Summary
In response to the recent novel coronavirus outbreak originating in Wuhan, Hubei province, China, observations concerning novel coronavirus mortality are of urgent public health importance. The present work presents the first review of the fatal novel coronavirus cases in China. Clinical data of fatal cases published by the Chinese Government were studied. As of 2 February 2020, the clinical data of 46 fatal cases were identified. The case fatality rate was significantly higher in Hubei province than the rest of China. While 67% of all deceased patients were male, gender was unlikely to be associated with mortality. Diabetes was likely to be associated with mortality. There is, however, not yet sufficient evidence to support the association between hypertension and mortality as similar prevalence of hypertension was also observed in the Hubei population.
Keywords: mortality, novel coronavirus, Wuhan pneumonia
1. INTRODUCTION
A series of viral pneumonia cases were confirmed in Wuhan, Hubei province, China in December 2019. A new coronavirus was identified and named by the World Health Organization first as 2019‐nCoV then SARS‐CoV‐2 as the cause of the disease COVID‐19. While the pathogenesis and aetiology of SARS‐CoV‐2 infection is still not completely known, it has been observed that it is genetically similar to SARS‐CoV and MERS‐CoV1 and that the incubation time is between 1 and 14 days.2 Unlike other human coronaviruses, some patients had low‐grade fever or were even asymptomatic yet remained infectious. Recently, snakes have been suggested as the natural reservoirs of SARS‐CoV‐2, assuming that the Huanan Seafood Wholesale Market was the origin of the virus.3
Fatal cases of COVID‐19 were first reported in an announcement by the Health Commission of Hubei province on 11 January 2020, claiming no evidence of human‐to‐human transmission.4 However, it was later confirmed that some patients did not have a history of exposure of the Huanan Seafood Wholesale Market. Cases outside of Hubei were first confirmed on 20 January 2020. As of 2 February 2020, over 17 000 cases were confirmed in China with a hospital fatality rate of 2.1% whereas in Hubei province was 3.1% significantly above the rest of China (Figure 1, data from the NHC).
Figure 1.
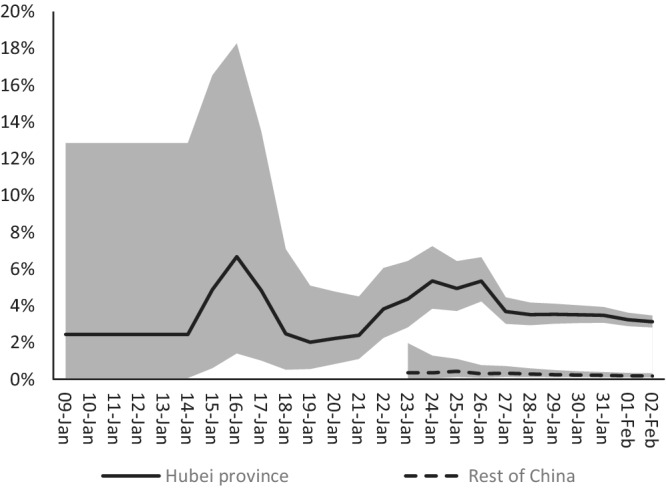
Trends of hospital fatality rates in Hubei province and the rest of China with 95% CI
Most fatal cases were reported in China with very limited clinical data available. In this context, the present study reviewed publicly available data, aiming to provide health professionals and authorities with useful observations concerning mortality. Given the lack of data from a control group, the present work focuses on clarifying fatal cases.
2. METHODS AND MATERIALS
Only materials officially released by the Chinese health authorities and municipal offices were considered. Therefore, a search was performed on the official web pages of the Chinese health authorities and municipal offices for individual level clinical data. There were no particular research terms. However, a full‐text search was performed on sections concerning the recent COVID‐19 epidemic. These sections were largely titled “Latest news,” “Current situation of novel coronavirus pneumonia” or alike. Only individual fatal cases associated with SARS‐CoV‐2 infection were included in the present work if the age or gender of the deceased patient was stated. Both official documents and press conferences were considered.
The following data were abstracted: gender, age, time from symptom onset to hospital admission, time from hospital admission to death, medical history and first symptoms.
2.1. Statistical analysis
For each of the measure studied, a confidence interval for the central tendency was calculated (eg, proportion for male, mean for age). The computation was done in a spreadsheet, Microsoft Office Excel version 2016. A regression model was estimated by regressing the time from hospital admission to death on other variables. The computation was done with the software R and the adjusted R 2 was used for the model selection criterion. Moreover, different functional forms were attempted to ensure normally distributed residuals free from autocorrelation and heteroskedasticity.
3. RESULTS
Forty‐six fatal cases were identified and included in the study including 39 cases in Hubei,5, 6, 7 one in Chongqing,8 two in Henan,9 two in Heilongjiang,10 one in Hebei11 and one in Sichuan.12 Of the seven cases outside Hubei, three had a travel history to Wuhan. Demographic and common clinical characteristics are illustrated in Table 1. The average age was 70.6 years (n = 45, 95% CI 52.0‐80.5) with no significant difference between men and women (t test P = .80). Eighty‐four percent of all deceased patients were of age 60 or above. Men accounted for 67.4% (95% CI 52.0%‐80.5%) of all deceased patients.
Table 1.
Demographic and clinical characteristics of deceased patients
| N | % | 95% CI | |
|---|---|---|---|
| Gender (male) | 46 | 67.4 | 52.0, 80.5 |
| Age (mean) | 45 | 70.6 | 67.0, 74.3 |
| Date of hospitalisation (median, range) | 45 | 14 January 2020 | 26 November 2019, 29 January 2020 |
| Time from first symptom onset to hospital admission (days, mean) | 33 | 6.2 | 5.1, 7.3 |
| Time from hospital admission to death (days, median, IQR) | 45 | 8.0 | 5.0, 12.0 |
| First symptoms | |||
| Fever | 29/44 | 65.9 | 50.1, 79.5 |
| Cough | 27/44 | 61.4 | 45.5, 75.6 |
| Dyspnoea | 12/44 | 27.3 | 15.0, 42.8 |
| Weakness | 8/44 | 18.2 | 8.2, 32.7 |
| Chest pain/discomfort | 6/44 | 13.6 | 5.2, 27.4 |
| Any comorbidity | 29/46 | 63.0 | 47.5, 76.8 |
| Diabetes | 11/42 | 26.2 | 13.9, 42.0 |
| Hypertension | 17/42 | 40.5 | 25.6, 56.7 |
| Cardiovascular and cerebrovascular disease | 8/43 | 23.3 | 11.8, 38.6 |
| Pulmonary disease | 7/43 | 16.3 | 6.8, 30.7 |
While the time from first symptom onset to hospital admission was normally distributed with mean 6.2 days, the time from hospital admission to death was log‐normally distributed (with mean 11 days and median 5 days), as suggested by the Jarque‐Bera normality test (P = .56) on the log‐transformed data. Therefore, the log‐transformed time from hospital admission to death was regressed in the model. Based on the adjusted R 2, the time from symptom onset to hospital admission, cardiovascular and cerebrovascular comorbidities, and age were selected as the independent variables (Table 2). With the exception of cardiovascular and cerebrovascular comorbidities, all other variables are significant at 5% level. The signs of the coefficients are reasonable as the time from hospitalisation to death was inversely related to age and the time from symptom onset to hospitalisation. The statistical significance of time from symptom onset to hospital suggests the need of timely hospitalisation. In fact, the coefficient of time from symptom onset to hospital admission means that, for any two identical patients who will eventually expire with hospital admission 1 day apart, the expected time from hospital admission to death of the patient with later hospital admission is 8.5% shorter than that of the other patient, all else being equal.
Table 2.
Regressing the log‐transformed time from hospital admission to death
| Dependent variable | Log(time from hospital admission to death) | |||
|---|---|---|---|---|
| Coefficients | 95% CI | P | Percentage change in time from hospital admission resulted from a one‐unit change in the independent variable | |
| Constant | 4.471 | 2.788, 6.153 | 0.000 | |
| Time from symptom onset to hospital admission (days) | −0.089 | −0.170, −0.009 | 0.031 | −8.549 |
| Age (years) | −0.026 | −0.048, −0.005 | 0.018 | −2.600 |
| Cardiovascular and cerebrovascular comorbidities | −0.600 | −1.233, 0.033 | 0.062 | −45.134 |
| R 2 | 0.327 | |||
Although a patient was admitted to the hospital for palpitation on 26 November 2019, it is important to note that palpitation was not a common symptom of COVID‐19 infection. Common first symptoms included fever (65.9%), cough (61.4%) and dyspnoea (27.3%). Hypertension and diabetes were the most common comorbidities, accounting for 40.5% and 26.2% of 42 cases, respectively. Despite the prevalence of pneumonia in patients infected with COVID‐19, only 16.3% (n = 43, 95% CI 6.8%‐30.7%) and 23.3% (n = 43, 95% CI 11.8%‐38.6%) of all deceased patients had pulmonary, and cardiovascular and cerebrovascular comorbidities, respectively. Chronic bronchitis (15.6%) and coronary heart disease (13.3%) were the most common. Some clinical findings were also reported in some cases with ground‐glass opacity commonly found on CT (100% for cases reporting CT results). Respiratory failure and bradycardia were observed in almost all cases immediately before death.
4. DISCUSSION
Since SARS‐CoV‐2 can cause lethal infections, an analysis of fatal cases is a public health priority. The present study clarifies fatal cases with details available in public records during the COVID‐19 epidemic in China as of 2 February 2020. A total of 46 fatal cases in six different provinces were identified.
It is not surprising that old age is associated with mortality as 84% of all deceased patients were of age 60 or above. While men accounted for 67.4% of all cases, gender was unlikely to be associated with mortality due to the previous observation that most of the infected patients were male.13
Not surprisingly, fever (65.9%, 95% CI 50.1%‐79.5%) and cough (61.4%, 95% CI 45.5%‐75.6%) remained the most common symptoms and were unlikely to be associated with death. However, the proportion of deceased patients with fever was lower than the previously reported >90%14 for all infected patients. There is however not sufficient evidence to show that fatality was associated with fever. Although a small proportion (27.3%) of all deceased patients were reported to have dyspnoea, it is possible that the proportion of surviving patients having dyspnoea is even lower. It has recently been suggested that dyspnoea was more commonly observed in patients requiring intensive care (ICU).15
Twenty‐nine of the 46 deceased patients had comorbidities (63.0%, 95% CI 47.5%‐76.8%), with hypertension (40.5%, 95% CI 25.6%‐56.7%) and diabetes (26.2%, 95% CI 13.9%‐42.0%) being the most common. While there is no data available from a control group, a chronic disease prevalence study in the Hubei population may shed light on understanding the relationship between comorbidities and COVID‐19 mortality. The most recent prevalence study16 in hypertension and diabetes in Hubei province indicated that 30.8% (95% CI 28.2%‐33.5%) of the population aged 30 or above accounted for hypertension whereas diabetes accounted for 5.6% (95% CI 4.3%‐7.0%). Therefore, the significant difference in the proportion of diabetes between the deceased patients (26.2%) and Hubei population (5.6%) suggested that diabetes might be associated with mortality. In contrast, there is not yet sufficient evidence to suggest that hypertension was associated with increased risk of mortality.
Although cardiovascular, cerebrovascular and pulmonary disease only accounted for small proportion of deceased patients, the results of the regression model suggested that cardiovascular and cerebrovascular disease were inversely correlated to the time from hospitalisation to death, suggested the possible role in mortality.
The significantly higher mortality rate in Hubei might be due to the delay of hospitalisation as implied by the average time of 6.2 days from first symptom onset to hospital admission. Most of the cases included in the study dated between December 2019 and mid‐January 2020, prior to the Chinese government's announcement of the public health concern about Wuhan pneumonia as well as possible human‐to‐human transmission. Coupled with the widely known influenza season in Wuhan around the Lunar New Year, pneumonia was mistaken for flu and therefore patients were not aware of the need of hospitalisation.
The present study has some limitations. First, the sample size is relatively small. As of 2 February 2020, 361 deaths have been reported in China, meaning that the fatal cases included in the study accounted for only 13%. As a result, findings of statistical tests and confidence intervals should be interpreted carefully. For instance, pulmonary and cardiovascular comorbidities were likely risk factors for mortality, albeit not statistically significant. Second, a control group should be included for study to verify the mortality risk factors identified in the study. The hospital mortality rate reported in the present study only considered hospitalised cases. It has been reported by the media that some patients were not hospitalised due to the lack of resources. Consequently, the actual case fatality rate might be much higher than the hospital fatality rate. Finally, the data studied were obtained from the official pages of the Chinese health authorities. It is possible that other cases were made public in other ways.
CONFLICT OF INTEREST
The author declares no conflicts of interest.
Leung C. Clinical features of deaths in the novel coronavirus epidemic in China. Rev Med Virol. 2020;30:e2103. 10.1002/rmv.2103
REFERENCES
- 1. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727‐733. 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. National Health Committee of the PRC Government . State Council Information Office Press Conference. http://www.nhc.gov.cn/xwzb/webcontroller.do?titleSeq=11209&gecstype=1. Accessed February 3, 2020.
- 3. Ji W, Wang W, Zhao X, Zai J, Li X. Homologous recombination within the spike glycoprotein of the newly identified coronavirus may boost cross‐species transmission from snake to human. J Med Virol. 2020;92:433‐440. 10.1002/jmv.25682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. National Health Committee of the PRC Government . Wuhan Municipal Health Commission's report on viral pneumonia with unknown etiology. http://www.nhc.gov.cn/xcs/yqtb/202001/1beb46f061704372b7ca41ef3e682229.shtml. Accessed February 3, 2020.
- 5. Health Commission of Hubei Province . Hubei Province Health Commission's report on pneumonia of new coronavirus infection, 2020. http://wjw.hubei.gov.cn/fbjd/dtyw/202001/t20200124_2014626.shtml. Accessed February 3, 2020.
- 6. Health Commission of Hubei Province . Hubei Province Health Commission's report on pneumonia of new coronavirus infection, 2020. http://wjw.hubei.gov.cn/fbjd/dtyw/202001/t20200125_2014854.shtml. Accessed February 3, 2020.
- 7. National Health Committee of the PRC Government . Epidemic situation of the new coronavirus infection on January 23. http://www.nhc.gov.cn/xcs/yqtb/202001/5d19a4f6d3154b9fae328918ed2e3c8a.shtml. Accessed February 3, 2020.
- 8. Information Office of Chongqing Municipal People's Government . Seventh routine news briefing on pneumonia prevention and control of new coronavirus infection. http://cq.cqnews.net/jrzb2/col607342.htm. Accessed February 3, 2020.
- 9. Information Office of Henan Provincial People's Government . Press conference on the new coronavirus epidemic prevention and control. http://www.ha.xinhuanet.com/news/2020-01/31/c_1125515584.htm. Accessed February 3, 2020.
- 10. Government of the People's Republic of China . Heilongjiang: open and transparent to the public and the initiative to fight the epidemic. http://www.gov.cn/xinwen/2020-02/01/content_5473540.htm. Accessed February 3, 2020.
- 11. Health Commission of Hebei Province . The second case of new coronavirus pneumonia confirmed in our province. http://www.hebwst.gov.cn/index.do?id=394918&templet=content&cid=45. Accessed February 3, 2020.
- 12. Chengdu Municipal Health Commission . Thirteen new coronavirus pneumonia cases in Chengdu. http://cdwjw.chengdu.gov.cn/cdwjw/gzdt/2020-01/30/content_516b4576ecc74698b88344d133dd211e.shtml. Accessed February 3, 2020.
- 13. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497‐506. 10.1016/s0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hui DS, Azhar EI, Madani TA, et al. The continuing 2019‐nCoV epidemic threat of novel coronaviruses to global health—the latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis. 2020;91:264‐266. 10.1016/j.ijid.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus‐infected pneumonia in Wuhan, China. JAMA. 2020. 10.1001/jama.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yu CH, Yuan RX, Bao JZ, Zhang QJ. Risk factors for hypertension and diabetes among floating population in Hubei Province: a cross‐section survey. Chin J Evidence‐Based Med. 2016;16(8):891‐896. 10.7507/1672-2531.20160138. [DOI] [Google Scholar]


