Abstract
Lung ultrasound (LU) has rapidly become a tool for assessment of patients stricken by the novel coronavirus 2019 (COVID‐19). Over the past two and a half months (January, February, and first half of March 2020) we have used this modality for identification of lung involvement along with pulmonary severity in patients with suspected or documented COVID‐19 infection. Use of LU has helped us in clinical decision making and reduced the use of both chest x‐rays and computed tomography (CT).
Keywords: COVID‐19, interstitial syndrome, lung ultrasound
1. LUNG ULTRASOUND
During this ongoing battle against the novel COVID‐19, LU has quickly been recognized as a tool for diagnosis and monitoring of lung involvement severity. 1
A normal LU demonstrates what are termed A lines. These are a repetition of the pleural line at the same distance from skin to the pleural line. This is indicative of air below the pleural line, corresponding to the parietal pleura. Lines may be complete or partial (Figure 1, Movie S1).
Figure 1.
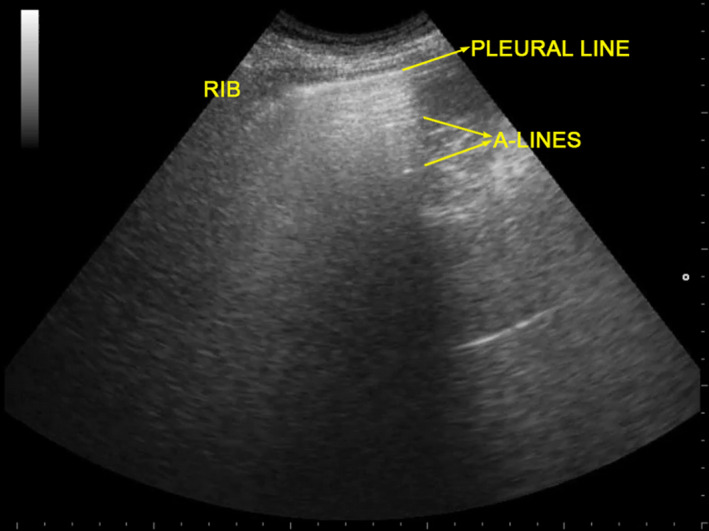
Lung ultrasound of normal aerated lung. A lines are visible: they are a repetition of the pleural line at the same distance from skin to pleural line. This indicates the presence of air below the pleural line (which corresponds to the parietal pleura). A lines can be complete or partial (as in this image)
Demonstration of B lines are described as hyperechoic laser‐like artifacts that resemble a “comet tail” (Figure 2). These arise from the pleural line and move in concert with a sliding lung. The A lines are generally not present. B1 lines are associated with an interstitial syndrome and diminished lung aeration. B2 lines are confluent lines appearing as a “white lung” (called also glass‐rockets), equivalent to computed tomography (CT) ground‐glass opacities. This suggests a more severe loss of lung aeration (Movies S2 and S3).
Figure 2.
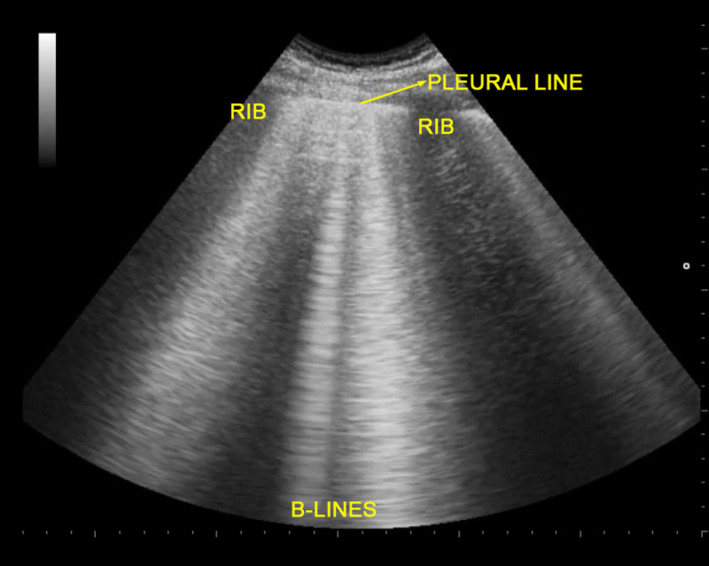
Lung ultrasound of interstitial syndrome, characterized by the presence of three or more B lines between two ribs. B lines are hyperechoic laser‐like artifacts that resemble a comet tail, arise from the pleural line and move in concert with lung sliding. A lines are wiped out
Lung consolidations (C) are associated with hepatization of lung parenchyma with or without air bronchograms, and suggest major loss of lung aeration (atelectasis vs pneumonia; Movie S4).
We have not identified an ultrasound appearance that would be pathognomonic of COVID‐19. 2
2. LUNG ULTRASOUND SCORE
The lung ultrasound score (LUS) has been shown to be a useful tool in intensive care (ICU) patients with adult respiratory distress syndrome (ARDS). We feel that this has been of value in assessing severity of lung involvement with COVID‐19. 3 , 4
One may perform a topographic analysis of the underlying lung regions daily without moving the patient. A scan of the three different areas of the thorax: anterior, lateral, and posterior, and then superior and inferior segments are performed. Thus, six specific regions for each lung are defined and categorized by one of four different aeration patterns.
A point scoring system is employed by region and ultrasound pattern as: A = 0 point, B1 = 1 point, B2 = 2 points, C = 3 points. Thus, a LUS of 0 is normal, and 36 would be the worst.
LUS score can be used to follow the clinical patient trajectory in which an increased score means decreased lung aeration, while on the contrary, a decrease in score means an increase in lung aeration limiting the need of chest x‐ray and CT scan. 2
An experienced sonographer can do this examination within 5 minutes, while brief training and about 25 supervised exams seem to be sufficient to achieve a basic ability to perform the study. 5 A prior study showed the impact of LU to affect clinical decisions in up to 50% of intensive care unit patients. 6
3. CLINICAL CONTEXT
Although a patient's clinical context allows for an improved pretest estimate of COVID‐19 lung involvement, it appears that LU may serve as a bedside tool to improve evaluation of lung involvement, and also reduce the use of chest x‐rays and CT. 7 In addition, several intensive care units following central venous line positioning with ultrasound, have not been routinely obtaining post insertion chest x‐rays. 8 , 9
While the ability of a chest x‐ray to discriminate a bacterial pneumonia from a non‐bacterial infection is no more than 60%, 10 LU has a higher sensitivity (80%). 11 Specific comparison studies in critically ill patients regarding viral pneumonia, however, are few. 12
4. CONCLUSION
During this pandemic we have used LU in patients suspected or diagnosed with COVID‐19. Application of LUS has allowed for identification of patients with lung involvement and severity. In addition, serial studies help us follow for progression or regression of disease.
With the application of LU we have had a noted reduction in use of chest x‐rays and CT scans during this pandemic, helping us to make care and management of our patients a little more efficient.
CONFLICT OF INTEREST
Luigi Vetrugno received travel support for Congress Lecture by Cook Medical. The other authors declare no conflict of interest.
AUTHORS’ CONTRIBUTIONS
LV and DO: concept, design, and drafting the manuscript. TB, FB, EB, FB, GF: critical revision of the manuscript for important intellectual content. RK and DL: critical review and editing of the manuscript. All authors read and approved the final manuscript.
Supporting information
Movie S1. Anterior region with A lines.
Movie S2. Posterior region with coalescent B lines.
Movie S3. A thickened and disrupted pleural line with B lines.
Movie S4. A subpleural consolidation disappearing with inspiration.
Vetrugno L, Bove T, Orso D, et al. Our Italian experience using lung ultrasound for identification, grading and serial follow‐up of severity of lung involvement for management of patients with COVID‐19. Echocardiography. 2020;37:625–627. 10.1111/echo.14664
REFERENCES
- 1. Peng QY, Wang XT, Zhang LN; Chinese Critical Care Ultrasound Study Group ( CCUSG ) . Finding of lung ultrasonography of novel coronavirus pneumonia during the 2019–2020 epidemic. Intensive Care Med. 2020. 10.1007/s00134-020-05996-6. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bouhemad B, Mongodi S, Gabriele V, Rouquette I. Ultrasound for “Lung Monitoring” of ventilation patients. Anesthesiology. 2015;122:437–447. [DOI] [PubMed] [Google Scholar]
- 3. Man MA, Dantes E, Domokos Hancu B, et al. Correlation between transthoracic lung ultrasound score and HRCT features in patients with interstitial lung diseases. J Clin Med. 2019;8(8):E1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zhao Z, Jiang L, Xi X, et al. Prognostic value of extravascular lung water assessed with lung ultrasound score by chest sonography in patients with acute respiratory distress syndrome. BMC Pulm Med. 2015;15:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rouby JJ, Arbelot C, Gao Y, et al. Training for lung ultrasound score measurement in critically Ill patients. Am J Respir Crit Care Med. 2018. 10.1164/rccm.201802-0227LE. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Xirouchaki N, Kondili E, Prinianakis G, et al. Impact of lung ultrasound on clinical decision making in critically ill patients. Intensive Care Med. 2014;40:57–65. [DOI] [PubMed] [Google Scholar]
- 7. Brogi E, Bignami E, Sidoti A, et al. Could the use of bedside lung ultrasound reduce the number of chest x‐rays in the intensive care unit? Cardiovasc Ultrasound. 2017;15:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Smit JM, Haaksma ME, Lim EHT, et al. Ultrasound to detect central venous catheter placement associated complications: a multicenter diagnostic accuracy study. Anesthesiology. 2020;132:781–794. [DOI] [PubMed] [Google Scholar]
- 9. Vetrugno L, Bove T, Orso D, Flabio B, Boero E, Ferrari G. Lung ultrasound and COVID‐19 “pattern”: not all that glitters today is gold tomorrow. J Ultrasound in Med. (Accepted for publication). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Courtoy I, Lande AE, Turner RB. Accuracy of radiographic differentiation of bacterial from nonbacterial pneumonia. Clin Pediatr (Phila). 1989;28(6):261–264. [DOI] [PubMed] [Google Scholar]
- 11. Berce V, Tomazin M, Gorenjak M, Berce T, Lovrenčič B. The usefulness of lung ultrasound for the aetiological diagnosis of community‐acquired pneumonia in children. Sci Rep. 2019;9(1):17957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Testa A, Soldati G, Copetti R, Giannuzzi R, Portale G, GentiloniSilveri N. Early recognition of the 2009 pandemic influenza A (H1N1) pneumonia by chest ultrasound. Crit Care. 2012;16(1):R30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Movie S1. Anterior region with A lines.
Movie S2. Posterior region with coalescent B lines.
Movie S3. A thickened and disrupted pleural line with B lines.
Movie S4. A subpleural consolidation disappearing with inspiration.


