed I, et al. Response of cardiac surgery units to COVID-19: an internationally-based quantitative survey [e-pub ahead of print]. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.120.047865, accessed April 29, 2020. [DOI] [PMC free article] [PubMed]
- 2.Wood D.A., Sathananthan J., Gin K. Precautions and procedures for coronary and structural cardiac interventions during the COVID-19 pandemic: guidance from Canadian Association of Interventional Cardiology. Can J Cardiol. 2020;36:780–783. doi: 10.1016/j.cjca.2020.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shah P.B., Welt F.G.P., Mahmud E. Triage considerations for patients referred for structural heart disease intervention during the COVID-19 pandemic: an ACC/SCAI position statement. JACC Cardiovasc Interv. 2020;13:1484–1488. doi: 10.1016/j.jcin.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wood D.A., Mahmud E., Thourani V.H. Safe reintroduction of cardiovascular services during the COVID-19 pandemic: from the North American society leadership. Ann Thorac Surg. 2020;110:733–740. doi: 10.1016/j.athoracsur.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haft J.W., Atluri P., Ailawadi G. Adult cardiac surgery during the COVID-19 pandemic: a tiered patient triage guidance statement. Ann Thorac Surg. 2020;110:697–700. doi: 10.1016/j.athoracsur.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hassan A., Arora R.C., Adams C. Cardiac surgery in Canada during the COVID-19 pandemic: a guidance statement from the Canadian Society of Cardiac Surgeons. Can J Cardiol. 2020;36:952–955. doi: 10.1016/j.cjca.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centers for Medicare & Medicaid Services Non-Emergent, Elective Medical Services, and Treatment Recommendations. https://www.cms.gov/files/document/31820-cms-adult-elective-surgery-and-procedures-recommendations.pdf Available at:
- 8.American Society of Anesthesiologists UPDATE: The Use of Personal Protective Equipment by Anesthesia Professionals During the COVID-19 Pandemic. https://www.asahq.org/about-asa/newsroom/news-releases/2020/03/update-the-use-of-personal-protective-equipment-by-anesthesia-professionals-during-the-covid-19-pandemic Available at:
- 9.American College of Surgeons Personal Protective Equipment (PPE): ASA and APSF Joint Statement on Perioperative Testing for the COVID-19 Virus. https://www.facs.org/covid-19/ppe Available at:
- 10.Kirkpatrick J.N., Mitchell C., Taub C., Kort S., Hung J., Swaminathan M. ASE statement on protection of patients and echocardiography service providers during the 2019 novel coronavirus outbreak. J Am Coll Cardiol. 2020;75:3078–3084. doi: 10.1016/j.jacc.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choi A.D., Abbara S., Branch K.R. Society of Cardiovascular Computed Tomography guidance for use of cardiac computed tomography amidst the COVID-19 pandemic. J Cardiovasc Comput Tomogr. 2020;14:101–104. doi: 10.1016/j.jcct.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mahmud ED, Dauerman HL, Welt FGP, et al. Management of acute myocardial infarction during the COVID-19 pandemic [e-pub ahead of print]. J Am Coll Cardiol. https://doi.org/10.1016/j.jacc.2020.04.039, accessed April 29, 2020. [DOI] [PMC free article] [PubMed]
- 13.Rexius H., Brandrup-Wognsen G., Odén A., Jeppsson A. Mortality on the waiting list for coronary artery bypass grafting: incidence and risk factors. Ann Thorac Surg. 2004;77:769–774. doi: 10.1016/j.athoracsur.2003.05.007. [discussion: 774-775] [DOI] [PubMed] [Google Scholar]
- 14.Seddon M., French J., Amos D., Ramanathan K., McLaughlin S., White H. Waiting times and prioritisation for coronary artery bypass surgery in New Zealand. Heart. 1999;81:586–589. doi: 10.1136/hrt.81.6.586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Malaisrie S.C., McDonald E., Kruse J. Mortality while waiting for aortic valve replacement. Ann Thorac Surg. 2014;98:1564–1570. doi: 10.1016/j.athoracsur.2014.06.040. [discussion: 1570-1571] [DOI] [PubMed] [Google Scholar]
- 16.De Fillippo O., D’Ascenzo F., Angelini F. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ramanathan K., Antognini D., Combes A. Planning and provision of ECMO services for severe ARDS during the COVID-19 pandemic and other outbreaks of emerging infectious diseases. Lancet Respir Med. 2020;8:518–526. doi: 10.1016/S2213-2600(20)30121-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention Coronavirus Disease 2019 (COVID-19). Strategies for Optimizing the Supply of N95 Respirators. https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirators-strategy/crisis-alternate-strategies.html Available at:
- 19.Centers for Disease Control and Prevention Coronavirus Disease 2019 (COVID-19). Checklist for Healthcare Facilities: Strategies for Optimizing the Supply of N95 Respirators During the COVID-19 Response. 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/checklist-n95-strategy.html Available at:
- 20.Centers for Disease Control and Prevention Interim Infection Prevention and Control Recommendations for Patients With Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings. https://www.cdc.gov/coronavirus/2019-ncov/infection-control/control-recommendations.html Available at:
- 21.Peng S, Huang L, Zhao B, et al. Clinical course of coronavirus disease 2019 in 11 patients after thoracic surgery and challenges in diagnosis [e-pub ahead of print]. J Thorac Cardiovasc Surg. 10.1016/j.jtcvs.2020.04.005, accessed April 29, 2020. [DOI] [PMC free article] [PubMed]