Abstract
Activated CD4 T cells are a major target of HIV infection. Results from the Step HIV vaccine trial highlighted a potential role for total activated CD4 T cells in promoting HIV acquisition. However, the influence of vaccine insert-specific CD4 T cell responses on HIV acquisition is not known. Here, using the data obtained from four macaque studies, we show that the DNA prime/modified vaccinia Ankara boost vaccine induced IFNγ+ CD4 T cells (Th1 cells) which rapidly migrate to multiple tissues including colon, cervix, and vaginal mucosa. These mucosal Th1 cells persisted at higher frequencies and expressed higher density of CCR5, a viral coreceptor, compared to cells in blood. Following intravaginal or intrarectal SIV/SHIV challenges, strong vaccine protection was evident only in animals that had lower frequencies of vaccine-specific Th1 cells but not in animals that had higher frequencies of Th1 cells, despite comparable vaccine-induced humoral and CD8 T cell immunity in both groups. An RNA transcriptome signature in blood at 7 days after priming immunization from one study was associated with induction of fewer Th1-type CD4 cells and enhanced protection. These results demonstrate that high and persisting frequencies of HIV vaccine-induced Th1-biased CD4 T cells in the intestinal and genital mucosa can mitigate beneficial effects of protective antibodies and CD8 T cells, highlighting a critical role of priming immunization and vaccine adjuvants in modulating HIV vaccine efficacy.
One sentence summary
Vaccine-induced IFNγ+ CD4 T cells migrate to and persist in mucosal tissue and negatively associate with protection against SIV
INTRODUCTION
There is a great need for the development of an effective prophylactic vaccine to control the HIV/AIDS epidemic worldwide (1, 2). The RV144 HIV vaccine trial, using a poxvirus vector prime and envelope protein boost modality, demonstrated a modest but encouraging 31.2% efficacy and established proof of concept that a vaccine can contribute to reduced acquisition of HIV-1 (3). The RV144 results also spurred renewed interest in HIV vaccines that use heterologous prime/boost vaccination approaches comprised of viral vectors and proteins. However, the unanticipated and concerning results from the Step trial, that tested the immunogenicity and efficacy of human adenovirus type 5 (Ad5) vector expressing HIV Gag, Pol and Nef, revealed enhanced risk of HIV acquisition among vaccinated individuals that were Ad5 seropositive and uncircumcised. These results alerted the field to the importance of activated CD4 T cells in modulating vaccine protection (4, 5).
Considerable efforts have been made to understand the mechanisms that contributed to enhanced risk of HIV acquisition in the Step trial using samples from trial participants (4–6) as well as modeling the Step trial using the penile SIV infection route in rhesus macaques (7). These studies showed that Ad5 vaccination induces CD4 T cells expressing the gut homing receptor α4β7 in blood (8), which is associated with a concomitant increase in the frequency of activated CD4 T cells, including Ad5-specific CD4 T cells (9). Together, these studies suggest a role for vaccine-induced CD4 T cells in enhancing the acquisition of HIV or SIV infection. Furthermore, another study that compared the ability of different viral vectors and DNA to induce activated CD4 T cells in rhesus macaques demonstrated an association between the presence of higher frequencies of activated CD4 T cells in the rectum of vaccinated animals and enhanced acquisition of SIVmac239 infection (10). Similarly, vaccination with varicella zoster vaccine (VZV) expressing SIV envelope gp120 that primarily induced CD4 T cell responses resulted in markedly higher SIV replication compared to unvaccinated controls (11). These studies suggest that total activated CD4 T cells following vaccination can also play a role in enhancing acquisition of HIV or SIV infection in settings where vaccination did not induce protective antibody responses.
Two critical findings of the RV144 trial are that vaccine-induced antibody responses are key correlates for reduced risk of HIV acquisition and vaccine efficacy appeared to have waned after a year following vaccination. These findings highlight the need to develop HIV vaccines that induce high magnitude, durable protective antibody responses. One strategy to achieve this goal is to induce strong CD4 T helper responses that include follicular helper CD4 T cells (Tfh). However, previous studies demonstrated that HIV-specific CD4 T cells are preferentially infected compared to non-HIV-specific memory CD4 T cells (12, 13). In addition, Tfh cells support active virus replication during chronic SIV and HIV infections (14–16), and these cells can be readily infected in vitro (17). These findings, combined with the potential for activated CD4 T cells to enhance acquisition, raise the possibility that high frequencies of vaccine-induced HIV-specific CD4 T cells may diminish protective efficacy by serving as targets during the early stages of infection/virus replication in the mucosa (reviewed by (6, 18)). Thus, it is important to understand the relationship between vaccine-induced HIV/SIV-specific CD4 T cell responses and vaccine efficacy in a model where there is evidence for vaccine protection. In this study, we utilized samples obtained from four DNA/MVA-based SIV vaccine studies in rhesus macaques (Table 1) to perform a comprehensive analysis of vaccine-induced CD4 T cell responses in blood and mucosal tissue, and to determine their effects on vaccine-mediated protection.
Table 1.
Details of vaccines and vaccinations discussed in the manuscript
| Study name | Vaccination regimen (schedule in weeks) | Vaccine inserts | Age range (Years) | Week of challenge initiation | Challenge virus used | Max No of challenges | Route & dose of challenge |
|---|---|---|---|---|---|---|---|
| M14 (n=10) | D-40L D-40L MM (0,8,16,24) | SIVmac239 Gag, Prt, RT and Env, CD40L with DNA | 3 to 6 | 48 | SIVmac251 | 8 | Intra Rectal, 6.47×10^2 TCID50 |
| P165 (n=33) | DDMM or D-GM D-GM MM (0,8,16,32) | SIVmac239 Gag, Prt, RT and Env; and GM-CSF with DNA in some animals | 3 to 17 | 57 | SIVsmE660-ABL (SIVsmE660 Hirsch 2000) | 12 | Intra Rectal, 4.12×10^2 TCID50 |
| M15 (17) | DDMM or D-GM D-GM MM (0,8,16,24) | SIVmac239 Gag, Prt, RT and Env; and GM-CSF with DNA in some animals | 3 to 19 | 48 | SIVsmE660-ABL (SIVsmE660 Hirsch 2000) | 12 | Intra Vaginal, 10.2×10^3 TCID50 |
| M19 (15) | DDMMM (0,8,16,24,38) | SIVmac239 Gag, Prt, RT and HIV 1086c Env | 4 to 15 | 58 | SHIV1157 ipd3N4 | 8 | Intra Vaginal, 4.5×10^5 TCID50 |
D, DNA (3mg/dose, intramuscular); D-GM, DNA co-expressing macaque GM-CSF (3mg/dose, intramuscular); M, MVA (1×108 pfu/dose, intramuscular).
RESULTS
Design of macaque studies trials
We utilized samples from macaque studies M14 (19), M15, M19, and P165 (20) (Table 1). These were selected to study protection against intrarectal (M14 and P165) or intravaginal (M15 and M19) infections and against SIV (M14, M15 and P165) or SHIV (M19) challenges. Some of the immunogenicity and protection results for M14 and P165 were published previously except for the influence of vaccine-induced CD4 T cells on protection (Fig. 2) and the data presented in figures 3 and 5 of this manuscript. The immunogenicity and protection data for M15 and M19 studies have not been reported previously. The details for each study are listed in Table 1. All studies used DNA prime/MVA boost vaccines expressing either SIVmac239 immunogens (20) or SHIV1086c immunogens (20).
Figure 2. Higher frequencies of vaccine-induced IFNγ+ CD4 T cell responses are associated with diminished vaccine efficacy.
(A) Kaplan-Meier curve illustrating the rate of SHIV1157ipd3N4 infection following intravaginal repeat dose challenge in the M19 study and (B) scatter plot showing the distribution of total SIV (Env + Gag)-specific CD4 T cell responses and Kaplan-Meier curves show the rate of infection stratified by the median frequency of total SIV-specific CD4 T cell responses (low vs. high) at one week after the 1st MVA boost (peak of vaccine response), (C, D) similar analyses for the P165 study with intrarectal infection and (E,F) the M14 study with intrarectal infection. Vac, Vaccinated animals; Cont, Control animals; I.Vag, Intravaginal; IR, Intrarectal; Low IFNγ, below the median; High IFNγ, above the median. P values in this figure were calculated using the Log-rank (Mantle-Cox) test.
Figure 3. Vaccine-elicited CCR5+ IFNγ+ MIP-1β-CD4 T cells but not GC-Tfh are associated inversely with protection.
(A) Co-expression of CCR5, IFNγ, IL-2, MIP-1β and TNFα by SIV-specific CD4 T cells at one week after the 1st MVA boost in the M14 study. (B) Correlation between acquisition of SIV infection and CCR5+ IFNγ+ MIP-1β-or CCR5+ IFNγ+ MIP-1β+ SIV-specific CD4 T cells at one week after the 1st MVA boost in M14 study. (C, D) Representative flow cytometry staining and correlation between the number of challenges to infection and the frequency of Env1-specific IFNγ+ CD4 T cells expressing (C) CCR5 or (D) CCR7 in the P165 study. (E) Representative flow cytometry staining and correlation between the number of challenges to infection and the frequency of germinal center resident T follicular helper cells (GC-Tfh) measured in a peripheral lymph node at 2 weeks after the 2nd MVA immunization in the P165 study. (F) Correlation between frequencies of Env1-specific IFNγ+ CD4 T cells in blood at one week after the 1st MVA immunization and GC-Tfh at 2 weeks after the 2nd MVA immunization. P values in this figure were calculated using the Pearson correlation test.
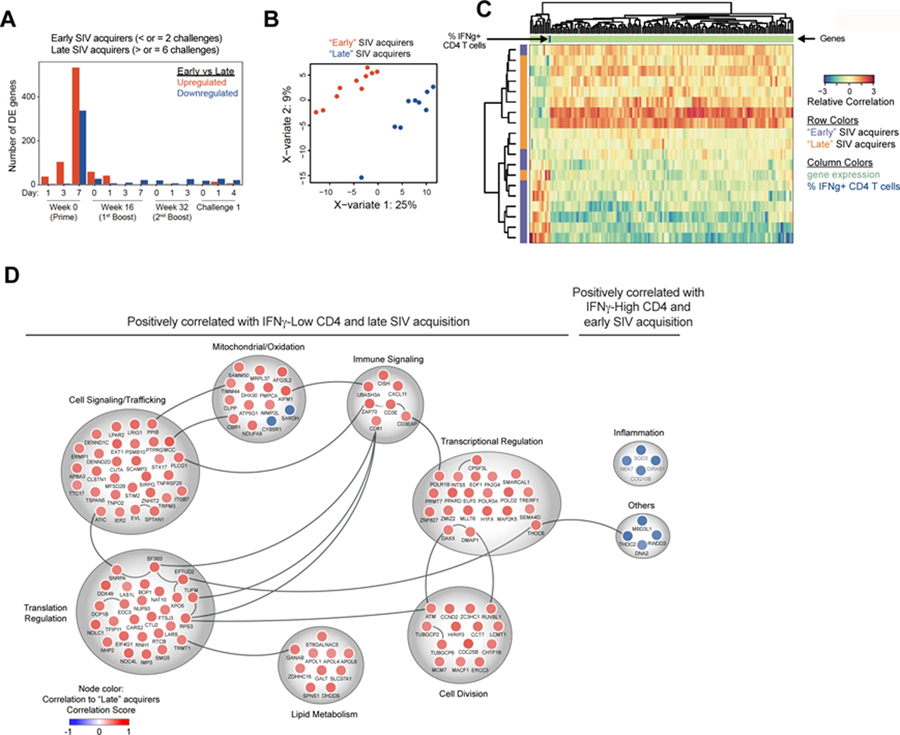
Figure 5. Global gene expression signature at 7 days post vaccination in blood is associated with the induction of low Th1-biased CD4 T cell response and strong vaccine protection.
(A) Bar graphs showing the number of genes which differentially up-or down-regulated in “early” (≤ 2 challenged) versus “late” (≥ 6 challenges or uninfected) SIV acquirers in P165 study. Differential expression analysis was based on animals from the two outcomes grouped together as sample ‘replicates’ at each time point. The cutoff criteria was defined as a 1.5 fold change (up or down), with a Benjamini-Hochberg adjusted (multiple-testing correction) p-value < 0.05. (B) Supervised sPLS-Discriminant Analysis, sPLS-DA showing the clustering of early and late SIV acquirers with each dot representing a single animal. (C) Clustered Image Matrix of block sPLS-DA that accounts for both % IFNγ+ CD4 T cell responses and SIV acquisition outcome. Each cell is colored in shades of red or blue, indicating the relative correlation score of an animal’s phenotypic output to the outcome variable. Each row represents one animal, and the SIV acquisition state of that animal is depicted by the purple (‘early’) or orange (‘late’) alongside each row. Each column represents one phenotypic measurement, with gene expression labeled in light green. The column representing % IFNγ+ CD4 T cells is labeled in dark blue on the top of the column. (D) Functional classification of genes identified in Fig.5c. Genes correlating positively or negatively with % IFNγ+ CD4 T cells and SIV acquisition outcome were grouped based on function and assessed for protein-protein interactions using Ingenuity IPA. Node color represents the correlation to late SIV acquisition (blue = negative correlation, red = positive correlation).
Vaccine-elicited IFNγ+ CCR5+ CD4 T cells persist at higher frequencies in the colon and genital mucosa compared to blood
To understand the anatomic distribution of DNA/MVA vaccine-induced T cell responses in blood and tissues, we performed a comprehensive analysis of vaccine-specific CD4 and CD8 T cells following vaccination in blood and multiple lymphoid and mucosal tissue in the M15 and M19 studies (Fig. 1). Consistent with our previous studies (19, 21), DNA/MVA vaccinations induced high frequencies of Gag-and Env-specific IFNγ-producing CD4 and CD8 T cells in blood (Fig. 1A; fig. S1). The SIV-specific CD4 responses peaked after the 1st MVA boost whereas the CD8 T cell responses peaked after the subsequent MVA boosts. The CD4 and CD8 T cell responses were equally targeted to both Gag and Env (fig. S1A–D). The vaccine-induced CD4 T cells also expressed other cytokines such as TNFα, IL-2, IL-21, and IL-4 (fig. S2 A, B). Cytokine co-expression analyses using the Boolean function revealed the majority of cytokine+ cells co-express IFNγ, including the IL-4+ cells, demonstrating the Th1 dominance of the vaccine-induced CD4 T cell response (fig. S2 C, D).
Figure 1. Vaccine-elicited CCR5+ CD4 T cells persist at higher frequencies in the colon and genital mucosa compared to blood.
(A) Temporal IFNγ+ CD4 and CD8 T cells in blood of M15 study animals. (B, C) SIV-specific IFNγ+ CD4 and CD8 T cells in multiple tissues at 20 weeks after the 2nd MVA boost (memory) in the M15 study. (D) Comparison of memory IFNγ+ CD4 and CD8 T cell responses in M15 study. (E) Temporal IFNγ+ CD4 and CD8 T cells in blood of M19 study animals. (F) SHIV-specific IFNγ+ CD4 T cells in multiple tissues at peak (week 1) and memory (20 weeks) after the 3rd MVA boost in the M19 study. (G) CCR5 expression on Gag and Env1-specific IFNγ+ CD4 T cells in systemic and mucosal tissues at peak and prechallenge in the M19 study. (H) Association between ENV1-or Gag-specific IFNγ+ CD4 T cells in blood at peak (Wk1 post-MVA 1) and tissues at the memory time point in the M15 (n=7) and M19 (n=3) studies. *, p<0.05 (compared to blood except in D where the comparison is with CD8 in the same tissue). P values in (B), (D), (F) and (G) were calculated using paired t test and in (H) with spearman rank correlation test.
It is important to understand the distribution and persistence of vaccine-induced CD4 T cells at the portal of virus entry, and how these cells influence protection. In the M15 study, we had the opportunity to measure, in a parallel group of vaccinated animals that were euthanized, the frequency of vaccine-induced IFNγ-producing CD4 T cells in multiple tissues including the gut and regions of the female reproductive tract (FRT) at about 20 weeks after the final MVA (memory phase, close to the day of challenge)(Fig. 1B). The vaccine-induced CD4 T cells migrated to multiple tissue including the colon, cervix, and vagina. Interestingly, the migration was highest to cervix and lowest to LNs among the tissue tested. Remarkably, although the IFNγ+ CD4 T cell response in the blood was very low or below detection limit (0.01%), these cells were maintained at significantly higher frequencies in cervix (p=0.02) and vagina (p=0.03) compared to blood. A similar distribution was also observed for SIV Env, SIV Gag and total SIV-specific CD4 T cells (fig. S3 A–C). However, the frequency of total proliferating CD4 T cells (fig. S3D) and total CD4 T cells (fig. S3E) was not significantly different between different compartments. In contrast, a different pattern was observed for vaccine-induced IFNγ+ CD8 T cells (Fig. 1C). Although the frequencies of IFNγ+ CD8 T cells were comparable between blood and multiple tissues such as spleen and colon, they were significantly lower in cervix and vagina (p=0.02)(Fig. 1D). These results demonstrated that DNA/MVA vaccine-induced IFNγ+ CD4 T cells but not CD8 T cells persist at high frequencies in genital mucosa.
To understand if the vaccine-induced IFNγ+ CD4 T cells have the potential to be infected by SIV or HIV, we determined CCR5 expression on these cells from the M19 study animals (Fig. 1 E–G). Similar to the M15 study, we observed strong migration of vaccine-induced IFNγ+ CD4 T cells to genital mucosa during effector (1 week after the 3rd MVA boost) and memory (close to the day of challenge) phases (Fig. 1F). During the effector phase, about 50% of the IFNγ+ CD4 T cells in the blood co-expressed CCR5 and nearly the entirety of IFNγ+ CD4 T cells (80–100%) in the genital tissue co-expressed CCR5. During the memory phase, the co-expression on cells in blood decreased to about 35% whereas the cells in the genital mucosa retained the high frequency co-expression. The proportion of CCR5+ cells within SIV-specific CD4 T cells was also significantly greater compared to total CD4 T cells in each tissue (Fig. S3f). Impressively, vaccine-induced IFNγ-producing CD4 T cells in blood after the 1st MVA boost (peak) showed a strong direct correlation with the frequency of vaccine-induced CD4 T cells in colon, cervix, and vagina during the memory phase (pre-challenge)(Fig. 1H). Collectively, these results demonstrate that DNA/MVA vaccination induces IFNγ+ CD4 T cells that migrate to the colon and genital mucosae, the majority of them express CCR5, and persist at high frequencies in these tissues compared to blood at 20 weeks after the final immunization. These results suggest that mucosal tissue-resident SIV-specific CD4 T cells have the potential to facilitate SIV acquisition.
Higher frequencies of vaccine-induced IFNγ+ CD4 T cell responses are associated with diminished vaccine efficacy following intravaginal and intrarectal challenges
At 22–24 weeks following the final immunization, M19 study animals were subjected to weekly intravaginal SHIV1157ipd3N4 challenges (8 maximum) to determine vaccine efficacy. As can be seen in Fig. 2A, we did not observe a delay in acquisition of SHIV infection in vaccinated animals compared to unvaccinated animals. To understand the influence of vaccine-induced IFNγ+ CD4 T cell response, we stratified vaccinated animals into two groups (IFNγ-Low and IFNγ-High) based on the median frequencies of SHIV-specific IFNγ producing CD4 T cells at the peak of the vaccine response (week 1 after the 1st MVA boost) (Fig. 2B). We discovered a marked difference for acquisition of infection in vaccinated animals. Animals that had lower frequencies of IFNγ+ CD4 T cells (below the median; IFNγ-Low) showed a significant delay in acquisition of SHIV infection (p=0.03 vs unvaccinated controls) whereas animals that induced higher frequencies of IFNγ+ CD4 T cells (above the median; IFNγ-High) showed no evidence for vaccine protection (p=0.4). These results demonstrate an association between higher frequencies of vaccine-induced IFNγ+ CD4 T cells and diminished DNA/MVA vaccine-mediated protection against heterologous intravaginal SHIV challenge.
Similar to the M19 study, animals in the M15 study were subjected to weekly intravaginal SIVsmE660 challenges (12 maximum) to determine vaccine efficacy. As we and others reported previously for intrarectal challenges (20, 22–25), the protection against intravaginal SIVsmE660 was significantly influenced by the TRIM5α genotype, and was mainly observed in TRIM5α restrictive animals but not in permissive animals (fig. S4 A–C). In addition, the group sizes were too small to be able determine the influence of vaccine-induced IFNγ+ CD4 T cell response on vaccine efficacy.
We next investigated if the same associations were true in our P165 (20) and M14 (19) studies in which animals were vaccinated with DNA/MVA SIV239 vaccine and challenged intrarectally with either SIVsmE660 (P165) or SIVmac251 (M14). For the P165 study analysis, we used only TRIM5α permissive animals to avoid the influence of restrictive TRIM5α on protection. In addition, we considered only Env1 peptide pool specific CD4 T cells since we do not have data for Gag-and Env2 peptide pool-specific CD4 T cells due to sample limitation. In both studies, we observed a significant delay in acquisition of intrarectal SIV infection in the vaccinated animals (p=0.01) (Fig. 2C–F). However, consistent with results from the M19 study, we also observed markedly enhanced protection in animals that had lower frequencies of vaccine-elicited IFNγ+ CD4 T cells when compared to those with higher frequencies of these cells or unvaccinated controls (p<0.01)(Fig. 2D, 2F). Again, there was no evidence of vaccine-mediated protection in animals with high frequencies of IFNγ+ CD4 T cells. Collectively, these data demonstrated that high frequencies of vaccine-elicited SIV-specific IFNγ+ CD4 T cells are associated with diminished efficacy of DNA/MVA vaccines against neutralization-sensitive and -resistant mucosal SIV/SHIV challenges in 3 rhesus macaque studies, regardless of whether the animals are challenged intrarectally or intravaginally.
Next, we calculated if there is a threshold value of IFNγ+ CD4 T cell response that statistically distinguished the rate of infection acquisition between IFNγ-Low and IFNγ-High animals. For this analysis we combined data from M14 and M19 studies that were performed in the same laboratory and divided animals into IFNγ-Low and IFNγ-High groups and analyzed rate of acquisition. This analysis identified 1.32% as the cut-off value (fig. S4D). Impressively, this value was very close to the cut-off we used to define IFNγ-Low and IFNγ-High groups in M19 (1.39%) and M14 (1.37%) studies individually (Fig. 2). However, given that the sensitivity of intracellular cytokine staining assays can vary significantly between the labs, this cut-off should not be regarded as an absolute value. We did not include P165 data for combined analyses because these were generated in a different laboratory and in addition we did not have data for Gag from all animals. Similarly, we did not include data from M15 since the protection in this study was influenced heavily by TRIM5α.
Vaccine-elicited CCR5+ IFNγ+ MIP-1β-CD4 T cells but not GC-Tfh are associated inversely with protection
We next investigated the co-expression of IFNγ, CCR5, IL-2, MIP-1β, and TNFα by vaccine-induced CD4 T cells and their association with acquisition of SIV infection in the M14 study (Fig. 3 A, B). We included MIP-1β since it can bind to CCR5 and potentially block HIV or SIV infection. The majority of IL-2, MIP-1β, and TNFα positive cells also expressed IFNγ+, and about half of the cytokine+ cells co-expressed CCR5. Interestingly, the CCR5+ IFNγ+ MIP-1β-cells but not CCR5+ IFNγ+ MIP-1β+ cells showed an inverse association with acquisition of infection (Fig. 3B).
Similarly, we determined associations between the expression of CCR5 and CCR7 (lymph node homing potential) and acquisition of infection in the P165 study (Fig. 3 C, D). We observed a significant inverse correlation between the CCR5+ IFNγ+ CD4 T cells and the number of challenges required for infection (p=0.02)(Fig. 3C). We also observed a significant inverse association between CCR7-IFNγ+ Env1-specific CD4 T cells and number of challenges to infection (p=0.04)(Fig. 3D), suggesting that effector CD4 T cells that lack homing potential to lymph nodes (LNs) could contribute to diminished vaccine efficacy, possibly by homing to tissues. This CCR5+ cell phenotype likely reflects the in vivo phenotype of the CD4 T cells, as opposed to being induced by the cell stimulation procedure, since in a previous study (26), we found that expression of CCR5 by antigen-stimulated sorted cells did not change significantly following 6hrs of in vitro stimulation.
Vaccine-induced Tfh responses in LNs are likely to be key for the induction of high titer and high quality antibody responses. We recently demonstrated that circulating CXCR5+ CD4 T cells induced by DNA/MVA vaccination predict the frequency of LN-resident germinal center (GC) Tfh cells and the persistence of antibody responses (27). Here, we investigated whether high frequencies of vaccine-induced Tfh cells could also contribute to diminished vaccine efficacy. We determined the frequency of GC Tfh cells in the LN at 2 weeks after the 2nd MVA boost (peak of the antibody response) and analyzed whether these frequencies correlate with the number of challenges to SIVsmE660 infection in the P165 study. Interestingly, the GC-Tfh cell frequencies in LNs were directly correlated with the number of challenges to infection (Fig. 3E). CXCR3 is a Th1 cell-associated chemokine receptor, and a previous study showed a direct association between CXCR3-Tfh and induction of broadly neutralizing antibodies in HIV-1 infected humans (28). In addition, we have shown that CXCR3+ but not CXCR3-Tfh express CCR5 (27). We therefore probed the association between CXCR3-GC-Tfh and acquisition of infection, and observed a direct correlation between the number of challenges with the frequency of CXCR3-GC-Tfh but not with CXCR3+ GC-Tfh (Fig. 3E). In addition, the frequency of Env-specific IFNγ+ CD4 T cells at 1 week after the first MVA immunization was inversely correlated with the frequency of GC-Tfh at 2 weeks after the second MVA immunization (Fig. 3F). Thus, these results collectively demonstrate that circulating SIV-specific Th1-biased CD4 T cells, but not LN-resident GC-Tfh cells, are associated with diminished vaccine efficacy. These observations suggest that a stronger Th1 response early in immunization may negatively affect the Tfh response in LNs.
Vaccine-specific antibody and CD8 T cell responses correlate with protection but only in animals that induced lower peak IFNγ+ CD4 T cell responses
In our prior DNA/MVA vaccine studies, the non-neutralizing effector functions of vaccine-elicited antibodies showed a direct correlation with protection (20, 29). Here, we investigated the association between multiple parameters of humoral immunity, the magnitude of vaccine-induced CD8 T cell response, and protection in animals that had low or high frequencies of IFNγ+ CD4 T cells at the peak of vaccine response (Fig. 4, and fig. S5). Specifically, for antibody responses, we measured the binding antibody to purified gp140 and gp160 (derived by solubilizing VLPs and capturing on conA (30, 31)), avidity index against gp160, neutralizing activity against the challenge virus, antibody dependent cellular cytotoxicity (ADCC) and antibody dependent cellular phagocytosis (ADCP) activities. Since we did not perform all of these measurements for all four studies, we performed correlation analyses where available. In general, we did not observe any neutralizing activity against the challenge virus except in P165 study (20).
Figure 4. Vaccine-specific antibody responses correlate with protection in animals with lower peak IFNγ+ CD4 T cell responses.
(A) Correlation between the number of challenges to infection and prechallenge Env-specific IgG in serum, peak Env-specific avidity and peak SHIV-specific CD8 T cells in the M19 study. (B) Correlation between the number of challenges to infection and prechallenge Env-specific IgG in rectal secretions in the P165 study. In each row, the panels on the far left show antibody responses in animals with low (below median) and high (above median) frequencies of vaccine-specific IFNγ+ CD4 T cells at week 1 after the 1st MVA boost. On some graphs fewer dots are visible than indicated due to an overlap for data between some animals. P values in this figure were calculated using the Pearson correlation test.
In the M19 study, we observed a strong direct association between protection and the titer of gp160 IgG in serum at prechallenge (Fig. 4A) and peak (fig. S5A), avidity against gp160 (Fig. 4A), and the magnitude of peak SHIV-specific IFNγ+ CD8 T cell response (Fig. 4A) but only in IFNγ-Low group animals. These associations were lost in IFNγ-High group animals despite having comparable humoral and CD8 T cell responses. Similarly, in the P165 study, the delay in acquisition of SIVsmE660 infection was directly associated with the titer of pre-challenge binding antibodies in rectal secretions (Fig. 4B) but only in IFNγ-Low group but not IFNγ-High group animals. Although vaccination induced measurable neutralizing antibody responses against the challenge virus, we did not find any significant association between titers of neutralizing antibodies and the delay in acquisition of infection (20). In conclusion, the data show that the antibody and CD8 T cell responses contribute to protection and strongly suggest that high frequencies of HIV vaccine-induced Th1-biased CD4 T cells can mitigate the beneficial effects of protective antibody and CD8 T cell responses.
Global gene expression signature in blood at 7 days post-vaccination identifies the induction of Th1-biased CD4 T cell response and vaccine protection
Next, we investigated gene expression signatures in blood to determine whether any were associated with the induction of Th1-biased CD4 T cell responses and enhanced vaccine protection. Using samples from the P165 study, we selected 10 vaccinated animals that acquired SIV infection within the first 2 challenges (early SIV acquirers) and 12 vaccinated animals that acquired SIV infection after 6 challenges (late SIV acquirers). We performed a microarray analysis on whole blood samples from both groups of animals at multiple days after the 1st DNA vaccination (Wk0), 1st MVA boost (Wk16), 2nd MVA boost (Wk32) and 1st intrarectal challenge (Wk57) (Fig. 5). When we compared the RNA expression, we observed a large number of genes that were either up-regulated or down-regulated compared to samples taken at Week 0 in both groups (Fig. 5A). Remarkably, the only time point at which there was a large number of differentially expressed genes between early and late SIV acquirers was 7 days after the 1st DNA vaccination. At this time point, 532 genes were increased in expression and 337 genes decreased in expression in early SIV acquirers compared to late SIV acquirers (Fig. 5A). Thus, our further analyses were performed using gene expression data from 7 days after the first DNA immunization.
Sparse Partial Least Squares Discriminant Analysis (sPLS-DA) is a supervised machine learning method that projects multiple variables onto the same geometric space to allow for correlations across multiple measurements within an experimental design, and it incorporates lasso penalization to identify the parameters contributing most highly to each component (32). sPLS-DA (supervised for protection outcome) of differentially expressed genes at Day 7 post DNA vaccination identified two clusters that clearly segregated animals into early and late SIV acquirers, potentially identifying gene signatures that are associated with protection status (Fig. 5B). Traditionally, the number of components run for analysis is chosen as k – 1, where k is the number of possible outcomes. As the possible outcomes in our experiment included “early” or “late” SIV acquirers, a single component for sPLS-DA would typically be used. However, for this exploratory analysis, we examined the first 2 components such that we could plot potential separation of outcomes within clusters. Parameter tuning determined that 150 and 100 genes should be selected from each of the first two components during sPLS-DA, providing a total of 250 genes to classify the animals into the clusters visualized in Fig. 5B. The largest separation between the clusters was seen along the first component; therefore we used this component to determine correlations with CD4 frequencies. These results clearly demonstrated that a gene signature as early as Day 7 post 1st DNA vaccination could separate the transcriptional profiles between favorable and unfavorable vaccine responses against SIVsmE660 infection in rhesus macaques.
We next performed a multivariate analysis that considered both protection outcome and the frequency of IFNγ+ ENV1-specific CD4 T cell response using block sPLS-DA (mixDIABLO) (Fig. 5C). Parameter tuning from the first component of sPLS-DA had identified 150 genes that were optimal for selection along this variate, and we used this parameter as the input for a one-component block sPLS-DA of gene expression and IFNγ+ CD4 frequencies against SIV infection outcome. In this analysis, the phenotypes were divided into 2 main branches based on correlation to early or late SIV acquisition, and these branches are labeled by those conditions where the phenotypes (particularly gene expression) are positively correlated. The cyan group (left) is positively correlated with early SIV acquisition and negatively correlated with late SIV acquisition. The genes in this group are positively correlated with % IFNγ+ CD4 T cells. The genes in the yellow cluster (right) are positively correlated with late SIV acquisition and negatively correlated with early SIV acquisition. This analysis identified a set of 139 genes that positively correlated with low IFNγ+ CD4 T cell responses and late SIV acquisition or negatively correlated with high IFNγ+ CD4 responses and early SIV acquisition. Similarly, a smaller set of 12 genes negatively correlated with low IFNγ+ CD4 T cell response and late SIV acquisition and positively correlated with high IFNγ+ CD4 and early SIV acquisition. The transcripts positively correlated with low IFNγ+ CD4 T cell response and late SIV acquisition represented a number of genes associated with cell proliferation, survival, apoptosis, transcription, translation, T cell activation, cell differentiation, and multiple intracellular processes especially those related to mitochondria (Fig. 5 C, D: Table S1). Importantly, network analysis showed that most of these genes cluster, indicating a high level of cooperation towards these functions. The negatively correlated genes represented genes associated with inflammation. In particular, higher NEK7 suggests a linkage to NLRP3 inflammasome activation and production of IL-18 and IL-1β (33). Higher SOD3 expression suggests greater inflammation, and has been shown to suppress Th2 and Th17 but not Th1 responses (34). DIRAS1 belongs to a distinct branch of the functionally diverse Ras superfamily of monomeric GTPases and controls the hyper-activation of GTPases. The increased RNA of DNA2 that is important for DNA replication and DNA repair also suggest a proinflammatory condition. RWDD3 is an enhancer of SUMO conjugation of proteins and enhances inhibition of NF-kB activation by stabilizing NF-kB inhibitor alpha. Collectively, these results reveal that strong induction of transcripts associated with cell proliferation and T cell activation, occurring in the setting of lower inflammation as early as Day 7 following DNA vaccination, associates with induction of lower Th1-biased CD4 T cell responses and better overall protection.
DISCUSSION
In this study, we investigated the role of vaccine-induced IFNγ+ CD4 T cell responses in modulating the protection afforded by DNA/MVA vaccines against pathogenic SIV/SHIVs, and against both intrarectal and intravaginal challenges. Our results demonstrated that higher frequencies of vaccine-induced Th1-biased CD4 T cell responses can mitigate the protective functions of vaccine-induced humoral and CD8 T cell responses and abrogate vaccine protection if frequencies exceed a threshold of about 1.4% in blood at one week post the 1st MVA boost under our assay conditions. Importantly, by further dissecting the phenotype of vaccine-induced CD4 T cells, our results indicate a strong role for Th1-biased CD4 T cells that express the viral co-receptor CCR5 in diminishing vaccine efficacy. In addition, our results show that during long-term memory, vaccine-induced IFNγ+ CD4 T cells are enriched in mucosal tissues compared to blood, and the majority of these cells express CCR5, and their frequencies in mucosal tissue correlate with Th1-biased CD4 T cell responses in blood at the peak of response (1 week after the 1st MVA boost). Remarkably, our results identify a strong association between a specific gene expression signature in blood, lower frequencies of Th1-biased CD4 T cells, and better protection outcome as early as 7 days after the first DNA prime. Collectively, these results argue that high frequencies of vaccine-induced Th1-biased CCR5+ CD4 T cells in mucosal tissues can override the beneficial effects of vaccination against SIV, and this phenotype seems to be established within days after the first immunization.
It is important to note that our results do not imply that vaccine-induced IFNγ+ CD4 T cell help is bad; rather they highlight that if frequencies exceed a certain threshold then they could counteract other protective functions. For example, the reduced risk of HIV infection acquisition in RV144 human HIV vaccine study was associated with stronger IFNγ+ CD4 T cell response (35). Similarly, in our recent macaque study, we observed a direct correlation between vaccine-induced IFNγ+ CD4 T cells and protection (36). However, in these instances, the vaccine-induced CD4 T cells are at least 10-fold lower than the threshold value that we defined in the study.
A remarkable finding of our study is that a specific gene expression signature in blood at 7 days after the first DNA immunization was associated with lower Th1-biased CD4 responses and delayed SIV acquisition. It was somewhat surprising to observe this level of change in gene expression in blood at this time point because a single DNA immunization does not induce detectable cellular and humoral responses in rhesus macaques. These data strongly suggest that the initial DNA prime sets the course for the protective phenotype. Importantly, the gene expression signature suggested that multiple immune pathways contribute to protection or delayed acquisition including pathways that are required for inducing a potent immune response, such as immune signaling, cell division, transcriptional and translational activation. However, the gene expression signature also indicated that induction of a lower pro-inflammatory response was important, suggesting that a stronger immune activation/proliferation in the presence of low inflammation promotes a lower Th1-biased CD4 T cell response and stronger Tfh response. This shift towards lower Th1 and stronger Tfh response could be beneficial to vaccination because of fewer potential target cells and greater help to B cells for induction of functional antibody responses.
There are some limitations to our study. A more complete understanding of how the mucosal tissue resident vaccine-induced Th1-biased CD4 T cells influence mucosal SIV acquisition will require further investigation. Our working hypothesis is that these vaccine-induced CD4 T cells serve as preferential targets early after virus exposure due to their high CCR5 expression and rapidly amplify the infection locally. This may tilt the balance towards productive infection in vaccinated animals that have stronger vaccine-induced Th1-biased CD4 T cell responses. To prove this hypothesis, one needs to determine the infection status of vaccine-induced CD4 T cells in the mucosa during the first few days after infection. However, it will be extremely hard and very expensive to study the infection status of virus-specific CD4 T cells in the mucosa early after productive infection in the repeat dose infection model, because not all animals will be infected at the first exposure and a large number of animals need to be euthanized early after infection. However, in support of our hypothesis, a previous study showed preferential infection of vaccine-induced CD4 T cells in vaccinated rhesus macaques compared to unvaccinated rhesus macaques very early in blood following single high dose SIVmac251 challenge that resulted in 100% infection of unvaccinated and vaccinated animals (13). As shown in that study, this preferential infection of vaccine-induced CD4 T cells was evident primarily at Day 7 post infection. This difference was not obvious at Days 10–21 (peak of virus replication) presumably because virus becomes systemic and infects non-virus specific CD4 T cells as well. Unfortunately, we did not collect PBMC from these studies at Day 7 post productive infection and thus are unable to investigate reservoirs at early time points. Another limitation of this study is that there may be additional mucosal markers such as α4β7, CD103, and CCR9 (required for homing to gut) on vaccine-induced IFNγ+ CD4 T cells may further help to refine the association between vaccine-induced CD4 T cells and protection. Unfortunately, we have not measured the expression of these markers in these studies. Another limitation of our study is that it is retrospective in nature. However, the fact that similar findings were found in four DNA/MVA vaccine studies irrespective of differences in the SIV strain and the route of challenge used strongly support the contribution of Th1 biased CD4 T cells in modulating SIV vaccine efficacy.
In conclusion, our results demonstrate that HIV vaccination approaches should minimize induction and migration of Th1-biased vaccine-induced CD4 T cells to mucosal tissues, and support the generation of Tfh responses. A major implication of these results is that it is absolutely critical to screen the phenotypic and functional quality of vaccine-induced CD4 T cell responses induced by different vaccine vectors and adjuvants with respect to Th differentiation and to minimize the induction of target cells in the mucosa. Our results strongly suggest that vaccination modalities/adjuvants that favor strong induction of Tfh responses over Th1-biased CD4 T cell response, could provide enhanced protection against HIV by inducing fewer target CD4 T cells. For example, adjuvants such as 3M052 (a TLR7/8 agonist) have been shown to induce a strong Tfh response with low Th1 response when compared to alum (37), and vaccination of rhesus macaques with Env protein and TLR7/8 + TLR4 agonists has been found more efficacious for generating protection against vaginal SIV challenge than has vaccination with the same Env protein and alum (37). More studies of molecules that modulate immune responses to vaccines are clearly needed to identify those which can generate CD4 T cells that promote high quality antibody responses and high frequencies of CD8 T cells without increasing numbers of CD4 target cells for HIV.
MATERIALS AND METHODS
Study design
The goal of this study was to determine the role of HIV vaccine-induced CD4 T cell response on protection against pathogenic mucosal HIV infection using the rhesus macaque model. To address this, we analyzed samples from four different macaque studies. These were selected to study protection against intrarectal (M14 and P165) or intravaginal (M15 and M19) infections and against SIV (M14, M15 and P165) or SHIV (M19) challenges. Animals were primed with two doses of DNA vaccines, and boosted with two doses of MVA vaccine. The DNA vaccines expressed SIVmac239 Gag, protease (PR), reverse transcriptase (RT); and SIV or HIV envelope (Env), Tat, and Rev. The MVA expressed SIVmac239 Gag, PR, RT, and SIV or HIV Env. At about 16–24 weeks post the final MVA, animals were challenged weekly either intrarectally or intravaginally, for a maximum of 8–12 weeks or until productively infected. Animals that showed greater than 60 copies/ml of plasma viral RNA at two consecutive weeks were considered productively infected. On the basis of M14 (19), P165 (20) and prior studies (31, 38), we included 15–20 animals in M15 and M19 studies. Veterinarians and animal research resources personnel that performed immunizations, and virology core personnel that determined plasma viral RNA were blinded for study group information. Due to logistical reasons, other assays were not performed on a blinded manner. Primary data are reported in data file S1.
Vaccines, vaccination regimen, and viral challenges for four macaque studies (see Table 1 for additional details)
Animals were either housed at the Yerkes National Primate Research Center or Bioqual Inc. and were cared for under the guidelines established by the Animal Welfare Act and the National Institute of Health (NIH) Guide for the Care and Use of Laboratory Animals using protocols approved by the respective Institutional Animal Care and Use Committee.
P165 study
Complete details of vaccines, vaccination schedule and viral challenges have been reported (20) and are summarized in Table 1. Briefly, 60 Indian origin rhesus macaques (Macaca mulatta) weighing from 2.6 to 15.3 Kg weight were housed at Bioqual Inc. Vaccinated animals received two DNA vaccinations (with and without GM-CSF as an adjuvant) on weeks 0 and 8, and two MVA vaccines on weeks 16 and 32. Twenty unvaccinated animals served as controls. All animals were challenged intrarectally with SIVsmE660-ABL using 412 TCID50 (determined using rhPBMC).
M15 study
20 female Indian rhesus macaques (Macca mulatta) from the Yerkes breeding colony were used. In this study, we used the same immunogens and challenge viruses that were used in P165 study with the following changes: there was an 8 week interval between each MVA vaccination, as opposed to 16 weeks in the P165 study, and 12 intravaginal challenges were employed using 1.02×104 TCID50 of SIVsmE660-ABL.
M14 study
10 male Indian rhesus macaques (Macca mulatta) from the Yerkes breeding colony were used. The complete details of vaccines, vaccination schedule and challenges have been reported previously (19). Briefly, the vaccine (D40LM40L) group was inoculated with 3 mg of DNA/SIV-CD40L (31) and 108 PFU of MVA/SIV premixed with 106 PFU of MVA expressing CD40L (MVA/CD40L). A group of SIV-naive rhesus macaques (RMs) served as controls. Eight weekly moderate-dose intrarectal challenges with SIVmac251were initiated at 22 to 24 weeks after the last immunization using 647 TCID50 (1.25×107 copies of viral RNA; 2006-Day 9 stock).
M19 study
22 Indian Rhesus macaques from the Yerkes breeding colony were cared for under the guidelines established by the Animal Welfare Act and the National Institute of Health (NIH) Guide for the Care and Use of Laboratory Animals using protocols approved by the Emory University Institutional Animal Care and Use Committee. All animals were immunized intramuscularly with two DNA primes (weeks 0 and 8 at 3mg/monkey/dose) followed by three MVA boosts (weeks 16, 24 and 38), with both vaccines encoding HIV-1 clade C 1086c env and Gag/Pol/RT derived from SIVmac239. Seven monkeys were necropsied at various time points to analyze the tissue specific immune responses. 15 monkeys were challenged 20 weeks after the last vaccination, intravaginally with 8 weekly low dose challenges using clade c SHIV1157-ipd3N4 virus.
ICS assays
SIV and SHIV-specific cellular immune responses were assessed by multi-parameter intracellular cytokine staining (ICS) assays following stimulation with SIVmac239 Gag, SIVmac239 Env, or HIV 1086c Env peptides as previously described (19, 20, 39). The following antibodies (clone names in parentheses) each conjugated to a different fluorochrome were used for detection of proteins by flow cytometry: CD3 (SP34–2), CD4 (L200), CD8 (RPA-T8), IFNγ (B27), IL-2 (MQ1–17H12), TNFα (MAb11), IL-21 (3A3-N2), IL-4 (MP4–25D2), MIP-1β (D21–1351), CCR5 (3A9) and CCR7 (150503). All values used in the analyses were background subtracted based on values in unstimulated cells that were mostly less that 0.01% and values that were higher than two-times the background were considered as positive.
Antibody assays
All antibody responses reported herein were measured according to the protocols described previously (19, 20). Briefly, SIV or HIV envelope specific antibody responses were assessed in serum using ELISAs. Plates were coated with SIVmac239 gp140 antigen (Immune Technology Corp) or HIV 1086c gp140 antigen (Duke Human Vaccine Institute). The concentrations of bound IgG were estimated relative to a standard curve that was created using purified monkey IgG and run in parallel to monkey sera samples. Rectal secretions were collected using premoistened Weck-Cel Sponges. Env gp140-specific IgG was measured by ELISA and expressed as nanograms of Env-specific IgG per micrograms of total IgG as described previously (19, 20).
A NaSCN displacement ELISA assay modeled after that described by Vermont was used for determining avidity (40). This assay was conducted using parallel titrations of test sera in our standard ELISA assay. Following the binding of the test sera, the parallel titrations were treated for 10 min at room temperature with PBS or 1.5 M NaSCN (prepared fresh in PBS). Then, the relative titer of bound Ab were determined using the standard ELISA procedure. The avidity index was calculated by dividing the dilution of the serum that gave an OD of 0.5 with NaSCN treatment by the dilution of the serum that gave an OD of 0.5 without NaSCN treatment and multiplying by 100.
RNA isolation and Microarray Assays
Total RNA was isolated from Paxgene tubes by use of Paxgene Blood RNeasy minikits (Qiagen) following the manufacturer’s protocol. RNA quality was assessed on an Agilent 2100 Bioanalyzer, using the Nanochip format. Fluorescently labeled probes were generated from each RNA sample using Agilent One-Color Low-Input Quick Amp labeling kit (Agilent Technologies) and hybridized to custom Agilent Rhesus (8×60K) oligonucleotide microarrays per manufacturer’s instructions. Slides were scanned with an Agilent DNA microarray scanner and Raw Agilent Microarray files were extracted using Agilent feature extractor version (version 10.7.3.1). Raw Microarray files were downloaded, background corrected using the “norm-exp” method with an offset of 1 and quantile normalized using the limma Bioconductor package in the R statistical software environment (version 3.1.3). Replicate probes were mean summarized, and low expressed probes were removed (41)(1). Exploratory analysis was performed in R, and batch correction was applied using the sva Bioconductor package. Statistical analysis was performed through the limma Bioconductor package. Raw and normalized expression data was submitted to the Gene Expression Omnibus, GEO (accession GSE93835).
Differential Expression and Multivariate Analysis
Normalized matrices were assessed for differential expression between early and late SIV acquirers at each microarray time point using the limma package (version 3.28.21) within R (version 3.3.1) (42). Animals were grouped by infection outcome and corrected for paired effects using the duplicate for correlation function within limma (41). Differential expression between early and late acquirers at any time point or for a time point compared to pre-vaccination was determined to be above a threshold of above 1.5 fold change above or below pre-vaccination samples (Week 0, Day 1), with a Benjamini-Hochberg adjusted p-value < 0.05. Numbers of differentially expressed genes in each condition were visualized using the ggplot2 package (version 2.1.0) (H. Wickham. ggplot2: Elegant Graphics for Data Analysis. Springer-Verlag New York, 2009). The union of all genes differentially expressed in at least one condition was plotted by heatmap, and clusters of genes determined by cutting the Euclidean-distance dendrogram were classified by their most highly enriched gene ontology term using DAVID (43). Multivariate analysis was conducted using the mixOmics package (version 6.1.0) (44, 45). Gene expression for Day 7 samples from all animals was collected and filtered by those probe IDs that could be annotated to known gene IDs for further analysis. sPLS-DA and mixDIABLO (block-sPLS-DA) analyses were run against the gene expression profiles using infection outcome alone or against frequencies of IFNγ+ CD4 T cells in blood and anti-gp140 antibody in serum and rectal secretions, respectively. sPLS-DA method was implemented within the R mixOmics package (Kim-Anh Le Cao, Florian Rohart, Ignacio Gonzalez, Sebastien Dejean, with key contributors Benoit Gautier, Francois Bartolo, contributions from Pierre Monget, Jeff Coquery, FangZou Yao and Benoit Liquet. (2016). mixOmics: Omics Data Integration Project. R package version 6.1.1. (https://CRAN.R-project.org/package=mixOmics)). Parameter tuning using 5 folds against 10 repeats was used to select the numbers of genes for each analysis. Although two components were selected for sPLS-DA to visualize separation of samples, mixDIABLO was run with one component each as recommended using the Y – 1 approach, which in this case is one less than the number of disease outcomes. Results were visualized using Clustered Image Matrices with clusters labeled by common gene ontologies and pathways as described elsewhere (43) (46). The 150 genes identified to be positively or negatively correlated with CD4 frequencies and SIV infection outcomes were run through network analysis using Ingenuity Pathway Analysis to obtain interactions among the corresponding genes and proteins. Additionally, each gene was assigned to a primary functional type according to overall Gene Ontology Functional Category Direct results through DAVID. Common functions were grouped together as network nodes connected by shared interactions as identified above, and the resulting network was visualized with Cytoscape 3.4.0 (47).
Statistical analysis
Kaplan-Meier curves and the log-rank Mantel Cox test were used to display and test for differences in rate of infection. The Wilcoxon Mann-Whitney U test was used to compare antibody and T cell responses and viral RNA copies between groups. The Pearson correlation test was used for correlations. P values were not corrected for multiple comparisons, and a 2-sided P value of 0.05 or less was considered significant. Statistical analyses were performed using GraphPad Prism version 6.0 for Mac (GraphPad Software).
Supplementary Material
Fig. S1. SIV-specific IFNγ+ CD4 and CD8 T cell responses in the M15 and M19 studies.
Fig. S2. DNA/MVA vaccine induced CD4 T cells are Th1 biased.
Fig. S3. Total and SIV-specific CD4 T cells in blood and tissues.
Fig. S4. Influence of vaccine induced IFNγ+ CD4 T cells on protection in the M15 study.
Fig. S5. Correlation between the number of challenges to infection and vaccine-specific responses in the M19 study.
Table S1. List of genes described in Fig. 5.
Data file S1. Primary data.
Acknowledgements
The authors thank the Yerkes Division of Research Resources for animal care; Emory CFAR virology core for viral load assays; Dr. Michael Katze for overseeing the sample processing for microarray assays; the NIH AIDS Research and Reference Reagent Program for the provision of peptides and cell lines; and Dr. Vanessa Hirsch for the SIVsmE660 challenge stock. We also thank Drs. Nancy Miller, Alan Schultz and Jon Warren of the Division of AIDS for council on the design and execution of SVEU P165 study. We are indebted to Dr. Tianwei Yu for his help with statistical analyses and to Robert L. Wilson for technical assistance in the measurement of mucosal antibodies. We thank Dr. Hanne Andersen from Bioqual, for her help in managing the P165 study. Rama Amara is a co-inventor of DNA/MVA vaccine technology that has been licensed to Geovax Inc., by Emory University.
Funding: This work was supported in part by National Institutes of Health Grants PO1 AI088575 (to R.R.A.), U19AI109633 (to RRA), U19AI096187 (to EH, RRA), UM1 AI124436 (to EH, RRA), Emory University CFAR grant P30 AI050409, NCRR/NIH base grants P51 OD011132 (to YNPRC), NIAID Contract HHSN272201300010C (to M.G.), P51OD01425 (to M.G), and P30 RR00168 (to NEPRC) and the Division of Intramural Research, NIAID, NIH. The P165 study was supported by the Simian Vaccine evaluation Unit of the Division of AIDS, NIAID.
Footnotes
Competing interests: R.R.A is a co-inventor of the DNA/MVA vaccine technology that has been licensed to Geovax Inc., by Emory University.
Data and materials availability: All data are available in the main text or the supplementary material.
References and Notes
- 1.Pharris A, Spiteri G, Noori T, Amato-Gauci AJ, Ten years after Dublin: principal trends in HIV surveillance in the EU/EEA, 2004 to 2013. Euro Surveill 19, 20968 (2014). [DOI] [PubMed] [Google Scholar]
- 2.Corey L, Gilbert PB, Tomaras GD, Haynes BF, Pantaleo G, Fauci AS, Immune correlates of vaccine protection against HIV-1 acquisition. Sci Transl Med 7, 310rv317 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rerks-Ngarm S, Pitisuttithum P, Nitayaphan S, Kaewkungwal J, Chiu J, Paris R, Premsri N, Namwat C, de Souza M, Adams E, Benenson M, Gurunathan S, Tartaglia J, McNeil JG, Francis DP, Stablein D, Birx DL, Chunsuttiwat S, Khamboonruang C, Thongcharoen P, Robb ML, Michael NL, Kunasol P, Kim JH, Investigators M-T, Vaccination with ALVAC and AIDSVAX to Prevent HIV-1 Infection in Thailand. New Engl J Med 361, 2209–2220 (2009). [DOI] [PubMed] [Google Scholar]
- 4.Buchbinder SP, Mehrotra DV, Duerr A, Fitzgerald DW, Mogg R, Li D, Gilbert PB, Lama JR, Marmor M, Del Rio C, McElrath MJ, Casimiro DR, Gottesdiener KM, Chodakewitz JA, Corey L, Robertson MN, T. Step Study Protocol, Efficacy assessment of a cell-mediated immunity HIV-1 vaccine (the Step Study): a double-blind, randomised, placebo-controlled, test-of-concept trial. Lancet 372, 1881–1893 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McElrath MJ, De Rosa SC, Moodie Z, Dubey S, Kierstead L, Janes H, Defawe OD, Carter DK, Hural J, Akondy R, Buchbinder SP, Robertson MN, Mehrotra DV, Self SG, Corey L, Shiver JW, Casimiro DR, T. Step Study Protocol, HIV-1 vaccine-induced immunity in the test-of-concept Step Study: a case-cohort analysis. Lancet 372, 1894–1905 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fauci AS, Marovich MA, Dieffenbach CW, Hunter E, Buchbinder SP, Immune Activation with HIV Vaccines. Science 344, 49–51 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Qureshi H, Ma Z-M, Huang Y, Hodge G, Thomas MA, DiPasquale J, DeSilva V, Fritts L, Bett AJ, Casimiro DR, Shiver JW, Robert-Guroff M, Robertson MN, McChesney MB, Gilbert PB, Miller CJ, Low-Dose Penile SIVmac251 Exposure of Rhesus Macaques Infected with Adenovirus Type 5 (Ad5) and Then Immunized with a Replication-Defective Ad5-Based SIV gag/pol/nef Vaccine Recapitulates the Results of the Phase IIb Step Trial of a Similar HIV-1 Vaccine. Journal of Virology 86, 2239–2250 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Benlahrech A, Harris J, Meiser A, Papagatsias T, Hornig J, Hayes P, Lieber A, Athanasopoulos T, Bachy V, Csomor E, Daniels R, Fisher K, Gotch F, Seymour L, Logan K, Barbagallo R, Klavinskis L, Dickson G, Patterson S, Adenovirus vector vaccination induces expansion of memory CD4 T cells with a mucosal homing phenotype that are readily susceptible to HIV-1. Proceedings of the National Academy of Sciences 106, 19940–19945 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bukh I, Calcedo R, Roy S, Carnathan DG, Grant R, Qin Q, Boyd S, Ratcliffe SJ, Veeder CL, Bellamy SL, Betts MR, Wilson JM, Increased Mucosal CD4+ T Cell Activation in Rhesus Macaques following Vaccination with an Adenoviral Vector. Journal of Virology 88, 8468–8478 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carnathan DG, Wetzel KS, Yu J, Lee ST, Johnson BA, Paiardini M, Yan J, Morrow MP, Sardesai NY, Weiner DB, Ertl HCJ, Silvestri G, Activated CD4+CCR5+ T cells in the rectum predict increased SIV acquisition in SIVGag/Tat-vaccinated rhesus macaques. Proceedings of the National Academy of Sciences 112, 518–523 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Staprans SI, Barry AP, Silvestri G, Safrit JT, Kozyr N, Sumpter B, Nguyen H, McClure H, Montefiori D, Cohen JI, Feinberg MB, Enhanced SIV replication and accelerated progression to AIDS in macaques primed to mount a CD4 T cell response to the SIV envelope protein. P Natl Acad Sci USA 101, 13026–13031 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Douek DC, Brenchley JM, Betts MR, Ambrozak DR, Hill BJ, Okamoto Y, Casazza JP, Kuruppu J, Kunstman K, Wolinsky S, Grossman Z, Dybul M, Oxenius A, Price DA, Connors M, Koup RA, HIV preferentially infects HIV-specific CD4+ T cells. Nature 417, 95–98 (2002). [DOI] [PubMed] [Google Scholar]
- 13.Mattapallil JJ, Douek DC, Buckler-White A, Montefiori D, Letvin NL, Nabel GJ, Roederer M, Vaccination preserves CD4 memory T cells during acute simian immunodeficiency virus challenge 10.1084/jem.20060657. J. Exp. Med 203, 1533–1541 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Perreau M, Savoye A-L, De Crignis E, Corpataux J-M, Cubas R, Haddad EK, De Leval L, Graziosi C, Pantaleo G, Follicular helper T cells serve as the major CD4 T cell compartment for HIV-1 infection, replication, and production. The Journal of Experimental Medicine 210, 143–156 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lindqvist M, van Lunzen J, Soghoian DZ, Kuhl BD, Ranasinghe S, Kranias G, Flanders MD, Cutler S, Yudanin N, Muller MI, Davis I, Farber D, Hartjen P, Haag F, Alter G, Schulze zur Wiesch J, Streeck H, Expansion of HIV-specific T follicular helper cells in chronic HIV infection. The Journal of Clinical Investigation 122, 3271–3280 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mylvaganam GH, Velu V, Hong J-J, Sadagopal S, Kwa S, Basu R, Lawson B, Villinger F, Amara RR, Diminished Viral Control during Simian Immunodeficiency Virus Infection Is Associated with Aberrant PD-1hi CD4 T Cell Enrichment in the Lymphoid Follicles of the Rectal Mucosa. The Journal of Immunology 193, 4527–4536 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kohler SL, Pham MN, Folkvord JM, Arends T, Miller SM, Miles B, Meditz AL, McCarter M, Levy DN, Connick E, Germinal Center T Follicular Helper Cells Are Highly Permissive to HIV-1 and Alter Their Phenotype during Virus Replication. The Journal of Immunology 196, 2711–2722 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lewis GK, DeVico AL, Gallo RC, Antibody persistence and T-cell balance: Two key factors confronting HIV vaccine development. Proceedings of the National Academy of Sciences 111, 15614–15621 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kwa S, Sadagopal S, Shen X, Hong JJ, Gangadhara S, Basu R, Victor B, Iyer SS, LaBranche CC, Montefiori DC, Tomaras GD, Villinger F, Moss B, Kozlowski PA, Amara RR, CD40L-Adjuvanted DNA/MVA SIV Vaccine Enhances Protection Against Neutralization Resistant Mucosal SIV Infection. Journal of Virology 89, 4690–4695 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chamcha V, Kannanganat S, Gangadhara S, Nabi R, Kozlowski PA, Montefiori DC, LaBranche CC, Wrammert J, Keele BF, Balachandran H, Sahu S, Lifton M, Santra S, Basu R, Moss B, Robinson HL, Amara RR, Strong, but Age-Dependent, Protection Elicited by a DNA/Modified Vaccinia Ankara Simian Immunodeficiency Virus Vaccine. Open Forum Infectious Diseases 3, ofw034 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kwa S, Lai LL, Gangadhara S, Siddiqui M, Pillai VB, Labranche C, Yu TW, Moss B, Montefiori DC, Robinson HL, Kozlowski PA, Amara RR, CD40L-Adjuvanted DNA/Modified Vaccinia Virus Ankara Simian Immunodeficiency Virus SIV239 Vaccine Enhances SIV-Specific Humoral and Cellular Immunity and Improves Protection against a Heterologous SIVE660 Mucosal Challenge. J Virol 88, 9579–9589 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Letvin NL, Rao SS, Montefiori DC, Seaman MS, Sun Y, Lim SY, Yeh WW, Asmal M, Gelman RS, Shen L, Whitney JB, Seoighe C, Lacerda M, Keating S, Norris PJ, Hudgens MG, Gilbert PB, Buzby AP, Mach LV, Zhang J, Balachandran H, Shaw GM, Schmidt SD, Todd JP, Dodson A, Mascola JR, Nabel GJ, Immune and Genetic Correlates of Vaccine Protection Against Mucosal Infection by SIV in Monkeys. Sci Transl Med 3, 81ra36 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Reynolds MR, Sacha JB, Weiler AM, Borchardt GJ, Glidden CE, Sheppard NC, Norante FA, Castrovinci PA, Harris JJ, Robertson HT, Friedrich TC, McDermott AB, Wilson NA, Allison DB, Koff WC, Johnson WE, Watkins DI, The TRIM5{alpha} genotype of rhesus macaques affects acquisition of simian immunodeficiency virus SIVsmE660 infection after repeated limiting-dose intrarectal challenge. J Virol 85, 9637–9640 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yeh WW, Rao SS, Lim SY, Zhang J, Hraber PT, Brassard LM, Luedemann C, Todd JP, Dodson A, Shen L, Buzby AP, Whitney JB, Korber BT, Nabel GJ, Mascola JR, Letvin NL, The TRIM5 gene modulates penile mucosal acquisition of simian immunodeficiency virus in rhesus monkeys. J Virol 85, 10389–10398 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kannanganat S, Wyatt LS, Gangadhara S, Chamcha V, Chea LS, Kozlowski PA, LaBranche CC, Chennareddi L, Lawson B, Reddy PB, Styles TM, Vanderford TH, Montefiori DC, Moss B, Robinson HL, Amara RR, High Doses of GM-CSF Inhibit Antibody Responses in Rectal Secretions and Diminish Modified Vaccinia Ankara/Simian Immunodeficiency Virus Vaccine Protection in TRIM5alpha-Restrictive Macaques. J Immunol, (2016). [DOI] [PMC free article] [PubMed]
- 26.Paiardini M, Cervasi B, Reyes-Aviles E, Micci L, Ortiz AM, Chahroudi A, Vinton C, Gordon SN, Bosinger SE, Francella N, Hallberg PL, Cramer E, Schlub T, Chan ML, Riddick NE, Collman RG, Apetrei C, Pandrea I, Else J, Munch J, Kirchhoff F, Davenport MP, Brenchley JM, Silvestri G, Low levels of SIV infection in sooty mangabey central memory CD4+ T cells are associated with limited CCR5 expression. Nat Med 17, 830–836 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Iyer SS, Gangadhara S, Victor B, Gomez R, Basu R, Hong JJ, Labranche C, Montefiori DC, Villinger F, Moss B, Amara RR, Codelivery of Envelope Protein in Alum with MVA Vaccine Induces CXCR3-Biased CXCR5+ and CXCR5-CD4 T Cell Responses in Rhesus Macaques. J Immunol 195, 994–1005 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Locci M, Havenar-Daughton C, Landais E, Wu J, Kroenke Mark A., Arlehamn Cecilia L., Su Laura F., Cubas R, Davis Mark M., Sette A, Haddad Elias K., Poignard P, Crotty S, Human Circulating PD-1+CXCR3−CXCR5+ Memory Tfh Cells Are Highly Functional and Correlate with Broadly Neutralizing HIV Antibody Responses. Immunity 39, 758–769 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Robinson HL, Amara RR, Protective immunity from a germinal center sanctuary. Nat Med 18, 1614–1616 (2012). [DOI] [PubMed] [Google Scholar]
- 30.Lai L, Vodros D, Kozlowski PA, Montefiori DC, Wilson RL, Akerstrom VL, Chennareddi L, Yu T, Kannanganat S, Ofielu L, Villinger F, Wyatt LS, Moss B, Amara RR, Robinson HL, GM-CSF DNA: an adjuvant for higher avidity IgG, rectal IgA, and increased protection against the acute phase of a SHIV-89.6P challenge by a DNA/MVA immunodeficiency virus vaccine. Virology 369, 153–167 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kwa S, Lai L, Gangadhara S, Siddiqui M, Pillai VB, Labranche C, Yu T, Moss B, Montefiori DC, Robinson HL, Kozlowski PA, Amara RR, CD40L-adjuvanted DNA/modified vaccinia virus Ankara simian immunodeficiency virus SIV239 vaccine enhances SIV-specific humoral and cellular immunity and improves protection against a heterologous SIVE660 mucosal challenge. J Virol 88, 9579–9589 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Le Cao KA, Martin PGP, Robert-Granie C, Besse P, Sparse canonical methods for biological data integration: application to a cross-platform study. Bmc Bioinformatics 10, (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shi H, Wang Y, Li X, Zhan X, Tang M, Fina M, Su L, Pratt D, Bu CH, Hildebrand S, Lyon S, Scott L, Quan J, Sun Q, Russell J, Arnett S, Jurek P, Chen D, Kravchenko VV, Mathison JC, Moresco EMY, Monson NL, Ulevitch RJ, Beutler B, NLRP3 activation and mitosis are mutually exclusive events coordinated by NEK7, a new inflammasome component. Nat Immunol 17, 250–258 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kwon M-J, Jeon Y-J, Lee K-Y, Kim T-Y, Superoxide Dismutase 3 Controls Adaptive Immune Responses and Contributes to the Inhibition of Ovalbumin-Induced Allergic Airway Inflammation in Mice. Antioxidants & Redox Signaling 17, 1376–1392 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rerks-Ngarm S, Pitisuttithum P, Nitayaphan S, Kaewkungwal J, Chiu J, Paris R, Premsri N, Namwat C, de Souza M, Adams E, Benenson M, Gurunathan S, Tartaglia J, McNeil JG, Francis DP, Stablein D, Birx DL, Chunsuttiwat S, Khamboonruang C, Thongcharoen P, Robb ML, Michael NL, Kunasol P, Kim JH, Vaccination with ALVAC and AIDSVAX to Prevent HIV-1 Infection in Thailand. New England Journal of Medicine 361, 2209–2220 (2009). [DOI] [PubMed] [Google Scholar]
- 36.Jones AT, Shen X, Walter KL, LaBranche CC, Wyatt LS, Tomaras GD, Montefiori DC, Moss B, Barouch DH, Clements JD, Kozlowski PA, Varadarajan R, Amara RR, HIV-1 vaccination by needle-free oral injection induces strong mucosal immunity and protects against SHIV challenge. Nat Commun 10, 798 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kasturi SP, Kozlowski PA, Nakaya HI, Burger MC, Russo P, Pham M, Kovalenkov Y, Silveira EL, Havenar-Daughton C, Burton SL, Kilgore KM, Johnson MJ, Nabi R, Legere T, Sher ZJ, Chen X, Amara RR, Hunter E, Bosinger SE, Spearman P, Crotty S, Villinger F, Derdeyn CA, Wrammert J, Pulendran B, Adjuvanting a Simian Immunodeficiency Virus Vaccine with Toll-Like Receptor Ligands Encapsulated in Nanoparticles Induces Persistent Antibody Responses and Enhanced Protection in TRIM5alpha Restrictive Macaques. J Virol 91, (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Amara RR, Villinger F, Altman JD, Lydy SL, O’Neil SP, Staprans SI, Montefiori DC, Xu Y, Herndon JG, Wyatt LS, Candido MA, Kozyr NL, Earl PL, Smith JM, Ma HL, Grimm BD, Hulsey ML, Miller J, McClure HM, McNicholl JM, Moss B, Robinson HL, Control of a mucosal challenge and prevention of AIDS by a multiprotein DNA/MVA vaccine. Science 292, 69–74 (2001). [DOI] [PubMed] [Google Scholar]
- 39.Hulot SL, Cale EM, Korber BT, Letvin NL, Vaccine-Induced CD8+ T Lymphocytes of Rhesus Monkeys Recognize Variant Forms of an HIV Epitope but Do Not Mediate Optimal Functional Activity. J Immunol, (2011). [DOI] [PubMed]
- 40.Vermont CL, van Dijken HH, van Limpt CJ, de Groot R, van Alphen L, van Den Dobbelsteen GP, Antibody avidity and immunoglobulin G isotype distribution following immunization with a monovalent meningococcal B outer membrane vesicle vaccine. Infect Immun 70, 584–590 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Smyth GK, Michaud J, Scott HS, Use of within-array replicate spots for assessing differential expression in microarray experiments. Bioinformatics 21, 2067–2075 (2005). [DOI] [PubMed] [Google Scholar]
- 42.Ritchie ME, Phipson B, Wu D, Hu Y, Law CW, Shi W, Smyth GK, limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res 43, e47 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Huang da W, Sherman BT, Lempicki RA, Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat Protoc 4, 44–57 (2009). [DOI] [PubMed] [Google Scholar]
- 44.Le Cao KA, Gonzalez I, Dejean S, integrOmics: an R package to unravel relationships between two omics datasets. Bioinformatics 25, 2855–2856 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gonzalez I, Cao KA, Davis MJ, Dejean S, Visualising associations between paired ‘omics’ data sets. BioData Min 5, 19 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chen EY, Tan CM, Kou Y, Duan Q, Wang Z, Meirelles GV, Clark NR, Ma’ayan A, Enrichr: interactive and collaborative HTML5 gene list enrichment analysis tool. BMC Bioinformatics 14, 128 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shannon P, Markiel A, Ozier O, Baliga NS, Wang JT, Ramage D, Amin N, Schwikowski B, Ideker T, Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res 13, 2498–2504 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig. S1. SIV-specific IFNγ+ CD4 and CD8 T cell responses in the M15 and M19 studies.
Fig. S2. DNA/MVA vaccine induced CD4 T cells are Th1 biased.
Fig. S3. Total and SIV-specific CD4 T cells in blood and tissues.
Fig. S4. Influence of vaccine induced IFNγ+ CD4 T cells on protection in the M15 study.
Fig. S5. Correlation between the number of challenges to infection and vaccine-specific responses in the M19 study.
Table S1. List of genes described in Fig. 5.
Data file S1. Primary data.