Abstract
Objective
This study aimed to assess the presence of novel coronavirus in tears and conjunctival secretions of SARS–CoV‐2‐infected patients.
Methods
A prospective interventional case series study was performed, and 30 confirmed novel coronavirus pneumonia (NCP) patients were selected at the First Affiliated Hospital of Zhejiang University from 26 January 2020 to 9 February 2020. At an interval of 2 to 3 days, tear and conjunctival secretions were collected twice with disposable sampling swabs for reverse‐transcription polymerase chain reaction (RT‐PCR) assay.
Results
Twenty‐one common‐type and nine severe‐type NCP patients were enrolled. Two samples of tear and conjunctival secretions were obtained from the only one patient with conjunctivitis yielded positive RT‐PCR results. Fifty‐eight samples from other patents were all negative.
Conclusion
We speculate that SARS‐CoV‐2 may be detected in the tears and conjunctival secretions in NCP patients with conjunctivitis.
Keywords: coronavirus, horizontal transmission, infection
Highlights
SARS‐CoV‐2 may be detected in the tears and conjunctival secretions in NCP patients with conjunctivitis.
SARS‐CoV‐2 was not detected in the conjunctival sac of NCP patients without conjunctivitis.
The possibility of eye infection and the ocular route as a potential infection source should be considered and further examined, and scientific protection should be carried out.
1. INTRODUCTION
In December 2019, 41 cases of unexplained pneumonia were clustered in Wuhan, Hubei Province, China. Most of the infected people were confirmed to be related to the South China Seafood Market. On 7 January 2020, the Chinese Center for Disease Control and Prevention isolated and confirmed this pathogen as a novel type of coronavirus through a throat swab. This coronavirus was then named 2019‐nCoV by the World Health Organization (WHO). 1 The origin of the virus remains unknown, and the virus‐host is suspected to be a species of bat. 2 On 25 January 2020, the WHO confirmed that the virus was spread via human‐to‐human transmission and family‐aggregated infections and is less contagious to healthcare professionals, unlike severe acute respiratory syndrome coronavirus (SARS‐CoV) and the Middle East respiratory syndrome‐related coronavirus. 3 On 31 January 2020, the WHO characterized the outbreak as a public health emergency of international concern. 4 At the close of day (on 18 February 2020 at 24:00:00), the cumulative number of infected people worldwide was 73 332, and the cumulative number of infected people in China was 72 528. The virus had spread to 25 other countries globally, with 1873 deaths worldwide. 5 At present, the mortality rate in China is about 2.58%, and the number of infected and dead people continues to increase. On 11 February 2020, the WHO officially named infection due to the virus as coronavirus disease 2019 (COVID‐19) 5 and the Coronavirus Study Group of the International Committee on Taxonomy of Viruses named 2019‐nCoV severe acute respiratory syndrome‐related coronavirus 2, or SARS‐CoV‐2. 6 At present, COVID‐19 poses a huge threat to China and the world. COVID‐19 is highly infectious and transmitted mainly through respiratory droplets and contact with infected persons. The possibility of feco‐oral and aerosol transmission remains to be further studied. 7 In 2004, some researchers found that the tears of SARS patients tested positive for viral nucleic acid, some patients only showed positive results with tear samples, 8 and the chromosome of SARS‐CoV‐2 was 82% similar to that of SARS‐CoV. 9 A previous study reported the case of a clinician who was infected while working with only his eyes unprotected. 10 Lu et al 11 reported that the disease can be transmitted through the mucous membranes, including the conjunctiva. There have been many case reports in which many ophthalmologists were found to be infected through routine diagnosis and treatment. 11 Considering that the virus is present in the body fluids of patients, tear fluid is a type of body fluid, and SARS‐CoV‐2 is similar to SARS‐CoV, it is speculated that there may be a risk of tear and conjunctival transmission. Therefore, this is a focus of the current research to understand whether COVID‐19 is transmitted via other routes and reduce further spread of the epidemic.
In the present study, the tear and conjunctival secretions of patients diagnosed with the novel coronavirus were collected for viral culture and reverse‐transcription polymerase chain reaction (RT‐PCR) assay, attempting to elucidate the presence of novel coronaviruses in tears and conjunctival secretions of SARS–CoV‐2‐infected patients, and provide evidence for further understanding the transmission route of this disease.
2. METHODS
A prospective interventional case series study was designed. We included cases of confirmed novel coronavirus pneumonia (NCP) patients at the First Affiliated Hospital of Zhejiang University from January 26, 2020 to February 9, 2020. The diagnostic criteria were (a) real‐time RT‐PCR assay of respiratory or blood specimens yielded positive results for the novel coronavirus nucleic acid and (b) computerized tomography lung imaging findings were consistent with viral pneumonia. The common‐type diagnostic criteria were the diagnosed patients exclude the severe‐type criteria. The severe‐type diagnostic criteria were (a) respiratory distress (respiratory rate, ≥30 cycles per minute), (b) oxygen saturation 93% or below or arterial partial pressure of oxygen (PaO2)/oxygen concentration FiO2 lesser than or equal to 300 mm Hg in the resting state, (c) respiratory failure requiring mechanical ventilation, (d) shock, and (e) other forms of organ failure requiring monitoring and treatment at the intensive care unit. 12
The study protocol was approved by the Ethics Committee of the First Affiliated Hospital of Zhejiang University School of Medicine, and all the included patients provided written informed consent themselves in advance.
We used the conjunctival swab technique (Figure 1) to collect tears and conjunctival secretions from patients. We opened the lower eyelid of each patient and used a disposable sampling swab to wipe the conjunctiva of the lower eyelid fornix of the patient's eyes without anesthesia. Then, we placed one side of the head of the sampling swab into the sample preservation solution of the disposable virus sample tube, broke off the end of the swab along the red scale, and closed the cap of the virus sampling tube. Each specimen was stored in a 4°C refrigerator and then sent to the laboratory of the First Affiliated Hospital of Zhejiang University. RT‐PCR assays were performed at the State Key Laboratory for Diagnosis and Treatment of Infectious Diseases. To avoid cross‐infection, gloves were changed after collecting each sample. At the time of collection of each sample, the patient's current temperature was recorded and a sputum sample obtained, and the sputum sample was also sent to the laboratory for examination. Two samples were taken from each patient, at intervals of 2 to 3 days. Before collecting the first sample, we recorded the time of onset of symptoms and how and when the antiviral drug was used for each patient.
Figure 1.
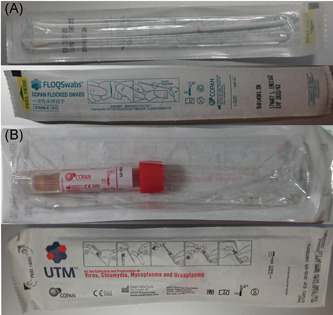
Conjunctival swab technique used to collect tears and conjunctival secretions. A, Conjunctival swabs; B, universal transport medium with stationary liquid inside
RT‐PCR protocol:
-
1.
The collected specimen was shaken for 30 seconds. We pipetted 1 to 2 mL of the specimen and stored it in an Eppendorf tube.
-
2.
The tube was then centrifuged at 12 000 r/min for 5 minutes and 300 µL of the supernatant was pipetted and added to the prepared deep well plate. Then, we added 20 µL of proteinase K and 6 µL of settling agent to extract the nucleic acid. The extraction was completed after about 22 minutes. Then, the nucleic acid was stored in a new Eppendorf tube.
-
3.
We prepared eight‐strip PCR tubes, added 20 µL of the mixed reaction solution (2019 Novel Coronavirus Nucleic Acid Detection Kit; Shanghai Berger Medical Technology Co Ltd), added 5 µL of the extracted nucleic acid, covered it, and ran the PCR reaction using the Roche LightCycler® 480 (Roche Diagnostics GmbH, Mannheim, Germany). After instantaneous centrifugation for 40 cycles, the PCR was completed in about 85 minutes; thereafter, we checked the amplification curves to judge whether the results were negative or positive.
3. RESULTS
Altogether, 21 patients with common‐type and 9 patients with severe‐type were included, with an average age of 54.50 ± 14.17 years and a male/female ratio of 7/3. By the time of first collection of tear and conjunctival secretions, the mean time of onset was 7.33 ± 3.82 days. The average body temperature of the patients was 37.09°C ± 0.69°C at the time of sampling. Details of the characteristics of the study participants are provided in Table 1.
Table 1.
Summary of patient characteristics
| Case | Sex | Age, y | Disease time, d | Sputum RT‐PCR (on admission) | Conjunctivitis | Severity scales | Sputum RT‐PCR | Conjunctival secretion RT‐PCR | Body temperature, °C | Interval time, d | Sputum RT‐PCR | Conjunctival secretion RT‐PCR | Body temperature, °C |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 46 | 8 | Positive | – | Common | Positive | Negative | 37.4 | 3 | Positive | Negative | 37.6 |
| 2 | M | 62 | 10 | Positive | – | Common | Positive | Negative | 36.4 | 3 | Positive | Negative | 36.2 |
| 3 | F | 63 | 5 | Positive | – | Common | Positive | Negative | 37.9 | 3 | Positive | Negative | 37.3 |
| 4 | F | 30 | 8 | Positive | – | Common | Positive | Negative | 37.4 | 3 | Positive | Negative | 36.5 |
| 5 | F | 45 | 14 | Positive | – | Common | Positive | Negative | 37.8 | 3 | Negative | Negative | 36.7 |
| 6 | M | 62 | 16 | Positive | – | Common | Positive | Negative | 36.5 | 3 | Positive | Negative | 36.6 |
| 7 | M | 50 | 11 | Positive | – | Common | Positive | Negative | 36.8 | 3 | Positive | Negative | 36.5 |
| 8 | F | 38 | 6 | Positive | – | Common | Positive | Negative | 37.3 | 3 | Positive | Negative | 37 |
| 9 | M | 30 | 4 | Positive | – | Common | Positive | Negative | 37 | 3 | Positive | Negative | 39.5 |
| 10 | F | 53 | 3 | Positive | – | Common | Positive | Negative | 38 | 3 | Positive | Negative | 37.4 |
| 11 | M | 51 | 7 | Positive | – | Common | Positive | Negative | 36.8 | 2 | Positive | Ngative | 37.1 |
| 12 | M | 70 | 6 | Positive | – | Common | Positive | Negative | 37.8 | 2 | Positive | Negative | 36.7 |
| 13 | F | 65 | 6 | Positive | – | Common | Positive | Negative | 36.9 | 2 | Positive | Negative | 37 |
| 14 | M | 51 | 8 | Positive | – | Common | Positive | Negative | 36.7 | 2 | Positive | Negative | 36.5 |
| 15 | F | 45 | 14 | Positive | – | Common | Positive | Negative | 37 | 2 | Positive | Negative | 36.6 |
| 16 | F | 64 | 7 | Positive | – | Common | Positive | Negative | 38.8 | 2 | Positive | Negative | 36.7 |
| 17 | M | 13 | 6 | Positive | – | Common | Positive | Negative | 36 | 2 | Positive | Negative | 36.2 |
| 18 | M | 55 | 10 | Positive | – | Common | Positive | Negative | 36.7 | 2 | Positive | Negative | 36.7 |
| 19 | M | 48 | 7 | Positive | – | Common | Positive | Negative | 36.7 | 2 | Negative | Negative | 36.5 |
| 20 | M | 57 | 2 | Positive | – | Common | Positive | Negative | 37.9 | 2 | Positive | Negative | 36.8 |
| 21 | M | 53 | 3 | Positive | + | Common | Positive | Positive | 36.2 | 2 | Positive | Positive | 36.5 |
| 22 | M | 60 | 1 | Positive | – | Severe | Positive | Negative | 37.3 | 2 | Negative | Negative | 37.6 |
| 23 | M | 72 | 5 | Positive | – | Severe | Positive | Negative | 36.1 | 2 | Positive | Negative | 36.4 |
| 24 | M | 51 | 8 | Positive | – | Severe | Positive | Negative | 38.2 | 2 | Positive | Negative | 37.1 |
| 25 | M | 83 | 3 | Positive | – | Severe | Positive | Negative | 36.4 | 2 | Positive | Negative | 36.5 |
| 26 | M | 74 | 12 | Positive | – | Severe | Positive | Negative | 36.7 | 2 | Positive | Negative | 36.9 |
| 27 | F | 65 | 7 | Positive | – | Severe | Positive | Negative | 36.4 | 2 | Positive | Negative | 36.9 |
| 28 | M | 62 | 11 | Positive | – | Severe | Positive | Negative | 36.4 | 2 | Positive | Negative | 37.9 |
| 29 | M | 51 | 11 | Positive | − | Severe | Negative | Negative | 37.7 | 2 | Negative | Negative | 37.2 |
| 30 | M | 66 | 1 | Positive | − | Severe | Positive | Negative | 37.6 | 2 | Positive | Negative | 37.8 |
| M: 21, F: 9 | 54.50 ± 14.17 | 7.33 ± 3.82 | +: 30, −: 0 | +:1, −:29 | S: 9, C: 21 | +: 29, −: 1 | +: 1, −: 29 | 37.09 ± 0.69 | 2.3 ± 0.5 | +: 26, −: 4 | +: 1, −: 29 | 36.96 ± 0.65 |
Abbreviation: RT‐PCR, reverse‐transcription polymerase chain reaction.
Two conjunctival swab samples from the only one common‐type patients with conjunctivitis (patient No. 21) yielded positive RT‐PCR results and his sputum samples were also positive. Fifty‐eight conjunctival swab samples from 20 common‐type patients and 9 severe‐type patients were all negative.
4. DISCUSSION
Currently, it is difficult to screen for NCP. Some patients have no obvious fever or respiratory manifestations, or even obvious symptoms in the early stages of the disease. 13 During clinical diagnosis and treatment, particularly at the outpatient clinic, it is difficult to quickly screen patients with early‐stage disease or carriers of the virus. According to recent reports, a large number of ophthalmologists involved in the diagnosis and treatment of the disease on a daily basis accidentally acquired NCP. Thus, many doctors suspect that it is related to contact with tears or conjunctival secretions of patients. 11 In the study of this small sample, we used conjunctival test paper to obtain tears and conjunctival secretions of 30 patients for standard RT‐PCR assay. Only one patient with conjunctivitis found viral RNA in his tear fluid and conjunctival secretion twice. The conjunctivitis was characterized by viral conjunctivitis with conjunctival congestion and aqueous secretion. The patient had no severe fever or respiratory symptoms when we collected his specimens. And the course of disease was in the early stage for only 3 days.
No viral RNA was detected in the tear fluid and conjunctival secretions of the severe or common‐type patients without conjunctivitis. While taking the tear fluid sample for testing, we obtained sputum samples from patients as control samples; 55 of the 60 sputum samples yielded positive results. This, to some extent, indicated that the tear and conjunctival secretions of patients without conjunctivitis were not an infectious route for SARS‐CoV‐2. At present, the transmission route of the novel coronavirus remains unclear, and many scholars believe that it may be transmitted through aerosols. 14 However, the most commonly used noncontact tonometer for ophthalmologic examination sprays a gas during the examination, which produces a large amount of aerosol in the local area. Moreover, aerosols may be concentrated in the local air for a long time, and general alcohol wipe disinfection is ineffective, causing great panic in the field of ophthalmology. 15 According to the results of this study, no virus particles were detected in tear and conjunctival secretions in patients without conjunctivitis. Therefore, current routine disinfection can prevent the spread of the virus; noncontact tonometer, ultrasound biomicroscopy, corneal confocal microscope, and others do not theoretically cause cross‐infection. The low abundance of the virus in tear and conjunctival secretions does not eliminate the risk of transmission through conjunctival tissue. As ophthalmologists come into contact with patients at a close‐range during the examination, the saliva of infected patients may still cause infection among medical staff through conjunctival tissue; thus, goggles are still necessary protective measures.
RT‐PCR is an effective technique for detecting viral nucleic acid. 16 , 17 Due to its high sensitivity and specificity, this method has the advantages of simplicity, convenience, and efficiency. Some scholars have found that RT‐PCR is effective for diagnosing novel coronavirus through meta‐analysis, is significantly better than smear‐dyeing inspection and culture identification, and it has become the gold standard for the diagnosis of coronavirus infections. However, there are inevitably many false positive and false negative results, which are often caused by sample contamination and damage to genetic material. 18 In 2003, some studies reported on the detection of virus particles in conjunctival secretions among SARS patients. 19 Researchers in Hong Kong obtained conjunctival secretions and conjunctival cells from 17 confirmed cases and tested them via viral RT‐PCR; the results were all negative. Researchers in Singapore also tested conjunctival secretions obtained from 34 highly suspected cases via RT‐PCR assay and found that three of the patients had positive results, although their pharyngeal secretions yielded negative results. Of course, the Singaporean researchers also mentioned the possibility of sample contamination during sampling, but due to the shortcomings of RT‐PCR technology, the existence of false negatives could not be ruled out. 8 On the basis of the results of our research, we collected tear and conjunctival secretions twice at an interval of 2 to 3 days and the results showed good consistency. Therefore, we were sure that SARS‐CoV‐2 existed in tears and conjunctival secretions in NCP patients with conjunctivitis. For patients without conjunctivitis, we detected no virus in tears and conjunctival secretions indicating that it is not a common route of its transmission. Nevertheless, the risk of transmission could not be completely eliminated.
The present study assessed the tears and conjunctival secretions in SARS‐CoV‐2‐infected patients. The results showed that the virus existed in the patients' tears and conjunctival secretions with conjunctivitis and there was no virus in the patients' conjunctival sac without conjunctivitis. However, this study had several limitations. First, the included sample size was relatively small. Simultaneously, although the samples were collected by the professional ophthalmologist (JHX), the collected tear and conjunctival secretions were limited, so sample concentration might be insufficient for RT‐PCR detection of the virus. Therefore, the possibility of virus particles in tear and conjunctival secretions in NCP patients without conjunctivitis cannot be completely ruled out. Second, only one patient enrolled got conjunctivitis and the virus was detected from his conjunctival secretion. However, the virus was not successfully isolated and cultured in the conjunctival secretion of the patient. We cannot tell whether all NCP patients with viral conjunctivitis exist with the virus in their conjunctival sac and whether the virus causes conjunctivitis. In addition, most patients in this study received antiviral treatment before sampling. Although sputum samples were also tested for comparison, the effect of drug treatment on the results could not be excluded. Therefore, further large‐sample and more comprehensive studies are needed to evaluate the role of novel coronaviruses in the eyes.
5. CONCLUSION
We speculate that SARS‐CoV‐2 may be detected in the tears and conjunctival secretions in NCP patients with conjunctivitis. Further high‐volume studies are warranted to evaluate this issue.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
JHX took part in sample collection. JT and ML took part in data collection and interpretation. YS and DG designed the study, analysis and interpretation of the data, and wrote the manuscript.
Xia J, Tong J, Liu M, Shen Y, Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS‐CoV‐2 infection. J Med Virol. 2020;92:589–594. 10.1002/jmv.25725
Contributor Information
Ye Shen, Email: idrshen@zju.edu.cn.
Dongyu Guo, Email: guodongyu666@sina.com.
REFERENCES
- 1. Lu H, Stratton CW, Tang YW. Outbreak of pneumonia of unknown etiology In Wuhan, China: the mystery and the miracle. J Med Virol. 2020;92:401‐402. 10.1002/jmv.25678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Zhang L, Shen FM, Chen F, Lin Z. Origin and evolution of the 2019 novel coronavirus. Clin Infect Dis. 2020:ciaa112. 10.1093/cid/ciaa112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization (WHO) . Novel coronavirus (2019‐nCoV) situation report—3 (23 January 2020). Geneva, Switzerland: World Health Organization; 2020. https://www.who.int/docs/default‐source/coronaviruse/situation‐reports/20200123‐sitrep‐3‐2019‐ncov.pdf?sfvrsn=d6d23643_8 [Google Scholar]
- 4. World Health Organization (WHO) . Statement on the Second Meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019‐nCoV). Geneva, Switzerland: World Health Organization; 2020. https://www.who.int/news‐room/detail/30‐01‐2020‐statement‐on‐the‐second‐meeting‐of‐the‐international‐health‐regulations [Google Scholar]
- 5. World Health Organization (WHO) . Novel Coronavirus (2019‐nCoV) Situation Report—29 (18 February 2020). Geneva, Switzerland: World Health Organization; 2020. https://www.who.int/docs/default‐source/coronaviruse/situation‐reports/20200218‐sitrep‐29‐covid‐19.pdf?sfvrsn=6262de9e_2 [Google Scholar]
- 6. Enserink M. Update: ‘A bit chaotic.’ Christening of new coronavirus and its disease name create confusion. sciencemag. 2020. https://www.sciencemag.org/news/2020/02/bit‐chaotic‐christening‐new‐coronavirus‐and‐its‐disease‐name‐create‐confusion [Google Scholar]
- 7.General Office of National Health Committee. Office of State Administration of Traditional Chinese Medicine. Notice on the issuance of a programme for the diagnosis and treatment of novel coronavirus (2019‐nCoV) infected pneumonia (trial 4th ed.) (In Chinese) 2020. https://bgs.satcm.gov.cn/zhengcewenjian/2020‐01‐28/12576.html. Accessed January 18, 2020.
- 8. Loon S‐C, Teoh SCB, Oon LLE, et al. The severe acute respiratory syndrome coronavirus in tears. Br J Ophthalmol. 2004;88(7):861‐863. 10.1136/bjo.2003.035931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chan JF‐W, Kok K‐H, Zhu Z, et al. Genomic characterization of the 2019 novel human‐pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerg Microbes Infect. 2020;9(1):221‐236. 10.1080/22221751.2020.1719902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dai X. Peking University Hospital Wang Guangfa disclosed treatment status on Weibo and suspected infection without wearing goggles. Beijing News, 24 January 2020. http://www.bjnews.com.cn/news/2020/01/23/678189.html. Accessed January 23, 2020
- 11. Lu CW, Liu XF, Jia ZF. 2019‐nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395:e39. 10.1016/S0140-6736(20)30313-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.General Office of National Health Committee. Office of State Administration of Traditional Chinese Medicine. Notice on the issuance of a programme for the diagnosis and treatment of novel coronavirus (2019‐nCoV) infected pneumonia (trial 5th ed.) (In Chinese) 2020. https://bgs.satcm.gov.cn/zhengcewenjian/2020‐02‐06/12848.html. Accessed February 6, 2020.
- 13. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497‐506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Schwartz DA, Graham AL. Potential maternal and infant outcomes from (Wuhan) coronavirus 2019‐nCoV infecting pregnant women: lessons from SARS, MERS, and other human coronavirus infections. Viruses. 2020;12(2):E194. 10.3390/v12020194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lian KY, Napper G, Stapleton FJ, Kiely PM. Infection control guidelines for optometrists 2016. Clin Exp Optom. 2017;100(4):341‐356. 10.1111/cxo.12544 [DOI] [PubMed] [Google Scholar]
- 16. Corman VM, Landt O, Kaiser M, et al. Detection of 2019 novel coronavirus (2019‐nCoV) by real‐time RT‐PCR. Euro Surveill. 2020;25(3). 10.2807/1560-7917.ES.2020.25.3.2000045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507‐513. 10.1016/S0140-6736(20)30211-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lin C, Ye R, Xia YL. A meta‐analysis to evaluate the effectiveness of real‐time PCR for diagnosing novel coronavirus infections. Genet Mol Res. 2015;14(4):15634‐15641. 10.4238/2015 [DOI] [PubMed] [Google Scholar]
- 19. Chan WM, Yuen KS, Fan DS, Lam DS, Chan PK, Sung JJ. Tears and conjunctival scrapings for coronavirus in patients with SARS. Br J Ophthalmol. 2004;88(7):968‐969. 10.1136/bjo.2003.039461 [DOI] [PMC free article] [PubMed] [Google Scholar]


