Abstract
A 17-year-old healthy girl underwent an uneventful esthetic septorhinoplasty. She was easily extubated and transferred to the postanesthesia care unit (PACU) with oxygen saturation (Spo2) of 96%. About 30 minutes after arrival in the PACU, she developed dyspnea with Spo2 of 84% and promptly received oxygen with bilevel positive airway pressure in conjunction with low-dose corticosteroid. The subsequent chest computed tomography (CT) revealed bilateral patchy infiltrates similar to the radiologic findings of Coronavirus Disease 2019 (COVID-19). Finally, a reverse transcriptase polymerase chain reaction (RT-PCR) of a pharyngeal specimen confirmed the diagnosis of COVID-19.
Coronavirus Disease 2019 (COVID-19) first presented as unusual pneumonia of unknown cause in late December 2019. Based on the existing data, >85% of COVID-19 patients are 30–79 years old and patients aged ≤19 years of age are rarely affected (about 2%). It seems that COVID-19 has a milder course and a better outcome in pediatric patients. A large series of 72,314 cases from China reported no death in children aged ≤9 years compared to people aged ≥80 years, with a case fatality rate of 14.8%.1
Herein, we report an asymptomatic COVID-19 patient aged 17 years, who developed postoperative respiratory distress as the first symptom of COVID-19 pneumonia shortly following an uneventful septorhinoplasty. A written informed consent for publication was obtained from the patient, and this article adheres to the applicable Enhancing the QUAlity And Transparency Of health Research (EQUATOR) guideline.
CASE DESCRIPTION
A 17-year-old healthy girl (weight 68 kg and height 172 cm) was admitted to the plastic surgery ward for esthetic septorhinoplasty. There was no significant medical or surgical history; she was not taking any medicines or illicit drugs and had no history of allergies. On admission, review of her respiratory and cardiovascular systems was noted to be normal. Preoperative physical examination was normal, with a blood pressure of 110/70 mm Hg, pulse of 90 beats/min, respiratory rate of 16 breaths/min, oral temperature of 36.6°C, and saturation of peripheral oxygen (Spo2) of 98%. Blood tests revealed a mild microcytic hypochromic anemia (hemoglobin 111 g L−1; white blood cell count 9.360 × 109 L−1; lymphocyte count 2.246 × 109 L−1).
On the day of surgery, she was premedicated with midazolam 2 mg·mL−1 intravenously and fentanyl 2 µg·kg−1. General anesthesia was induced with propofol 2 mg·kg−1 and rocuronium 0.5 mg·kg−1 and maintained with propofol 0.15 mg·kg−1·min−1 and remifentanil 0.4 µg·kg−1·min−1. She was intubated with a 6.5-mm endotracheal tube. The operation lasted 70 minutes, and the intraoperative course was uneventful. Anesthesia was reversed using atropine and neostigmine 0.04 mg·kg−1, and the patient was extubated. She was transferred to the postanesthesia care unit (PACU) with normal spontaneous breathing, Spo2 of 96%, and bilateral hemostatic nasal packing. About 30 minutes after arrival in the PACU, while the patient was awake and alert, she complained of trouble breathing. She was tachypneic, with Spo2 of 84. The auscultation of lung was unremarkable. There was no evidence of upper respiratory obstruction or pulmonary edema. She promptly received oxygen with bilevel positive airway pressure (BiPAP) and dexamethasone 8 mg. Due to the recent surgery, however, the mask was placed only over her mouth. The Spo2 increased, and the patient was admitted to the intensive care unit while she was still on BiPAP. As the cause of her hypoxemic event was still unclear, a chest computed tomography (CT) was ordered. Surprisingly, imaging revealed bilateral multilobar patchy opacities predominantly in the posterior and peripheral regions, consistent with previously described radiologic features of COVID-19 (Figure). A reverse transcriptase polymerase chain reaction (RT-PCR) of a pharyngeal specimen confirmed the diagnosis of COVID-19. She was treated with hydroxychloroquine sulfate 200 mg twice daily and was discharged 48 hours later without any complaints (with Spo2 98%). She was isolated at home and daily monitored for 2 weeks after discharge, and the follow-up was unremarkable.
Figure.
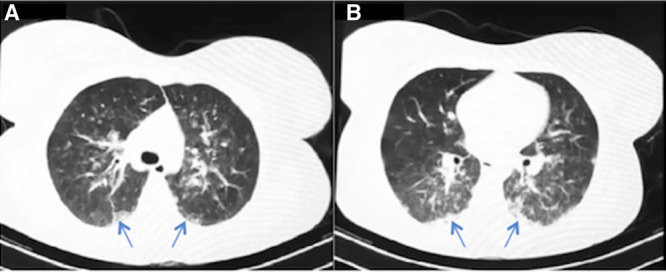
Axial view of a lung CT 4 h after extubation. It revealed bilateral multilobar patchy opacities (arrows) predominantly in posterior and peripheral regions (A and B). CT indicates computed tomography.
DISCUSSION
Ventilatory events are not uncommon in the PACU. Critical ventilatory events have been reported to complicate 0.8%–6.9% of surgeries.2 An advanced age (>60 years) and a medical history of diabetes mellitus, chronic obstructive pulmonary disease, and sleep apnea have been attributed to the postoperative ventilatory complications.3 Atelectasis has been considered as the pathophysiological mainstay for ventilatory complications in the PACU.2,3 In young patients without any underlying disease, like our case, upper airway obstruction, alveolar hypoventilation due to residual effects of neuromuscular blockers, and aspiration pneumonia should be considered first.2,4 In our patient, the physical examination of upper respiratory tract and the auscultation of lung did not give any clue in favor of these diagnoses. The patient was tachypneic and had no pathological breath sound, such as stridor or crackles.
Usage of occlusive nasal packs, accumulation of bloody secretions in pharynx, and stimulation of laryngeal reflex could potentially increase the risk of ventilatory events following rhinoplasty.5 In our patient, nasal tampons were removed early after developing dyspnea, and the examination of pharynx was unremarkable. In patients developing postoperative ventilatory distress, negative pressure pulmonary edema (NPPE) should be taken into account, especially following aerodigestive tract surgeries. Postoperative NPPE has been attributed to the laryngospasm due to stimulation of the superior laryngeal nerve by bloody secretions or during intubation, extubation, or removal of throat packing.5 The physical examination of the upper and lower respiratory tract of our patient did not give any clue in favor of laryngospasm or pulmonary edema. The chest CT of patient revealed bilateral peripheral infiltrates consistent with pulmonary involvement of COVID-19.
In conclusion, we endorse that elective surgeries should be postponed during this viral pandemic to avoid putting medical personnel at risk of infection. COVID-19 should be considered in the differential diagnosis of ventilatory distress and hypoxemia, independent of whether the patient is symptomatic or not.
ACKNOWLEDGEMENTS
We gratefully acknowledge the critical review of manuscript by Dr BobbieJean Sweitzer.
DISCLOSURES
Name: Ramin Rahmanzade.
Contribution: This author helped to devise the project and the main conceptual idea, gather the data, review the literature, write the manuscript, and proof the final version.
Name: Reza Rahmanzadeh.
Contribution: This author helped to devise the project, gather the data, and review the literature and made substantial contribution by revising and proofing the manuscript.
Name: Seyed Mohammad Reza Hashemian.
Contribution: This author was intensivist of patient and helped substantially to devise the project and the main conceptual idea, gather the data, and revise the manuscript.
This manuscript was handled by: BobbieJean Sweitzer, MD, FACP.
GLOSSARY
- BiPAP
- bilevel positive airway pressure
- COVID-19
- Coronavirus Disease 2019
- CT
- computed tomography
- EQUATOR
- Enhancing the QUAlity And Transparency Of health Research
- NPPE
- negative pressure pulmonary edema
- PACU
- postanesthesia care unit
- RT-PCR
- reverse transcriptase polymerase chain reaction
- Spo2
- saturation of peripheral oxygen
Funding: None.
The authors declare no conflicts of interest.
Ramin Rahmanzade and Reza Rahmanzadeh contributed equally to this work.
REFERENCES
- 1.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention [epub ahead of print]. JAMA. 2020. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 2.Karcz M, Papadakos PJ. Respiratory complications in the postanesthesia care unit: a review of pathophysiological mechanisms. Can J Respir Ther. 2013; 49:21–29 [PMC free article] [PubMed] [Google Scholar]
- 3.Kelkar KV. Post-operative pulmonary complications after non-cardiothoracic surgery. Indian J Anaesth. 2015; 59:599–605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miskovic A, Lumb AB. Postoperative pulmonary complications. Br J Anaesth. 2017; 118:317–334 [DOI] [PubMed] [Google Scholar]
- 5.Westreich R, Sampson I, Shaari CM, Lawson W. Negative-pressure pulmonary edema after routine septorhinoplasty: discussion of pathophysiology, treatment, and prevention. Arch Facial Plast Surg. 2006; 8:8–15 [DOI] [PubMed] [Google Scholar]


