ABSTRACT
The 2016 and 2017 National Immunization Surveys-Teen (NIS-Teen) highlighted disparities in human papillomavirus (HPV) vaccination coverage by metropolitan statistical area (MSA) status. Coverage with ≥1 dose of HPV vaccine was significantly lower among teens in suburban and mostly rural areas than it was among those in mostly urban areas. Reasons underlying this disparity are poorly understood; this analysis sought to identify sociodemographic factors associated with not initiating the HPV vaccine series and to determine whether these factors differed by MSA status. Using NIS-Teen data for a sample of 41,424 adolescents from the 2016 and 2017 survey years, multivariate logistic regression was utilized to assess associations between various sociodemographic factors and non-initiation of the HPV vaccine series by MSA status. Adjusted prevalence ratios and 95% confidence intervals are reported. A secondary analysis assessed missed opportunities for HPV vaccination by MSA status and estimated what coverage could be if these missed opportunities had not occurred. Most factors associated with not receiving HPV vaccine were similar across all three MSAs, including living in the South, having a mother with some college education, not having an 11–12-year-old well-child visit, and not receiving a provider recommendation for vaccination. Others were associated with non-initiation of the HPV vaccine series in only specific MSAs. Teens in suburban areas (82.2%) were more likely to miss opportunities for HPV vaccination than those in mostly urban (79.3%) areas. Coverage with ≥1 dose of HPV vaccine in all three MSAs would be substantially higher if these missed opportunities had been eliminated.
KEYWORDS: Human papillomavirus (HPV), adolescents, urban, rural, disparity, sociodemographic factors
Introduction
The Advisory Committee on Immunization Practices (ACIP) recommends adolescents aged 11–12 years routinely receive one dose of the tetanus, diphtheria, and acellular pertussis vaccine (Tdap), one dose of quadrivalent meningococcal conjugate vaccine (MenACWY), and the first dose of human papillomavirus (HPV) vaccine. The recommendation is for administration of all three vaccines at the same 11–12-year-old preventive visit.1 The 9-valent (9vHPV) vaccine, which is currently the only HPV vaccine available in the United States, provides protection against genital warts and precancerous lesions caused by HPV infection.2 In addition, HPV vaccination is indicated for the prevention of cervical, vulvar, vaginal, and anal cancers caused by high-risk HPV types 16, 18, 31, 33, 45, 52, and 58.2 The Centers for Disease Control and Prevention (CDC) estimate that over 90% of these HPV-attributable cancers could be prevented with vaccination.3 Data from the 2017 National Immunization Survey-Teen (NIS-Teen) indicate that 88.7% of teens had received ≥1 dose of Tdap and 85.1% had received ≥1 dose of MenACWY but only 65.5% of adolescents had received ≥1 dose of HPV vaccine and only 48.6% completed the vaccine series.4 Despite high coverage rates for Tdap and MenACWY, low coverage rates for HPV vaccine indicate that many teens miss opportunities to prevent HPV infections and HPV-attributable cancers.
CDC recently highlighted a disparity in HPV vaccination coverage by metropolitan statistical area (MSA) status. In 2016, coverage for ≥1 dose HPV vaccine among adolescents in MSA, non-principal cities and non-MSAs was 7.5 and 15.6 percentage points lower than it was among those in MSA, principal cities, respectively.5 This disparity was not observed for Tdap and was less pronounced for MenACWY. The disparity in HPV vaccination coverage by MSA status persisted the following year. In 2017, coverage for ≥1 dose HPV vaccine among adolescents in MSA, non-principal cities and non-MSAs was 7.0 and 10.8 percentage points lower than it was among those in MSA, principal cities, respectively.4 In this analysis, we refer to MSA, principal cities as “mostly urban” areas; MSA, non-principal cities as “suburban” areas; and non-MSAs as “mostly rural” areas. This disparity in HPV vaccination coverage is concerning because the burden of HPV-associated cancers is often highest in rural areas. One study examined incidence rates and annual percentage change for HPV-associated cancers during 1995–2013; rates of HPV-associated cancers were higher in rural compared to urban areas.6 Similarly, a more recent analysis examined cervical cancer stage at diagnosis by urban-rural status.7 Authors noted higher incidence of cervical cancer in rural counties at every stage, when compared to urban counties.7 Several factors may contribute to the increased disease burden in rural areas, including a lack of primary care providers and a lack of provider recommendations for screening and preventive care services.8-10 Regarding HPV vaccination as a specific preventive measure, barriers in rural areas may include financial and/or access-related limitations in addition to lack of provider recommendation for vaccination.8-11 Geographic disparities pertaining to knowledge of HPV, its linkage to cervical cancer, and HPV vaccine have also been reported, with rural residents being less informed.12 Finally, fatalistic beliefs about cancer prevention efforts among rural residents and its negative impact on HPV vaccination have also been cited as contributing factors.13-15
There are limited data examining differences in HPV vaccination coverage by MSA status, particularly among adolescents not initiating the HPV vaccine series. A 2014 analysis noted lower coverage for ≥1 dose of HPV vaccine among adolescents living in other areas when compared to those living in mostly urban areas.8 More recently, a 2016 analysis by Henry et al. found that adolescent girls living in urban communities had higher odds of initiating the HPV vaccine series than those in rural areas.9 Another analysis found that U.S. males in urban areas were more likely to initiate the vaccine series than those from rural communities.10 However, reasons underlying the disparity are poorly understood. Identifying factors associated with not receiving HPV vaccine is an initial step toward understanding this disparity. The purpose of this analysis was to identify sociodemographic factors associated with not initiating the HPV vaccine series and to determine whether these factors differed by MSA status.
Materials and methods
The data source utilized for this analysis was the NIS-Teen for the 2016 and 2017 survey years. CDC conducts the NIS-Teen annually to estimate coverage of ACIP-recommended adolescent vaccines among a nationally representative sample of adolescents aged 13–17 years in the 50 U.S. states, the District of Columbia, and certain local areas. The survey consists of two phases: the first is a household telephone interview and the second a provider questionnaire. During the first phase, random digit dialing is used to identify households with age-eligible adolescents. Once an eligible adolescent is identified, a standardized household telephone interview is performed and parents or guardians are asked questions about their teen’s vaccination history and about sociodemographic characteristics of the adolescent and their household. Parents or guardians are also asked for permission to contact the teens’ vaccination provider(s). During the second phase and with parental/guardian consent, an immunization history questionnaire is mailed to the adolescent’s vaccination provider(s). Providers indicate the types of vaccinations the teen has received along with the number of doses and dates of administration. Thus, vaccination coverage estimates are based on provider-reported vaccination histories.11 Some providers were employed by federally qualified health centers. Data for NIS-Teen are weighted to account for nonresponses and noncoverage, allowing for population-based estimates. Details of NIS-Teen sampling methodology have been published elsewhere, and information about this methodology is publicly available.16-18 The NIS-Teen protocol was reviewed and approved by CDC’s National Center for Health Statistics Research Ethics Review Board.
We analyzed combined NIS-Teen data for the 2016 and 2017 survey years to examine whether unvaccinated teens (for HPV vaccine) differed by geographic area. MSA status was determined by household county of residence: mostly urban areas, suburban areas, and mostly rural areas. We began by estimating the weighted percentage of multiple sociodemographic characteristics overall and by MSA status. Descriptive characteristics were divided into three categories and chosen based on previous studies indicating associations with HPV vaccine uptake.10,19-23 The three categories included adolescent characteristics (age, sex, race/ethnicity, immigration status, and region of residence); maternal characteristics (maternal age, maternal educational attainment, maternal marital status; and parental awareness of the Vaccines for Children [VFC] program24); and access-to-care factors (income-to-poverty ratio, insurance status, the presence or absence of an 11–12-year-old well-child visit, parental report of provider recommendation for HPV vaccine, and vaccination facility type). Poverty level was analyzed using the “income-to-poverty ratio” variable, which is the ratio of each family’s income to their respective poverty threshold based on family size and federal poverty guidelines.25 Ratios less than 100% represent family incomes below the federal definition of poverty, while those above 100% are above the poverty level.25 Insurance categories were mutually exclusive and categorized as either private only, any Medicaid, other, or uninsured. Of note, “other” includes the Children’s Health Insurance Program (CHIP), military insurance, Indian Health Service, and any other type of health insurance not mentioned elsewhere. Although the “provider recommendation for HPV vaccine” variable was based on parental report, we included it in the “access-to-care” category because multiple studies have strongly linked provider recommendation with parental acceptance of the HPV vaccine for their teen(s).26-28 Vaccination facility types were designated as either all-private facilities, all public facilities, all hospital facilities, all sexually transmitted disease (STD)/school/teen clinics or other facilities, mixed facilities, or “other” facility types. Mixed vaccination facility types refers to teens who visited a combination of facility types (e.g., visiting both public and private facilities for vaccines) while “other” facilities included military clinics; Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) clinics; and pharmacies. Using mostly-urban areas as the reference group, t-tests were used to compare the weighted percentage of sociodemographic factors by MSA status. We then performed a bivariate analysis to identify sociodemographic factors associated with non-initiation of the HPV vaccine series within each MSA. A multiple logistic regression analysis was then conducted to evaluate if these relationships changed after adjusting for each of the other sociodemographic factors. Adjusted prevalence ratios and their corresponding 95% confidence intervals (95% CI) are reported.
Since ACIP recommends administration of HPV vaccine during the same pre-adolescent visit as Tdap and MenACWY, a secondary analysis was performed to evaluate missed-opportunities for HPV vaccination by MSA status. A missed opportunity was defined as a health-care encounter during which an adolescent received at least one other vaccine but did not initiate the HPV vaccine series. Similar to a prior analysis, for girls, we included all health-care encounters that occurred on or after a girl’s 11th birthday and before her 13th birthday, and on or after March 23, 2007 when the ACIP recommendations for the use of the quadrivalent HPV vaccine for girls were published in CDC’s Morbidity and Mortality Weekly Report (MMWR).29 For boys, we included health-care encounters occurring on or after a boy’s 11th birthday and before his 13th birthday, and on or after December 23, 2011 when the ACIP recommendations for the use of the quadrivalent HPV vaccine for males were published in the MMWR.29 Similarly, we also calculated what coverage for ≥1 dose of HPV vaccine among the combined 2016 and 2017 survey sample would potentially be, if these missed opportunities had been eliminated.
To account for the complex survey design, all analyses for this study were performed using SAS-callable SUDAAN® 11 (RTI International, Research Triangle Park, North Carolina). Statistical significance was set at an alpha level of 0.05.
Results
A total of 41,424 adolescents were in the combined NIS-Teen 2016 and 2017 survey samples (20,475 in 2016; 20,949 in 2017). The distribution of teens by geographic area was 40.7% from mostly urban areas, 46.9% from suburban areas, and 12.4% from mostly rural areas (Table 1). As reported in Table 1, the majority of adolescents in the sample were aged 13–15 years (60.6%), U.S. born (93.5%), and lived in a household where the mother was married (67.8%). A plurality of adolescents had a mother who was a college graduate (40.0%) and lived in households with an income-to-poverty ratio at the lowest level – <133% (31.5%) (Table 1). Most adolescents had parents who were unaware of the VFC program (62.4%) and had parents who reported receiving a provider recommendation for HPV vaccine (73.4%). About half of adolescents were non-Hispanic white (52.5%), had a mother who was age 45 years or older (47.9%), had private insurance (51.4%), and had a well-child visit at age 11 or 12 years (47.0%). Of note, a higher proportion of adolescents who had initiated the HPV vaccine series (51.7%) had an 11–12-year-old well-child visit compared to unvaccinated (for HPV vaccine) teens (38.9%) (data not included in tables).
Table 1.
Characteristics of adolescents aged 13–17 years by metropolitan statistical area (MSA) status – National Immunization Survey–Teen, United States, 2016–2017.
| Metropolitan Statistical Area (MSA) |
||||||||
|---|---|---|---|---|---|---|---|---|
| Overall |
Mostly Urban |
Suburban |
Mostly Rural |
|||||
| Characteristic | Sample Size | Weighted % (95% C.I.) | Sample Size | Weighted % (95% C.I.) | Sample Size | Weighted % (95% C.I.) | Sample Size | Weighted % (95% C.I.) |
| Total | 41,424 | 100.0 (---------) | 16,523 | 40.7 (39.8–41.6) | 16,530 | 46.9 (46.0–47.8) | 8,371 | 12.4 (12.0–12.9) |
| Survey Year | ||||||||
| 2016 | 20,475 | 50.0 (49.4–50.6) | 7,979 | 49.3 (48.1–50.6) | 8,248 | 50.0 (48.8–51.1) | 4,248 | 52.3 (50.6–54.1)* |
| 2017 | 20,949 | 50.0 (49.4–50.6) | 8,544 | 50.7 (49.4–51.9) | 8,282 | 50.0 (48.9–51.2) | 4,123 | 47.7 (45.9–49.4)* |
| Age (years) | ||||||||
| 13–15 | 25,502 | 60.6 (59.7–61.5) | 10,218 | 59.6 (58.1–61.1) | 10,171 | 61.7 (60.4–63.0)* | 5,113 | 59.7 (57.8–61.5) |
| 16–17 | 15,922 | 39.4 (38.5–40.3) | 6,305 | 40.4 (38.9–41.9) | 6,359 | 38.3 (37.0–39.6)* | 3,258 | 40.3 (38.5–42.2) |
| Sex | ||||||||
| Male | 21,918 | 51.0 (50.1–52.0) | 8,766 | 51.6 (50.1–53.1) | 8,709 | 50.4 (49.0–51.7) | 4,443 | 51.7 (49.8–53.6) |
| Female | 19,506 | 49.0 (48.0–49.9) | 7,757 | 48.4 (46.9–49.9) | 7,821 | 49.6 (48.3–51.0) | 3,928 | 48.3 (46.4–50.2) |
| Race/ethnicity | ||||||||
| Non-Hispanic White | 25,893 | 52.5 (51.6–53.4) | 8,312 | 41.0 (39.7–42.4) | 11,323 | 58.4 (57.0–59.7)* | 6,258 | 68.2 (66.3–70.0)* |
| Non-Hispanic Black | 3,733 | 13.8 (13.2–14.4) | 2,197 | 19.0 (17.9–20.3) | 1,116 | 10.3 (9.5–11.2)* | 420 | 9.6 (8.4–10.9)* |
| Hispanic | 7,105 | 23.4 (22.6–24.3) | 4,009 | 29.0 (27.5–30.5) | 2,279 | 21.5 (20.2–22.9)* | 817 | 12.6 (11.3–14.0)* |
| American Indian/Alaskan Native | 557 | 0.9 (0.8–1.0) | 131 | 0.5 (0.4–0.7) | 129 | 0.6 (0.5–0.9) | 297 | 3.1 (2.4–3.9)* |
| Asian | 1,680 | 4.3 (3.9–4.7) | 855 | 5.4 (4.7–6.1) | 721 | 4.2 (3.7–4.9)* | 104 | 1.0 (0.6–1.7)* |
| Other | 2,456 | 5.1 (4.7–5.4) | 1,019 | 5.1 (4.6–5.7) | 962 | 4.9 (4.4–5.5) | 475 | 5.5 (4.7–6.4) |
| Immigration status | ||||||||
| Born in U.S. | 39,126 | 93.5 (93.0–94.0) | 15,226 | 90.7 (89.6–91.7) | 15,757 | 94.8 (94.1–95.4)* | 8,143 | 97.9 (97.4–98.4)* |
| Born outside U.S. | 2,045 | 6.5 (6.0–7.0) | 1,203 | 9.3 (8.3–10.4) | 678 | 5.2 (4.6–5.9)* | 164 | 2.1 (1.6–2.6)* |
| Region | ||||||||
| Northeast | 8,024 | 16.4 (16.1–16.7) | 2,288 | 12.3 (11.7–13.0) | 4,520 | 22.0 (21.3–22.7)* | 1,216 | 8.7 (7.8–9.7)* |
| Midwest | 8,798 | 21.4 (21.0–21.8) | 3,204 | 20.1 (19.3–21.0) | 3,061 | 19.2 (18.5–19.9) | 2,533 | 33.9 (32.3–35.5)* |
| South | 15,652 | 38.3 (37.8–38.9) | 7,080 | 37.9 (36.7–39.1) | 6,204 | 37.5 (36.4–38.5) | 2,368 | 43.1 (41.3–44.9)* |
| West | 8,950 | 23.9 (23.2–24.5) | 3,951 | 29.7 (28.3–31.1) | 2,745 | 21.4 (20.1–22.7)* | 2,254 | 14.3 (13.2–15.5)* |
| Mother’s age | ||||||||
| ≤34 years | 3,285 | 8.7 (8.2–9.2) | 1,496 | 10.1 (9.3–11.0) | 1,038 | 7.2 (6.5–8.0)* | 751 | 9.4 (8.4–10.5) |
| 35–44 years | 16,757 | 43.4 (42.5–44.3) | 6,492 | 43.2 (41.7–44.7) | 6,419 | 41.7 (40.4–43.1) | 3,846 | 50.5 (48.6–52.3)* |
| ≥45 years | 21,382 | 47.9 (47.0–48.8) | 8,535 | 46.7 (45.2–48.2) | 9,073 | 51.1 (49.7–52.4)* | 3,774 | 40.1 (38.3–41.9)* |
| Mother’s educational level | ||||||||
| <High School | 4,770 | 13.3 (12.6–14.0) | 2,370 | 16.1 (14.9–17.4) | 1,437 | 10.9 (9.9–12.0)* | 963 | 12.8 (11.6–14.2)* |
| High School | 6,394 | 22.3 (21.5–23.1) | 2,503 | 22.6 (21.3–24.0) | 2,232 | 20.2 (19.1–21.4)* | 1,659 | 29.0 (27.2–30.9)* |
| Some college or college graduate | 10,535 | 24.4 (23.6–25.2) | 3,846 | 22.9 (21.7–24.2) | 4,108 | 24.4 (23.2–25.6)* | 2,581 | 29.4 (27.8–31.1)* |
| > College graduate | 19,725 | 40.0 (39.2–40.9) | 7,804 | 38.4 (37.0–39.8) | 8,753 | 44.5 (43.2–45.8)* | 3,168 | 28.8 (27.2–30.4)* |
| Mother’s marital status | ||||||||
| Married | 29,234 | 67.8 (66.9–68.7) | 11,061 | 63.5 (62.0–65.0) | 12,359 | 72.2 (70.9–73.5)* | 5,814 | 64.6 (62.6–66.5) |
| Widowed/divorced/separated | 6,951 | 23.1 (22.2–23.9) | 2,856 | 24.2 (22.8–25.6) | 2,548 | 21.0 (19.9–22.2)* | 1,547 | 27.3 (25.5–29.1)* |
| Never married | 2,541 | 9.2 (8.6–9.8) | 1,433 | 12.3 (11.3–13.4) | 694 | 6.7 (6.0–7.6)* | 414 | 8.1 (7.0–9.5)* |
| Parent aware of VFC program | ||||||||
| Yes | 15,877 | 37.6 (36.7–38.5) | 6,192 | 36.6 (35.2–38.1) | 6,187 | 37.4 (36.1–38.7) | 3,498 | 41.3 (39.4–43.1)* |
| No | 25,547 | 62.4 (61.5–63.3) | 10,331 | 63.4 (61.9–64.8) | 10,343 | 62.6 (61.3–63.9) | 4,873 | 58.7 (56.9–60.6)* |
| Family income to poverty ratio | ||||||||
| <133% | 10,380 | 31.5 (30.6–32.4) | 4,988 | 38.9 (37.4–40.4) | 2,997 | 23.3 (22.1–24.5)* | 2,395 | 38.5 (36.7–40.4) |
| 133%–<322% | 11,256 | 27.9 (27.1–28.8) | 4,055 | 25.6 (24.3–26.9) | 4,219 | 28.0 (26.8–29.3)* | 2,982 | 35.5 (33.7–37.3)* |
| 322%–<503% | 8,281 | 17.4 (16.8–18.1) | 2,903 | 14.2 (13.3–15.1) | 3,782 | 20.9 (19.9–22.0)* | 1,596 | 14.8 (13.6–16.1) |
| >503% | 11,507 | 23.1 (22.4–23.9) | 4,577 | 21.4 (20.3–22.6) | 5,532 | 27.8 (26.7–29.0)* | 1,398 | 11.2 (10.1–12.3)* |
| Medical insurance† | ||||||||
| Private only | 24,016 | 51.4 (50.5–52.3) | 8,951 | 45.7 (44.2–47.2) | 10,804 | 59.0 (57.7–60.4)* | 4,261 | 41.0 (39.3–42.8)* |
| Any Medicaid | 12,707 | 37.3 (36.4–38.3) | 5,585 | 43.0 (41.4–44.5) | 3,998 | 29.9 (28.6–31.2)* | 3,124 | 47.2 (45.3–49.1)* |
| Other‡ | 3,181 | 7.0 (6.6–7.5) | 1,289 | 6.5 (6.0–7.2) | 1,235 | 7.4 (6.8–8.1)* | 657 | 7.1 (6.3–8.1) |
| Uninsured | 1,520 | 4.2 (3.9–4.6) | 698 | 4.8 (4.1–5.5) | 493 | 3.6 (3.1–4.2)* | 329 | 4.7 (3.9–5.6) |
| Well child visit at age 11–12 years¶ | ||||||||
| Yes | 20,223 | 47.0 (46.1–47.9) | 7,952 | 45.2 (43.8–46.7) | 8,969 | 51.0 (49.6–52.3)* | 3,302 | 37.6 (35.8–39.4)* |
| No | 9,518 | 22.2 (21.4–22.9) | 3,316 | 21.2 (20.0–22.4) | 3,147 | 19.3 (18.3–20.4)* | 3,055 | 36.2 (34.4–38.0)* |
| Don’t know | 11,683 | 30.8 (30.0–31.7) | 5,255 | 33.6 (32.1–35.0) | 4,414 | 29.7 (28.5–31.0)* | 2,014 | 26.3 (24.6–28.0)* |
| Parental report of provider recommendation for vaccine | ||||||||
| Yes | 28,639 | 73.4 (72.5–74.3) | 11,497 | 74.0 (72.5–75.4) | 11,764 | 74.2 (72.9–75.5) | 5,378 | 68.3 (66.4–70.1)* |
| No | 9,202 | 26.6 (25.7–27.5) | 3,497 | 26.0 (24.6–27.5) | 3,481 | 25.8 (24.5–27.1) | 2,224 | 31.7 (29.9–33.6)* |
| Vaccination facility type | ||||||||
| All private facilities | 20,483 | 52.8 (51.9–53.7) | 8,629 | 52.8 (51.3–54.3) | 9,730 | 59.4 (58.1–60.7)* | 2,124 | 27.6 (25.9–29.3)* |
| All public facilities | 6,048 | 15.4 (14.7–16.1) | 2,016 | 15.1 (14.0–16.3) | 1,537 | 11.4 (10.4–12.4)* | 2,495 | 31.7 (29.9–33.5)* |
| All hospital facilities | 4,911 | 10.0 (9.5–10.5) | 2,218 | 11.6 (10.7–12.5) | 1,698 | 8.8 (8.1–9.6)* | 995 | 9.3 (8.3–10.5)* |
| All STD/school/teen clinics or other facilities | 705 | 2.1 (1.8–2.5) | 319 | 2.1 (1.7–2.6) | 252 | 2.2 (1.7–2.8) | 134 | 1.9 (1.3–2.6) |
| Mixed** | 8,382 | 18.4 (17.8–19.1) | 2,915 | 17.0 (15.9–18.1) | 2,973 | 16.9 (15.9–17.9) | 2,494 | 29.0 (27.4–30.7)* |
| Other†† | 599 | 1.3 (1.1–1.4) | 294 | 1.4 (1.1–1.7) | 249 | 1.3 (1.1–1.6) | 56 | 0.6 (0.4–0.9)* |
Abbreviation: VFC = Vaccines for Children; STD = sexually transmitted disease.
*Statistically different compared with adolescents living in mostly urban areas (p < .05).
†Insurance categories are mutually exclusive.
‡Includes Indian Health Service, military, Children’s Health Insurance Program, and some private.
¶Status of health-care visit at age 11–12 years based on provider-reported data.
**Mixed indicates that the facility is identified to be in more than one of the facility categories, such as private, public, hospital, and STD/school/teen clinics.
††Includes military, WIC clinics, and pharmacies.
Demographic differences by MSA status
Sociodemographic and access-to-care characteristics varied significantly by MSA status. As shown in Table 1, the majority of teens living in suburban (58.4%) and mostly rural (68.2%) areas were non-Hispanic white compared to those living in mostly urban areas (41.0%). Compared to teens in mostly urban areas, those living in suburban areas had a higher proportion of mothers aged 45 years or older (51.1%), who were married (72.2%), and who had a graduate school education (44.5%). Teens living in mostly rural areas had a higher percentage of mothers aged 35–44 years (50.5%), who were previously married (27.3%), and with either a high school (29.0%) or some college (29.4%) education compared to those in mostly urban areas. There were similar proportions of families with an income-to-poverty ratio at the lowest level (<133%) in mostly urban (38.9%) and mostly rural (38.5%) areas. Fewer families in mostly rural areas (11.2%) had an income-to-poverty ratio at the highest level (>503%), compared to those in mostly urban areas (21.4%). Most families with an income-to-poverty ratio at the highest level lived in suburban areas (27.8%). The majority of suburban teens had private insurance (59.0%) while almost half of mostly rural teens had Medicaid (47.2%). More suburban teens had an 11–12-year-old well-child visit (51.0%) while fewer mostly rural teens (37.6%) had this visit compared to mostly urban (45.2%) teens. Fewer parents of teens living in mostly rural areas reported receiving a provider recommendation for HPV vaccine (68.3%) than their mostly urban counterparts (74.0%); there was no difference in provider recommendation of HPV vaccine for parents living in suburban (74.2%) compared to mostly urban areas (Table 1).
Factors associated with non-initiation of the HPV vaccine series in all MSA categories
A significantly higher percentage of suburban (39.2%) and mostly rural (45.4%) teens had not received any doses of HPV vaccine compared to mostly urban teens (32.0%) (Table 2). Several adolescent, parental, and access-to-care factors were associated with higher percentages of non-initiation of the HPV vaccine series in all three MSA categories in the unadjusted analysis, including sex (male), region of residence (Midwest and South), maternal education (>college graduate), maternal age (≥45 years), income-to-poverty ratio (≥133%), not having an 11–12-year-old well-child visit, and not receiving a provider recommendation for HPV vaccine (Table 2). After adjusting for all sociodemographic variables, factors associated with non-initiation of the HPV vaccine series in all MSAs included region of residence (South), maternal education (some college/college graduate), not having an 11–12-year-old well-child visit, and not receiving a provider recommendation for HPV vaccine (Table 3). Of note, although we primarily focused on factors associated with higher percentage of adolescents not initiating the HPV vaccine series, we did find that a significantly lower percentage of non-Hispanic black and Hispanic teens were unvaccinated compared to non-Hispanic white teens, both overall and in each MSA category (Table 2).
Table 2.
The proportion of adolescents aged 13–17 years not receiving HPV vaccine by MSA status for select sociodemographic and access-to-care characteristics – United States. National Immunization Survey – Teen, 2016–2017 (N = 41,424).
| Metropolitan Statistical Area (MSA) |
||||
|---|---|---|---|---|
| Overall |
Mostly urban |
Suburban |
Mostly rural |
|
| Characteristic | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) |
| Total | 37.0 (36.2–37.9) | 32.0 (30.6–33.3) | 39.2 (37.9–40.5)* | 45.4 (43.5–47.2)* |
| Survey Year | ||||
| 2016† | 39.6 (38.4–40.8) | 34.1 (32.1–36.0) | 41.5 (39.7–43.4) | 49.6 (47.0–52.2) |
| 2017 | 34.5 (33.3–35.7)‡ | 29.9 (28.1–31.8)‡ | 36.9 (35.2–38.7)*‡ | 40.7 (38.1–43.4)*‡ |
| Age (years) | ||||
| 13–15† | 38.8 (37.6–39.9) | 33.1 (31.4–34.9) | 41.7 (40.0–43.4) | 45.8 (43.4–48.2) |
| 16–17 | 34.4 (33.1–35.7)‡ | 30.2 (28.1–32.4)‡ | 35.3 (33.4–37.2)*‡ | 44.7 (41.8–47.7)* |
| Sex | ||||
| Female† | 33.2 (32.0–34.4) | 28.4 (26.5–30.3) | 35.1 (33.3–37.0) | 41.4 (38.8–44.1) |
| Male | 40.7 (39.5–41.9)¶ | 35.3 (33.4–37.2)¶ | 43.3 (41.5–45.0)*¶ | 49.1 (46.5–51.6)*¶ |
| Race/ethnicity | ||||
| Non-Hispanic white† | 42.7 (41.6–43.7) | 38.0 (36.2–39.9) | 43.7 (42.2–45.2)* | 48.4 (46.3–50.5)* |
| Non-Hispanic black | 32.1 (29.7–34.5)‡ | 31.9 (28.6–35.4)‡ | 30.8 (27.2–34.7)‡ | 38.2 (31.5–45.4)‡ |
| Hispanic | 27.8 (25.8–29.9)‡ | 23.7 (21.1–26.5)‡ | 31.0 (27.7–34.5)*‡ | 38.5 (32.9–44.5)*‡ |
| AI/AN | 38.7 (30.8–47.2) | 32.6 (21.0–46.8) | 50.8 (35.7–65.7) | 32.3 (21.8–45.1)‡ |
| Asian | 33.5 (29.2–38.0)‡ | 27.1 (22.0–32.9)‡ | 39.4 (32.7–46.5)* | 50.5 (27.6–73.1) |
| Other | 37.3 (33.9–40.8)‡ | 34.8 (29.7–40.4) | 38.0 (32.8–43.6) | 42.4 (34.7–50.5) |
| Immigration status | ||||
| U.S. born† | 37.5 (36.7–38.4) | 32.7 (31.3–34.1) | 39.4 (38.0–40.7) | 45.4 (43.5–47.3) |
| Foreign born | 29.6 (26.0–33.5)‡ | 25.1 (20.2–30.6)‡ | 35.4 (29.8–41.3)* | 41.2 (29.7–53.7)* |
| Region | ||||
| Northeast† | 31.2 (29.6–32.8) | 22.1 (19.7–24.8) | 35.0 (33.0–37.1)* | 37.0 (31.2–43.1)* |
| Midwest | 38.7 (37.3–40.2)¶ | 31.4 (29.2–33.7)¶ | 41.6 (39.3–44.0)*¶ | 46.8 (43.7–49.9)*¶ |
| South | 41.9 (40.6–43.1)¶ | 38.4 (36.4–40.4)¶ | 43.4 (41.6–45.3)*¶ | 46.8 (43.8–49.9)*¶ |
| West | 31.7 (29.4–34.1) | 28.2 (25.2–31.5)¶ | 34.0 (30.2–38.1)* | 42.8 (38.3–47.3)* |
| Maternal education | ||||
| <High school† | 26.8 (24.4–29.3) | 20.5 (17.4–24.1) | 30.4 (26.1–35.0)* | 41.0 (35.8–46.3)* |
| High school | 35.7 (33.9–37.6)¶ | 29.8 (26.9–32.8)¶ | 39.1 (36.1–42.1)*¶ | 42.1 (38.3–46.0)* |
| Some college/college graduate | 40.5 (38.8–42.3) ¶ | 36.5 (33.7–39.5) ¶ | 42.3 (39.7–45.0)*¶ | 44.9 (41.8–48.1)* |
| >College graduate | 39.0 (37.8–40.3) ¶ | 35.3 (33.3–37.4) ¶ | 39.8 (38.0–41.5)*¶ | 51.1 (47.9–54.3)* ¶ |
| Maternal age (years) | ||||
| ≤34† | 31.9 (29.1–34.8) | 27.6 (23.6–32.0) | 33.3 (28.7–38.2) | 42.6 (36.9–48.6)* |
| 35–44 | 37.1 (35.8–38.5)¶ | 31.4 (29.4–33.6) | 40.4 (38.4–42.5)*¶ | 42.8 (40.1–45.5)* |
| ≥45 | 37.9 (36.7–39.1)¶ | 33.4 (31.5–35.3)¶ | 39.1 (37.4–40.8)*¶ | 49.3 (46.4–52.2)*¶ |
| Parent aware of VFC program | ||||
| Yes† | 36.8 (35.5–38.2) | 31.4 (29.2–33.7) | 38.9 (36.8–41.1)* | 45.4 (42.7–48.3)* |
| No | 37.1 (36.1–38.2) | 32.3 (30.6–34.0) | 39.4 (37.8–41.0)* | 45.3 (42.8–47.8)* |
| Income to poverty ratio | ||||
| <133%† | 29.8 (28.3–31.4) | 25.0 (22.9–27.3) | 32.5 (29.9–35.3)* | 39.4 (36.4–42.6)* |
| 133%–<322% | 41.3 (39.7–43.0)¶ | 36.3 (33.7–39.0)¶ | 42.8 (40.2–45.4)*¶ | 48.9 (45.8–52.0)*¶ |
| 322%–<503% | 43.0 (41.0–44.9)¶ | 39.4 (36.3–42.7)¶ | 44.1 (41.4–46.9)*¶ | 47.8 (43.4–52.2)*¶ |
| >503% | 37.2 (35.5–38.9)¶ | 34.4 (31.6–37.3)¶ | 37.5 (35.3–39.8)* ¶ | 51.5 (46.3–56.6)*¶ |
| Medical insurance** | ||||
| Private only† | 40.9 (39.7–42.0) | 36.5 (34.7–38.4) | 41.7 (40.1–43.3)* | 52.2 (49.6–54.9)* |
| Any Medicaid | 30.3 (28.9–31.8)‡ | 25.5 (23.4–27.8)‡ | 32.8 (30.3–35.3)*‡ | 38.8 (36.0–41.6)*‡ |
| Other†† | 40.7 (37.9–43.7) | 39.6 (35.1–44.2) | 42.0 (37.6–46.6) | 39.1 (32.9–45.7) ¶ |
| Uninsured | 43.5 (39.1–48.0) | 35.4 (29.3–42.0) | 46.7 (39.5–54.0)* | 61.3 (52.2–69.6)* |
| 11–12 y.o. well-child visit‡‡ | ||||
| Yes† | 30.7 (29.6–31.8) | 25.9 (24.2–27.7) | 33.4 (31.8–35.1)* | 35.1 (32.3–38.0)* |
| No | 46.3 (44.4–48.2)¶ | 40.0 (37.0–43.1)¶ | 49.6 (46.5–52.8)*¶ | 51.9 (48.8–54.9)*¶ |
| Don’t know | 40.0 (38.4–41.7)¶ | 35.0 (32.5–37.6)¶ | 42.4 (40.0–44.9)*¶ | 51.1 (47.3–54.8)*¶ |
| Provider recommendation for HPV vaccine¶¶ | ||||
| Yes† | 27.8 (26.9–28.8) | 24.6 (23.2–26.2) | 29.4 (28.0–30.8)* | 32.8 (30.6–35.1)* |
| No | 59.7 (57.6–61.6)¶ | 50.2 (46.9–53.5)¶ | 64.9 (61.9–67.8)*¶ | 68.7 (65.2–72.1)*¶ |
| Vaccination facility type | ||||
| All private facilities† | 36.9 (35.7–38.1) | 32.3 (30.4–34.2) | 39.6 (38.0–41.2)* | 43.6 (40.1–47.1)* |
| All public facilities | 36.9 (34.7–39.2) | 31.4 (27.9–35.1) | 35.9 (31.8–40.2) | 46.9 (43.5–50.3)* |
| All hospital facilities | 32.9 (30.5–35.4)‡ | 28.0 (24.6–31.7)‡ | 34.9 (31.1–38.9)*‡ | 45.8 (39.8–51.9)* |
| All STD/school/teen clinics or other facilities | 38.3 (31.1–45.9) | 38.2 (27.3–50.5) | 33.6 (24.0–44.7) | 59.1 (42.6–73.7)* |
| Mixed*** | 37.4 (35.5–39.3) | 30.4 (27.5–33.6) | 40.8 (37.7–44.0)* | 43.2 (39.9–46.5)* |
| Other††† | 52.4 (45.3–59.4)¶ | 48.3 (38.2–58.6)¶ | 54.8 (44.2–65.0)¶ | 63.1 (42.2–80.0)* |
Abbreviations: AI/AN = American Indian/Alaskan Native; CI = confidence interval; HPV = human papillomavirus; STD = sexually transmitted disease; y.o. = years old. VFC = Vaccines for Children.
*Statistically different compared with adolescents living in mostly urban areas (p < .05).
†Reference level for characteristic.
‡Statistically significantly lower (p < .05) compared to the reference level for characteristic.
¶Statistically significantly higher (p < .05) compared to the reference level for characteristic.
**Insurance categories are mutually exclusive.
††Includes Indian Health Service, military, Children’s Health Insurance Program, and some private.
‡‡Status of health-care visit at age 11–12 years based on provider-reported data.
¶¶By parental report.
***Mixed indicates that the facility is identified to be in more than one of the facility categories, such as private, public, hospital, and sexually transmitted disease/school/teen clinics.
†††Includes military, Special Supplemental Nutrition Program for Women, Infants and Children (WIC) clinics, and pharmacies.
Table 3.
Factors associated with not receiving HPV vaccine by MSA status – National Immunization Survey–Teen, United States, 2016–2017, N = 41, 424.
| Characteristic | Overall |
Metropolitan Statistical Area (MSA) |
||
|---|---|---|---|---|
| Mostly urban |
Suburban |
Mostly rural |
||
| aPR % (95% CI) | aPR % (95% CI) | aPR % (95%CI) | aPR % (95% CI) | |
|
Metropolitan Statistical Area (MSA) Mostly urban* Suburban Mostly rural |
Ref. 1.11 (1.06–1.18)† 1.18 (1.10–1.26)† |
|||
|
Age (years) 13–15* 16–17 |
Ref. 0.92 (0.87–0.97)† |
Ref. 0.94 (0.84–1.04) |
Ref. 0.90 (0.83–0.97)† |
Ref. 0.94 (0.85–1.03) |
|
Sex Female* Male |
Ref. 1.08 (1.03–1.13)† |
Ref. 1.09 (1.00–1.19) |
Ref. 1.08 (1.02–1.16)† |
Ref. 1.06 (0.98–1.15) |
|
Race/ethnicity Non-Hispanic white* Non-Hispanic black Hispanic AI/AN Asian Other |
Ref. 0.85 (0.78–0.92)† 0.75 (0.69–0.81)† 1.02 (0.80–1.28) 0.78 (0.67–0.90)† 0.93 (0.83–1.03) |
Ref. 0.94 (0.83–1.07) 0.72 (0.63–0.83)† 0.85 (0.55–1.33) 0.67 (0.51–0.87)† 0.93 (0.76–1.13) |
Ref. 0.75 (0.66–0.86)† 0.77 (0.68–0.87)† 1.25 (0.89–1.76) 0.87 (0.73–1.04) 0.93 (0.80–1.07) |
Ref. 0.79 (0.64–0.98)† 0.77 (0.65–0.91)† 0.89 (0.64–1.22) 0.66 (0.40–1.10) 0.95 (0.80–1.14) |
|
Region Northeast* Midwest South West |
Ref. 1.10 (1.03–1.17)† 1.22 (1.15–1.30) † 1.01 (0.93–1.10) |
Ref. 1.26 (1.09–1.45)† 1.55 (1.35–1.78)† 1.26 (1.07–1.49)† |
Ref. 1.05 (0.97–1.14) 1.11 (1.03–1.20)† 0.91 (0.80–1.02) |
Ref. 1.20 (1.02–1.41)† 1.32 (1.12–1.56)† 1.19 (1.00–1.42)† |
|
Maternal education <High school* High school Some college/college graduate >College graduate |
Ref. 1.21 (1.07–1.37)† 1.35 (1.20–1.53)† 1.29 (1.14–1.46)† |
Ref. 1.28 (1.03–1.58)† 1.40 (1.13–1.74)† 1.33 (1.07–1.66)† |
Ref. 1.16 (0.97–1.38) 1.30 (1.08–1.56)† 1.19 (0.99–1.43) |
Ref. 1.17 (0.96–1.43) 1.29 (1.07–1.56)† 1.42 (1.17–1.73)† |
|
Maternal marital status Married* Widowed/divorced/separated Never married |
Ref. 0.93 (0.87–0.99)† 0.86 (0.77–0.97)† |
Ref. 0.91 (0.81–1.03) 0.91 (0.76–1.08) |
Ref. 0.94 (0.86–1.03) 0.77 (0.62–0.94)† |
Ref. 0.92 (0.83–1.02) 0.88 (0.73–1.06) |
|
Maternal age (years) ≤34* 35–44 ≥45 |
Ref. 1.14 (1.03–1.26)† 1.14 (1.02–1.26)† |
Ref. 1.18 (0.99–1.40) 1.19 (0.99–1.42) |
Ref. 1.20 (1.01–1.42)† 1.17 (0.98–1.40) |
Ref. 0.93 (0.80–1.07) 0.98 (0.84–1.14) |
|
Income to poverty ratio <133%* 133%–<322% 322%–<503% >503% |
Ref. 1.14 (1.05–1.24)† 1.11 (1.01–1.22)† 1.01 (0.92–1.12) |
Ref. 1.15 (1.01–1.32)† 1.14 (0.96–1.35) 1.03 (0.86–1.24) |
Ref. 1.16 (1.02–1.31)† 1.13 (0.98–1.30) 1.01 (0.88–1.16) |
Ref. 1.07 (0.95–1.20) 0.98 (0.84–1.13) 1.04 (0.88–1.24) |
|
Medical insurance‡ Private only* Any Medicaid Other¶ Uninsured |
Ref. 0.84 (0.78–0.91)† 0.99 (0.90–1.08) 1.02 (0.89–1.16) |
Ref. 0.86 (0.74–0.99)† 1.08 (0.92–1.26) 0.94 (0.74–1.19) |
Ref. 0.83 (0.74–0.94)† 0.99 (0.87–1.13) 1.04 (0.86–1.25) |
Ref. 0.88 (0.78–0.99)† 0.86 (0.71–1.02) 1.09 (0.88–1.36) |
|
11–12 y.o. well-child visit** Yes* No Don’t know |
Ref. 1.39 (1.30–1.48)† 1.31 (1.24–1.39)† |
Ref. 1.47 (1.30–1.66)† 1.40 (1.25–1.56)† |
Ref. 1.35 (1.24–1.48)† 1.24 (1.15–1.34)† |
Ref. 1.33 (1.20–1.48)† 1.33 (1.19–1.48)† |
|
Provider recommendation for HPV vaccine†† Yes* No |
Ref. 2.10 (2.00–2.20)† |
Ref. 2.06 (1.89–2.25)† |
Ref. 2.16 (2.02–2.30)† |
Ref. 1.99 (1.82–2.16)† |
|
Vaccination facility type All private facilities* All public facilities All hospital facilities All STD/school/teen clinics or other facilities Mixed‡‡ Other¶¶ |
Ref. 0.94 (0.86–1.02) 0.91 (0.83–0.98)† 0.97 (0.80–1.19) 0.88 (0.81–0.94)† 1.14 (0.96–1.35) |
Ref. 0.96 (0.83–1.12) 0.89 (0.77–1.03) 1.03 (0.80–1.32) 0.76 (0.66–0.88)† 0.8 0.89 (0.64–1.22) |
Ref. 0.89 (0.77–1.02) 0.88 (0.79–0.99)† 0.84 (0.58–1.20) 0.95 (0.86–1.05) 1.25 (1.00–1.57) |
Ref. 1.00 (0.89–1.12) 1.02 (0.88–1.17) 1.44 (1.12–1.85)† 0.96 (0.85–1.08) 1.42 (1.04–1.94) |
Abbreviations: aPR = adjusted prevalence ratio; CI = confidence interval; HPV = human papillomavirus; STD = sexually transmitted disease; y.o. = year old.
*Reference level.
†p < .05 by t-test compared with reference group.
‡Insurance categories are mutually exclusive.
¶Includes Indian Health Service, military, Children’s Health Insurance Program, and some private.
**Status of health-care visit at age 11–12 years based on provider-reported data.
††By parental report.
‡‡Mixed indicates that the facility is identified to be in more than one of the facility categories such as private, public, hospital, STD/school/teen clinics.
¶¶Includes military, Special Supplemental Nutrition Program for Women, Infants and Children (WIC) clinics, and pharmacies.
Factors associated with non-initiation of the HPV vaccine series in specific MSA categories
Some factors were associated with non-initiation of the HPV vaccine series in only certain MSA categories in the unadjusted analysis. As shown in Table 2, in mostly urban areas, region of residence (West) was associated with non-initiation of the vaccine series. In suburban areas, maternal age ≥35 years was associated with non-initiation of the vaccine series. In mostly urban and suburban areas, associated factors for not initiating vaccination included maternal education (high school, some college/college graduate) and receiving vaccines in “other” vaccination facility types. Of note, although receiving vaccines from “other” vaccination facility types was an associated access-to-care factor in mostly urban and suburban areas, the 95% confidence interval (CI) was wide and thus the estimate may not be reliable. The unadjusted analysis did not identify additional factors associated with non-initiation of HPV vaccination in mostly rural areas that were different from the associated factors previously identified in all MSA categories.
After adjusting for all sociodemographic factors, the likelihood of not initiating the HPV vaccine series was higher among teens in suburban (adjusted prevalence ratio [aPR] 1.11; 95% CI 1.06–1.18) and mostly rural (aPR 1.18; 95% CI 1.10–1.26) areas compared to teens in mostly urban areas (Table 3). We identified other factors positively associated with non-initiation of the HPV vaccine series in only certain MSAs in the adjusted analysis. For mostly urban areas, residing in the Midwest (aPR 1.26, 95% CI 1.09–1.45) or the West (aPR 1.26, 95% CI 1.07–1.49); maternal high school education (aPR 1.28; 95% CI 1.03–1.58) or >college graduate (aPR 1.33; 95% CI 1.07–1.66); and income-to-poverty ratio of 133%–<322% (aPR 1.15; 95% CI 1.01–1.32) were associated factors. In suburban areas, male sex (aPR 1.08; 95% CI 1.02–1.16), maternal age 35–44 years (aPR 1.20; 95% CI 1.01–1.42), and income-to-poverty ratio of 133%–<322% (aPR 1.16; 95% CI 1.02–1.31) were associated with non-initiation of HPV vaccine (Table 3). In mostly rural areas, residing in the Midwest (aPR 1.20; 95% CI 1.02–1.41) or the West (aPR 1.19; 95% CI 1.00–1.42), maternal education >college graduate (aPR 1.42; 95% CI 1.17–1.73), and receiving vaccines at STD/school/teen clinics or other facilities (aPR 1.44, 95% CI 1.12–1.85) were associated with non-initiation of HPV vaccine (Table 3).
Missed opportunities for HPV vaccination among teens by MSA status
Overall, 37.0% of teens in the combined 2016 and 2017 survey sample had not initiated the HPV vaccine series. Among this unvaccinated (for HPV vaccine) sample, a significantly higher percentage of suburban (82.2%) vs. mostly urban (79.3%) teens had missed opportunities for HPV vaccination (Table 4). However, there was no difference in the percentage of mostly rural teens (78.9%) with missed opportunities for HPV vaccination when compared to mostly urban teens (Table 4). Taking the entire 2016 and 2017 survey sample into account, if these unvaccinated adolescents had initiated the HPV vaccination series during health-care visits when they received another vaccine, coverage for ≥1 dose of HPV vaccine could have been 93.4% among mostly urban teens, 93.0% among suburban teens, and 90.4% among teens in mostly rural areas (Figure 1).
Table 4.
Adolescents aged 13–17 years unvaccinated for HPV vaccine with missed opportunities* for initiation of the HPV vaccine series by MSA status – National Immunization Survey–Teen, United States, 2016–2017, n = 15,387.
| Missed Opportunities for ≥1 HPV Vaccine |
||
|---|---|---|
| n | % (95% CI) | |
| Total U.S. Overall | 15,387 | 80.7 (79.5–81.8) |
| MSA status | ||
| Mostly-urban | 5,311 | 79.3 (77.3–81.3) |
| Suburban | 6,455 | 82.2 (80.4–83.8)† |
| Mostly-rural | 3,621 | 78.9 (76.7–81.0) |
Abbreviations: HPV = human papillomavirus; MSA = metropolitan statistical area
*A missed opportunity for girls was defined as a health-care encounter occurring on or after her 11th birthday and before her 13th birthday, and on or after March 23, 2007, during which time she received at least one vaccination, but not the first dose of the HPV vaccine series; a missed opportunity for boys was defined as a health-care encounter occurring on or after his 11th birthday and before his 13th birthday, and on or after December 23, 2011, during which time he received at least one vaccination, but not the first dose of the HPV vaccine series.
†Statistically different compared with adolescents in mostly urban areas (p < .05).
Figure 1.
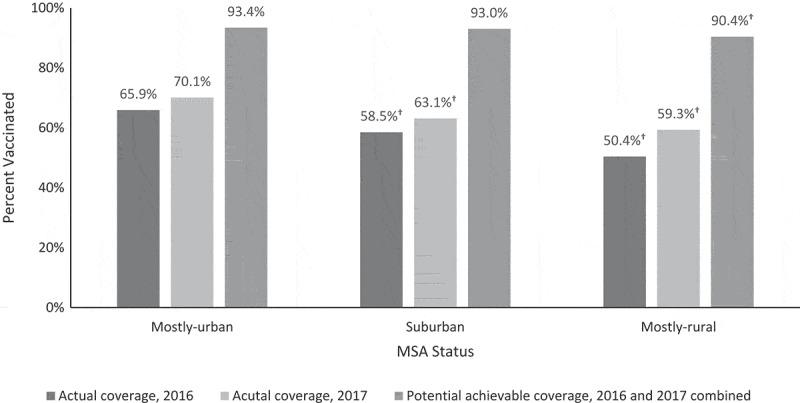
Actual and potentially achievable vaccination coverage with ≥1 dose of human papillomavirus (HPV) vaccine if missed opportunities* for vaccination had been eliminated among teens by age 13 years, – National Immunization Survey-Teen, United States, 2016–2017, N = 41,424.
Discussion
Teens from both suburban and mostly rural areas were less likely to get HPV vaccine than those in mostly urban areas. However, most factors associated with not initiating the HPV vaccine were similar across all three MSAs, and similar to those reported in other studies examining sociodemographic factors associated with HPV vaccination in general.4,19,20,30 These associated factors include living in the South, having a mother with some college education, not having an 11–12-year-old well-child visit, and not receiving a provider recommendation for HPV vaccination.
Some associated factors were unique to specific MSAs such as male sex and maternal age of 35–44 years in suburban areas, and receiving vaccines from STD/school/teen clinics or other facilities in mostly rural areas. Although males (50.4%) and mothers aged 35–44 years (41.7%) represent large proportions of the suburban sample, the proportion of mostly rural teens visiting STD/school/teen clinics or other facilities for vaccines was quite small (1.9%). As the majority of mostly rural teens did not rely on these sites for vaccinations, this factor likely does not account for the disparity in HPV vaccination coverage in mostly rural MSAs. Thus additional factors, perhaps those not collected by the NIS-Teen, may be driving the disparity in mostly rural areas.
Prior studies have evaluated sociodemographic factors associated with HPV vaccination with differing results. Though two studies found no association between sociodemographic factors and HPV vaccine initiation,31,32 several studies did. A systematic review by Kessels et al. identified race/ethnicity, insurance status, well-child visits, and provider recommendation as factors associated with HPV vaccination among adolescent girls.19 One study among adolescent girls in rural-frontier U.S. states found that non-Hispanic white race/ethnicity, older parental age (>35 years), higher parental educational attainment, living above the federal poverty threshold, having private insurance, and visiting private vaccination facilities were associated with non-initiation of the HPV vaccine series.20 Results from an additional study found that non-Hispanic white parents of higher socioeconomic status were less likely to accept HPV vaccine for their children.33 Another analysis identified not having a well-child visit and lack of provider recommendation as factors associated with non-initiation.30
Teens in mostly rural areas were less likely to initiate HPV vaccination compared to those in mostly urban areas. These teens were less likely to have had an 11–12-year-old well-child visit, suggesting that access to care may contribute to the disparity. By not attending this preventive visit, the likelihood of receiving a provider recommendation for HPV vaccine may be reduced. Additionally, providers in rural areas may be less comfortable discussing HPV vaccine recommendations, as our study found parents in mostly rural areas were less likely to report receiving a provider recommendation for HPV vaccine than parents in mostly urban MSAs. Furthermore, a relative shortage of pediatricians has been observed in rural areas,34 and non-pediatrician providers may be less familiar with vaccine recommendations for adolescents.35
As previously mentioned, we defined missed opportunities as health-care encounters during which an adolescent received at least one other vaccine but did not initiate the HPV vaccine series. Based on this definition, teens in suburban areas were more likely to miss opportunities for HPV vaccination than those in mostly urban MSAs. This may not be surprising since suburban teens were also more likely to have had an 11–12-year-old well-child visit, which is when Tdap and MenACWY vaccines are recommended. Although this finding was statistically significant and may be contributing to the disparity in HPV vaccination coverage in suburban areas to some degree, the absolute difference in missed opportunities among adolescents in suburban and mostly urban areas was small and may not be programmatically significant. Still, these results differ from other studies, which found that use of preventive services by adolescents was associated with fewer missed opportunities.13,36 However, results from our study are not directly comparable to those from these other studies based on differences in how missed opportunities were defined. In addition, these other studies did not look at missed opportunities by MSA status, which may also account for the difference. More importantly, we show what coverage for ≥1 dose of HPV vaccine would be if these missed opportunities had not occurred. Although it would still be lower among adolescents in mostly rural areas, coverage in all three MSAs would be substantially higher and comparable to coverage rates for other routinely recommended adolescent vaccines.
There is still so much to learn about the factors underlying differences in HPV vaccination coverage by MSA status. The more we learn about what is driving these disparities, the more informed public health professionals will be when developing interventions to address them. Based on the results of this analysis, similar interventions would be beneficial across geographic areas and might include targeting efforts to boost HPV vaccine uptake in the South and continuing to stress the importance of a strong provider recommendation. Several studies support the influence of a high-quality provider recommendation on HPV vaccine acceptance.26-28 Recent data highlight the components of a high-quality provider recommendation, which include taking an announcement approach rather than a more conversational tone with parents.37 Equipping providers with the tools they need to make strong recommendations and to address parents’ questions and concerns is a priority, since providers are often the primary source of information about HPV vaccine for families. Since the data show that these parents are less likely to accept HPV vaccine for their teen(s), it may be beneficial to develop promotional messages that resonate with parents with higher levels of education, which may also include parents with higher levels of health literacy. Similar to another analysis,33 our study also suggests that there may be room to customize interventions by MSA status. For example, in suburban areas, we might consider ways we could reach older mothers, especially those of higher socioeconomic status. This demographic group may seek out sources other than pediatricians for health-related information.21 We might also consider innovative ways to frame conversations about HPV vaccine around males since our data show that males are less likely to be vaccinated in suburban areas. Interventions addressing missed opportunities may be more appropriate in suburban areas, while those addressing access to care might be more effective in mostly rural areas. Teens in mostly rural areas are more likely to visit non-traditional vaccination facility types for immunizations than those in other MSAs. Thus, ensuring health-care professionals other than pediatricians is familiar with adolescent vaccine recommendations and comfortable making strong recommendations are also important in mostly rural areas. Finally, our data show that teens in mostly rural areas are more likely to receive vaccines from public facilities compared to those in mostly urban areas. With this in mind, implementing strategies in public facilities, particularly at the local level, may be the key to closing the gap in HPV vaccination coverage rates between these two MSAs. Although the literature is scarce regarding viable solutions for suburban communities, possible solutions for improving HPV vaccine uptake in rural areas have been suggested. Authors from one study conducted in the largely rural state of Alabama concluded that a multimodal approach encompassing activities aimed at improving parental education about HPV vaccine, communication between providers and parents, as well as school-based approaches might be effective.38 An additional analysis on barriers to HPV vaccination in rural Alabama asked unvaccinated teens and their parents for strategies they believed would improve acceptance of HPV vaccine in their communities. Both teens and their caregivers indicated that more information about the vaccine would be helpful.39 Another analysis conducted in South Carolina, another state with a large rural population, had similar findings.40
This analysis is subject to several previously reported limitations.4,5 In addition to these, we based MSA status on household county of residence, which is not as granular as other approaches, including rural-urban commuting area (RUCA) codes, which are based on population density, urbanization, and daily commuting patterns. As a result, non-MSAs (mostly rural areas) may include urban populations not located within an MSA as well as completely rural areas. Conversely, MSA-principal cities (mostly urban areas) may include some rural populations. Also, although NIS-Teen collects data on provider type (e.g., Pediatrics, Family Practice, Obstetrics/Gynecology, etc.), this information is incomplete for the unvaccinated population by geographic area. As a result, we were unable to examine the effect of provider type on HPV vaccination rates by MSA status, which would be beneficial when planning interventions. Another limitation is how provider recommendation for HPV vaccine was ascertained. This variable is based on parental report and thus subject to recall bias. In addition, the outcome of interest for this analysis was “not receiving HPV vaccine”. Understandably, choosing this as the outcome variable rather than vaccination coverage may limit comparability with other analyses. However, our goal was to increase our understanding of the unvaccinated population for this vaccine. Additionally, factors other than the ones assessed in this analysis may be driving disparities in coverage, particularly in rural areas. Prior studies have cited factors such as religiosity and fatalistic beliefs about cancer prevention behaviors as potential barriers to HPV vaccine uptake in rural areas and these concepts may be difficult to assess via a survey.14,41,42 In addition, since this study analyzed national-level data, it may be difficult to identify associations at the local level. Finally, because this is a cross-sectional analysis, we are unable to infer causality based on the associations we identified.
Improving HPV vaccination rates among adolescents is a public health priority. However, it will be difficult to improve rates without a better understanding of what is driving the disparity in coverage by geographic area; identifying factors associated with these differences is an initial step toward this end. Future studies will enable public health authorities to advocate for effective interventions to address these disparities.
Acknowledgments
We thank all NIS–Teen participants and the following persons with funding or employment by the Centers for Disease Control and Prevention: Tara Vogt, PhD, MPH; James Singleton PhD; Lauri Markowitz MD; and Mary Ann Kirkconnell Hall, MPH.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Robinson CL, Romero JR, Kempe A, Pellegrini C, Szilagyi P.. Advisory committee on immunization practices recommended immunization schedule for children and adolescents aged 18 years or younger - United States, 2018. MMWR Morb Mortal Wkly Rep. 2018;67(5):156–57. doi: 10.15585/mmwr.mm6705e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Merck Sharp & Dohme Corp . Package insert -Gardasil 9-. Whitehouse Station (NJ): MERCK & CO., INC.; 2006–2018.
- 3.Centers for Disease Control and Prevention . Cancers Associated with Human Papillomavirus, United States—2011–2015 USCS Data Brief, No. 4. Atlanta (GA): Centers for Disease Control and Prevention; 2018.
- 4.Walker TY, Elam-Evans LD, Yankey D, Markowitz LE, Williams CL, Mbaeyi SA, Fredua B, Stokley S. National, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 years - United States, 2017. MMWR Morb Mortal Wkly Rep. 2018;67(33):909–17. doi: 10.15585/mmwr.mm6733a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walker TY, Elam-Evans LD, Singleton JA, Yankey D, Markowitz LE, Fredua B, Williams CL, Meyer SA, Stokley S. National, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 years - United States, 2016. MMWR Morb Mortal Wkly Rep. 2017;66(33):874–82. doi: 10.15585/mmwr.mm6633a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zahnd WE, James AS, Jenkins WD, Izadi SR, Fogleman AJ, Steward DE, Colditz GA, Brard L. Rural-urban differences in cancer incidence and trends in the United States. Cancer Epidemiol Biomarkers Prev. 2017;27(11):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yu L, Sabatino SA, White MC. Rural-urban and racial/ethnic disparities in invasive cervical cancer incidence in the United States, 2010-2014. Prev Chronic Dis. 2019;16:E70. doi: 10.5888/pcd16.180447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Curtis CR, Dorell C, Yankey D, Jeyarajah J, Chesson H, Saraiya M, Gold R, Dunne EF, Stokley S. National human papillomavirus vaccination coverage among adolescents aged 13-17 years-National Immunization Survey–Teen, United States, 2011. MMWR Suppl. 2014;63:61–70. [PubMed] [Google Scholar]
- 9.Henry KA, Stroup AM, Warner EL, Kepka D. Geographic factors and human papillomavirus (HPV) vaccination initiation among adolescent girls in the United States. Cancer Epidemiol Biomarkers Prev. 2016;25(2):309–17. doi: 10.1158/1055-9965.EPI-15-0658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Henry KA, Swiecki-Sikora AL, Stroup AM, Warner EL, Kepka D. Area-based socioeconomic factors and human papillomavirus (HPV) vaccination among teen boys in the United States. BMC Public Health. 2017;18(1):19. doi: 10.1186/s12889-017-4567-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moss JL, Gilkey MB, Rimer BK, Brewer NT. Disparities in collaborative patient-provider communication about human papillomavirus (HPV) vaccination. Hum Vaccin Immunother. 2016;12(6):1476–83. doi: 10.1080/21645515.2015.1128601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mohammed KA, Subramaniam DS, Geneus CJ, Henderson ER, Dean CA, Subramaniam DP, Burroughs TE. Rural-urban differences in human papillomavirus knowledge and awareness among US adults. Prev Med. 2018;109:39–43. doi: 10.1016/j.ypmed.2018.01.016. [DOI] [PubMed] [Google Scholar]
- 13.Wong CA, Taylor JA, Wright JA, Opel DJ, Katzenellenbogen RA. Missed opportunities for adolescent vaccination, 2006-2011. J Adolesc Health. 2013;53(4):492–97. doi: 10.1016/j.jadohealth.2013.05.009. [DOI] [PubMed] [Google Scholar]
- 14.Vanderpool RC, Dressler EV, Stradtman LR, Crosby RA. Fatalistic beliefs and completion of the HPV vaccination series among a sample of young Appalachian Kentucky women. J Rural Health. 2015;31(2):199–205. doi: 10.1111/jrh.12102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vanderpool RC, Huang B, Deng Y, Bear TM, Chen Q, Johnson MF, Paskett ED, Robertson LB, Young GS, Iachan R. Cancer-related beliefs and perceptions in Appalachia: findings from 3 states. J Rural Health. 2019;35(2):176–88. doi: 10.1111/jrh.12359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention . About the National Immunization Surveys (NIS). Atlanta (GA): Centers for Disease Control and Prevention; 2018.
- 17.Jain N, Singleton JA, Montgomery M, Skalland B. Determining accurate vaccination coverage rates for adolescents: the National Immunization Survey-Teen 2006. Public Health Rep. 2009;124(5):642–51. doi: 10.1177/003335490912400506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention . NIS-Teen Data and Documentation for 2015 to Present. Atlanta (GA): Centers for Disease Control and Prevention; 2018.
- 19.Kessels SJ, Marshall HS, Watson M, Braunack-Mayer AJ, Reuzel R, Tooher RL. Factors associated with HPV vaccine uptake in teenage girls: a systematic review. Vaccine. 2012;30(24):3546–56. doi: 10.1016/j.vaccine.2012.03.063. [DOI] [PubMed] [Google Scholar]
- 20.Lai D, Ding Q, Bodson J, Warner EL, Kepka D. Factors associated with increased HPV vaccine use in rural-frontier U.S. states. Public Health Nurs. 2016;33(4):283–94. doi: 10.1111/phn.12223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Loke AY, Kwan ML, Wong YT, Wong AKY. The uptake of human papillomavirus vaccination and its associated factors among adolescents: a systematic review. J Prim Care Community Health. 2017;8(4):349–62. doi: 10.1177/2150131917742299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Radisic G, Chapman J, Flight I, Wilson C. Factors associated with parents’ attitudes to the HPV vaccination of their adolescent sons: a systematic review. Prev Med. 2017;95:26–37. doi: 10.1016/j.ypmed.2016.11.019. [DOI] [PubMed] [Google Scholar]
- 23.Mohammed KA, Vivian E, Loux TM, Arnold LD. Factors associated with parents’ intent to vaccinate adolescents for human papillomavirus: findings from the 2014 National Immunization Survey-Teen. Prev Chronic Dis. 2017;14:E45. doi: 10.5888/pcd14.160314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention . Vaccines for Children Program (VFC). Atlanta (GA): Centers for Disease Control and Prevention; 2018.
- 25.United States Census Bureau . Current Population Survey Subject Definitions. United States Census Bureau; 2015. https://www.census.gov/programs-surveys/cps/technical-documentation/subject-definitions.html
- 26.Gilkey MB, Calo WA, Moss JL, Shah PD, Marciniak MW, Brewer NT. Provider communication and HPV vaccination: the impact of recommendation quality. Vaccine. 2016;34(9):1187–92. doi: 10.1016/j.vaccine.2016.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Landis K, Bednarczyk RA, Gaydos LM. Correlates of HPV vaccine initiation and provider recommendation among male adolescents, 2014 NIS-Teen. Vaccine. 2018;36(24):3498–504. doi: 10.1016/j.vaccine.2018.04.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ylitalo KR, Lee H, Mehta NK. Health care provider recommendation, human papillomavirus vaccination, and race/ethnicity in the US National Immunization Survey. Am J Public Health. 2013;103(1):164–69. doi: 10.2105/AJPH.2011.300600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stokley S, Jeyarajah J, Yankey D, Cano M, Gee J, Roark J, Curtis RC, Markowitz L. Human papillomavirus vaccination coverage among adolescents, 2007-2013, and postlicensure vaccine safety monitoring, 2006-2014–United States. MMWR Morb Mortal Wkly Rep. 2014;63:620–24. [PMC free article] [PubMed] [Google Scholar]
- 30.Dorell CG, Yankey D, Santibanez TA, Markowitz LE. Human papillomavirus vaccination series initiation and completion, 2008-2009. Pediatrics. 2011;128(5):830–39. doi: 10.1542/peds.2011-0950. [DOI] [PubMed] [Google Scholar]
- 31.Monnat SM, Rhubart DC, Wallington SF. Differences in human papillomavirus vaccination among adolescent girls in metropolitan versus non-metropolitan areas: considering the moderating roles of maternal socioeconomic status and health care access. Matern Child Health J. 2016;20(2):315–25. doi: 10.1007/s10995-015-1831-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kester LM, Zimet GD, Fortenberry JD, Kahn JA, Shew ML. A national study of HPV vaccination of adolescent girls: rates, predictors, and reasons for non-vaccination. Matern Child Health J. 2013;17(5):879–85. doi: 10.1007/s10995-012-1066-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Warner EL, Ding Q, Pappas LM, Henry K, Kepka D. White, affluent, educated parents are least likely to choose HPV vaccination for their children: a cross-sectional study of the National Immunization Study - Teen. BMC Pediatr. 2017;17(1):200. doi: 10.1186/s12887-017-0969-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shipman SA, Lan J, Chang CH, Goodman DC. Geographic maldistribution of primary care for children. Pediatrics. 2011;127(1):19–27. doi: 10.1542/peds.2010-0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Esposito S, Principi N, Cornaglia G; Group EVS . Barriers to the vaccination of children and adolescents and possible solutions. Clin Microbiol Infect. 2014;20(Suppl 5):25–31. doi: 10.1111/1469-0691.12447. [DOI] [PubMed] [Google Scholar]
- 36.Lee GM, Lorick SA, Pfoh E, Kleinman K, Fishbein D. Adolescent immunizations: missed opportunities for prevention. Pediatrics. 2008;122(4):711–17. doi: 10.1542/peds.2007-2857. [DOI] [PubMed] [Google Scholar]
- 37.Brewer NT, Hall ME, Malo TL, Gilkey MB, Quinn B, Lathren C. Announcements versus conversations to improve HPV vaccination coverage: a randomized trial. Pediatrics. 2017;139:1. doi: 10.1542/peds.2016-1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dilley SE, Peral S, Straughn JM Jr., Scarinci IC. The challenge of HPV vaccination uptake and opportunities for solutions: lessons learned from Alabama. Prev Med. 2018;113:124–31. doi: 10.1016/j.ypmed.2018.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Boyd ED, Phillips JM, Schoenberger YM, Simpson T. Barriers and facilitators to HPV vaccination among rural Alabama adolescents and their caregivers. Vaccine. 2018;36(28):4126–33. doi: 10.1016/j.vaccine.2018.04.085. [DOI] [PubMed] [Google Scholar]
- 40.Cartmell KB, Young-Pierce J, McGue S, Alberg AJ, Luque JS, Zubizarreta M, Brandt HM. Barriers, facilitators, and potential strategies for increasing HPV vaccination: a statewide assessment to inform action. Papillomavirus Res. 2018;5:21–31. doi: 10.1016/j.pvr.2017.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Thomas T, Blumling A, Delaney A. The influence of religiosity and spirituality on rural parents’ health decision making and human papillomavirus vaccine choices. ANS Adv Nurs Sci. 2015;38(4):E1–E12. doi: 10.1097/ANS.0000000000000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thomas TL, Strickland OL, DiClemente R, Higgins M, Haber M. Rural African American parents’ knowledge and decisions about human papillomavirus vaccination. J Nurs Scholarsh. 2012;44(4):358–67. doi: 10.1111/j.1547-5069.2012.01479.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


