In 2014, the worst outbreak of Ebola virus disease (EVD) emerged in sub‐Saharan Africa (SSA) causing fear and panic. The outbreak which started in Guinea quickly moved across to Sierra Leone and Liberia. With an average EVD case fatality rate of around 50% (range: 25%‐90%), there were many casualties, and the number of recorded deaths exceeded 11 300 by June 2016. 1 Activities in the affected countries were severely disrupted, with the social and economic burden estimated at US $53.2 billion, the most significant component being attributed to deaths from non‐Ebola causes. 2
The catastrophic consequences of the EVD outbreak were ascribed to a failure of leadership at many levels. 3 The World Health Organization (WHO), for example, admitted that its initial response was slow and insufficient, not aggressive enough, that it suffered from poor coordination, and had significant gaps in its risk communication strategies. 4 However, several other factors contributed to the scale of the EVD outbreak in SSA including weak health systems, the absence of sufficiently trained personnel, limited resources, highly porous international borders, and mistrust of government and health officials. 5 Thus, post‐Ebola discussions generated broad consensus among global health actors regarding the need for greater investment in health systems strengthening to reduce the potential for similar future outbreaks as well as improve response to imminent threats. In particular, the need to train community, laboratory, public health, and clinical personnel, provide infection‐control equipment, supplies, and protocols as well as establish laboratory facilities with high biosafety capabilities, health facilities (including those with safe isolation units) and proper communication systems to effectively deliver important public health messages were highlighted. 6
Today, the world is confronting yet another infectious disease outbreak with the novel coronavirus, COVID‐19 (2019‐nCoV) now declared a global pandemic. More than 169 000 confirmed cases in over 140 countries had been reported resulting in more than 6500 deaths as at 16 March 2020. 7 In China, cities have been sealed off, and the authorities have built an entirely new hospital in Wuhan, where the outbreak emerged. As the virus spreads, Europe has been severely hit and is now considered the “epicenter” of the COVID‐19 epidemic with several of its cities on lockdown.
As of 16 March 2020, 135 confirmed COVID‐19 cases across 24 countries SSA had been reported (Figure 1). 7 These numbers are considerably low when compared with other jurisdictions, although, if anything, the recent EVD outbreak has taught us that within fragile national health systems, things can quickly spiral out of control. While many countries in SSA have instituted screening measures, the focus has been at the ports of entry, with screening targeted at people with a recent travel history to outbreak areas abroad. However, screening travelers for fever has been shown to be largely ineffective, 8 because it is unable to detect people who are in their incubation phase (which could exceed 12 days for COVID‐19). 9 Thus, many cases within communities are likely being missed, and the possibility for widespread infections in SSA could be imminent, mindful of the fact that unlike EVD which required very close contact for transmission, being a viral respiratory disease, COVID‐19 has a higher transmission potential.
Figure 1.
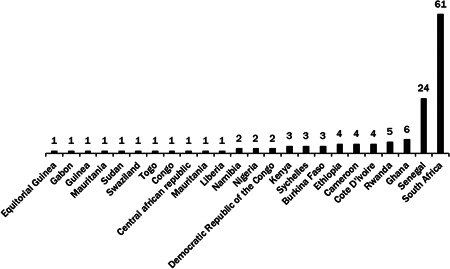
Number of confirmed cases of COVID‐19 in sub‐Saharan African countries as of 16 March 2020 7
Importantly, governments in SSA need to intensify education to improve the public's knowledge about COVID‐19′s transmission dynamics and control. For example, emphasizing basic behavioral changes including frequent and thorough hand washing, covering mouth/nose with a tissue when coughing or sneezing, and crowd avoidance is critical. Moreover, highlighting that medical masks provide little protection to the general public and that hoarding them could lead to price hikes and shortages for health care workers or that there is currently no approved vaccine to prevent COVID‐19 are all essential. Ultimately, the containment of COVID‐19 would require citizen commitment and responsibility besides government interventions.
Overall, strategies adopted need to recognize local sociocultural issues and challenges. For example, measures such as social distancing may be difficult to implement in certain crowded SSA neighborhoods where many generations often cohabit. 10 To achieve the greatest impact, consistent and credible messaging that is coordinated among key traditional and religious leaders, media, and political actors are critical. Furthermore, health officials need to use diverse communication channels to disseminate information about the progress of the outbreak, and the interventions being implemented in a transparent and timely manner.
Data from other regions suggest that a significant proportion of patients infected with COVID‐19 require hospitalization. 11 , 12 , 13 In Italy for example, 9% to 11% of all COVID‐19 patients were admitted into the intensive care unit (ICU). 11 If such trends emerge in SSA, high levels of deaths could occur owing to underdeveloped infrastructure to support critical care delivery. 14 For example, Mato and colleagues, 15 reported that in 2009, there were just eight ICU beds for port Harcourt and its environs in Nigeria, an area with an estimated population of more than 9 million people. A 2015 survey of 21 hospitals in Kenya by Okech et al 16 also found that there were only 130 ICU beds and 204 specialized intensive care nurses, and in Namibia, just 18 ICU beds were present across more than 350 public facilities nationwide in 2019. 17 Thus, governments in SSA need to have clear strategies about how they would deal with COVID‐19 patients needing hospitalization or critical care to avoid disrupting the entire health system which could further increase deaths from other non‐COVID‐19 causes as was noted during the EVD outbreak. Moreover, given the high out‐of‐pocket expenditure in this region—a critical barrier to accessing health care, 18 governments need to outline and inform the public how COVID‐19‐related care is being funded. Importantly, it would be essential for COVID‐19‐related services such as testing, and treatment be provided free to all citizens and these services should ideally be made available nationwide and not only in urban areas so as to improve reporting at health care facilities which could help curb further community transmissions.
Ultimately, robust response from governments in SSA will require the availability and allocation of sufficient funds. The government of Ghana, for example, recently announced a US $100 million fund to cover the expansion of infrastructure, purchase of materials and equipment, and public education. 19 The United Nations has also released US $15 million to help the world's most vulnerable countries fight the outbreak. 20 However, these funds are meager compared to the US where Congress recently approved US $8.3 billion 21 or in Australia where $AUD 2.4 billion has been outlined by the federal government to fight the same outbreak. 22 The WHO and its partners have recently launched a Solidarity Response Fund to support country‐level efforts. 23 Regardless, any response within SSA must consider the potential economic consequences for the residents many of whom are informal (self‐employed) petty traders and whose businesses are already being adversely impacted due to COVID‐19‐related restrictions. Without any proper financial support, such individuals may not adhere to quarantine directives and may continue to engage in social activities or work to cater for their families, which could hamper efforts to contain the virus.
The never‐ending battle between humans and microbes is once again at the full display with COVID‐19 threatening the lives of millions of individuals around the world. The over 1 billion people residing in SSA are particularly vulnerable to the pandemic due to several sociocultural, health care, economic, and political factors. However, governments in this region can act swiftly and implement appropriate strategies to contain the virus and minimize any adverse socioeconomic impacts. Strong political leadership and coordinated efforts are needed to ensure that the calamities of the EVD outbreak are never repeated again.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
RO, AL, and AA contributed to manuscript conception, writing, and revision. All authors approved the final version before submission.
Agyeman AA, Laar A, Ofori‐Asenso R. Will COVID‐19 be a litmus test for post‐Ebola sub‐Saharan Africa? J Med Virol. 2020;92:1373–1375. 10.1002/jmv.25780
REFERENCES
- 1. World Health Organization (WHO) . Ebola virus disease. https://www.who.int/news‐room/fact‐sheets/detail/ebola‐virus‐disease. Accessed 15 March 2020.
- 2. Huber C, Finelli L, Stevens W. The economic and social burden of the 2014 Ebola outbreak in West Africa. J Infect Dis. 2018;218(suppl_5):S698‐S704. [DOI] [PubMed] [Google Scholar]
- 3. Fidler D. Epic failure of Ebola and Global Health Security. Brown J World Aff. 2015;21(2):179‐197. [Google Scholar]
- 4. United Nations . Joint statement on the Ebola response and WHO reforms. https://un.org.au/2015/04/20/joint‐statement‐on‐the‐ebola‐response‐and‐who‐reforms/. Accessed 15 March 2020.
- 5. Coltart CE, Lindsey B, Ghinai I, Johnson AM, Heymann DL. The Ebola outbreak, 2013–2016: old lessons for new epidemics. Philos Trans R Soc Lond B Biol Sci. 2017;372(1721):20160297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gostin L. Ebola: towards an International Health Systems Fund. Lancet. 2014;384(9951):e49‐e51. [DOI] [PubMed] [Google Scholar]
- 7. Coronavirus COVID‐19 Global Cases . https://www.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6. Accessed 16 March 2020.
- 8. Gostic KM, Kucharski AJ, Lloyd‐Smith JO. Effectiveness of traveller screening for emerging pathogens is shaped by epidemiology and natural history of infection. eLife. 2015;4:e05564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID‐19) from publicly reported confirmed cases: estimation and application. [published online ahead of print March 10, 2020]. Ann Intern Med. 10.7326/M20-0504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Odimegwu C, Ndagurwa P, Singini MG, Baruwa OJ. Cohabitation in sub‐Saharan Africa: a regional analysis. South Afr J Demogr. 2018;18(1):111‐170. [Google Scholar]
- 11. Remuzzi A, Remuzzi G. COVID‐19 and Italy: what next? [published online ahead of print March 13, 2020]. Lancet. pii: S0140‐6736(20)30627‐9. 10.1016/S0140-6736(20)30627-9 [DOI] [Google Scholar]
- 12. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID‐19) outbreak in China. [published online ahead of print February 24, 2020]. JAMA. 10.1001/jama.2020.2648 [DOI] [PubMed] [Google Scholar]
- 13. Guan WJ, Ni ZY, Hu Y, Liang WH. Clinical characteristics of coronavirus disease 2019 in China. [published online ahead of print February 28, 2020]. N Engl J Med. 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Okafor UV. Challenges in critical care services in sub‐Saharan Africa: perspectives from Nigeria. Indian J Crit Care Med. 2009;13(1):25‐27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mato CN, Onwuchekwa AC, Aggo AT. Pattern of admissions to the University of Port Harcourt Teaching Hospital intensive care unit—a 10‐year analysis. South Afr J Crit Care. 2009;25(1):10‐15. [Google Scholar]
- 16. Okech UK, Chokwe T, Mung'ayi V. The operational setup of intensive care units in a low income country in East Africa. East Afr Med J. 2015;92(2):72‐80. [Google Scholar]
- 17. The Namibian . Only 18 ICU beds available in the public sector. https://www.namibian.com.na/189697/archive‐read/Only‐18‐ICU‐beds‐in‐public‐health‐sector. Accessed 16 March 2020.
- 18. EY . Global analysis of health insurance in Africa. https://www.ey.com/Publication/vwLUAssets/EY‐global‐analysis‐of‐health‐insurance‐in‐sub‐saharan‐africa/%24File/ey‐global‐analysis‐of‐health‐insurance‐in‐sub‐saharan‐africa.pdf. Accessed 16 March 2020.
- 19. Ministry of health Ghana . “$100 Million Provided To Enhance Coronavirus Preparedness And Response Plan”—President Akufo‐Addo. http://www.moh.gov.gh/100‐million‐provided‐to‐enhance‐coronavirus‐preparedness‐and‐response‐plan‐president‐akufo‐addo/. Accessed 16 March 2020.
- 20. World Health Organization . UN releases US $15 million to help vulnerable countries battle the spread of the coronavirus. https://www.who.int/news‐room/detail/01‐03‐2020‐un‐releases‐us‐15‐million‐to‐help‐vulnerable‐countries‐battle‐the‐spread‐of‐the‐coronavirus. Accessed 16 March 2020.
- 21. The Wall Street Journal . House passes $8.3 billion to battle coronavirus. https://www.wsj.com/articles/congress‐reaches‐8‐billion‐deal‐to‐combat‐coronavirus‐11583343193. Accessed 16 March 2020.
- 22. Prime Minister of Australia . $2.4 billion health plan to fight COVID. https://www.pm.gov.au/media/24‐billion‐health‐plan‐fight‐covid‐19. Accessed 16 May 2020.
- 23. World Health Organization . WHO, UN Foundation and partners launch first‐of‐its‐kind COVID‐19 Solidarity Response Fund. https://www.who.int/news‐room/detail/13‐03‐2020‐who‐un‐foundation‐and‐partners‐launch‐first‐of‐its‐kind‐covid‐19‐solidarity‐response‐fund. Accessed 16 May 2020.


