Abstract
Introduction:
Ambient air pollution is a known risk factor for adverse birth outcomes, but the role of ultrafine particles (UFPs) is not well understood. Aircraft-origin UFPs adversely affect air quality over large residential areas downwind of airports, but their reproductive health burden remains uninvestigated.
Objectives:
This analysis evaluated whether UFPs from jet aircraft emissions are associated with increased rates of preterm birth (PTB) among pregnant mothers living downwind of Los Angeles International Airport (LAX).
Methods:
This population-based study used birth records, provided by the California Department of Public Health, to ascertain birth outcomes and a novel, validated geospatial UFP dispersion model approach to estimate in utero exposures. All mothers who gave birth from 2008 to 2016 while living within of LAX were included in this analysis (; including 15,134 PTBs).
Results:
In utero exposure to aircraft-origin UFPs was positively associated with PTB. The odds ratio (OR) per interquartile range (IQR) increase [9,200 particles per cubic centimeter (cc)] relative UFP exposure was 1.04 [95% confidence interval (CI): 1.02, 1.06]. When comparing the fourth quartile of UFP exposure to the first quartile, the OR for PTB was 1.14 (95% CI: 1.08, 1.20), adjusting for maternal demographic characteristics, exposure to traffic-related air pollution, and airport-related noise.
Conclusion:
Our results suggest that emissions from aircraft play an etiologic role in PTBs, independent of noise and traffic-related air pollution exposures. These findings are of public health concern because UFP exposures downwind of airfields are common and may affect large, densely populated residential areas. https://doi.org/10.1289/EHP5732
Introduction
Approximately 1 in 10 births in the United States are preterm (Martin et al. 2018), increasing the infant’s risk for developing complications, such as respiratory problems, infections, developmental delays, and vision or hearing impairments (WHO 2018). Prematurity is also the leading cause of neonatal mortality (Harrison and Goldenberg 2016) and generates an annual economic burden in the United States of [Institute of Medicine (U.S.) 2007].
Exposure to ambient air pollution during pregnancy has previously been identified as a risk factor for adverse birth outcomes, including preterm birth (PTB) (Maisonet et al. 2004; Ponce et al. 2005; Ritz et al. 2000, 2002; Ritz and Yu 1999; Šrám et al. 2005; Stillerman et al. 2008; Wilhelm and Ritz 2003, 2005). The effect of ambient air pollution from ground-transportation emissions on birth outcomes has been extensively studied, but the effects of aircraft emissions have not. During landing, takeoff, and taxiing, aircraft generate pollutant plumes that are blown downwind of airports, potentially adversely affecting the health of residents. The pollutants include particulate matter (PM), especially ultrafine particles (UFPs) from jet engines; volatile organic compounds; oxides of sulfur; and oxides of nitrogen (Carslaw et al. 2006; Ratliff et al. 2009; Valotto and Varin 2016; Yu et al. 2004). PM has traditionally been measured and regulated in terms of mass concentration of particles with aerodynamic diameter less than () or less than (). Ultrafine or nanoparticles, which are less than in diameter, are not routinely monitored or regulated. They account for little mass, but make up the majority of particles in terms of number and surface area (Hinds 1999). On an equal mass basis, UFPs may have more impact on health than do particulates with larger aerodynamic diameters, such as (Hyder et al. 2014; Lamichhane et al. 2015; Lee et al. 2013) and (Ritz et al. 2000; Wilhelm and Ritz 2005), due to their greater mobility in the body and greater surface area.
Recent studies report adverse air quality impacts from landing jets over large areas downwind of major airports (Hudda et al. 2016, 2018, 2014; Keuken et al. 2015; Masiol et al. 2017b, 2017a; Riley et al. 2016). For example, jets approaching Los Angeles International Airport (LAX) in Los Angeles, California, produce ground-level UFP concentrations more than twice the nearby ambient levels at distances up to away from the airport (Hudda et al. 2014). Here, we evaluated whether UFPs from jet aircraft emissions increase rates of PTB near LAX based on an AERMOD dispersion model for UFPs that we built and validated with spatially extensive ground-level measurements.
Materials and Methods
Sample Population and Health Outcome
We identified all mothers who gave birth from 2008 through 2016 while living within of LAX using birth certificates obtained from the California Department of Public Health. Our health outcome, PTB, was defined as a live birth occurring before 37 wk gestation (yes/no). We excluded birth records with implausible gestational ages ( or , ), implausible birth weights ( or , ), nonsingleton pregnancies (), or missing data on any covariates () leaving 174,186 births. This study was approved by the University of California Los Angeles Institutional Review Board and the California Health and Human Services Agency’s Committee for the Protection of Human Subjects. This study used routinely collected administrative data only and thus required no contact with research participants. Therefore, a waiver of informed consent was granted because it would not affect the rights of the participant nor could this research be practicably carried out without the waiver. Privacy and confidentiality were assured by using an encrypted and secure, internet-disabled computer for all data storage and analysis.
Exposure Assessment—UFPs
The U.S. Environmental Protection Agency (U.S. EPA) AERMET model was used first to generate relevant meteorological parameters from surface measurements available at LAX. Hourly vector averages of wind speed and direction were compiled from raw 5-min average measured values. Figure S1 shows the hourly directional and speed frequency distributions (wind rose) during the modeling period. We then used U.S. EPA’s AERMOD meteorological dispersion model to predict air quality impacts downwind of the airport, assuming two steady-state, volumetric line sources, in cross-section, to represent the emissions from descending aircraft approaching both runways. These two volume line sources were aligned in the same direction as the runways, which closely matched the predominant wind directions shown in Figure S1. One end of each source was placed at ground level on the eastern edge of each corresponding runway to account for the approximately induced downward plume travel from the interacting rotational energy of the vortices, which lowers the effective source positions relative to the actual position of the landing aircraft (Graham and Raper 2006). The other ends of the line sources were located at elevation to match the 3-degree approach angle as shown in Figure S2.
Due to the lack of regulation or standards for particle number, UFP emissions have not been well characterized historically and estimating UFP emission rates from jets involves high uncertainty (Durdina et al. 2017). For this reason, we initially assumed a nominal daily average total emission rate from both sources of . These emissions were then allowed to vary on a relative basis by hour of the day, based on reported flight activity patterns, with nearly all flight activity occurring between 0700 and 2300 hours (7 A.M. and 11 P.M.), as shown in Figure S3 (LAWA 2014).
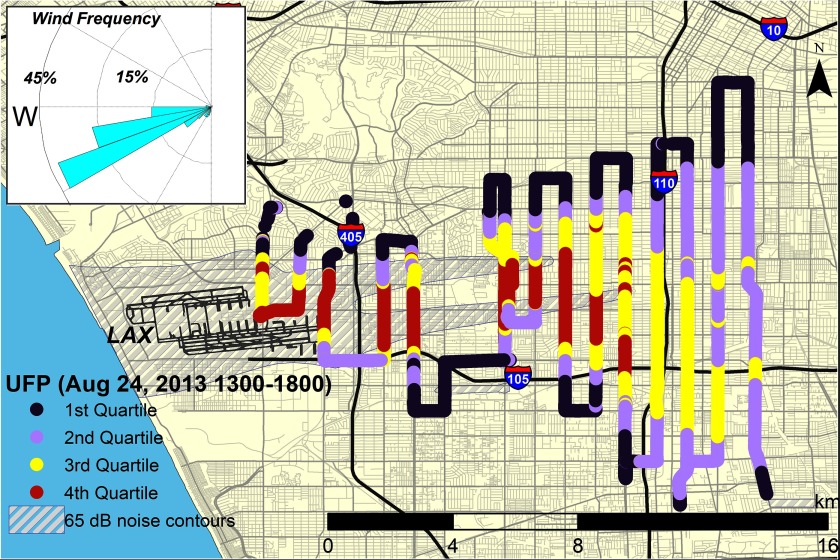
To determine and validate adjustments to this emission rate, we regressed the resulting AERMOD predictions against direct downwind measurements made along the transects shown in Figure S4 on seven days, five in summer and two in winter (Figure 1) (Hudda et al. 2014). The average values for all days along each transect were then compared with the volume line source model relative predictions, based on the nominal emissions rates and scaled to match observed values during the same hourly time periods using a simple linear regression model. We included an intercept in the model to account for any residual background not included in the prior adjustments. Predicted vs. measured values are shown in Figure S5. The model was 0.71 with an root mean square error (RMSE) of 2,300 particles per cc and a mean absolute percentage error of 6%. The intercept was statistically significant with a value of 13,900 [] particles per cc.
Figure 1.
Measured ultrafine particles (UFP) concentrations downwind of Los Angeles International Airport (LAX) on 3 December 2013 with area above average noise in gray. Base layers obtained from USGS.gov (USGS 2019).
For sensitivity tests, we compared results from modeling UFP concentrations from an area source representing the ground-level emissions from the airport runway and tarmac. We also tested a 10-degree angle of ascent (Yim et al. 2013). Neither of these configurations predicted UFP concentrations that were significantly correlated with the observations.
The 3-degree, dual volume line source model was then run for the period January 2008 through December 2016. Average values were computed for each month during that period at the receptor locations shown in Figure S6. We assumed that the meteorology derived from the LAX data applied over the entire modeling region. The monthly activity patterns shown in Figure S7 relative to the overall average were then used to adjust the monthly average model predictions at each receptor location. Particle number concentrations reported here are based on an AERMOD conversion factor of .
Using the UFP dispersion model, we linked average per trimester and per pregnancy period UFP exposures within the buffer to geocoded maternal addresses reported on the birth certificate. Additionally, we evaluated noncircular, ellipsoid exposure buffers with semiminor axes of 10, 12, and and semimajor axes of 22.5, 18.8, and , respectively, to preserve the original exposure buffer area of . These ellipses were aligned with the prevailing daytime wind direction of 263 degrees, the angle at which the runways are oriented.
Covariates
We controlled for concentrations as a ground-level vehicle traffic surrogate for combustion emissions similar to methods used in previous studies (Ritz et al. 2009; Singer et al. 2004). Briefly, with a Land Use Regression (LUR) model we estimated annual exposures for Los Angeles County using data collected over 2 wk from 201 passive air samplers (part number PS-100; Ogawa & Company USA). Final predicted concentration surfaces explained 85% of the variation of measured concentrations. Mothers were assigned the annual average concentrations of the year during which the majority of their pregnancy occurred.
The analysis also included the known PTB risk factors (Campbell et al. 2017; Fuchs et al. 2018; Kyrklund-Blomberg and Cnattingius 1998; Luo et al. 2006; Ruiz et al. 2015) listed in the birth certificates, including parental age; mother’s race/ethnicity [Hispanic (any race), non-Hispanic black, non-Hispanic white, and non-Hispanic Asian and non-Hispanic Other (including Native American and Hawaiian/Pacific Islander); maternal educational attainment; maternal nativity (U.S.- or foreign-born); and maternal smoking (ever/never during pregnancy)].
Thirty-nine noise monitors in the communities surrounding the airport routinely record noise from overhead flights and generate publicly reported community noise equivalent levels (CNELs). These monitors are deployed and managed by the airport authority and are certified by the California Department of Transportation, Division of Aeronautics. Monitors are located up to north and south and east of the airport boundary, roughly following the usual approach pattern to LAX. Almost no monitoring occurs west of the airport because its western edge abuts the Pacific Ocean (LAWA 2015). Monitored data are the input into the Federal Aviation Administration’s Integrated Noise Model to generate estimated annual noise impact areas due to aircraft activity. The areas affected above an annual average of , the acceptable CNEL limit for individuals living near an airport, according to the California Department of Transportation (California Department of Transportation Division of Aeronautics) and the day–night average noise level threshold used by the Federal Aviation Administration (FAA) to make policy assessments (FAA 2018) are shown in Figure S8. We included CNEL values at each mother’s residence as a dichotomous variable, either above or below .
To further control for confounding by neighborhood socioeconomic status (nSES), we also adjusted for a composite score of nSES based on a principal component analysis selection of seven indicator variables generated from United States census data. Mothers were assigned a quintile nSES index (, ), based on the ranking of their census tract’s median household income, median rent, median house value, percent living 200% below poverty level, percent of blue-collar workers, percent unemployed, and education index (Yost et al. 2001).
Statistical Analysis
We assessed the association between quartiles of residential location-specific aircraft UFP concentrations during pregnancy and PTB using logistic regression (SAS version 9.3; SAS Institute, Inc.). Quartiles were defined by cut points at 5,300 particles/cc, 8,600 particles/cc, and 14,600 particles/cc. These cut points remained consistent across all models. In covariate-adjusted models, we estimated the odds ratio (OR) for PTB in each quartile of UFP exposure relative to the lowest quartile. To evaluate the role of maternal nativity and race/ethnicity, we conducted jointly stratified analyses because the health outcomes of some recent immigrant groups may differ from native-born individuals with the same race/ethnicity (Hoggatt et al. 2012; McDonald and Kennedy 2004). We also evaluated a continuous measure of UFP, examining a linear, per-IQR increase in relative UFP exposure and sensitivity analyses using a mixture of exposure quantiles. Additionally, we analyzed the association between quartiles of UFP exposure and very PTB () using an adjusted logistic regression model.
Further sensitivity analyses included stratifying by nSES (quintiles) and educational attainment (high school education or less, some college to bachelor’s degree, or more than a bachelor’s degree) to estimate the association between UFP and PTB in population subgroups. Using monthly estimates of UFP exposure, per-trimester exposure estimates were generated. Per-trimester exposure models were modeled to assess potential periods of greater sensitivity to pollutants during gestation. Pearson correlations across trimesters and with other pollutants, nSES, and UFP exposures were also analyzed. To isolate aircraft movements at LAX from activities at a nearby municipal airport [Santa Monica Municipal Airport (SMO)], we additionally excluded in some sensitivity analyses residents living within a and buffer distance from the SMO airport. Subjects for whom any covariate data were missing were excluded from analyses.
Results
Demographic factors by PTB status for the infants born within a radius of LAX between 2008 and 2016 are shown in Table 1. Most mothers were Hispanic with a high school degree or less. Mean age at delivery was 29 y (). PTB occurred in 8.7% of all births and was more common in black and Hispanic mothers and mothers with less education and among male births. Demographic factors are also shown by quartile of UFP exposure in Table S1. In higher quartiles of exposure, mothers tended to be younger, more frequently Hispanic or black, and had less education than mothers in lower exposure quartiles. The mean UFP exposure concentration was 12,000 particles/cc (), with a minimum of 2,500 particles/cc and maximum of 120,000 particles/cc. The IQR was 9,200 particles/cc.
Table 1.
Maternal and infant demographics by gestational age.
| Total | () | () |
|---|---|---|
| Gestational age, mean weeks (SD), | 34.5 (2.8) | 39.7 (1.4) |
| Birth weight, mean grams (SD), | 2,598 (752) | 3,348 (444) |
| Parity, mean children (SD), | 2.3 (2.3) | 2.1 (2.4) |
| Quintile of nSES Index,a mean (SD), | 1.9 (1.3) | 2.2 (1.4) |
| Infant sex [ (%)] | ||
| Male | 8,282 (54.7) | 80,774 (50.8) |
| Female | 6,850 (45.3) | 78,278 (49.2) |
| Missing () | 2 | 0 |
| Maternal age [ (%)] | ||
| 1,322 (8.7) | 11,658 (7.3) | |
| 20–24 | 2,980 (19.7) | 30,731 (19.3) |
| 25–29 | 3,440 (22.7) | 38,339 (24.1) |
| 30–34 | 3,702 (24.5) | 43,372 (27.3) |
| 3,690 (24.4) | 34,952 (22.0) | |
| Missing () | 1 | 2 |
| Maternal Race [ (%)] | ||
| White | 1,842 (12.2) | 29,749 (18.7) |
| Black | 3,027 (20.0) | 22,487 (14.1) |
| Hispanic | 8,997 (59.5) | 89,592 (56.3) |
| Asian | 916 (6.1) | 13,670 (8.6) |
| Others | 352 (2.3) | 3,554 (2.2) |
| Missing () | 216 | 2,526 |
| Maternal education [ (%)] | ||
| High school graduate or less | 8,909 (58.9) | 81,542 (51.3) |
| Some college to bachelor’s degree | 4,928 (32.6) | 57,883 (36.4) |
| More than a bachelor’s degree | 1,297 (8.6) | 19,627 (12.3) |
| Missing () | 435 | 4,584 |
| Maternal nativity [ (%)] | ||
| U.S.-born | 10,802 (71.4) | 111,087 (70.0) |
| Foreign-born | 4,332 (28.6) | 47,965 (30.2) |
| LUR modeled exposure, mean ppb (SD), | 23.8 (2.6) | 23.6 (2.7) |
| High noise at residence [ (%)] | ||
| CNEL | 779 (5.2) | 6,685 (4.2) |
| CNEL | 14,355 (94.8) | 152,367 (95.8) |
| Cigarette smoking [ (%)] | ||
| Ever during pregnancy | 157 (1.0) | 923 (0.6) |
| Never during pregnancy | 14,977 (99.0) | 158,129 (99.4) |
| Missing | 1,686 | 11,681 |
Note: Data are complete unless otherwise indicated. CNEL, community noise equivalent level; dB, decibels; LUR, land use regression.
nSES measured as a composite index of seven indicator variables based on U.S. census data at the census tract level.
In unadjusted logistic regression models, the highest quartile of pregnancy average UFP exposure was associated with a 1.32 OR of giving birth to a preterm baby in comparison with the lowest quartile. Controlling for demographic factors as well as traffic pollution and noise, the OR for PTB in the upper quartile of UFP exposure was 1.14 (95% CI: 1.08, 1.20) (Table 2), with the odds increasing monotonically with each increase in exposure quartile. When we stratified by maternal race/ethnicity and nativity when comparing the fourth quartile of UFP exposure to the first, we found the strongest associations among foreign-born women, particularly for Asian and Hispanic women (Table S2). By contrast, stronger associations were found in U.S.-born black women relative to foreign-born black women, though the sample size among black women was markedly smaller (Table S3). Exposure to the highest quartile of traffic-related () relative to the lowest () was associated with an OR of 1.15 (95% CI: 1.09, 1.22). Additionally, exposure to noise CNEL was associated with an OR of 1.10 (95% CI: 1.01, 1.19) (Table 2). Of note, maternal exposure with high airport noise was only moderately correlated with aircraft-origin UFPs (Pearson correlation coefficient ) and weakly inversely correlated with traffic-related () (Table S4).
Table 2.
Adjusted odds ratios (ORs) [95% confidence intervals (CIs)] of preterm birth.a
| Variable | 95% CI | |||
|---|---|---|---|---|
| Unadjusted model | Adjusted model 1b | Adjusted model 2c | Adjusted model 3d | |
| UFP | ||||
| Quartile 1 () | Ref | Ref | Ref | Ref |
| Quartile 2 (5,340–8,600 particles/cc) | 1.17 (1.11, 1.22) | 1.01 (0.96, 1.07) | 1.03 (0.98, 1.08) | 1.03 (0.98, 1.08) |
| Quartile 3 (8,600–14,600 particles/cc) | 1.27 (1.22, 1.33) | 1.05 (1.00, 1.10) | 1.08 (1.02, 1.13) | 1.08 (1.02, 1.13) |
| Quartile 4 () | 1.32 (1.27, 1.39) | 1.11 (1.05, 1.16) | 1.16 (1.10, 1.22) | 1.14 (1.08, 1.20) |
| Quartile 1 () | — | — | Ref | Ref |
| Quartile 2 () | — | — | 1.10 (1.05, 1.15) | 1.10 (1.05, 1.16) |
| Quartile 3 () | — | — | 1.10 (1.05, 1.16) | 1.11 (1.05, 1.15) |
| Quartile 4 () | — | — | 1.15 (1.09, 1.21) | 1.15 (1.09, 1.22) |
| Exposed to noise CNEL | — | — | — | 1.10 (1.01, 1.19) |
Note: —, Data not available; CNEL, community noise equivalent level; dB, decibels; ppb, parts per billion; Ref, reference.
PTB .
Adjusted for maternal age, maternal educational attainment, SES, maternal race, and cigarette smoking. Educational attainment was recorded in 9 ordinal categories: No formal education, 8th grade or less, 9th grade through 12th grade with no diploma, high school graduate or GED, some college credit with no degree, associate’s degree, bachelor’s degree, master’s degree, doctorate or professional degree.
Adjusted for all variables in Adjusted Model 1 and .
Adjusted for all variables in Adjusted Model 2 and airport noise.
In additional sensitivity analyses using different quantiles of UFP exposure, the results remained consistent (Table S5). A monotonic dose–response of increasing risk of PTB with increasing exposure to UFP was evident for all exposure categorizations we examined. For UFPs using a continuous variable we estimated the OR of PTB to be 1.04 (95% CI: 1.02, 1.06) per IQR increase in UFP. When we explored exposure to UFP at different times during pregnancy, we found that the per-trimester effect estimates were nearly identical to those for the entire pregnancy (Table S6). However, the UFP averages for trimesters and the whole pregnancy were highly correlated (Table S3); hence, our ability to detect differences between trimester-specific exposures was diminished. When we modified the aspect ratio of the exposure area, generating an ellipsoid buffer, we observed only minor changes in effect estimates (Table S7).
We also conducted stratified analyses to assess potential effect measure modifiers. When we stratified by quintile of nSES, we observed a modest increase in the odds of PTB associated with UFP exposure with decreasing nSES when comparing the fourth quartile of UFP exposure to the first, though estimates were not behaving strictly monotonically (Table S8). We also found nSES and UFP exposures to be negatively correlated [Pearson correlation coefficient: , (Table S9)]; i.e., mothers living in areas with the lowest nSES tended to be exposed to higher levels of aircraft-origin UFPs relative to women living in areas with higher nSES. Stratifying by education suggested an increased risk of PTB due to UFP exposure in all quartiles of exposure among women with less than a high school education (OR 1.19, 95% CI: 1.10, 1.28). On the other hand, for those with some college education, the estimated effect sizes for UFP exposure were smaller (OR 1.10, 95% CI: 1.00, 1.21) (Table S10).
We also estimated the association between UFPs and very PTB (), and the OR for the highest quartile (1.13) of exposure was very similar to the overall estimate, but the CI was wider (95% CI: 0.98, 1.31) (Table S11). When excluding mothers living close to a nearby municipal airport (SMO), overall effect estimates changed only slightly. Specifically, after excluding mothers living within and of SMO, the ORs for the highest quartile of UFP exposure relative to the lowest quartile increased to 1.15 (95% CI: 1.09, 1.21) and 1.18 (95% CI: 1.11, 1.25), respectively (Table S12).
Discussion
We found in utero exposures to jet-specific UFP emissions, estimated using a spatially validated AERMOD dispersion model, to be associated with increased odds of PTB among mothers living within of LAX. This is the first study to report such associations for an adverse birth outcome among residents living in the incoming flight paths and downwind of a major airport. We also found associations between PTB and vehicular traffic-related air pollution , modeling with an LUR as reported previously in a study of births between 1997 and 2006 in Los Angeles (Wu et al. 2009), but the effect sizes were slightly weaker than those we estimated for LAX UFPs. These results suggest an association between traffic-related air pollution and PTB that has been previously reported for other population-based birth outcome studies (Ji et al. 2019; Ritz et al. 2007, 2000; Wilhelm et al. 2011) and was consistent across different categorizations of the UFP exposure variable.
Our results suggest that exposure to aircraft-origin UFP may be independently associated with PTB after accounting for coexposure to traffic-related air pollution and aircraft noise. Whether noise was included or excluded from models, the effect estimates for UFP exposure remained the same. Although previous research found some evidence for an etiological role of noise in PTB (Argys et al. 2019), other research has not consistently detected this link (Ristovska et al. 2014). In our cohort, although exposure to airport-related noise does appear to be associated with an increased risk for PTB for those living very close to the airport (Figure S8), aircraft-origin UFPs were associated with PTB in an area downwind of the LAX airfield that is much larger than the one affected by high noise levels. In fact, in 2010, more than 1.9 million residents lived within the buffer we studied (U.S. Census Bureau 2010). For comparison, aircraft activity at LAX has been previously estimated to generate an average particle number concentration equivalent to 280 km–790 km of freeway emissions, which represents emissions equivalent to 19%–53% of the total freeway length in all of Los Angeles County (Hudda et al. 2014).
An important aspect of this study is that it distinguishes aircraft-origin UFPs from traffic-origin UFPs. A previous study in California implicated vehicle traffic UFPs in PTBs from 2000 to 2008 (Laurent et al. 2016). However, the CALINE4 traffic model used to estimate exposures did not include the contributions of aircraft-origin UFP. In comparison with the sharp UFP gradients resulting from vehicle traffic that are limited to a few hundred meters from roadways, UFP emissions from jets, particularly landing planes, show unusually large impact areas with relatively little small-scale spatial variability (e.g., almost no change over hundreds of meters) (Hudda and Fruin 2016). This characteristic allowed for more accurate exposure estimates compared to with ground-source UFP concentrations from roadways, which typically have sharp downwind concentrations gradients (Kaur et al. 2006).
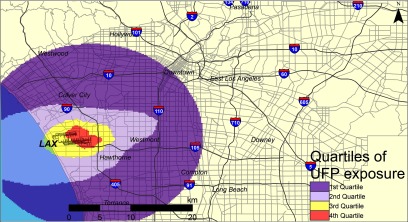
There is a relatively rapid downward transport of these aircraft-origin UFPs and thus very little time for physical aging of these UFP particles due to coagulation with larger particles. This downward transport is due to a combination of large-scale daytime, convective velocities of up to 1 m/s that are enhanced by local-scale jet wingtip vortices that can extend vertically downward for several hundred meters at similar, superimposed velocities (Graham and Raper 2006). This combination results in plumes from descending aircraft reaching ground level in approximately a few minutes near the airport and up to 15–20 min at downwind from the airport. At these plume transport times, UFPs emitted by jet engines have a characteristic coagulation half-life of about an hour, assuming that they are emitted into a background aerosol with a number concentration of and count mean diameter of (Seinfeld and Pandis 2006). These half-lives depend on the number concentration and size of the surrounding background particles. However, the smaller UFPs that are transported downward from this elevated source spend even less time interacting with potentially higher concentrations of existing particles that occur at ground level, such as those found on or near major roadways. It is therefore not surprising that the typical size of these UFPs in the downwind footprint shown in Figure 2 are typically very small , indicating minimal coagulation losses (Hudda and Fruin 2016; Hudda et al. 2014; Riley et al. 2016; Shirmohammadi et al. 2016). Furthermore, due to the consistency of daytime onshore breeze directions at LAX, the location of elevated, ground-level UFPs concentrations downwind and to the east of LAX is very stable (Hudda and Fruin 2016; Hudda et al. 2014), producing relatively large contrasts in concentrations between residences inside the area of impact in comparison with those located outside.
Figure 2.
Estimated UFP exposure quartiles from AERMOD results. Base layers obtained from USGS.gov (USGS 2019).
An interesting finding is that the effect estimates for UFPs and PTB were somewhat stronger among foreign-born Hispanic and Asian women, possibly because those women are less likely to be employed during pregnancy in comparison with U.S.-born mothers (von Ehrenstein et al. 2013, 2014); thus, they could have spent more time at their residences during pregnancy, which may have resulted in greater exposure and/or reduced exposure misclassification, which could possibly explain the stronger effect sizes we estimated. Alternatively, the foreign-born women may have been at increased risk for PTB due to decreased utilization of prenatal care (Heaman et al. 2013)—possibly driven by several barriers, including language comprehension (Edwards 1994) and access to health care (Gagnon 2004)—or working in physically demanding occupations that adversely affect birth outcomes (von Ehrenstein et al. 2013).
Several aspects of UFP could contribute to the estimated effects on PTB. Inhaled UFPs penetrate the lung mucosa and can translocate to other parts of the body because their size facilitates movement across cell barriers, entrance into the bloodstream, and relocation to distal tissues (Baldauf et al. 2016), including the placenta (Bové et al. 2019). Additionally, UFPs escape the usual clearance mechanisms by phagocytes, which remove larger particles like and (Li et al. 2016). Murine cell–based experiments have linked UFP exposures with an increased oxidative stress response and inflammation (Li et al. 2003; Nel et al. 2001), mechanisms that have been implicated in PTB (Ferguson et al. 2015; Romero et al. 1991; Vadillo-Ortega et al. 2014). For example, at concentrations occurring in ambient Los Angeles air, one experiment found large increases in measures of oxidative stress, such as heme oxygenase expression, intracellular glutathione depletion, and reactive oxygen species generation (via dithiothreitol assay) in exposure to quasi-UFP size fractions () in comparison with fine or coarse PM fractions (Li et al. 2003). In humans, intrauterine inflammation is common in PTB (Üstün et al. 2001), and PTB is associated with an unusually large presence of proinflammatory immune cells and tumor necrosis factor-α (Romero et al. 1989).
Another important physiochemical property of UFPs that may increase their pathogenic potential is their large particle surface area. Depending on their sources, they may carry adsorbed or condensed air toxics, such as polycyclic aromatic hydrocarbons (PAHs) (Sioutas et al. 2005). In fact, UFPs are responsible for up to 30% of the PAHs deposited in the lung (Kawanaka et al. 2009). UFP plumes from aircraft emissions are highly enriched in particle-bound PAHs (Kinsey 2009) and an order of magnitude higher than background particle-bound PAH levels reported up to downwind of LAX (Hudda et al. 2014). Other research in the Los Angeles area has found that UFPs contain much higher PAH content than fine () particles and coarse () particles (Li et al. 2003). With respect to aircraft-based PAHs, a study of emissions within the plane loading area of a major airport showed that the particle-bound PAHs were composed of high-molecular-weight compounds with high toxicity (Lai et al. 2013). Altogether, there is evidence suggesting that UFPs, especially those of aircraft-origin, carry pathogenic PAHs linked to inflammation (den Hartigh et al. 2010; Schober et al. 2007) and PTB (Wilhelm et al. 2011).
Another source of aviation emissions located in the study area is the general aviation airport SMO ( north of LAX), but the aircraft using this airfield are smaller, using Avgas, which contains tetraethyl lead (ASTM International 2017). In utero lead exposure is a known cause of adverse birth outcomes (Andrews et al. 1994). To account for potential lead exposures in areas near this municipal airport, we excluded births within a 2- and distance from SMO, but this exclusion did not change our effect estimates for UFPs.
Our study has several strengths. The UFP dispersion model allowed us to assess exposure profiles in a large population encompassing tens of thousands of births. Due to the daytime wind directions at LAX being very consistent throughout the entire year, the locations at which UFP exposures occur downwind of LAX are quite stable (Hudda and Fruin 2016; Hudda et al. 2014). Such consistency allows for accurate exposure estimation at residences across the years due to improved AERMOD exposure model generalizability. Further, the outcome data were derived from birth records, reported and recorded in a uniform manner in California.
Another strength of our study is its public health importance. UFP exposures have received limited research attention, and this project addresses impacts of aircraft movements that could have profound public health impacts, given the ever-growing demand for air travel. In the United States, more than 40,000 daily flights (FAA 2017) service nearly 400 primary airports (FAA 2013). UFP emissions from these aircraft are spread across large residential areas. For example, in the United States, people live near 89 major airports (i.e., in areas with noise levels). Due to the noise from airports, many of the UFP affected areas are low nSES with especially vulnerable populations. In analyses by nSES, PTB was associated with higher levels of aircraft-origin UFP exposures only in low nSES areas (Table S8). Low nSES communities are overrepresented in housing stock located directly downwind of this highly trafficked airport. In addition, because lower household income has been shown to be inversely correlated with air conditioner use (Malig et al. 2010), the proximity might be magnifying air pollution exposures due to the opening of windows in homes lacking air conditioning, which can result in increased indoor UFP concentrations (Rim et al. 2013). Although we cannot confirm this hypothesis in our data, it is one possible explanation for this observation. Another explanation is increased susceptibility to PTB among low-nSES pregnant women, possibly due to differences in health care access.
This study has some limitations, including a semiecological exposure assessment because we are estimating UFP exposures only at the home address provided on the birth certificate, and we cannot account for time spent by mothers at work, in transit, or at other residences prior to birth. A previous study estimated that 9%–32% of mothers move during their pregnancy (Bell and Belanger 2012). We were not able to adjust for exposure to in our analyses because only a single government-operated monitor is located in the area of interest and does not provide spatial variation in measures. However, our adjustment for LUR modeled , a valid marker for traffic-related air pollution in the region (Su et al. 2009), helped control for spatially distinct traffic-related pollutants that may act as confounders on a fine spatial scale. Future studies of this type would benefit from greater temporal coverage of UFP measurements for dispersion model validation, perhaps via fixed monitors. Finally, our assumption of a constant per-aircraft UFP emission rate did not account for possible changes in relative emission factors over the study period. Unfortunately, adequate information to quantify historical trends for aircraft UFP emission factors is not available.
Conclusion
An increased risk of PTB was estimated with in utero exposure to higher concentrations of aircraft-origin UFPs in women living near LAX. Although in utero air pollution exposure from particulate matter—especially from traffic-related combustion sources—are known risk factors for PTB, our results suggest that emissions from aircraft might play an independent etiological role in adverse birth outcomes. These findings are of great public health concern because UFP exposures downwind of airfields are common and may affect large densely populated residential areas.
Supplementary Material
Acknowledgments
This work was supported by National Institute of Environmental Health Sciences grants 1K25ES019224-01 and 1K25ES019224-01.
References
- Andrews KW, Savitz DA, Hertz-Picciotto I. 1994. Prenatal lead exposure in relation to gestational age and birth weight: a review of epidemiologic studies. Am J Ind Med 26(1):13–32, PMID: 8074121, 10.1002/ajim.4700260103. [DOI] [PubMed] [Google Scholar]
- Argys LM, Averett SL, Yang M. 2019. IZA DP No. 12605: Residential Noise Exposure and Health: Evidence from Aviation Noise and Birth Outcomes. IZA Institute of Labor Economics. http://ftp.iza.org/dp12605.pdf.
- ASTM International. 2017. ASTM D910-17a, Standard Specification for Leaded Aviation Gasolines, 10.1520/D0910-17A. [DOI]
- Baldauf RW, Devlin RB, Gehr P, Giannelli R, Hassett-Sipple B, Jung H, et al. . 2016. Ultrafine particle metrics and research considerations: review of the 2015 UFP Workshop. Int J Environ Res Public Health 13(11):1054, PMID: 27801854, 10.3390/ijerph13111054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell ML, Belanger K. 2012. Review of research on residential mobility during pregnancy: consequences for assessment of prenatal environmental exposures. J Expo Sci Environ Epidemiol 22(5):429–438, PMID: 22617723, 10.1038/jes.2012.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bové H, Bongaerts E, Slenders E, Bijnens EM, Saenen ND, Gyselaers W, et al. . 2019. Ambient black carbon particles reach the fetal side of human placenta. Nat Commun 10(1):3866, PMID: 31530803, 10.1038/s41467-019-11654-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- California Department of Transportation Division of Aeronautics. Noise Standards. vol. 21, https://dot.ca.gov/hq/planning/aeronaut/documents/statenoisestnds.pdf [accessed 21 January 2019].
- Campbell EE, Gilliland J, Dworatzek PDN, De Vrijer B, Penava D, Seabrook JA. 2017. Socioeconomic status and adverse birth outcomes: a population-based Canadian sample. J Biosoc Sci 1–12, PMID: 28270256, 10.1017/S0021932017000062. [DOI] [PubMed] [Google Scholar]
- Carslaw DC, Beevers SD, Ropkins K, Bell MC. 2006. Detecting and quantifying aircraft and other on-airport contributions to ambient nitrogen oxides in the vicinity of a large international airport. Atmos Environ 40(28):5424–5434, 10.1016/j.atmosenv.2006.04.062. [DOI] [Google Scholar]
- den Hartigh LJ, Lamé MW, Ham W, Kleeman MJ, Tablin F, Wilson DW. 2010. Endotoxin and polycyclic aromatic hydrocarbons in ambient fine particulate matter from Fresno, California initiate human monocyte inflammatory responses mediated by reactive oxygen species. Toxicol In Vitro 24(7):1993–2002, PMID: 20801209, 10.1016/j.tiv.2010.08.017. [DOI] [PubMed] [Google Scholar]
- Durdina L, Brem BT, Setyan A, Siegerist F, Rindlisbacher T, Wang J. 2017. Assessment of particle pollution from jetliners: from smoke visibility to nanoparticle counting. Environ Sci Technol 51(6):3534–3541, PMID: 28230356, 10.1021/acs.est.6b05801. [DOI] [PubMed] [Google Scholar]
- Edwards N. 1994. Factors influencing prenatal class attendance among immigrants in Ottawa-Carleton. Can J Public Health 85(4):254–258, PMID: 7987748. [PubMed] [Google Scholar]
- FAA (Federal Aviation Administration). 2017. Air Traffic by the Numbers. https://www.faa.gov/air_traffic/by_the_numbers/ [accessed 21 January 2019].
- FAA. 2013. Commercial Service Airports, based on Calendar Year 2012 Enplanements.
- FAA. 2018. FAA History of Noise. https://www.faa.gov/regulations_policies/policy_guidance/noise/history/ [accessed 23 January 2019].
- Ferguson KK, McElrath TF, Chen Y-H, Loch-Caruso R, Mukherjee B, Meeker JD. 2015. Repeated measures of urinary oxidative stress biomarkers during pregnancy and preterm birth. Am J Obstet Gynecol 212(2):208.e1–8, PMID: 25111586, 10.1016/j.ajog.2014.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuchs F, Monet B, Ducruet T, Chaillet N, Audibert F. 2018. Effect of maternal age on the risk of preterm birth: a large cohort study. PLoS One 13(1):e0191002, PMID: 29385154, 10.1371/journal.pone.0191002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gagnon A. 2004. The Responsiveness of the Canadian Health Care System towards Newcomers. In: Changing Health Care in Canada: The Romanow Papers, vol. 2, 349–388. Forest P-G, Marchildon, GP, Mclntosh T, eds. Toronto, Canada: University of Toronto Press. [Google Scholar]
- Graham A, Raper DW. 2006. Transport to ground of emissions in aircraft wakes. Part I: Processes. Atmos Environ 40(29):5574–5585, 10.1016/j.atmosenv.2006.05.015. [DOI] [Google Scholar]
- Harrison MS, Goldenberg RL. 2016. Global burden of prematurity. Semin Fetal Neonatal Med 21(2):74–79, PMID: 26740166, 10.1016/j.siny.2015.12.007. [DOI] [PubMed] [Google Scholar]
- Heaman M, Bayrampour H, Kingston D, Blondel B, Gissler M, Roth C, et al. . 2013. Migrant women’s utilization of prenatal care: a systematic review. Matern Child Health J 17(5):816–836, PMID: 22714797, 10.1007/s10995-012-1058-z. [DOI] [PubMed] [Google Scholar]
- Hinds W. 1999. Aerosol technology : properties, behavior, and measurement of airborne particles. New York: Wiley. [Google Scholar]
- Hoggatt KJ, Flores M, Solorio R, Wilhelm M, Ritz B. 2012. The “Latina Epidemiologic Paradox” revisited: the role of birthplace and acculturation in predicting infant low birth weight for Latinas in Los Angeles, CA. J Immigr Minor Health 14(5):875–884, PMID: 22160842, 10.1007/s10903-011-9556-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudda N, Fruin SA. 2016. International airport impacts to air quality: size and related properties of large increases in ultrafine particle number concentrations. Environ Sci Technol 50(7):3362–3370, PMID: 26971965, 10.1021/acs.est.5b05313. [DOI] [PubMed] [Google Scholar]
- Hudda N, Gould T, Hartin K, Larson TV, Fruin SA. 2014. Emissions from an international airport increase particle number concentrations 4-fold at 10 km downwind. Environ Sci Technol 48(12):6628–6635, PMID: 24871496, 10.1021/es5001566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudda N, Simon MC, Zamore W, Brugge D, Durant JL. 2016. Aviation emissions impact ambient ultrafine particle concentrations in the greater Boston area. Environ Sci Technol 50(16):8514–8521, PMID: 27490267, 10.1021/acs.est.6b01815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudda N, Simon MC, Zamore W, Durant JL. 2018. Aviation-related impacts on ultrafine particle number concentrations outside and inside residences near an airport. Environ Sci Technol 52(4):1765–1772, PMID: 29411612, 10.1021/acs.est.7b05593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyder A, Lee HJ, Ebisu K, Koutrakis P, Belanger K, Bell ML. 2014. PM2.5 exposure and birth outcomes: use of satellite- and monitor-based data. Epidemiology 25(1):58–67, PMID: 24240652, 10.1097/EDE.0000000000000027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (U.S.). 2007. Preterm Birth: Causes, Consequences, and Prevention. Behrman R and Butler A, eds. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Ji X, Meng X, Liu C, Chen R, Ge Y, Kan L, et al. . 2019. Nitrogen dioxide air pollution and preterm birth in Shanghai, China. Environ Res 169:79–85, PMID: 30423521, 10.1016/j.envres.2018.11.007. [DOI] [PubMed] [Google Scholar]
- Kaur S, Clark RDR, Walsh PT, Arnold SJ, Colvile RN, Nieuwenhuijsen MJ. 2006. Exposure visualisation of ultrafine particle counts in a transport microenvironment. Atmos Environ 40(2):386–398, 10.1016/j.atmosenv.2005.09.047. [DOI] [Google Scholar]
- Kawanaka Y, Tsuchiya Y, Yun S-J, Sakamoto K. 2009. Size distributions of polycyclic aromatic hydrocarbons in the atmosphere and estimation of the contribution of ultrafine particles to their lung deposition. Environ Sci Technol 43(17):6851–6856, PMID: 19764259, 10.1021/es900033u. [DOI] [PubMed] [Google Scholar]
- Keuken MP, Moerman M, Zandveld P, Henzing JS, Hoek G. 2015. Total and size-resolved particle number and black carbon concentrations in urban areas near Schiphol airport (Netherlands). Atmos Environ 104:132–142, 10.1016/j.atmosenv.2015.01.015. [DOI] [Google Scholar]
- Kinsey J. 2009. Characterization of emissions from commercial aircraft engines during the Aircraft Particle Emissions eXperiment (APEX) 1 to 3. Washington, DC: Environmental Protection Agency. http://nepis.epa.gov/Exe/ZyPURL.cgi?Dockey=P1005KRK.txt [accessed 2 April 2019]. [DOI] [PubMed]
- Kyrklund-Blomberg NB, Cnattingius S. 1998. Preterm birth and maternal smoking: risks related to gestational age and onset of delivery. Am J Obstet Gynecol 179(4):1051–1055, PMID: 9790397, 10.1016/s0002-9378(98)70214-5. [DOI] [PubMed] [Google Scholar]
- Lai C-H, Chuang K-Y, Chang J-W. 2013. Characteristics of nano-/ultrafine particle-bound PAHs in ambient air at an international airport. Environ Sci Pollut Res Int 20(3):1772–1780, PMID: 22821344, 10.1007/s11356-012-1083-x. [DOI] [PubMed] [Google Scholar]
- Lamichhane DK, Leem J-H, Lee J-Y, Kim H-C. 2015. A meta-analysis of exposure to particulate matter and adverse birth outcomes. Environ Health Toxicol 30:e2015011, PMID: 26796890, 10.5620/eht.e2015011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurent O, Hu J, Li L, Kleeman MJ, Bartell SM, Cockburn M, et al. . 2016. A statewide nested case–control study of preterm birth and air pollution by source and composition: California, 2001–2008. Environ Health Perspect 124(9):1479–1486, PMID: 26895492, 10.1289/ehp.1510133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LAWA (Los Angeles World Airports). 2014. California State Airports Noise Standards Quarterly Report: Fourth Quarter 2013. Los Angeles, CA: Los Angeles World Airports. https://www.lawa.org/-/media/lawa-web/noise-complaint-quarterly/2013/4q13/4q13-quarterly-report.ashx [accessed 30 January 2019].
- LAWA. 2015. LAX Noise Management Program. Los Angeles, CA: Los Angeles World Airports. https://www.lawa.org/-/media/lawa-web/tenants411/file/lax-noise-brochure.ashx [accessed 9 December 2018].
- Lee P-C, Roberts JM, Catov JM, Talbott EO, Ritz B. 2013. First trimester exposure to ambient air pollution, pregnancy complications and adverse birth outcomes in Allegheny County, PA. Matern Child Health J 17(3):545–555, PMID: 22544506, 10.1007/s10995-012-1028-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li N, Georas S, Alexis N, Fritz P, Xia T, Williams MA, et al. . 2016. A work group report on ultrafine particles (American Academy of Allergy, Asthma & Immunology): why ambient ultrafine and engineered nanoparticles should receive special attention for possible adverse health outcomes in human subjects. J Allergy Clin Immunol 138(2):386–396, PMID: 27130856, 10.1016/j.jaci.2016.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li N, Sioutas C, Cho A, Schmitz D, Misra C, Sempf J, et al. . 2003. Ultrafine particulate pollutants induce oxidative stress and mitochondrial damage. Environ Health Perspect 111(4):455–460, PMID: 12676598, 10.1289/ehp.6000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Z-C, Wilkins R, Kramer MS, Fetal and Infant Health Study Group of the Canadian Perinatal Surveillance System. 2006. Effect of neighbourhood income and maternal education on birth outcomes: a population-based study. CMAJ 174(10):1415–1420, PMID: 16682708, 10.1503/cmaj.051096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maisonet M, Correa A, Misra D, Jaakkola J. 2004. A review of the literature on the effects of ambient air pollution on fetal growth. Environ Res 95(1):106–115, PMID: 15068936, 10.1016/j.envres.2004.01.001. [DOI] [PubMed] [Google Scholar]
- Malig B, Green R, Basu R, Rauch S, Ostro B. 2010. The effects of temperature and use of air conditioning on hospitalizations. Am J Epidemiol 172(9):1053–1061, PMID: 20829270, 10.1093/aje/kwq231. [DOI] [PubMed] [Google Scholar]
- Martin JA, Hamilton BE, Osterman MJK. 2018. Births in the United States, 2017. NCHS Data Brief, PMID: 30156535, 10.1021/acs.jpclett.7b01206. [DOI] [PubMed] [Google Scholar]
- Masiol M, Harrison RM, Vu TV, Beddows D. 2017a. Sources of sub-micrometre particles near a major international airport. Atmos Chem Phys 17(20):12379–12403, 10.5194/acp-17-12379-2017. [DOI] [Google Scholar]
- Masiol M, Hopke PK, Felton HD, Frank BP, Rattigan OV, Wurth MJ, et al. . 2017b. Analysis of major air pollutants and submicron particles in New York City and Long Island. Atmos Environ 148:203–214, 10.1016/j.atmosenv.2016.10.043. [DOI] [Google Scholar]
- McDonald JT, Kennedy S. 2004. Insights into the “healthy immigrant effect”: health status and health service use of immigrants to Canada. Soc Sci Med 59(8):1613–1627, PMID: 15279920, 10.1016/j.socscimed.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Nel AE, Diaz-Sanchez D, Li N. 2001. The role of particulate pollutants in pulmonary inflammation and asthma: evidence for the involvement of organic chemicals and oxidative stress. Curr Opin Pulm Med 7(1):20–26, PMID: 11140402, 10.1097/00063198-200101000-00004. [DOI] [PubMed] [Google Scholar]
- Ponce NA, Hoggatt KJ, Wilhelm M, Ritz BR. 2005. Preterm birth: the interaction of traffic-related air pollution with economic hardship in Los Angeles neighborhoods. Am J Epidemiol 162(2):140–148, PMID: 15972941, 10.1093/aje/kwi173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratliff G, Sequeira C, Waitz I, Ohsfeldt M, Thrasher T, Graham M, et al. . 2009. Aircraft Impacts on Local and Regional Air Quality in the United States. Cambridge, MA: Partnership for AiR Transportation Noise and Emissions Reduction Project; https://web.mit.edu/aeroastro/partner/reports/proj15/proj15finalreport.pdf [accessed 10 December 2018]. [Google Scholar]
- Riley EA, Gould T, Hartin K, Fruin SA, Simpson CD, Yost MG, et al. . 2016. Ultrafine particle size as a tracer for aircraft turbine emissions. Atmos Environ (1994) 139:20–29, PMID: 27795692, 10.1016/j.atmosenv.2016.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rim D, Wallace LA, Persily AK. 2013. Indoor ultrafine particles of outdoor origin: importance of window opening area and fan operation condition. Environ Sci Technol 47(4):1922–1929, PMID: 23384189, 10.1021/es303613e. [DOI] [PubMed] [Google Scholar]
- Ristovska G, Laszlo HE, Hansell AL. 2014. Reproductive outcomes associated with noise exposure—a systematic review of the literature. Int J Environ Res Public Health 11(8):7931–7952, PMID: 25101773, 10.3390/ijerph110807931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritz B, Turner M, Ghosh JK, Qiu J, Jerrett M, Su J, et al. . 2009. Traffic-Related Air Pollution and Asthma in Economically Disadvantaged and High Traffic Density Neighborhoods in Los Angeles County, California. Sacramento, CA: California Air Resources Board. https://ww2.arb.ca.gov/sites/default/files/classic//research/apr/past/04-323.pdf [accessed 1 December 2019].
- Ritz B, Wilhelm M, Hoggatt KJ, Ghosh J. 2007. Ambient air pollution and preterm birth in the environment and pregnancy outcomes study at the University of California, Los Angeles. Am J Epidemiol 166(9):1045–1052, PMID: 17675655, 10.1093/aje/kwm181. [DOI] [PubMed] [Google Scholar]
- Ritz BR, Yu F. 1999. The effect of ambient carbon monoxide on low birth weight among children born in southern California between 1989 and 1993. Environ Health Perspect 107(1):17–25, PMID: 9872713, 10.1289/ehp.9910717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritz BR, Yu F, Chapa G, Fruin S. 2000. Effect of air pollution on preterm birth among children born in Southern California between 1989 and 1993. Epidemiology 11(5):502–511, PMID: 10955401, 10.1097/00001648-200009000-00004. [DOI] [PubMed] [Google Scholar]
- Ritz BR, Yu F, Fruin S, Chapa G, Shaw GM, Harris JA. 2002. Ambient air pollution and risk of birth defects in southern California. Am J Epidemiol 155(1):17–25, PMID: 11772780, 10.1093/aje/155.1.17. [DOI] [PubMed] [Google Scholar]
- Romero R, Manogue KR, Mitchell MD, Wu YK, Oyarzun E, Hobbins JC, et al. . 1989. Infection and labor. IV. Cachectin-tumor necrosis factor in the amniotic fluid of women with intraamniotic infection and preterm labor. Am J Obstet Gynecol 161(2):336–341, PMID: 2764054, 10.1016/0002-9378(89)90515-2. [DOI] [PubMed] [Google Scholar]
- Romero R, Mazor M, Tartakovsky B. 1991. Systemic administration of interleukin-1 induces preterm parturition in mice. Am J Obstet Gynecol 165(4 pt 1):969–971, PMID: 1951564, 10.1016/0002-9378(91)90450-6. [DOI] [PubMed] [Google Scholar]
- Ruiz M, Goldblatt P, Morrison J, Kukla L, Švancara J, Riitta-Järvelin M, et al. . 2015. Mother’s education and the risk of preterm and small for gestational age birth: a DRIVERS meta-analysis of 12 European cohorts. J Epidemiol Community Heal 69(9):826–833, PMID: 25911693, 10.1136/jech-2014-205387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schober W, Lubitz S, Belloni B, Gebauer G, Lintelmann J, Matuschek G, et al. . 2007. Environmental polycyclic aromatic hydrocarbons (PAHs) enhance allergic inflammation by acting on human basophils. Inhal Toxicol 19 (suppl 1):151–156, PMID: 17886062, 10.1080/08958370701496046. [DOI] [PubMed] [Google Scholar]
- Seinfeld JH, Pandis SN. 2006. Atmospheric Chemistry and Physics: From Air Pollution to Climate Change. New York: John Wiley & Sons. Inc. [Google Scholar]
- Shirmohammadi F, Sowlat MH, Hasheminassab S, Saffari A, Ban-Weiss G, Sioutas C. 2016. Emission rates of particle number, mass and black carbon by the Los Angeles International Airport (LAX) and its impact on air quality in Los Angeles. Atmos Environ 151:82–93, 10.1016/j.atmosenv.2016.12.005. [DOI] [Google Scholar]
- Singer BC, Hodgson AT, Hotchi T, Kim JJ. 2004. Passive measurement of nitrogen oxides to assess traffic-related pollutant exposure for the East Bay Children’s Respiratory Health Study. Atmos Environ 38(3): 393–403, 10.1016/j.atmosenv.2003.10.005. [DOI] [Google Scholar]
- Sioutas C, Delfino RJ, Singh M. 2005. Exposure assessment for atmospheric ultrafine particles (UFPs) and implications in epidemiologic research. Environ Health Perspect 113(8):947–955, PMID: 16079062, 10.1289/ehp.7939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Šrám RJ, Binková B, Dejmek J, Bobak M. 2005. Ambient air pollution and pregnancy outcomes: a review of the literature. Environ Health Perspect 113(4):375–382, PMID: 15811825, 10.1289/ehp.6362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stillerman KP, Mattison DR, Giudice LC, Woodruff TJ. 2008. Environmental exposures and adverse pregnancy outcomes: a review of the science. Reprod Sci 15(7):631–650, PMID: 18836129, 10.1177/1933719108322436. [DOI] [PubMed] [Google Scholar]
- Su JG, Jerrett M, Beckerman B. 2009. A distance-decay variable selection strategy for land use regression modeling of ambient air pollution exposures. Sci Total Environ 407(12):3890–3898, PMID: 19304313, 10.1016/j.scitotenv.2009.01.061. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. 2010. Population & Housing Unit Counts–Blocks. Washington, DC: US Census Bureau. https://www.census.gov/geographies/mapping-files/time-series/geo/tiger-data.2010.html [accessed 5 January 2019].
- USGS (United States Geological Survey). 2019. The National Map–Service Endpoints. https://viewer.nationalmap.gov/services/ [accessed 1 February 2019].
- Üstün C, Koçak I, Bariş S, Uzel A, Saltik F. 2001. Subclinical chorioamnionitis as an etiologic factor in preterm deliveries. Int J Gynaecol Obstet 72(2):109–115, PMID: 11166743, 10.1016/s0020-7292(00)00280-0. [DOI] [PubMed] [Google Scholar]
- Vadillo-Ortega F, Osornio-Vargas A, Buxton MA, Sánchez BN, Rojas-Bracho L, Viveros-Alcaráz M, et al. . 2014. Air pollution, inflammation and preterm birth: a potential mechanistic link. Med Hypotheses 82(2):219–224, PMID: 24382337, 10.1016/j.mehy.2013.11.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valotto G, Varin C. 2016. Characterization of hourly NOx atmospheric concentrations near the Venice International Airport with additive semi-parametric statistical models. Atmos Res 167:216–223, 10.1016/j.atmosres.2015.07.023. [DOI] [Google Scholar]
- von Ehrenstein OS, Wilhelm M, Ritz B. 2013. Maternal occupation and term low birth weight in a predominantly Latina population in Los Angeles, California. J Occup Environ Med 55(9):1046–1051, PMID: 23969503, 10.1097/JOM.0b013e31829888fe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Ehrenstein OS, Wilhelm M, Wang A, Ritz BR. 2014. Preterm birth and prenatal maternal occupation: the role of Hispanic ethnicity and nativity in a population-based sample in Los Angeles, California. Am J Public Health 104(suppl 1):S65–72, 10.2105/AJPH.2013.301457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilhelm M, Ghosh JK, Su J. 2011. Traffic-related air toxics and preterm birth: a population-based case-control study in Los Angeles County, California. Environ Health (10):89, PMID: 21981989, 10.1186/1476-069X-10-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilhelm M, Ritz BR. 2005. Local variations in CO and particulate air pollution and adverse birth outcomes in Los Angeles County, California, USA. Environ Health Perspect 113(9):1212–1221, PMID: 16140630, 10.1289/ehp.7751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilhelm M, Ritz BR. 2003. Residential proximity to traffic and adverse birth outcomes in Los Angeles County, California, 1994–1996. Environ Health Perspect 111(2):207–216, PMID: 12573907, 10.1289/ehp.5688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (World Health Organization). 2018. Preterm birth. Geneva, Switzerland: WHO. https://www.who.int/news-room/fact-sheets/detail/preterm-birth [accessed 4 January 2019].
- Wu J, Ren C, Delfino RJ, Chung J, Wilhelm M, Ritz B. 2009. Association between local traffic-generated air pollution and preeclampsia and preterm delivery in the south coast air basin of California. Environ Health Perspect 117(11):1773–1779, PMID: 20049131, 10.1289/ehp.0800334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yim SHL, Stettler MEJ, Barrett S. 2013. Air quality and public health impacts of UK airports. Part II: Impacts and policy assessment. Atmos Environ 67:184–192, 10.1016/j.atmosenv.2012.10.017. [DOI] [Google Scholar]
- Yost K, Perkins C, Cohen R, Morris C, Wright W. 2001. Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control 12(8):703–711, PMID: 11562110, 10.1023/a:1011240019516. [DOI] [PubMed] [Google Scholar]
- Yu KN, Cheung YP, Cheung T, Henry RC. 2004. Identifying the impact of large urban airports on local air quality by nonparametric regression. Atmos Environ 38(27):4501–4507, 10.1016/j.atmosenv.2004.05.034. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.