On 20 January 2020, the first COVID‐19 case was reported in Shanghai, China. As of 12 March 2020, 344 cases with laboratory‐confirmed COVID‐19 infection have been detected in Shanghai, of which three died, 321 patients are discharged, 20 patients still receive ongoing treatments (Shanghai Municipal Health Commission, 2020). All confirmed patients with COVID‐19 were centralized in Shanghai Public Health Medical Centre to receive standardized treatments. Shanghai is an international metropolis with more than 27 million residents, of which 9.7 million are commuting population. It has been a challenge for Shanghai to control the COVID‐19 outbreak among the high‐density and high‐mobility population. On 21 January 2020, Shanghai Municipal Health Commission set‐up fever clinics in 110 hospitals as frontline services to screen suspected patients. The hospitals went into a ‘state of alert’ and adopted strategies to cope with the COVID‐19 outbreak (Cohen & Normile, 2020; Wang, Horby, Hayden, & Gao, 2020).
Zhongshan Hospital of Fudan University is a general hospital listed as the top 5 academic centre in China and is one of the assigned sentinel hospitals with fever clinics. A hospital‐wide COVID‐19 committee was set‐up and initiated a response framework to prevent and safeguard patients, family, and staff from COVID‐19 infection. We briefly present our response framework, including procedures, human resources, patient management, and staff emotional support, to share our experiences in this global health emergency.
Procedures and policies were initiated based on the characteristics of COVID‐19 targeting the sources of infection, routes of transmission, diagnosing, treating, and reporting. Other procedures were related to wearing personal protective equipment, allocation of supplies, and patient transfers (Chang, Xu, Rebaza, Sharma, & Dela Cruz, 2020). Allocation of supplies was strictly based on the stratification of infection risk. All procedures were dynamic, and changes were implemented based on the emerging new COVID‐19 knowledge to ensure up‐to‐date requirements and reality of managing the hospital in a challenging climate (Sun, Chen, & Viboud, 2020).
Human resource management involved a review of staff capacity and identified staff availability to allocate to a COVID‐19 rapid response team. The criteria for nurses were minimal 3‐year work experience in emergency, critical care, respiratory, or infection departments. For doctors the criterium was being an attending physician or above. To ensure staff availability of the vital units, we assigned nurses and doctors to emergency departments and fever clinic. Furthermore, responding to the national‐wide assignment, our hospital organized four teams comprised of 47 doctors, 110 nurses, and six administrators to support the hospitals in Wuhan and the Shanghai Public Health Medical Centre.
Patient management and flow was regulated to safeguard in‐ and out‐of‐hospital patients. To minimize intra‐hospital infection among fever patients, two COVID‐19 fever clinics, independently located, were successively set‐up with 17 quarantine rooms for highly suspected patients. As of 27 February 2020, the fever clinics received 3,145 patients, monitored 44 suspected patients and three patients were confirmed with COVID‐19 (Figure 1). Hospital entrances were controlled by staff and each patient/visitor had to follow safety procedures (Figures 2 and 3). These included temperature check and a survey of clinical history (Table 1). Only patients with critical conditions were admitted after COVID‐19 screening from 23 January–3 February 2020. During the outbreak, we continued the haemodialysis and chemotherapy outpatient services under strict surveillances. With the daily confirmed cases decreasing in Shanghai, we gradually resumed outpatient services and elective surgery to satisfy the medical demand of patients while preventing the intra‐hospital infection. Restricted visiting times were implemented (10:00–12:00 hrs and 14:00–16:00 hrs), and only one visitor per patient was allowed. Social media channels were initiated to communicate and provide online consultations with the public and chronically ill patients.
Figure 1.
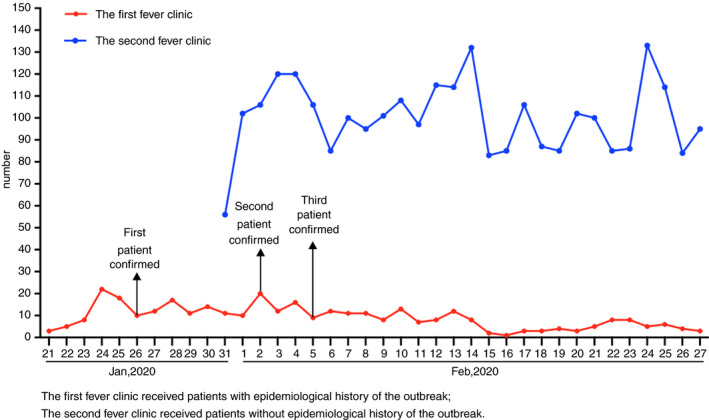
Patient flow of the fever clinics [Colour figure can be viewed at wileyonlinelibrary.com]
Figure 2.
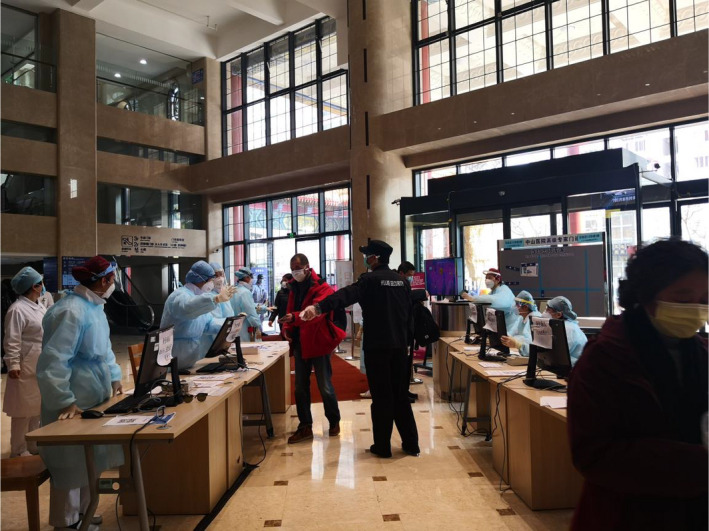
Entrance of outpatient department: conducting temperature check and epidemiological survey
Figure 3.

Four steps to complete entrance check in inpatient ward: temperature check; hands disinfection; epidemiological survey; visiting information record [Colour figure can be viewed at wileyonlinelibrary.com]
Table 1.
Survey clinical and contact history
| Items | Answer of the patient | Answer of the visitor | |||
|---|---|---|---|---|---|
| Clinical symptoms and signs | Did you have fever over the previous 14 days? | No | Yes | No | Yes |
| Did you have symptoms related respiratory tract infection, such as cough, over the previous 14 days? | No | Yes | No | Yes | |
| Did you frequently feel fatigued over the previous 14 days? | No |
Yes (diagnosed with: ______) |
No |
Yes (diagnosed with: ______) |
|
| Did you frequently have diarrhoea over the previous 14 days? | No | Yes | No | Yes | |
| Contact traces | Did you have travel history or residence history in Wuhan and surrounding areas or other communities with COVID−19 case reports over the previous 14 day? | No |
Yes (Name of city: _____) (Arrival date at Shanghai: ) |
No |
Yes (Name of city: _____) (Arrival date at Shanghai: ) |
| Did you have contact with patients with fever or respiratory tract symptoms from Wuhan and surrounding areas or other communities with COVID−19 case reports over the previous 14 days? | No | Number of people with fever you contacted: ____ | No | Number of people with fever you contacted: ____ | |
| Their relations with you: ____ | No | Their relations with you: ____ | |||
| District of the patents: ____ | No | District of the patents: ____ | |||
| Date of patients’ arrival to Shanghai: ____ | No | Date of patients’ arrival to Shanghai: ____ | |||
| Were you around the clustering occurrence of COVID−19 or epidemically associated with COVID−19 confirmed patients? | No | Number of people you contacted: ____ | No | Number of people you contacted: ____ | |
| Date of your contact: ____ | No | Date of your contact: ____ | |||
| Date of patients’ arrival to Shanghai: ____ | No | Date of patients’ arrival to Shanghai: ____ | |||
| Their relations with you: ____ | No | Their relations with you: ____ | |||
| District of the people you contacted: ____ | No | District of the people you contacted: ____ | |||
Please filling the form and return it back to nurses. Thank you for your cooperation!
I acknowledgement the above information is true . Signature (patient): Date:
Relationship with patient: Signature (family): Date:
The unexpected outbreak with high transmission brings fear and anxiety to medical staff. Emotional support was initiated by psychosocial intervention teams COVID‐19 Balint group (Abeni et al., 2014). These groups included psychiatrists and volunteers. Besides, a telephone hotline and WeChat account (smartphone application with similar features as WhatsApp/Facebook) were provided as well. Front‐line medical and nursing staff (N = 160) who are working in Wuhan and their family members were provided with similar psychological support.
The COVID‐19 outbreak is challenging for all healthcare professionals on a collective and individual level. The unconditional professionalism of staff is heroic to combat the COVID‐19 epidemic. By implementing the response framework, our hospital was able to maintain its operational business for all patients without any intra‐hospital COVID‐19 infections. By sharing our clinical experience, we hope that other hospitals facing COVID‐19 outbreaks in their countries can enhance their preparedness and performance to safeguard patients, families, and staff.
CONFLICT OF INTEREST
We declare no competing interest.
REFERENCES
- Abeni, M. S. , Magni, M. , Conte, M. , Mangiacavalli, S. , Pochintesta, L. , Vicenzi, G. , … Corso, A. (2014). Psychological care of caregivers, nurses and physicians: A study of a new approach. Cancer Medicine, 3(1), 101–110. 10.1002/cam4.163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang, D. , Xu, H. , Rebaza, A. , Sharma, L. , & Dela Cruz, C. S. (2020). Protecting health‐care workers from subclinical coronavirus infection. The Lancet Respiratory Medicine, 8(3), e13. 10.1016/S2213-2600(20)30066-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, J. , & Normile, D. (2020). New SARS‐like virus in China triggers alarm. Science, 367(6475), 234–235. 10.1126/science.367.6475.234 [DOI] [PubMed] [Google Scholar]
- Shanghai Municipal Health Commission . (2020). Yesterday at 0–12, no new confirmed cases of coronavirus pneumonia in Shanghai. 12th March 2020. Retrived from http://wsjkw.sh.gov.cn/xwfb/20200312/26f752ed950e46a19b99851bc63d76f9.html.
- Sun, K. , Chen, J. , & Viboud, C. (2020). Early epidemiological analysis of the coronavirus disease 2019 outbreak based on crowdsourced data: a population level observational study. Lancet Digital Health, 10.1016/S2589-7500(20)30026-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, C. , Horby, P. W. , Hayden, F. G. , & Gao, G. F. (2020). A novel coronavirus outbreak of global health concern. The Lancet, 395(10223), 470–473. 10.1016/S0140-6736(20)30185-9 [DOI] [PMC free article] [PubMed] [Google Scholar]


