Less than six months ago, no‐one had heard of COVID‐19 and few people knew what a coronavirus was, yet today it is on everyone's lips. On 11 March 2020, the WHO declared the outbreak a global pandemic, and the disease has spread to multiple countries across the globe. COVID‐19 is characterized by a fever, dry cough, fatigue and shortness of breath, and for the majority the symptoms will be minor; however, for a few, the illness can progress to pneumonia and multi‐organ failure. While data are emerging, it seems that the mortality rate is of the order of 1–2% [1]. So, what does the epidemic mean for people with diabetes?
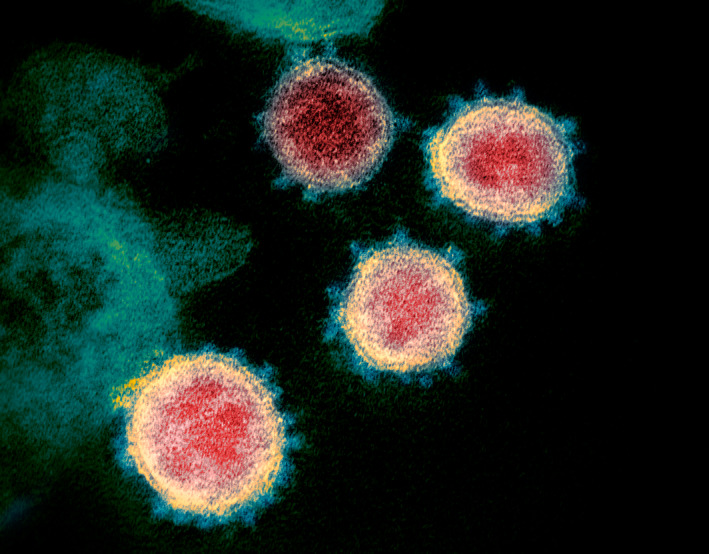
Credit: NIAID‐RML / NATIONAL INSTITUTES OF HEALTH / SCIENCE PHOTO LIBRARY
Caption: COVID‐19 coronavirus particles, coloured transmission electron micrograph (tEM). Also called severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), this virus causes the disease COVID‐19. This sample was isolated from a patient in the USA. SARS‐CoV‐2 was first identified in Wuhan, China, in December 2019. It is an enveloped RNA (ribonucleic acid) virus. The coronaviruses take their name from their crown (corona) of surface proteins, which are used to attach and penetrate their host cells. As of mid‐March 2020, over 230,000 people have been infected with over 9,500 deaths.
People with diabetes have a higher overall risk of infection that results from multiple perturbations of innate immunity. While humoral immunity appears relatively unaffected, people with diabetes have impaired phagocytosis by neutrophils, macrophages and monocytes, impaired neutrophil chemotaxis and bactericidal activity, and impaired innate cell‐mediated immunity. As overall mortality related to cardiovascular disease continues to decline among people with diabetes, pneumonia has become an increasingly important cause of death in diabetes, with different contributing pathogens [2].
Whether people with diabetes have a higher susceptibility to COVID‐19 is currently unknown, but there is a perception that the risk is higher both of infection and severe disease. For example, the first three deaths related to COVID‐19 in Hong Kong all occurred in people with diabetes. In a large series, 173 cases of 1099 laboratory‐confirmed COVID‐19 cases (16%) in China were classified as severe [3]. Sixteen percent of those with severe disease had diabetes; in contrast only 5.7% of the remaining 926 cases with mild disease had diabetes. Likewise, 24% of those with severe disease had hypertension, compared to 13% among those with mild disease, highlighting the increased risk of adverse outcomes among those with chronic diseases like diabetes.
It is currently unknown why people with diabetes, hypertension or other chronic diseases are more severely affected by COVID‐19, but one possible explanation involves angiotensin‐converting enzyme 2 (ACE2). ACE2 is present in cardiac, kidney, lung and intestinal tissue, and by converting angiotensin II to angiotensin 1–7, it counteracts the effects of angiotensin II and promotes vasodilation. In a similar manner to the coronavirus that caused Severe Acute Respiratory Syndrome (SARS‐CoV), the novel coronavirus responsible for COVID‐19 utilizes ACE2 on the surfaces of epithelial cells to bind and gain entry to infected cells [4, 5]. Diabetes and conditions such as hypertension are associated with activation of the renin‐angiotensin system in different tissues. Furthermore, people with diabetes and hypertension are often treated with ACE inhibitors and angiotensin receptor blockers (ARBs), which can lead to increased expression of ACE2, thereby facilitating viral uptake and increasing the risk of severe infection for people with diabetes [6]. Whilst these observations have led to suggestions that switching people on renin‐angiotensin system blockers to other agents may modify disease risk [6], this would be premature and unwarranted in the absence of any experimental evidence to support this approach. On the contrary, treatment with ARBs has been proposed as a potential therapeutic strategy for COVID‐19 [7], supported by observations that blocking the renin‐angiotensin system in animal models attenuated the lung injury caused by the SARS‐CoV, which also utilizes ACE2 [8]. A recent position statement from the European Society of Cardiology also strongly recommends that physicians and patients continue treatment with their usual anti‐hypertensive treatment and that there is no clinical or scientific evidence to suggest that treatment with ACE inhibitors or ARBs should be discontinued because of the COVID‐19 infection [9].
Direct infection, however, is not the only issue for people with diabetes. The infection and outbreak has challenged the delivery of healthcare in many ways. Healthcare professionals in hospitals may be re‐deployed to caring for the increasing caseloads of people admitted with fever and suspected disease, and the workforce may be further diminished as healthcare providers become affected by the disease. Clinic visits may be postponed and treatment for diabetes‐related issues may be delayed. There may be an unwillingness of people with diabetes to expose themselves to potential infection and so they may avoid attendance at hospitals, clinics and retinal screening, although this may be overcome to a certain extent by utilising phone or video consultations or other forms of communication. As healthcare delivery becomes increasingly interrupted and fragmented, access to basic medical supplies such as insulin may become increasingly difficult, somewhat akin to the challenges faced in other natural disasters. Panic buying has already made it harder for people with diabetes to obtain alcohol wipes or gel to perform hygiene before injection or glucose monitoring in some regions.
Lack of access to medications and supplies has also been experienced by people who need to undergo quarantine. Colleagues in Hong Kong, for example, were contacted by people quarantined on a cruise ship who had run out of medications, including insulin, due to unexpected delays to their travels and difficulty in gaining access to medications. Another contagion that has occurred as a result of COVID‐19 is fear, and the resulting anxiety and sleep disturbances may adversely affect glucose control.
Some important lessons have been learned with regard to controlling the epidemic and should be shared and highlighted. Back in March 2003, almost exactly 17 years ago, several Asian countries and subsequently other countries were hit by the SARS outbreak caused by the SARS coronavirus [10]. Since then, many measures have been implemented in the region to prevent similar outbreaks of infectious diseases. For example, in Hong Kong, these measures include increasing distances between inpatient beds, and provision of negative‐pressure ventilation rooms and isolation wards in all major public hospitals. There are defined protocols for protection against aerosol‐generating procedures, as well as a public health response alert system. Perhaps most important of all, however, is the response and attitude of the general public. Having experienced the threat of a major infectious disease outbreak, the population as a whole has developed a high degree of awareness, tenacity and preparedness in doing their part to help avoid transmission.
In Hong Kong, people have accepted the need for frequent handwashing, environmental hygiene and wearing surgical masks, regardless of whether one has respiratory symptoms or not. There is tolerance towards social isolation and avoiding unnecessary gatherings during the outbreak. These social‐distancing measures, coupled with government policies towards restricting travel, limiting transmission in large‐scale institutions, such as universities and schools, rigorous contact tracing, early testing, diagnosis, isolation and treatment, appear to be having some effect in controlling the spread in some Asian countries, and flattening the epidemic curve [11]. As an increasing number of countries find themselves battling a rapid rise in cases, the lessons learned should serve to inform and guide the public health response to this alarming pandemic. These lessons are only now being learned in Europe.
Lastly, another casualty of the COVID‐19 epidemic was this year's Diabetic Medicine symposium [12]. In line with many other medical organizations, Diabetes UK took the decision to cancel this year's Professional Conference in a bid to limit spread of the virus. Although people cannot hear the lectures, the accompanying review articles are still available in the journal [13, 14, 15].
Diabet. Med. 37, 723–725(2020)
References
- 1. Baud D, Qi X, Nielsen‐Saines K, Musso D, Pomar L, Favre G. Real estimates of mortality following COVID‐19 infection. Lancet Infect Dis 2020; 10.1016/S1473-3099(20)30195-X. Epub 12 March 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wu H, Lau ESH, Ma RCW, Kong APS, Wild SH, Goggins W et al. Secular trends in all‐cause and cause‐specific mortality rates in people with diabetes in Hong Kong, 2001–2016: a retrospective cohort study. Diabetologia 2020; 63: 757–766. [DOI] [PubMed] [Google Scholar]
- 3. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med 2020; 10.1056/NEJMoa2002032. Epub 28 February 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lu R, Zhao X, Li J, Niu P, Yang B, Wu H et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 2020; 395 (10024): 565–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hoffman M, Kleine‐Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S et al. SARS‐CoV‐2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020: 10.1016/j.cell.2020.02.0524. Epub 4 March 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID‐19 infection? Lancet Resp Med 2020; 10.1016/S2213-2600(20)30116-8. Epub 11 March 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zhang H, Penninger JM, Li Y, Zhong N, Slutsky AS. Angiotensin‐converting enzyme 2 (ACE2) as a SARS‐CoV‐2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med 2020; 10.1007/s00134-020-05985-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Imai Y, Kuba K, Rao S, Huan Y, Guo F, Guan B et al. Angiotensin‐converting enzyme 2 protects from severe acute lung failure. Nature 2005; 436: 112–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. de Simone G, ESC Council on Hypertension . Position Statement of the ESC Council on Hypertension on ACE‐Inhibitors and Angiotensin Receptor Blockers. European Society of Cardiology. 13 March 2020. Available at https://www.escardio.org/Councils/Council‐on‐Hypertension‐(CHT)/News/position‐statement‐of‐the‐esc‐council‐on‐hypertension‐on‐ace‐inhibitors‐and‐ang.
- 10. Lee N, Hui D, Wu A, Chan P, Cameron P, Joynt GM et al. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Eng J Med 2003; 348: 1986–1994. [DOI] [PubMed] [Google Scholar]
- 11. Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD. How will country‐based mitigation measures influence the course of the COVID‐19 epidemic? Lancet 2020; 10.1016/S0140-6736(20)30567-5. Epub 9 March 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Nouwen A, Speight J, Pouwer F. Holt RIG How psychosocial and behavioural research has shaped our understanding of diabetes. Diabet Med 2020; 37: 377–379. [DOI] [PubMed] [Google Scholar]
- 13. Snoek FJ. Looking back on 25 years of the PSAD study group. Diabet Med 2020; 37: 380–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. De Wit M, Trief PM, Huber JW, Willaing I. State of the art: understanding of, and integration in, the social context and diabetes care. Diabet Med 2020; 37: 473–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kubiak T, Priesterroth L, Barnard‐Kelly KD. Psychosocial aspect of diabetes technology. Diabet Med 2020; 37: 448–454. [DOI] [PubMed] [Google Scholar]


